Abstract
Antenatal glucocorticoids treatment has been shown to correct pulmonary immaturity. The thymidine analog bromodeoxyuridine (BrdU) is incorporated into S-phase cells and used as a marker of DNA synthesis. In this study, we investigated the effect of antenatal glucocorticoid administration on DNA synthesis and RNA and protein content in nitrofen-induced congenital diaphragmatic hernia (CDH) in rats to better understand the effect of antenatal glucocorticoids on CDH lung. The CDH model was induced in pregnant rats using nitrofen. Dexamethasone (0.25 mg/kg) was given on d 18.5 and 19.5 of gestation (term = 22 d). BrdU was administered 1 h before fetuses were killed on d 21, and detected by immunohistochemistry. DNA synthesis was evaluated by percentage of BrdU-incorporated nuclei (BrdU labeling index). Total RNA and soluble protein were extracted from another set of left lungs to measure RNA and protein content. BrdU labeling index and total RNA content were significantly decreased in CDH lung compared with control rats. Antenatal dexamethasone treatment significantly increased BrdU labeling index and RNA and protein content in the left CDH lung. Our findings of decreased DNA synthesis and decreased RNA and protein content in CDH lung suggest that lung growth and development are suppressed in hypoplastic CDH lung. Increased DNA synthesis and increased RNA and protein content in dexamethasone-treated CDH lung suggest that antenatal glucocorticoids may accelerate fetal lung growth and development in CDH.
Similar content being viewed by others
Main
The high mortality in patients with CDH has been shown to be the result of pulmonary hypoplasia and persistent pulmonary hypertension(1). Although newer treatment modalities, including high-frequency ventilation, extracorporeal membrane oxygenation, surfactant therapy, and nitric oxide inhalation, have been introduced in an attempt to improve survival in patients with CDH, the mortality in this condition still remains high(1, 2).
Recent improvements in antenatal sonography have resulted in a large number of CDH cases being diagnosed antenatally(3), which provided a possibility of antenatal treatment for severe CDH patients. Recently, antenatal administration of glucocorticoid has been proposed as a noninvasive modality in promoting fetal lung maturation and differentiation. Several control trials have shown the beneficial effects of antenatal glucocorticoid therapy as a means of promoting lung maturation and preventing respiratory distress syndrome in premature human newborns(4, 5). In experimentally produced CDH in animals, it has been reported that antenatal glucocorticoid treatment improves surfactant biochemical immaturity, increases lung compliance and distensibility, enhances lung morphology, and reduces pulmonary vascular adventitial and medial thickness(6–11). The exact mechanism by which antenatal glucocorticoid therapy improves pulmonary immaturity in CDH is not fully understood.
BrdU is a thymidine analog that is incorporated into the newly replicated DNA of S-phase cells. Since an antibody specific for BrdU was developed by Gratzner(12), immunohistochemical staining of BrdU-labeled nuclei has been used to evaluate DNA synthesis and cell kinetics both in vitro and in vivo(12, 13). As DNA-synthesizing cells are in the proliferative phase of the cell cycle, BrdU can be used as a marker of cell proliferation activity. The percentage of BrdU-positive cells (BrdU LI) is often used to evaluate the proliferative activity of malignant tumors to predict the prognosis(13). BrdU LI and RNA levels are considered to indicate cellular activity. In the present study, we investigated the effect of antenatal Dex administration on DNA synthesis as well as protein and RNA content in CDH lung in rats to elucidate the mechanisms involved in the acceleration of fetal lung development by antenatal glucocorticoid treatment.
METHODS
Creation and treatment of CDH.
Timed pregnant Sprague Dawley rats (vaginal plug positive, d 0; term, d 22) were administered 100 mg of nitrofen (WAKO Chemicals, Osaka, Japan) dissolved in olive oil as a single dose via a stomach tube under short-term anesthesia on d 9.5 of gestation to induce CDH in fetal rats. In control animals, the same dose of olive oil was given without nitrofen. Antenatal Dex (0.25 mg/kg) or normal saline was administered intraperitoneally on d 18.5 and 19.5 of gestation. The dose and timing of Dex administration were chosen as it approximates dose and timing currently used in human pregnancy to hasten maturation of fetal lungs(4, 5), and it is known to be the lowest effective dose that has resulted in biochemical and morphologic improvement with the least effect on somatic and pulmonary growth(6). The fetuses were divided into three groups: nonnitrofen, non-CDH, and nonsteroid (control, n = 16); nitrofen-induced CDH (CDH, n = 16); and nitrofen-induced CDH with antenatal Dex treatment (CDH + Dex, n = 16). Eight lungs in each group were used for the immunohistochemical detection of BrdU. Left lungs in the other eight fetuses in each group were used for the measurement of RNA and protein content.
Administration and immunohistochemical detection of BrdU.
To label cells synthesizing DNA, the pregnant rats received an i.v. bolus injection of 50 mg/kg BrdU in saline. One hour later, cesarean section was performed under anesthesia, lungs were dissected out, and the weights of the fetus, lungs, and liver were recorded. The lungs were immediately inflated with 10% formalin at a pressure of 20 cm H2O.
BrdU incorporation into proliferating cells was determined immunohistochemically using a mouse MAb. The specimens were fixed in 10% formalin and embedded in paraffin. Three-micrometer-thick paraffin sections were cut, mounted on poly-lysine–coated glass slides, and stained using standard streptavidin-biotin immunoperoxidase method (Universal LSAB 2 kit, Dako Ltd., Glostrup, Denmark). To denature DNA and expose BrdU incorporated in nucleus, the dewaxed sections were placed in 10 mM citrate buffer (pH 6.0) and heated in a microwave oven twice for 5 min before staining. Anti-BrdU MAb (Dako) was used as the first antibody at a dilution of 1:40, at 4°C overnight. A light hematoxylin counterstain was used for nuclear identification. Controls for specificity consisted of omission of the first antibody.
Counting procedure of BrdU-labeled cells.
BrdU uptake by DNA replicating cells was evaluated in two components separately:1) the alveolar walls comprising epithelial cells (pneumocytes), endothelial cells, and fibroblasts in the bronchoalveolar duct and alveolar sacs excluding terminal bronchiolar epithelium; and 2) airway epithelium in bronchioles, including terminal bronchiolar epithelium. Smooth muscle and vascular and hematogenous elements were excluded from counting. A minimum of two different sections from each specimen were chosen for counting. The total number of nuclei in each of these compartments, and the number of BrdU-positive nuclei therein, were counted using a computerized image analysis system (Interactive Image Processing System IPS ver. 4.01, Alcatel TITN Answare, Cedex, France). At least 10 random fields of alveolar region and all bronchioles were captured with video camera at ×400 magnification, and at least 1,000 nuclei of each component were evaluated per section. Results were expressed as the percentage of BrdU-positive nuclei (BrdU LI).
Measurement of total RNA and protein content.
Another set of lungs were dissected, snap-frozen, and stored at −70°C until RNA and protein were extracted. Weights of the fetus and left lung were recorded. Total RNA and soluble protein were extracted from eight left lungs in each group using commercially supplied solution (Trizol Reagent, Life Technologies, Paisley, U.K.) according to the recommended protocol. RNA concentration of the extract was measured using a Beckman DU 640 UV spectrometer (Beckman Instrument Inc., Fullerton, CA, U.S.A.), and protein concentration was measured using BCA Protein Assay Kit (Pierce, Rockford, IL, U.S.A.). Total RNA and soluble protein content was calculated as the total amount extracted (in micrograms) divided by left lung weight (in milligrams).
Statistics.
Results were expressed as means ± SD. Data were analyzed by ANOVA. The statistical significance between groups was determined by Fisher's protected least significant difference test. StatView software (Abacus Concepts, Berkeley, CA, U.S.A.) was used for all statistical work. A p value of less than 0.05 was taken as significant.
RESULTS
Immunostaining of BrdU.
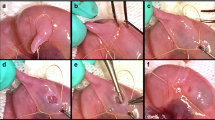
Immunoreactivity of BrdU was confined to the nucleus, and positive nuclei were easily detectable in each specimen (Figs. 1–3). Numerous BrdU-positive nuclei were found both in the alveolar wall and airway epithelium in the normal control lung (Fig. 1). The number of BrdU-positive nuclei was markedly decreased in CDH lungs (Fig. 2) and increased in CDH lung by antenatal Dex treatment (Fig. 3).
The data of BrdU LI are summarized in Table 1. The cells in alveolar walls showed higher BrdU LI than those in airway epithelium in each group. BrdU LI was significantly decreased in the CDH group compared with the control group both in alveolar wall and airway epithelium in both lungs (p < 0.01). Antenatal Dex treatment significantly increased BrdU LI both in alveolar walls and airway epithelium in left lung (p < 0.05). In right lung, BrdU LI was slightly increased in the CDH + Dex group compared with the CDH group; however, there was no statistical difference. To determine whether these alterations were restricted to the lung, the BrdU LI was also determined in liver. There was no difference of BrdU LI in the liver cells among the three groups (data not shown).
Total RNA and protein content.
Lung weight/body weight ratio and total RNA and protein content are shown in Table 2. Left lung weight was significantly smaller in CDH fetuses than in control animals (p < 0.01). It was increased by antenatal Dex treatment, but this was not statistically significant. RNA content was significantly decreased in the CDH group compared with the control group (p < 0.05). Protein content was also decreased in the CDH group compared with the control group, but this was not statistically significant. RNA as well as protein content was significantly increased in the CDH lung by antenatal Dex treatment (p < 0.05).
DISCUSSION
The beneficial effects of antenatal glucocorticoid therapy are now well established as a means of promoting lung maturation and preventing respiratory distress syndrome in premature infants(4, 5). The similarities between the lungs of babies who die from CDH and the lungs of premature infants with respiratory distress syndrome suggest a possible role for prenatal glucocorticoids in enhancing lung maturation in CDH. Little is known, however, about the underlying regulatory mechanisms of accelerated fetal lung growth by glucocorticoids.
The present study focused on the effects of antenatal glucocorticoid therapy on DNA synthesis. To evaluate the cellular DNA synthesis, we used a thymidine analog, BrdU, a sensitive and specific indicator of DNA synthesis and cell proliferation. We also measured total RNA and protein content of lungs to evaluate cellular protein synthesizing activity. Our results clearly showed that DNA synthesis and total RNA content were significantly decreased in nitrofen-induced CDH lung compared with control lungs. Antenatal Dex treatment significantly enhanced DNA synthesis and increased total RNA and protein content in CDH lung. These findings suggest that cellular proliferative activity and protein synthesis are suppressed in hypoplastic CDH lung, resulting in the retardation of lung growth and development. Antenatal glucocorticoid administration accelerates fetal lung growth and development by stimulating the cellular proliferative activity and protein synthesis in hypoplastic CDH lung.
Increased DNA synthesis and RNA and protein content are reported in other models of accelerated lung growth, such as tracheal occlusion and postpneumonectomy lung. Tracheal occlusion before birth can cause dramatic lung growth and maturation in fetuses with pulmonary hypoplasia(14–16). De Paepe et al.(17) showed that increased cell proliferation and accelerated architectural and cellular maturation were observed in lungs in the tracheal-occluded fetal rabbit by postligation d 4 and 5. Brody et al.(18) and Rannels et al.(19) have shown that DNA synthesis was elevated and total lung RNA and protein were increased during rapid lung growth after pneumonectomy. Knowledge of these cellular mechanisms may help us to elucidate the physiologic and molecular basis of lung development seen in these conditions, including Dex-treated CDH lung, and may enable us to manipulate fetal and perinatal lung growth with antenatal therapy.
Recently, antenatal administration of glucocorticoids has been proposed as a noninvasive modality in promoting fetal lung maturation and differentiation. In experimentally produced CDH in animals, antenatal glucocorticoid treatment has been reported to improve morphologic and surfactant biochemical immaturity(6, 7). Our findings of increased DNA and protein synthesis by antenatal Dex treatment may suggest that these improvements were regulated at the molecular level. Losty et al.(8) have reported that antenatal Dex treatment increases lung compliance and distensibility. One of the possible mechanisms by which antenatal glucocorticoids therapy improves pulmonary compliance is that glucocorticoids increases lung tissue volume by stimulating lung proliferative activity and protein synthesis.
Beck et al.(20) reported that lung weight per body weight was 13% increased by antenatal betamethasone administration in rhesus fetus, and Asabe et al.(21) reported that lung weight per body weight was about 20% increased by antenatal Dex treatment in the oligohydramnios-induced hypoplastic lung of rabbit fetuses. Our findings suggest that increased DNA synthesis and RNA and protein contents by antenatal Dex treatment may be responsible for the increase of lung weight seen in these models.
In the present study, DNA synthesis and RNA and protein contents were significantly increased, whereas lung weight was not significantly increased in Dex-treated CDH lung. One possible reason is the removal of excess lung water by Dex treatment. Ariagno et al.(22) demonstrated a marked steroid-induced reduction in lung water content in newborn mice raised in an 80% oxygen environment. They showed that the decrease in lung water was related to a loss of fluid from the interstitial tissue of the lung. Sahebjami et al.(23) have also shown that steroids can accelerate the resolution of pulmonary edema and improve alveolar volume. Their findings, together with our results of increase in lung proliferative activity as well as RNA and protein content by antenatal Dex treatment, suggest that Dex treatment induces pulmonary fluid shifts, which may reduce lung edema and improve lung function.
The mechanisms by which antenatal glucocorticoids increase pulmonary DNA and protein synthesis are unclear. Glucocorticoids influence numerous physiologic and pathologic processes. Steroidal control of lung morphogenesis is mediated by regulating the effects of growth factors, cytokines, and their receptors(24–26). There is increasing evidence to suggest that growth factors play a crucial role in fetal lung development in a paracrine or autocrine fashion. Recently, we evaluated mRNA expression of various peptide growth factors in Dex-treated CDH lung in rats. Our results showed that IGF-I and IGF-II were decreased by antenatal Dex treatment, whereas basic fibroblast growth factor, platelet-derived growth factor, and transforming growth factor-β1 were increased(27, 28). These results lead us to speculate that a prenatal imbalance may exist between synthesis of various growth factors and cytokines in the lung, and that glucocorticoids may stimulate cellular DNA and protein synthesis by regulating these growth factors and cytokines, resulting in acceleration of lung development. Further studies are needed to evaluate the effect of antenatal glucocorticoids on other possible mediators that increase cellular DNA and protein synthesis, such as hormones, growth factors, and cytokines.
Abbreviations
- BrdU:
-
bromodeoxyuridine
- CDH:
-
congenital diaphragmatic hernia
- Dex:
-
dexamethasone
- LI:
-
labeling index
References
Puri P 1994 Congenital diaphragmatic hernia. Curr Prob Surg 10: 787–846.
Henneberg SW, Jepsen S, Anderson PK, Pederson SA 1995 Inhalation of nitric oxide as a treatment of pulmonary hypertension in congenital diaphragmatic hernia. J Pediatr Surg 30: 853–855.
Dommergues M, Luis-Sylvestre C, Mandelbrot L, Oury JF, Herlicoviez M, Body G, Gamerre M, Durnez Y 1996 Congenital diaphragmatic hernia: can prenatal ultrasonography predict outcome?. Am J Obstet Gynecol 174: 1377
Crowley P, Chalmers I, Keirse MJ 1990 The effects of corticosteroid administration before preterm delivery: an overview of the evidence from controlled trials. Br J Obstet Gynecol 97: 11–25.
Capsi E, Schreyer P, Weinraub Z, Rief R, Levi I, Mundel G 1976 Prevention of the respiratory distress syndrome in premature infants by antepartum glucocorticoid therapy. Br J Obstet Gynecol 83: 187–193.
Suen HC, Bloch KD, Donahoe PK 1994 Antenatal glucocorticoid corrects pulmonary immaturity in experimentally induced congenital diaphragmatic hernia in rats. Pediatr Res 35: 523–529.
Suen HC, Losty P, Donahoe PK, Schnitzer JJ 1994 Combined antenatal thyrotropin-releasing hormone and low-dose glucocorticoid therapy improves the pulmonary biochemical immaturity in congenital diaphragmatic hernia. J Pediatr Surg 29: 359–363.
Losty PD, Suen HC, Manganaro TF, Donahoe PK, Schnitzer JJ 1995 Prenatal hormonal therapy improves pulmonary compliance in the nitrofen-induced CDH rat model. J Pediatr Surg 30: 420–426.
Schnitzer JJ, Hedrick HL, Pscheco BA, Losty PD, Ryan DP, Doody DP, Donahoe PK 1996 Prenatal glucocorticoid therapy reverses pulmonary immaturity in congenital diaphragmatic hernia in fetal sheep. Ann Surg 224: 430–439.
Taira Y, Miyazaki E, Ohshiro K, Yamataka T, Puri P 1998 Administration of antenatal glucocorticoids prevents pulmonary artery structural changes in nitrofen-induced congenital diaphragmatic hernia in rats. J Pediatr Surg 33: 1052–1056.
Okoye BO, Losty PD, Lloyd DA, Gosney JR 1998 Effect of prenatal glucocorticoids on pulmonary vascular muscularization in nitrofen-induced congenital diaphragmatic hernia. J Pediatr Surg 33: 76–80.
Gratzner HG 1982 Monoclonal antibody to 5-bromo and 5-iododeoxyuridine. Science 218: 474–475.
Meyer JS, Nauert J, Koehmit S 1989 Cell kinetics of human tumors by in vitro bromodeoxyuridine labelling. J Histochem Cytochem 37: 1449–1454.
DiFlore JW, Fauza DO, Slavin R, Peters CA, Fackler JC, Wilson JM 1994 Experimental fetal tracheal ligation reverses the structural and physiological effects of pulmonary hypoplasia in congenital diaphragmatic hernia. J Pediatr Surg 29: 248–257.
Hedrick MH, Estes JM, Sullivan KM, Bealer JF, Kitterman JA, Flake AW, Adzick NS, Harrison MR 1994 Plug the lung until it grows (PLUG): a new method to treat congenital diaphragmatic hernia in utero. J Pediatr Surg 29: 612–617.
Nardo L, Hooper SB, Harling R 1995 Lung hypoplasia can be reversed by short-term obstruction of the trachea in fetal sheep. Pediatr Res 38: 690–696.
De Paepe ME, Johnson BD, Papadakis K, Sueishi K, Luks FI 1998 Temporal pattern of accelerated lung growth after tracheal occlusion in the fetal rabbit. Am J Pathol 152: 179–190.
Brody JS, Burki R, Kaplan N 1978 Deoxynucleic acid synthesis in lung cells during compensatory lung growth after pneumonectomy. Am Rev Respir Dis 117: 307–316.
Rannels DE, White DM, Watkins CA 1979 Rapidity of compensatory lung growth following pneumonectomy in adult rats. J Appl Physiol 46: 326–333.
Beck JC, Mitzner W, Johnson JWC 1981 Betamethasone and the rhesus fetus: effect on lung morphometry and connective tissue. Pediatr Res 15: 235–240.
Asabe K, Hashimoto S, Suita S, Sueishi K 1996 Maternal dexamethasone treatment enhances the expression of surfactant apoprotein A in the hypoplastic lung of rabbit fetuses induced by oligohydramnios. J Pediatr Surg 31: 1369–1375.
Ariagno RL, Sweeney TE, Northway WH 1986 Dexamethasone decreases lung water without affecting lung compliance in infant mice raised in 80 oxygen environment. Am Rev Respir Dis 133:A108( abstr)
Sahebjami H, Jacob G, Massaro D 1974 Influence of corticosteroid on recovery from oxygen toxicity. Am J Rev Respir Dis 110: 566–571.
Melik M, Choy HA, Jaskoll T 1996 Glucocorticoids, tumor necrosis factor-α, and epidermal growth factor regulation of pulmonary morphogenesis: a multivariate in vitro analysis of their related actions. Dev Dyn 205: 365–378.
Stewart AG, Fernandes D, Tomlinson PR 1995 The effect of glucocorticoids on proliferation of human cultured airway smooth muscle. Br J Pharmacol 116: 3219–3226.
Wang J, Kuliszewski M, Yec W, Sedlackova l, Xu J, Tesu J, Post M 1995 Cloning and expression of glucocrticoid-induced genes in fetal rat lung fibroblasts. J Biol Chem 270: 2722–2728.
Oue T, Taira Y, Shima H, Miyazaki E, Puri P 1998 Insulin-like growth factor I and II levels in hypoplastic lung in nitrofen induced diaphragmatic hernia in rats. Pediatr Surg Int 15: 175–179.
Oue T, Shima H, Taira Y, Puri P 2000 Antenatal glucocorticoids administration upregulates peptide growth factors gene expression in nitrofen induced congenital diaphragmatic hernia in rats. J Pediar Surg 35: 109–112.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Oue, T., Shima, H., Guarino, N. et al. Antenatal Dexamethasone Administration Increases Fetal Lung DNA Synthesis and RNA and Protein Content in Nitrofen-Induced Congenital Diaphragmatic Hernia in Rats. Pediatr Res 48, 789–793 (2000). https://doi.org/10.1203/00006450-200012000-00015
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200012000-00015