Abstract
Close attention to nutritional management is essential for optimizing growth and neurodevelopment of the preterm infant. Protein intake and the protein to energy ratio are the main determinants of growth and body composition. Yet large, multi-center, randomized controlled trials are lacking to guide protein delivery for the preterm infant. Until these studies are pursued, smaller trials must be used to inform clinical practice. This review summarizes the randomized controlled trials that have been performed to test the impact of higher vs. lower protein delivery to the preterm infant. We consider the trials that varied protein delivery rates during parenteral and enteral phases of nutrition. Considerable heterogeneity exists across study designs. Still, cumulative evidence from these trials provides a framework for current recommendations for protein intake in the preterm infant.
Similar content being viewed by others
Introduction
The preterm infant requires enough protein to promote the growth and remodeling of cells, tissues, and organs to accrue lean body mass. Protein intake is the limiting nutrient regarding growth [1], so providing an adequate supply of protein to the preterm infant is critical. Several observational studies have shown that protein intakes are positively correlated with improved growth, brain size, and neurodevelopmental outcome, highlighting the benefit of enhanced protein delivery to the preterm infant [2,3,4,5,6,7]. However, associations identified in cohort studies limit the ability to fully measure the strength and influence of severity of illness as a confounding factor. Preterm infants in those cohorts who were sicker may have received less protein or utilized protein less effectively. Thus, randomized controlled trials (RCTs) to define the optimal dose and delivery of protein are essential, especially those that are adequately powered to measure differences in neurodevelopmental outcomes.
The current goals of nutrition for the preterm infant are to supply enough amino acids to avoid a catabolic state and achieve positive nitrogen balance. Recommendations for protein delivery generally range from 2.5 to 4.5 g/kg per day, depending on the route of delivery (enteral vs. parenteral), gestational and postnatal age of the infant, adequacy of growth, and degree of cumulative protein deficit [8,9,10,11,12]. Several studies have demonstrated that parenteral amino acids initiated on the first day of life are tolerated from a metabolic standpoint, increase protein synthesis rates, and promote positive nitrogen balance [13,14,15,16]. It has been recommended to provide enough protein to the preterm infant to support continued high rates of protein accretion by mimicking placental delivery of amino acids, which is 3.5–4 g/kg per day in the late second trimester and early third trimester [17, 18]. While such reference values may represent the protein requirement for a fetus, those delivery rates may not translate into optimal intakes for the preterm infant born at the equivalent gestational age (GA) [19]. Commercial amino acid solutions for parenteral nutrition do not replicate the same balance of amino acids transferred by the placenta to the fetus [20], and the placenta assists in the clearance of protein degradation products from the fetus. The low birth weight preterm infant is often critically ill during the immediate postnatal period, resulting in alterations in metabolic demand, cytokines, and hormone profiles, all of which impact the utilization of nutrients [21]. Several studies and commentaries have called into question the safety of using doses of parenteral amino acids that exceed 3.5 g/kg per day, especially in the first 1–2 postnatal days or when preterm infants are critically ill [11, 19, 22,23,24]. Furthermore, there are differences in safety profiles and efficacy for promoting growth and neurodevelopment when protein is delivered parenterally vs. enterally, requiring route of protein delivery to be a critical consideration.
Unfortunately, there has been a dearth of large, multi-center, RCTs that also account for the wide range of metabolic stress and postnatal maturity in preterm infants to specifically guide protein delivery. Thus, care providers in the NICU are left with many unanswered questions about what dose of protein will safely support optimal growth. Therefore, the goal of this review is to summarize the smaller RCTs available that test the efficacy and safety of different doses of amino acids given parenterally, and protein given enterally, in the preterm infant.
Estimating protein requirements for preterm infants
Two methods have been used to estimate protein requirements in preterm infants. The first is the factorial approach which uses the chemical composition of the human fetus based on a constructed “reference fetus” [25]. Macronutrient requirements are calculated based on the sum of nutrients required to replace losses and those needed for accretion of tissue to meet average fetal weight gain per day [1] (Table 1). An alternate way to estimate macronutrient requirements is the empirical approach, which tests feedings with varying energy and protein content and uses growth and/or nitrogen balance as an outcome [26,27,28,29] (Table 2). Estimation of protein requirements using factorial and empirical approaches as well as systematic reviews of the literature have been used to inform guidelines published by international societies regarding protein delivery to preterm infants. Current guidelines for enteral protein delivery are shown in Table 3. Guidelines for parenteral amino acid delivery advise more generally for all preterm infants without specification by either birthweight, GA at birth, or chronological age. The European Society for Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) recommends that parenteral amino acids should be administered to the preterm infant immediately after birth with at least 1.5 g/kg per day and increase to 2.5 g/kg per day the next day. From day 2 onwards, parenteral amino acid intakes should be between 2.5 and 3.5 g/kg per day with at least 65 kcal/kg per day of energy [11]. The American Academy of Pediatrics Committee on Nutrition and the American Society of Parenteral and Enteral Nutrition (ASPEN) similarly recommend a maximal parenteral dose of 3–3.5 g/kg per day of protein [8, 10]. There is consistent guidance that amino acids should not be advanced beyond a maximum of 3.5 g/kg per day and that higher doses be provided on a research basis only [11].
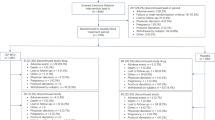
Randomized controlled trials evaluating the effect of parenteral amino acid intake on growth and neurodevelopmental outcome
There have been several small RCTs aimed to test the effects of different doses of parenteral amino acids on preterm infant growth and neurodevelopment (Table 4). Most trials compared a “higher” vs. a “lower” (or standard) dose of amino acids, with amino acid delivery rates in the higher groups that ranged from 3 to 4.5 g/kg per day vs. the lower groups that ranged from 2.5 to 3 g/kg per day. Several trials also varied the rapidity of advancement of amino acids, with the higher group starting either at the maximal dose within the first 24 hours of life or using a more rapid advancement to a maximum dose over 1–2 days compared to the lower group which used a stepwise increase over the first week of life. The mean GA among trials was approximately 27 weeks, with a range of 23–33 weeks. Some trials varied both parenteral and enteral protein delivery as well as carbohydrate and lipid delivery and even additional nutrients. The primary outcomes of most trials were growth and/or neurodevelopmental outcome and included biochemical measurements to track tolerance of higher amino acid doses. Results from each trial are briefly summarized in Table 4 and reviewed in more depth below. We report targeted amino acid delivery from each RCT; however, actual protein delivery did not always match targeted delivery and sometimes differed only minimally between groups.
Growth outcomes
Reported growth outcomes are variable as a result of higher vs. lower parenteral amino acid intake (Table 4). Several studies did not find differences in short term growth outcomes from increasing amino acid delivery in the first week of life [30,31,32,33,34,35,36]. In four of the trials that demonstrated greater growth when infants were randomized to higher parenteral amino acids, dextrose and/or lipid doses were also increased. For example, Can et al. randomized infants <34 weeks GA to receive a faster (3 g/kg per day amino acids advanced by 1 g/kg per day to 4 g/kg per day with a similar lipid advancement) vs. standard advancement of amino acids and lipid (1.5 g/kg per day amino acids advanced by 1 g/kg per day to 4 g/kg per day and slower lipid advancement) [37]. Length and occipital frontal head circumference (OFC) at 40 weeks postmenstrual age (PMA) were higher in the faster advancement group. Vlaardingerbroek et al. randomized infants <1500 g to one of three groups that included differences in amino acid and lipid delivery: higher (3.6 g/kg per day amino acids and 3 g/kg per day lipid), standard (2.4 g/kg per day amino acids and 3 g/kg per day lipid), or control (2.4 g/kg per day amino acids and 2.8 g/kg per day lipid) [38]. Amino acid dose was adjusted downward when blood urea nitrogen concentrations (BUN) exceeded 39 mg/dL, which occurred more frequently in the higher nutrient groups. Weight and OFC were greater at 6 weeks and weight was greater at 2 years in the higher amino acid group [39]. Morgan et al. randomized infants <29 weeks GA and <1200 g to receive enhanced (3.8 g/kg per day amino acids and lipid, 15.6 g/kg per day glucose) vs. standard parenteral nutrition (2.8 g/kg per day amino acids and lipid and 13.5 g/kg per day glucose) [40]. Enhanced nutrition resulted in larger OFC at both 28 days and 36 weeks corrected GA. Infants were not randomized until 120 h of life, so differences in amino acid delivery likely did not occur until later in the first week. Moltu et al. randomized infants <1500 g to receive higher (3.5 g/kg per day with multicomponent intravenous lipid containing fish oil and an enteral protein supplement with amino acids and vitamin A) vs. standard amino acids (2 g/kg per day increased to 3.5 g/kg per day using only enteral nutrition and a two-oil intravenous lipid without fish oil) [41]. The higher amino acid group had a lower proportion of infants discharged with a weight below the 10th%, though the study was stopped early due to higher septicemia in the intervention group. Scattolin et al., however, randomized infants <1250 g to receive higher (2 g/kg per day advanced by 1 g/kg per day to 4 g/kg per day) vs. standard amino acids (1.5 g/kg per day advanced by g/kg per day to 3 g/kg per day) without differences in other macronutrients or energy delivery [42]. The higher amino acid group had faster growth rates and higher weight and length at 36 weeks PMA.
Worse growth outcomes also have been reported in infants randomized to higher parenteral amino acid delivery, though in all these studies, the rate of advancing amino acids was also faster. Blanco et al. randomized infants with a birth weight <1000 g to receive early and high (2 g/kg per day advanced by 1 g/kg per day to 4 g/kg per day) vs. standard amino acids (0.5 g/kg per day advanced by 0.5 g/kg per day to 3 g/kg per day). There was no difference between groups for the primary outcome of hyperkalemia [43]. Secondary analyses demonstrated no differences between groups in weight, length and OFC z-scores at NICU discharge but lower growth z-scores at 6-, 12-, and 18-months corrected GA in the early and high amino acid group [44]. Uthaya et al. randomized infants <31 weeks GA in a multicenter RCT to receive immediate (3.6 g/kg per day from day 1) vs. incremental amino acids (1.7 g/kg per day and increased to 2.7 g/kg per day by day 3) in a 2 × 2 multifactorial study design with different lipid sources [45]. There was no difference in non-adipose mass measured by MRI at term corrected GA; however, infants in the immediate and higher amino acid group had smaller OFC at 40 weeks PMA. Balakrishnan et al. randomized infants <1250 g to receive rapid (3–4 g/kg per day advancing to 4 g/kg per day by day 1) vs. standard advancement of amino acids (1–2 g/kg per day advancing by 0.5 g/kg per day to 4 g/kg per day) [46]. Both groups reached equivalent amino acid delivery by day 7. After controlling for small for GA status, the more rapidly advanced group had smaller OFC at 36 weeks PMA and at NICU discharge.
Neurodevelopmental outcomes
Some of the RCTs that evaluated growth also evaluated neurodevelopmental outcomes at 2 years corrected GA and found no differences in those randomized to receive higher vs. lower parenteral amino acids [38, 39, 44, 46] (Table 4). Additionally, Burattini et al. randomized infants 500–1249 g to receive higher (2.5 g/kg per day advanced by 0.5 g/kg per day to 4 g/kg per day) vs. standard amino acids (1.5 g/kg per day advanced by 0.5 g/kg per day to 2.5 g/kg per day) and found no difference in neurodevelopmental outcome at 2 years [32]. Bellagamba et al. randomized infants 500–1249 g to receive higher (1.5 g/kg per day advanced 0.5 g/kg per day to 3.5 g/kg per day) vs. standard amino acids (1.5 g/kg per day advanced 0.5 g/kg per day to 2.5 g/kg per day) and found no difference in neurodevelopmental outcome [30]. Bloomfield et al. randomized infants <1000 g to receive a supplement of amino acids via an umbilical arterial catheter in addition to standard parenteral nutrition (total amino acid dose of 3.4 g/kg per day) vs. saline (total amino acid dose of 2.6 g/kg per day) beginning on the first day of life [47]. There were no differences in either growth or survival without disability at 2 years corrected GA between groups. Concerningly, however, moderate-to-severe neurodisability was more common in infants randomized to the higher amino acid group.
Biochemical differences and adverse outcomes
Plasma biochemical markers have been monitored as a measure of tolerance to parenteral amino acid dose. Amino acids in the circulation either enter energy-dependent protein synthetic pathways or are directly oxidized as an energy source through entry into the tricarboxylic acid cycle and ultimately the urea cycle for clearance of nitrogen [48, 49] (Fig. 1). Therefore, BUN is often used as a marker of amino acid utilization. While it was evaluated at different times during the intervention in each trial’s protocol, BUN was always higher in the higher vs. standard amino acid groups (Table 4). To monitor metabolic tolerance of higher amino acids, some studies monitored blood gas measurements and serum electrolytes, calcium, and phosphorus concentrations. Moltu et al. found a higher incidence of hypophosphatemia and hypokalemia in the higher amino acid and nutrient delivery group [50], and Bloomfield et al. found that more infants randomized to receive additional amino acids via an umbilical arterial catheter developed refeeding syndrome, including hypophosphatemia, hypercalcemia, and hypokalemia [47]. Some studies also monitored serum amino acid concentrations as a measure of protein sufficiency and/or toxicity and found either minimal differences [31] or elevated concentrations in the higher amino acid groups [33, 51, 52]. Clinical implications of higher amino acid concentrations could not be determined by these studies.
Randomized controlled trials evaluating the effect of enteral protein intake on growth and neurodevelopmental outcome
Several RCTs have compared higher vs. standard amounts of enteral protein on preterm infant growth and neurodevelopmental outcome (Table 5). Enteral protein delivery in the higher groups ranged from 3.2 to 4.8 g/kg per day vs. standard groups, which ranged from 2.9 to 4.1 g/kg per day. The average GA of subjects enrolled among studies was 29 weeks, ranging from 25 to 32 weeks. Different combinations of mother’s own milk, donor human milk, and preterm formulas were used in each of the studies. This is an important variable given the inter-individual variation in protein content in mother’s own milk and that protein is almost always lower in donor human milk because it is often donated by mothers of term infants later in lactation [53,54,55]. Some studies directly measured protein content using human milk analyzers [56,57,58], but most studies estimated milk protein content (estimates ranging between 1.1 and 1.7 g/100 mL). However, the proportions of milk type were comparable between groups within each individual study and included a majority of mother’s own milk. Likewise, type of human milk fortifier (HMF) varied across studies; some directly compared the same fortifier and varied the amount of protein, some compared two different formulations of fortifier (liquid vs. powder, intact vs. hydrolyzed protein, whey vs. casein), and others adjusted the protein within a fortifier based on BUN concentrations. All HMF used in the reported studies was bovine derived. Some studies varied other components of enteral nutrition such as lipid content. Results from each trial are briefly summarized in Table 5. Formulation of fortification that was used and actual protein delivered to each group are described in more depth below.
Growth outcomes
Two studies showed no difference in growth outcomes from higher enteral protein delivery [58, 59], no trials found a reduction in growth, and most found an improvement in growth (Table 5). Porcelli et al. randomized infants <1500 g to receive higher (1 g/100 mL whey HMF; 4.3 g/kg per day) vs. standard protein content (0.7 g/100 mL 60% whey and 40% casein HMF; 4.1 g/kg per day) for 21 days [60]. Greater weight gain velocity and greater achieved weight and OFC were observed in the higher protein group. Arslanoglu et al. randomized infants between 24 and 34 weeks GA to receive an adjustable regimen using supplemental protein based on BUN (0.8 g/100 ml hydrolyzed whey HMF and 0.3 g/100 mL whey supplemental protein; 3.2 g/kg per day) vs. standard protein (2.9 g/kg per day) until 2000 g [56]. Greater weight and OFC gains were observed in the adjustable group. Miller et al. randomized infants <31 weeks GA to receive higher (1.4 g/100 mL extensively hydrolyzed whey HMF; 4.2 g/kg per day) vs. standard protein (1 g/100 mL; 3.6 g/kg per day) for 4 weeks [57]. Achieved weight was greater and fewer infants were discharged <10th% for length in the higher protein group, though there was no difference in the rate of weight gain. Moya et al. randomized infants <1250 g to receive higher (1.8 g/100 mL hydrolyzed whey liquid HMF; 4.5 g/kg per day) vs. lower protein (1 g/100 mL hydrolyzed whey powdered HMF; 3.6 g/kg per day) for 28 days [61]. While there was no difference in weight gain, linear growth rate and achieved weight and length at the end of the study were higher in the higher protein group. Kim et al. randomized infants <33 weeks GA to receive higher (1.67 g/100 mL extensively hydrolyzed casein liquid HMF; 3.9 g/kg per day) vs. lower protein (1 g/100 mL intact whey powdered HMF; 3.3 g/kg per day) for 28 days [62]. There was no difference in rate of weight gain; but in a subgroup analysis of pre-defined strict protocol followers, those fed the higher protein fortifier achieved greater weight and linear growth. Rigo et al. randomized infants <32 weeks GA to receive higher (1.4 g/100 mL partially hydrolyzed whey HMF; 4.5 g/kg per day) vs. standard protein (1 g/100 mL extensively hydrolyzed whey; 3.8 g/kg per day) for 21 days [63]. Rate of weight gain and weight and OFC for age z-score were greater in the higher protein group, without a difference in linear growth. Finally, Salas et al. randomized infants 25-28 weeks GA to receive higher (1.67 g/100 mL extensively hydrolyzed casein liquid HMF and 0.75 g/100 mL extensively hydrolyzed casein liquid protein supplement; 3.9 g/kg per day) vs. standard protein (3.3 g/kg per day) until 32 weeks PMA [64]. Fat free mass and fat mass z-scores were higher at 36 weeks PMA and weight and length change in z-scores from birth to 3 months were higher in the high protein group.
Neurodevelopmental outcomes
We identified two RCTs that evaluated neurodevelopmental outcome from varying enteral protein delivery. Biastini et al. randomized infants <1250 g to receive higher (0.6 g/100 ml hydrolyzed powder HMF and 0.8 g/100 mL supplemental protein based on BUN; 4.8 g/kg per day) vs. standard protein (3.5 g/kg per day) for 28 days [65]. Infants receiving higher protein had higher hearing and language scores at 12 and 18 months and greater length gain at 9 months corrected GA. Dogra et al. randomized infants <1500 g to receive higher (1 g/100 mL extensively hydrolyzed whey HMF; 4.2 g/kg per day) vs. lower protein (0.4 g/100 mL whey HMF; 3.6 g/kg per day) [66]. There were no differences in growth or neurodevelopmental outcome at 12- and 18-months corrected GA, though OFC and weight gain were greater in higher protein group at 40 weeks PMA.
Biochemical differences and adverse outcomes
Minimal differences in biochemical markers were reported from higher enteral protein delivery, except for higher BUN and improved prealbumin concentrations (Table 5). No adverse events were reported.
Summary and interpretation of results
Parenteral amino acid intake
Outcomes related to growth and neurodevelopment from trials that have compared higher vs. lower parenteral amino acid intake in preterm infants are mixed. Some trials showed a benefit in growth outcomes from higher amino acid delivery, yet those studies either advanced to higher amino acid intake outside of the first few days of life or concurrently increased non-protein energy delivery. Some trials showed no difference between higher vs. lower amino acid dose on short-term growth outcomes or neurodevelopment. These conclusions are consistent with a Cochrane Review assessing trials that compared higher vs. lower intake of parenteral amino acids [67]. The conclusions were that higher amino acid intake in parenteral nutrition reduced the incidence of postnatal growth failure but did not affect mortality, with insufficient evidence to show an effect on neurodevelopmental outcome. Of particular concern, however, are the reports of smaller head circumference and worse neurodevelopmental outcomes when amino acid dose is at or above 3.5 g/kg per day beginning in the first 1–2 days of life. Given the current state of evidence from the literature, initiation of parenteral amino acids in the first day of life, with an increase in delivery rates that span the first 3–4 days of life to a maximum dose of 3.5 g/kg per day may be considered the safest and most efficacious approach for the preterm infant <1500 g and <32 weeks GA. Per ESPGHAN and ASPEN recommendations, parenteral amino acid intakes above 3.5 g/kg per day should only be administered as part of clinical trials [11, 24]. Close attention to amino acid delivery is warranted when administering starter TPN in the first day of life, or individually prepared TPN formulations thereafter, that contain a fixed percentage of amino acids. If higher fluid intakes are required, non-protein containing fluids may be administered to not exceed recommended amino acid delivery.
Enteral protein intake
Most trials demonstrated that in preterm infants, higher enteral protein intake ranging from 3.9 to 4.5 g/kg per day improved short-term growth. The lack of any adverse events or biochemical changes other than higher BUN reflect the gastrointestinal and metabolic tolerance of higher enteral protein delivery. Furthermore, several studies found an increase in prealbumin as a result of higher protein delivery, which is considered an indicator of growth in the neonate [68]. While improvements in weight gain were the predominant growth outcome, there were also beneficial effects on linear and head growth. Linear growth represents lean body mass and reflects organ growth and development, including the brain, and thus should be monitored, in addition to weight gain [69]. The current paucity of trials limits the ability to make conclusions about the effect of increased enteral protein delivery on neurodevelopmental outcome. Current recommendations for enteral protein delivery in preterm infants by major international societies range from 3.5 to 4.5 g/kg per day (Table 3). Based on our own experience, recent evidence [70,71,72], and ESPGHAN guidelines [9], we recommend enteral protein delivery at the higher end of that range (>4 g/kg per day, provided concomitant energy intakes are optimal) when there is evidence for cumulative protein deficit, administration of donor milk or unfortified mother’s own milk, and/or poor growth, especially poor linear growth (Table 6).
Considerations for why delivering high doses of amino acids parenterally is not as impactful on growth as delivering similar doses of enteral protein for the preterm infant
Review of the current RCTs highlights the potential risks of excessive administration of parenteral amino acids and reinforces the safety and benefit of using higher enteral protein intakes on growth. There are several reasons for why this may be the case. First, there is no storage site for free amino acids, which may raise the risk for toxicity from elevated concentrations of specific amino acids and/or a nitrogen load that cannot be adequately cleared by the urea cycle. However, the level at which higher amino acid, ammonia, or urea concentrations become harmful or toxic in the preterm infant is unknown. Second, there have been persistent concerns about suboptimal composition of amino acids in commercially available solutions for the preterm infant [19]. An imbalance in amino acid concentrations, with some amino acids in excess and others limiting, in the context of suboptimal ratios with nonprotein calories, may result in higher amino acid oxidation rather than enhanced protein synthesis. Third, delivering the ideal protein to energy ratio is less likely in the infant receiving parenteral nutrition; if hyperglycemia or hyperlipidemia develops, clinicians commonly restrict dextrose and lipid infusions yet do not alter amino acids accordingly [19, 20]. It is essential to maintain a total energy delivery of 30–40 kcal/g of protein to optimize the protein to energy ratio [19]. Finally, preterm infants randomized in parenteral amino acid trials were gestationally and postnatally younger when receiving higher doses compared to those infants in enteral protein trials. Nutritional provision in excess of metabolic capacity in the critically ill, more immature infant may contribute to their inability to use amino acids for protein accretion.
Limitations of currently available RCTs that test protein dose
When reviewing trials that have tested parenteral and enteral protein delivery, there are several limitations to consider. Most trials are small and enrolled patients from only one or two centers. Several different types of commercially available parenteral amino acid solutions were used among the studies. What defines an optimal parenteral amino acid formulation for preterm infants remains unknown, particularly for infants born at the lowest GA or when considering infants in the acute phase of illness. Similarly, trials that compared enteral protein delivery varied the type of protein (whey vs. casein), formulation of HMF (powder vs. liquid), degree of protein hydrolyzation (intact vs. partial vs. extensive), generation of the fortifier (older vs. newer HMF formulations), amount other macronutrients (lipid content, dextrose), whether diets were isocaloric, and the relative amounts of milk type (mother’s own milk vs. donor human milk vs. preterm formula). Only a few studies used human milk analysis to report the actual content of protein [56,57,58] and most studies estimated human milk protein content prior to addition of HMF, thereby limiting accuracy of determining actual protein delivery. These variables make it difficult to independently and strictly compare the amount of protein that was received and evaluate studies in a systematic way. Furthermore, the difference in amino acids or enteral protein that was received by the infants often was less than the difference that was intended by the study design. Very few preterm infants born <24 weeks of gestation were included in RCTs, yet these infants are at highest risk for postnatal growth failure and adverse neurodevelopment. It is important to note that neurodevelopmental outcomes were seldom the primary outcome of clinical trials and thus results are underpowered.
Conclusion
Close attention to nutritional delivery and protein intake is of utmost importance for the health of preterm infants to promote growth and neurodevelopment. Avoiding prolonged interruption of amino acids for very low birth weight infants prevents a catabolic state, reduces risk of hyperkalemia and hyperglycemia, and promotes positive nitrogen balance [20]. At the same time, caution is warranted when rapidly advancing amino acids to doses of >3.5 g/kg per day in the first 1–2 days of life. Given the preponderance of evidence for the safe and effective use of higher enteral protein doses, it may be prudent to increase protein delivery during the convalescent growth phase of a preterm infant when they are receiving full enteral feeds and are in a period of relative medical stability. However, it is still not known whether restoring a protein deficit is as effective for neurodevelopment as preventing it from happening in the first place. Expanded outcomes as a result of protein delivery to include body composition and lean mass growth [2], adequately powered school age neurodevelopmental outcome assessments, and later life incidence of metabolic disease are critically needed, as are more sophisticated and predictive biomarkers to monitor protein tolerance and effectiveness. Finally, many questions remain about the ceiling for safe and effective amino acid administration for the more complex preterm infant who is born prior to 24 weeks of gestation, or affected by intrauterine growth restriction, or who develops critical illness so that the approach to protein delivery may be personalized to the individual patient.
References
Ziegler EE. Meeting the nutritional needs of the low-birth-weight infant. Ann Nutr Metab. 2011;58:8–18.
Bell KA, Matthews LG, Cherkerzian S, Palmer C, Drouin K, Pepin HL, et al. Associations of growth and body composition with brain size in preterm infants. J Pediatr. 2019;214:20–6.e2.
Bell KA, Matthews LG, Cherkerzian S, Prohl AK, Warfield SK, Inder TE, et al. Associations of body composition with regional brain volumes and white matter microstructure in very preterm infants. Arch Dis Child Fetal Neonatal Ed. 2022;107:533–8.
Coviello C, Keunen K, Kersbergen KJ, Groenendaal F, Leemans A, Peels B, et al. Effects of early nutrition and growth on brain volumes, white matter microstructure, and neurodevelopmental outcome in preterm newborns. Pediatr Res. 2018;83:102–10.
Poindexter BB, Langer JC, Dusick AM, Ehrenkranz RA, National Institute of Child H, Human Development Neonatal Research N. Early provision of parenteral amino acids in extremely low birth weight infants: relation to growth and neurodevelopmental outcome. J Pediatr. 2006;148:300–5.
Stephens BE, Walden RV, Gargus RA, Tucker R, McKinley L, Mance M, et al. First-week protein and energy intakes are associated with 18-month developmental outcomes in extremely low birth weight infants. Pediatrics. 2009;123:1337–43.
Yang J, Chang SS, Poon WB. Relationship between amino acid and energy intake and long-term growth and neurodevelopmental outcomes in very low birth weight infants. J Parenter Enter Nutr. 2016;40:820–6.
American Academy of Pediatrics Committee on Nutrition. Nutritional needs of low-birth-weight infants. Pediatrics 1985;75:976–86.
Embleton ND, Moltu SJ, Lapillonne A, van den Akker CHP, Carnielli V, Fusch C, et al. Enteral nutrition in preterm infants (2022): a position paper from the ESPGHAN committee on nutrition and invited experts. J Pediatr Gastroenterol Nutr. 2023;76:248–68.
Robinson DT, Calkins KL, Chen Y, Cober MP, Falciglia GH, Church DD, et al. Guidelines for parenteral nutrition in preterm infants: the American Society for parenteral and enteral nutrition. J Parenter Enter Nutr. 2023;47:830–58.
van Goudoever JB, Carnielli V, Darmaun D, Sainz de Pipaon M. ESPGHAN/ESPEN/ESPR/CSPEN guidelines on pediatric parenteral nutrition: amino acids. Clin Nutr. 2018;37:2315–23.
Ziegler EE. Protein requirements of very low birth weight infants. J Pediatr Gastroenterol Nutr. 2007;45:S170–S4.
Ibrahim HM, Jeroudi MA, Baier RJ, Dhanireddy R, Krouskop RW. Aggressive early total parental nutrition in low-birth-weight infants. J Perinatol. 2004;24:482–6.
te Braake FW, van den Akker CH, Wattimena DJ, Huijmans JG, van Goudoever JB. Amino acid administration to premature infants directly after birth. J Pediatr. 2005;147:457–61.
Thureen PJ, Melara D, Fennessey PV, Hay WW. Effect of low versus high intravenous amino acid intake on very low birth weight infants in the early neonatal period. Pediatr Res. 2003;53:24–32.
van den Akker CH, te Braake FW, Wattimena DJ, Voortman G, Schierbeek H, Vermes A, et al. Effects of early amino acid administration on leucine and glucose kinetics in premature infants. Pediatr Res. 2006;59:732–5.
Kennaugh JM, Bell AW, Teng C, Meschia G, Battaglia FC. Ontogenetic changes in the rates of protein synthesis and leucine oxidation during fetal life. Pediatr Res. 1987;22:688–92.
Lemons JA, Adcock EW 3rd, Jones MD Jr, Naughton MA, Meschia G, Battaglia FC. Umbilical uptake of amino acids in the unstressed fetal lamb. J Clin Investig. 1976;58:1428–34.
Embleton ND, van den Akker CHP. Protein intakes to optimize outcomes for preterm infants. Semin Perinatol. 2019;43:151154.
Morgan C. Early amino acid administration in very preterm infants: Too little, too late or too much, too soon? Semin Fetal Neonatal Med. 2013;18:160–5.
Ramel SE, Brown LD, Georgieff MK. The impact of neonatal illness on nutritional requirements-one size does not fit all. Curr Pediatr Rep. 2014;2:248–54.
Embleton ND, Van Den Akker CH. Early parenteral amino acid intakes in preterm babies: does NEON light the way? Arch Dis Child Fetal Neonatal Ed. 2018;103:F92–4.
Martin CR. Parenteral protein in extremely preterm infants - more is not better. N. Engl J Med. 2022;387:1712–3.
Robinson DT, Taylor SN, Moya F. Preterm infant nutrition: considerations for infants at risk of refeeding syndrome. J Perinatol. 2023;43:120–3.
Ziegler EE, O’Donnell AM, Nelson SE, Fomon SJ. Body composition of the reference fetus. Growth 1976;40:329–41.
Kashyap S, Forsyth M, Zucker C, Ramakrishnan R, Dell RB, Heird WC. Effects of varying protein and energy intakes on growth and metabolic response in low birth weight infants. J Pediatr. 1986;108:955–63.
Kashyap S, Schulze KF, Forsyth M, Zucker C, Dell RB, Ramakrishnan R, et al. Growth, nutrient retention, and metabolic response in low birth weight infants fed varying intakes of protein and energy. J Pediatr. 1988;113:713–21.
Rigo J. Protein, amino acid and other nitrogen compounds. In: Tsang RC, Uauy R, Koletzko B, Zlotkin S, editors. Nutrition of the Preterm Infant. Cincinnati, OH: Digital Educational Publishing; 2005. p. 45–80.
Ziegler EE Protein requirements of preterm infants. In: Fomon SJ, Heird WC, editors. Energy and Protein Needs During Infancy. New York: Academic Press; 1986. p. 69-85.
Bellagamba MP, Carmenati E, D’Ascenzo R, Malatesta M, Spagnoli C, Biagetti C, et al. One extra gram of protein to preterm infants from birth to 1800 g: a single-blinded randomized clinical trial. J Pediatr Gastroenterol Nutr. 2016;62:879–84.
Bulbul A, Okan F, Bulbul L, Nuhoglu A. Effect of low versus high early parenteral nutrition on plasma amino acid profiles in very low birth-weight infants. J Matern Fetal Neonatal Med. 2012;25:770–6.
Burattini I, Bellagamba MP, Spagnoli C, D’Ascenzo R, Mazzoni N, Peretti A, et al. Targeting 2.5 versus 4 g/kg/day of amino acids for extremely low birth weight infants: a randomized clinical trial. J Pediatr. 2013;163:1278-82.e1.
Clark RH, Chace DH, Spitzer AR. Effects of two different doses of amino acid supplementation on growth and blood amino acid levels in premature neonates admitted to the neonatal intensive care unit: a randomized, controlled trial. Pediatrics. 2007;120:1286–96.
Li Y, Sun Z, Hu Y, Li B, Bu X, Luo Y, et al. Early administration of amino acids with different doses in low birth weight premature infants. J Res Med Sci. 2020;25:49.
Tan MJ, Cooke RW. Improving head growth in very preterm infants-a randomised controlled trial I: neonatal outcomes. Arch Dis Child Fetal Neonatal Ed. 2008;93:F337–41.
Tan M, Abernethy L, Cooke R. Improving head growth in preterm infants-a randomised controlled trial II: MRI and developmental outcomes in the first year. Arch Dis Child Fetal Neonatal Ed. 2008;93:F342–6.
Can E, Bulbul A, Uslu S, Comert S, Bolat F, Nuhoglu A. Effects of aggressive parenteral nutrition on growth and clinical outcome in preterm infants. Pediatr Int. 2012;54:869–74.
Vlaardingerbroek H, Vermeulen MJ, Rook D, van den Akker CH, Dorst K, Wattimena JL, et al. Safety and efficacy of early parenteral lipid and high-dose amino acid administration to very low birth weight infants. J Pediatr. 2013;163:638–44.e1-5.
Roelants JA, Vlaardingerbroek H, van den Akker CHP, de Jonge RCJ, van Goudoever JB, Vermeulen MJ. Two-Year Follow-up of a randomized controlled nutrition intervention trial in very low-birth-weight infants. J Parenter Enter Nutr. 2018;42:122–31.
Morgan C, McGowan P, Herwitker S, Hart AE, Turner MA. Postnatal head growth in preterm infants: a randomized controlled parenteral nutrition study. Pediatrics. 2014;133:e120–8.
Moltu SJ, Blakstad EW, Strømmen K, Almaas AN, Nakstad B, Rønnestad A, et al. Enhanced feeding and diminished postnatal growth failure in very-low-birth-weight infants. J Pediatr Gastroenterol Nutr. 2014;58:344–51.
Scattolin S, Gaio P, Betto M, Palatron S, De Terlizzi F, Intini F, et al. Parenteral amino acid intakes: possible influences of higher intakes on growth and bone status in preterm infants. J Perinatol. 2013;33:33–9.
Blanco CL, Falck A, Green BK, Cornell JE, Gong AK. Metabolic responses to early and high protein supplementation in a randomized trial evaluating the prevention of hyperkalemia in extremely low birth weight infants. J Pediatr. 2008;153:535–40.
Blanco CL, Gong AK, Schoolfield J, Green BK, Daniels W, Liechty EA, et al. Impact of early and high amino acid supplementation on ELBW infants at 2 years. J Pediatr Gastroenterol Nutr. 2012;54:601–7.
Uthaya S, Liu X, Babalis D, Doré CJ, Warwick J, Bell J, et al. Nutritional evaluation and optimisation in neonates: a randomized, double-blind controlled trial of amino acid regimen and intravenous lipid composition in preterm parenteral nutrition. Am J Clin Nutr. 2016;103:1443–52.
Balakrishnan M, Jennings A, Przystac L, Phornphutkul C, Tucker R, Vohr B, et al. Growth and neurodevelopmental outcomes of early, high-dose parenteral amino acid intake in very low birth weight infants: a randomized controlled trial. J Parenter Enter Nutr. 2018;42:597–606.
Bloomfield FH, Jiang Y, Harding JE, Crowther CA, Cormack BE. Early amino acids in extremely preterm infants and neurodisability at 2 Years. N Engl J Med. 2022;387:1661–72.
Brosnan JT, Brosnan ME. Branched-chain amino acids: enzyme and substrate regulation. J Nutr. 2006;136:207S–11S.
Liechty EA, Barone S, Nutt M. Effect of maternal fasting on ovine fetal and maternal branched-chain amino acid transaminase activities. Biol Neonate. 1987;52:166–73.
Moltu SJ, Strømmen K, Blakstad EW, Almaas AN, Westerberg AC, Brække K, et al. Enhanced feeding in very-low-birth-weight infants may cause electrolyte disturbances and septicemia-a randomized, controlled trial. Clin Nutr. 2013;32:207–12.
Strommen K, Haag A, Moltu SJ, Veierod MB, Blakstad EW, Nakstad B, et al. Enhanced nutrient supply to very low birth weight infants is associated with higher blood amino acid concentrations and improved growth. Clin Nutr ESPEN. 2017;18:16–22.
Blanco CL, Gong AK, Green BK, Falck A, Schoolfield J, Liechty EA. Early changes in plasma amino acid concentrations during aggressive nutritional therapy in extremely low birth weight infants. J Pediatr. 2011;158:543–8.e1.
Arnold M, Adamkin D, Radmacher P. Improving fortification with weekly analysis of human milk for VLBW infants. J Perinatol. 2017;37:194–6.
de Halleux V, Rigo J. Variability in human milk composition: benefit of individualized fortification in very-low-birth-weight infants. Am J Clin Nutr. 2013;98:529s–35s.
Radmacher PG, Lewis SL, Adamkin DH. Individualizing fortification of human milk using real time human milk analysis. J Neonatal Perinat Med. 2013;6:319–23.
Arslanoglu S, Moro GE, Ziegler EE. Adjustable fortification of human milk fed to preterm infants: does it make a difference? J Perinatol. 2006;26:614–21.
Miller J, Makrides M, Gibson RA, McPhee AJ, Stanford TE, Morris S, et al. Effect of increasing protein content of human milk fortifier on growth in preterm infants born at <31 wk gestation: a randomized controlled trial. Am J Clin Nutr. 2012;95:648–55.
Reid J, Makrides M, McPhee AJ, Stark MJ, Miller J, Collins CT. The effect of increasing the protein content of human milk fortifier to 1.8 g/100 mL on growth in preterm infants: a randomised controlled trial. Nutrients. 2018;10:634.
Maas C, Mathes M, Bleeker C, Vek J, Bernhard W, Wiechers C, et al. Effect of increased enteral protein intake on growth in human milk-fed preterm infants: a randomized clinical trial. JAMA Pediatr. 2017;171:16–22.
Porcelli P, Schanler R, Greer F, Chan G, Gross S, Mehta N, et al. Growth in human milk-Fed very low birth weight infants receiving a new human milk fortifier. Ann Nutr Metab. 2000;44:2–10.
Moya F, Sisk PM, Walsh KR, Berseth CL. A new liquid human milk fortifier and linear growth in preterm infants. Pediatrics. 2012;130:e928–e35.
Kim JH, Chan G, Schanler R, Groh-Wargo S, Bloom B, Dimmit R, et al. Growth and tolerance of preterm infants fed a new extensively hydrolyzed liquid human milk fortifier. J Pediatr Gastroenterol Nutr. 2015;61:665–71.
Rigo J, Hascoët JM, Billeaud C, Picaud JC, Mosca F, Rubio A, et al. Growth and nutritional biomarkers of preterm infants fed a new powdered human milk fortifier: a randomized trial. J Pediatr Gastroenterol Nutr. 2017;65:e83–e93.
Salas AA, Jerome M, Finck A, Razzaghy J, Chandler-Laney P, Carlo WA. Body composition of extremely preterm infants fed protein-enriched, fortified milk: a randomized trial. Pediatr Res. 2022;91:1231–7.
Biasini A, Monti F, Laguardia MC, Stella M, Marvulli L, Neri E. High protein intake in human/maternal milk fortification for ≤1250 gr infants: intrahospital growth and neurodevelopmental outcome at two years. Acta Biomed. 2018;88:470–6.
Dogra S, Thakur A, Garg P, Kler N. Effect of differential enteral protein on growth and neurodevelopment in infants <1500 g: a randomized controlled trial. J Pediatr Gastroenterol Nutr. 2017;64:e126–e32.
Osborn DA, Schindler T, Jones LJ, Sinn JK, Bolisetty S. Higher versus lower amino acid intake in parenteral nutrition for newborn infants. Cochrane database Syst Rev. 2018;3:Cd005949.
Kim DH, Lee NM, Kim SY, Yi DY, Yun SW, Chae SA, et al. Effectiveness of prealbumin as an indicator of growth in neonates. Medicine. 2021;100:e27603.
Pfister KM, Ramel SE. Linear growth and neurodevelopmental outcomes. Clin Perinatol. 2014;41:309–21.
Belfort M, Cherkerzian S, Bell K, Soldateli B, Cordova Ramos E, Palmer C, et al. Macronutrient intake from human milk, infant growth, and body composition at term equivalent age: a longitudinal study of hospitalized very preterm infants. Nutrients. 2020;12:2249.
Khaira S, Pert A, Farrell E, Sibley C, Harvey-Wilkes K, Nielsen HC, et al. Expressed breast milk analysis: role of individualized protein fortification to avoid protein deficit after preterm birth and improve infant outcomes. Front Pediatr. 2021;9:652038.
Miller M, Vaidya R, Rastogi D, Bhutada A, Rastogi S. From parenteral to enteral nutrition: a nutrition-based approach for evaluating postnatal growth failure in preterm infants. J Parenter Enter Nutr. 2014;38:489–97.
Acknowledgements
We would like to acknowledge Kendra Hendrickson, MS, RD, CNSC, CSP and Susan Marshall, MS, RD, CSPCC, CNSC for their nutritional expertise during preparation of this manuscript.
Funding
The Ludeman Family Center for Women’s Health Research, University of Colorado Anschutz Medical Campus (LDB). The content of this manuscript does not represent the official views of the funding organizations.
Author information
Authors and Affiliations
Contributions
LDB, DTR and JS performed the literature review; LDB drafted the manuscript; LDB, DTR and JS edited the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brown, L.D., Stremming, J. & Robinson, D.T. Targeting optimal protein delivery in parenteral and enteral nutrition for preterm infants: a review of randomized, controlled trials. J Perinatol 44, 603–611 (2024). https://doi.org/10.1038/s41372-023-01847-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-023-01847-6