Abstract
Patients with HBeAg-negative chronic hepatitis B may experience an immune response after stopping nucleos(t)ide analogue (NA)therapy, which may potentially trigger HBsAg loss or off-therapy sustained viral control. The immunological mechanisms determining clinical response remain poorly understood. To identify inflammatory signatures associated with defined outcomes, we analysed plasma cytokines and chemokines from 57 HBeAg-negative patients enrolled in the Nuc-Stop Study at baseline and 12 weeks after NA cessation. Clinical response at 12 weeks was classified into four groups: immune control, viral relapse, evolving clinical relapse, and resolving clinical relapse. Twelve weeks after treatment cessation 17 patients (30%) experienced immune control, 19 (33%) viral relapse, 6 (11%) evolving clinical relapse, and 15 (26%) resolving clinical relapse. There was a significant increase in interferon-γ-induced protein 10 (IP-10; p = 0.012) and tumor necrosis factor (TNF; p = 0.032) in patients with evolving clinical relapse. Sparse partial least-squares multivariate analyses (sPLS-DA) showed higher first component values for the clinical relapse group compared to the other groups, separation was driven mainly by IP-10, TNF, IL-9, IFN-γ, MIP-1β, and IL-12. Our results demonstrate that evolving clinical relapse after NA cessation is associated with a systemic increase in the proinflammatory cytokines IP-10 and TNF.
Clinical trial registration: ClinicalTrials.gov, Identifier: NCT03681132.
Similar content being viewed by others
Introduction
In 2016, the World Health Organization (WHO) launched a goal to eliminate viral hepatitis as a major public health threat by 20301. Hepatitis B virus (HBV) infection is one of the leading causes of cirrhosis and hepatocellular carcinoma worldwide and is estimated to cause between 555,000 and 865,000 deaths per year2,3,4. There is no definite cure and suppressive nucleos(t)ide analogue (NA) therapy is the mainstay of treatment. Functional cure, defined as hepatitis B surface antigen (HBsAg) loss, is the ultimate treatment goal but is rarely achieved in patients on NA treatment, with an annual incidence of 0.15–0.33% in chronic hepatitis B (CHB) patients5,6,7,8. Treatment duration is therefore indefinite and potentially lifelong.
A decade ago, Hadziyannis et al. observed that 39% of patients lost HBsAg following NA therapy cessation in hepatitis B e antigen (HBeAg)-negative CHB patients. Since then, several studies have looked into whether stopping NA therapy can initiate an immune response that may trigger HBsAg loss5,9,10,11,12,13,14,15,16; however, the proportion who achieve this endpoint has been lower than what was reported in Hadziyannis’ study5,7,11,15,17. Identifying patients more likely to reach HBsAg loss is essential to avoid futile treatment stops. Furthermore, identifying patients who may experience detrimental outcomes of treatment cessation is crucial for patient safety.
The immune system plays a complex role in the course of HBV infection and gaining better knowledge of the immune mechanisms involved in the different phases of HBV infection is a vital step toward a treatment strategy to achieve functional cure. As signalling molecules of the immune system, cytokines have a fundamental role in both mediating and regulating the immune response. Rebound after treatment cessation in HBeAg-negative CHB has been reported to be associated with an increase in IFN-γ-induced protein 10 (IP-10), tumor necrosis factor (TNF), interleukin (IL)-10, and IL-1214. Cytokines and chemokines may have an unexploited potential as prediction biomarkers or therapeutic targets in CHB18. To attempt to identify the immunological mechanisms that determine clinical response and clinical relapse after treatment cessation, we analysed selected cytokines and chemokines at baseline and 12 weeks after treatment cessation in patients with HBeAg-negative CHB who participated in the Nuc-Stop Study19.
Materials and methods
Study design and participants
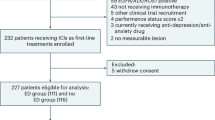
This was a sub-study of 57 CHB patients enrolled in the Nuc-Stop Study, a multicentre randomized trial where patients with HBeAg-negative CHB stopped NA therapy and were followed up for three years19. Inclusion took place between 2018 and 2020 from three centres in Norway: 26 from Oslo University Hospital, 25 from Akershus University Hospital, and 6 from Vestfold Hospital. All patients were non-cirrhotic and virally suppressed with tenofovir (including both tenofovir disoproxil fumarate and tenofovir alafenamide) or entecavir for at least 24 months prior to stopping NA therapy. None of the patients had coinfection with HIV, hepatitis C or hepatitis D, other active liver disease, previous hepatocellular carcinoma, or a history of decompensated liver disease. Patients with alcohol consumption of more than 14 (women) or 21 (men) standard units of alcohol per week during the past six months were excluded.
All study participants stopped NA therapy at inclusion and were followed up 4, 8, and 12 weeks after treatment cessation, and then 3-monthly until end-of-study. All study visits consisted of clinical evaluation and blood collection for analyses of HBV DNA and liver enzymes. In addition, serum and plasma at baseline and 12 weeks were stored at − 80 °C in a research biobank for later analyses. For the current analyses, plasma samples collected at baseline (the day of treatment withdrawal) and after 12 weeks were analysed.
Multiplex cytokine assay
Plasma cytokines and chemokines were analysed on a Luminex IS 200 with the Bio-Plex Pro Human Cytokine 27-plex Assay (Cat. no.: M500KCAF0Y, Bio-Rad Laboratories Inc., Hercules, USA). The plasma samples were thawed and kept on ice, gently vortexed, and spun down at 10,000 g for 10 min at 4 °C. The supernatant of each sample was further diluted (1:4), and 50 µl was loaded into each well. Plasma from each individual donor was analysed on the same assay plate in duplicate. Internal kit controls were included to determine the intra- and inter-coefficient of variation expressed as a percentage (% CV). The plasma concentration of the following cytokines and chemokines was determined: IL-1β, IL-1 receptor agonist (RA), IL-2, IL-4, IL-5, IL-6, IL-7, IL-8, IL-9, IL-10, IL-12p70, IL-13, IL-15, IL-17, eotaxin, basic fibroblast growth factor (FGF), granulocyte-colony-stimulating factor (G-CSF), granulocyte–macrophage colony stimulating factor (GM-CSF), interferon (IFN)-γ, IP-10, monocyte chemoattractant protein (MCP)-1, macrophage-inflammatory protein (MIP)-1α, MIP-1β, platelet-derived growth factor (PDGF)-BB, regulated upon activation, normally T-expressed, and presumably secreted (RANTES), vascular endothelial growth factor (VEGF), and TNF. Any cytokine that was undetectable by the Luminex assay in more than 50% of the participants at either time point was excluded from subsequent statistical analyses. Consequently, IL-5, IL-10, IL-15, MIP-1α, and VEGF were omitted from further investigation.
Definition of clinical response at 12 weeks
When analysing the change in cytokine concentrations from baseline to 12 weeks (delta value between baseline and 12 weeks), clinical response at 12 weeks was classified as follows:
-
Immune control (HBV DNA ≤ 2000 IU/ml and alanine aminotransferase (ALT) ≤ 80 U/L)
-
Viral relapse (HBV DNA > 2000 IU/ml and ALT ≤ 80 U/L)
-
Evolving clinical relapse (HBV DNA > 2000 IU/ml, ALT > 80 U/L and increasing from week 8 to 12)
-
Resolving clinical relapse (HBV DNA > 2000 IU/ml, ALT > 80 U/L and decreasing from week 8 to 12)
The rationale for choosing the above levels of differentiation for ALT and HBV DNA was based on the European Association for the Study of the Liver clinical practice guidelines20. ALT > 2 × ULN corresponds to ALT > 80 U/L.
Clinical relapse was divided into evolving clinical relapse and resolving clinical relapse based on whether ALT was increasing or decreasing from week eight to week twelve (Fig. 1). This was done to better capture the differences in immunological and inflammatory dynamics between a progressing flare and a subsiding flare.
Evolving clinical relapse and resolving clinical relapse were merged into one group (“clinical relapse”) for the analysis of the baseline concentrations of the cytokines, since the timing of relapse was then irrelevant.
Statistical analyses
Comparisons between three or four groups of continuous variables were performed by Kruskal–Wallis test, followed by Bonferroni post hoc tests. Categorical variables were compared using Fisher´s exact test. In addition, a multivariate supervised sparse Partial Least Square Discriminant Analysis (sPLS-DA) was used to investigate differences in cytokine profiles at baseline and differences in change in cytokines from baseline to 12 weeks. Correlations between two continuous variables were analysed using Spearman´s test. To examine the predictive value of baseline variables, a receiver operating characteristic (ROC) analysis was performed. The area under the ROC curve (AUC), sensitivity, specificity, and predictive values were calculated. Statistical analyses were performed using IBM SPSS Statistics version 28 (SPSS Inc., Chicago, IL, USA) and STATA SE 17 (StataCorp, College Station, TX, USA). sPLS-DA was executed using mixOmics R package version 6.24.021. P-values less than 0.05 were considered statistically significant.
Ethical consideration
This study was conducted in compliance with the Declaration of Helsinki and International Conference on Harmonisation/Good Clinical Practice. The Regional Committees for Medical and Health Research Ethics (REK No. 2018/998) and the Norwegian Medicines Agency (EudraCTnr. 2018-000724-34) approved the protocol. The Nuc-Stop Study was registered at ClinicalTrials.gov (Identifier: NCT03681132). All patients signed informed consent to participate in the study.
Ethics approval statement
This study was conducted in compliance with the Declaration of Helsinki and International Conference on Harmonisation/Good Clinical Practice. The Regional Committees for Medical and Health Research Ethics (REK No. 2018/998) and the Norwegian Medicines Agency (EudraCTnr. 2018-000724-34) approved the protocol.
Patient consent statement
All patients signed informed consent to participate in the Nuc-Stop Study.
Results
Clinical characteristics of the study population
The baseline characteristics of the 57 study participants are shown in Table 1. The median age was 45 (interquartile range 40–52) years, and 72% were men. All the most common HBV genotypes were represented, and genotypes, age, sex, and ethnic background were evenly distributed among the four clinical response groups. All patients were treated with potent NAs with a high barrier to resistance at enrolment, with tenofovir as the most common treatment (74%).
More patients in the immune control group had stopped entecavir treatment whereas more patients in the viral relapse, evolving clinical relapse, and resolving clinical relapse groups had stopped tenofovir treatment (p < 0.01, Fisher’s exact test). There was also a difference in duration of antiviral treatment where patients in the evolving and resolving clinical relapse groups had a longer treatment duration before treatment cessation (p = 0.042, Kruskal–Wallis test).
By definition, the patients with clinical relapse, both evolving and resolving, had a higher peak ALT and HBV DNA than the other groups (Fig. 2). One of six patients in the evolving clinical relapse group and eight of 16 patients in the resolving clinical relapse group re-started treatment in week eight since they met the predefined safety criteria in the Nuc-Stop Study (ALT > 800 U/L)19.
Dynamic changes in ALT and HBV DNA the initial 12 weeks after NA therapy cessation, by clinical response at 12 weeks. (a) Median ALT at baseline, 4 weeks, 8 weeks, and 12 weeks. (b) Median log10 HBV DNA at baseline, 4 weeks, 8 weeks, and 12 weeks. Error bars represent the interquartile ranges. HBV hepatitis B virus, ALT alanine aminotransferase.
Changes in cytokines from baseline to 12 weeks
The change in cytokine concentrations from baseline to 12 weeks was calculated, and the four clinical response groups: immune control, viral relapse, evolving clinical relapse, and resolving clinical relapse, were compared. There was a significant difference in change in IP-10 between the four groups (p = 0.012, Kruskal–Wallis test) (Fig. 3). Patients with evolving clinical relapse had a significantly greater increase in IP-10 compared with the immune control group (p = 0.007, Bonferroni post-hoc test) but not compared with the other groups. There was a weak correlation between peak ALT and change in IP-10 (Spearman r = 0.34, p = 0.01) (Fig. 4a). The correlation between peak ALT and absolute IP-10 at 12 weeks was stronger (Spearman r = 0.41, p < 0.01) (Fig. 4b).
Changes in IP-10 and TNF plasma levels 12 weeks after NA therapy cessation. Shown are the differences in change (delta value between baseline and 12 weeks) in IP-10 (a) and TNF (b) from baseline to 12 weeks in the different response groups at 12 weeks. The boxes represent the interquartile ranges (IQR), and the middle lines represent the medians. IP-10 interferon-γ-induced protein 10, TNF tumor necrosis factor.
Scatter diagrams of peak ALT and change in IP-10 and absolute IP-10 at 12 weeks, and peak ALT and change in TNF and absolute TNF at 12 weeks. (a) Correlation between peak ALT and change in IP-10. (b) Correlation between peak ALT and absolute IP-10 at 12 weeks. (c) Correlation between peak ALT and change in TNF. (d) Correlation between peak ALT and absolute TNF at 12 weeks. The values for Spearman’s correlation coefficient are given. Peak ALT is the highest ALT value measured during the first 12 weeks after NA therapy cessation. Change in IP-10 and TNF are the delta values for IP-10 and TNF between baseline and 12 weeks. Absolute IP-10 and TNF are the values for IP-10 and TNF measured at 12 weeks after NA therapy cessation. ALT alanine aminotransferase, IP-10 interferon-γ-induced protein 10, TNF tumor necrosis factor.
Between the four groups, there was also a significant difference in change of TNF from baseline to 12 weeks (p = 0.032, Kruskal–Wallis test) (Fig. 3) with a significantly greater increase in evolving clinical relapse compared with the immune control (p = 0.036, Bonferroni post-hoc test) and viral relapse (p = 0.031, Bonferroni post-hoc test) groups. Peak ALT did not correlate with change in TNF (Spearman r = 0.23, p = 0.09) (Fig. 4c). Likewise, there was no correlation between peak ALT and absolute TNF at 12 weeks (Spearman r = -0.06, p = 0.66) (Fig. 4d).
There were no significant differences between the four clinical response groups for changes in any of the other 20 cytokines.
When looking at the change in cytokines from baseline to 12 weeks using sPLS-DA, the evolving clinical relapse group had higher first component values than the immune control, viral relapse, and resolving clinical relapse groups. This separation was driven mainly by IP-10, TNF, IL-9, IFN-γ, MIP-1β, and IL-12 (Fig. 5b).
Sparse partial least square discriminant analysis (sPLS-DA) of baseline cytokines and changes in cytokines 12 weeks after NA therapy cessation. (a) Two-dimensional sPLS-DA of baseline cytokines in the immune control, viral relapse, and clinical relapse groups. (b) Two-dimensional sPLS-DA of changes in plasma levels of cytokines from baseline to 12 weeks (delta values) in the immune control, viral relapse, evolving clinical relapse, and resolving clinical relapse groups. To the right are the main contributing variables to component 1 for the delta values. IP-10, TNF, IL-9, IFN-γ, MIP-1β, and IL-12 are the main drivers for a more positive first component in the evolving clinical relapse group. sPLS-DA sparse Partial Least Square Discriminant Analysis, IP-10 IFN-γ-induced protein 10, TNF tumor necrosis factor, IL-9 interleukin-9, IFN-γ interferon-γ, IL-12 interleukin-12.
Cytokine analysis at baseline
The differences in baseline cytokine concentrations between patients with immune control, viral relapse, and clinical relapse at 12 weeks were assessed. As displayed in Fig. 6, we found a significantly higher G-CSF value at baseline for patients with clinical relapse (p = 0.043). Using the Bonferroni post hoc test, G-CSF was significantly higher only when comparing patients with clinical relapse to the immune control group (p = 0.039).
There were no significant differences between the clinical response groups in any of the other 21 cytokines.
A ROC analysis was performed to define an optimal cut-off for baseline G-CSF to discriminate between patients who experienced clinical relapse and not. The cut-off that maximized specificity and sensitivity was 250 pg/ml, with a sensitivity of 0.71, specificity of 0.64, positive predictive value of 0.54, negative predictive value of 0.79 and AUC of 0.68.
As an unbiased approach, sPLS-DA analysis was performed to investigate whether integrated cytokine profiles at baseline could predict clinical and virological response 12 weeks after treatment cessation. There was no clear separation of the response groups (immune control, viral relapse, and clinical relapse) based on the 22 baseline cytokines included in the analysis (Fig. 5a).
Discussion
Cytokines are an indispensable part of the immune response, and several studies have investigated the role of cytokines in HBV infection14,22,23,24,25. However, the role the individual cytokines play in HBV infection pathogenesis and disease progression is poorly understood25. In this study, we found that evolving clinical relapse 12 weeks after NA cessation was associated with specific increases in IP-10 and TNF. The separation of the evolving clinical relapse group from the other three response groups at 12 weeks (immune control, viral relapse, and resolving clinical relapse), was visualized by sPLS-DA and driven mainly by IP-10, TNF, IL-9, IFN-γ, and IL-12.
IP-10, also known as C-X-C motif chemokine ligand-10 (CXCL10), is secreted by a diversity of cells, including but not limited to monocytes, neutrophils, eosinophils, activated T lymphocytes, natural killer cells, endothelial cells, and hepatocytes26,27. It is a chemokine (chemotactic cytokine) that attracts peripheral leucocytes into the liver25. In acute HBV infection, IP-10 is found to be higher in patients who resolve the infection than in patients who develop persistent infection22. We found a significant increase in IP-10 plasma levels, 12 weeks after treatment cessation in patients with evolving clinical relapse (viz a progressive flare). This is consistent with previous studies that have found an increase in IP-10 during hepatic flares24,28. It has been argued that IP-10 can be used as a predictor of treatment response and progression of disease25. Wang et al. found that IP-10 was an independent predictor of significant fibrosis, and that the serum level of IP-10 was positively correlated with the severity of liver fibrosis26. Serum IP-10 level has also been found to be associated with HBsAg seroclearance in CHB29. IP-10 probably plays a key role in HBV infection and may be useful in distinguishing the phases of infection, with the highest levels in active hepatitis30. Thus, our finding is consistent with prior observations and confirms the importance of IP-10 in the immune response against HBV.
TNF is a proinflammatory cytokine mainly produced by monocytes and macrophages. It has been shown in vitro that human macrophages secrete TNF in response to high titres of HBV31. Among CHB patients with liver cirrhosis, TNF is found to correlate with ongoing inflammation32. An association between liver damage and TNF producing CD4 T-cells has been found in patients with CHB flare33. TNF plays an important role in the defence against many infections, and the role of TNF in HBV immunity is supported by the finding that the use of TNF inhibitors can lead to HBV reactivation34. Our finding of an elevation in TNF in patients with evolving clinical relapse is in line with a study by Hall et al., who found increased activity of TNF in patients with hepatitis flares after stopping NA therapy24. Another study found no increase in TNF in patients with a CHB flare28, but this study included only five patients stopping NA therapy. Our observation of an increase in TNF during a HBV flare is plausible, as TNF is a potent proinflammatory cytokine.
In line with our findings from the conventional statistical analyses, sPLS-DA showed a higher first component value for the evolving clinical relapse group compared to the immune control, viral relapse, and resolving clinical relapse groups when looking at the change in cytokines from baseline to 12 weeks. This separation was driven mainly by IP-10, TNF, IL-9, IFN-γ, MIP-1β, and IL-12, all pro-inflammatory cytokines, suggesting that these are upregulated during a progressive flare. Both IFN-γ and MIP-1β have been found to increase after CHB treatment cessation35. IL-12 levels are associated with ALT levels, and high levels of IL-12 has also been linked to HBeAg or HBsAg seroconversion25,36.
We found that G-CSF at baseline was elevated in patients with clinical relapse 12 weeks after NA therapy cessation. G-CSF is a hematopoietic growth factor and stimulates neutrophil development and differentiation37. G-CSF therapy has been used in HBV associated acute on chronic liver failure, and some Asian studies have found improved liver function and survival rates in patients receiving this treatment38,39. However, a European multicentre study on acute on chronic liver failure of different etiologies failed to demonstrate any positive effect of G-CSF therapy40. To our knowledge, the role of G-CSF in HBV infection is still elusive, and further exploration is warranted.
At present, baseline cytokines have not proven their role as predictors of outcome after treatment cessation in CHB. Wübbolding et al. have suggested that a combination of cytokines can be valuable as predictors of outcome but found poor performance of single cytokines23. Hall et al. found no difference in baseline cytokine production between flare and non-flare patients with HBeAg-negative CHB who stopped NA treatment, but their analyses did not include G-CSF24. Our finding that sPLS-DA analysis showed no clear differentiation of baseline cytokine profiles between the 12-weeks clinical response groups are in line with these observations. The ROC analysis we performed to further examine the ability of baseline G-CSF to predict outcome yielded a low AUC of 0.68, indicating that baseline G-CSF alone is not suitable for this purpose. Our established cut-off of 250 pg/ml had limited value in clinical decision making due to insufficient sensitivity and specificity.
After stopping NA therapy, about 20–25% of patients experience an ALT flare that typically occurs during the first 12–24 weeks after treatment cessation41. It has been established that stopping tenofovir leads to an earlier flare than stopping entecavir; usually patients stopping tenofovir experience a flare within 12 weeks, whereas patients stopping entecavir experience a flare closer to 24 weeks or later42,43,44,45. The mechanisms behind the difference in relapse patterns are unclear, but may be due to differences in immunomodulatory effects46. We measured cytokines at baseline and 12 weeks after NA cessation, and type of NA therapy could have affected our results. As expected, most patients treated with entecavir were in the immune control group whereas most patients treated with tenofovir were in the viral and clinical relapse groups at 12 weeks (Table 1).
Re-start of antiviral treatment was more common in the resolving clinical relapse group, where eight patients re-started treatment at the 8 weeks visit, compared to the evolving clinical relapse group, where only one patient re-started treatment at week eight. One could argue that re-treatment at week eight led to a fall in HBV DNA and ALT and consequently classification as resolving clinical relapse four weeks later. Thus, re-treatment may have impeded an immunological process in these patients.
Duration of NA treatment before cessation differed significantly across the clinical response groups; the longest median duration was observed in the evolving clinical relapse group (81 months) and the shortest in the immune control group (34 months). Duration of NA treatment is perceived as vital for the outcome in stop-studies as longer duration of viral suppression is thought to be associated with enhanced immune restoration17. Our study supports this hypothesis as the evolving clinical relapse group with presumably the highest immune activity was the group with the longest treatment prior to cessation.
The strength of our study was the rigorous, prospective study design where all patients underwent close monitoring after treatment cessation. All common viral genotypes were represented, as well as different age groups and ethnicities.
The study also had some limitations. First, the sample size was small. In particular, the small size of the evolving clinical relapse group limited statistical power, and there are possibly other interesting cytokine dynamics that we failed to unravel. Second, we only measured cytokine levels at baseline and 12 weeks thereafter. Due to the short half-lives of cytokines, we may have missed possibly intricate dynamics. Finally, we only described short-term response (12 weeks), and longer follow-up is needed to observe if these early changes in cytokines and chemokines can predict HBsAg loss which usually happens several months to years after NA cessation. We will continue to follow these patients to evaluate if the cytokine dynamics between baseline and 12 weeks of follow-up can predict long-term effects of treatment cessation.
In conclusion, we found that the immunological response occurring with HBV reactivation after NA cessation is associated with an increase in IP-10 and TNF. Longer follow-up is needed to evaluate whether these cytokines can distinguish beneficial flare from detrimental flare and predict long-time outcome after treatment withdrawal in chronic HBeAg-negative hepatitis B.
Data availability
The data that support the findings of this study are available upon reasonable request from the corresponding author.
References
WHO. Hepatitis B Fact sheet 2020, https://www.who.int/news-room/fact-sheets/detail/hepatitis-b (2020).
Trépo, C., Chan, H. L. & Lok, A. Hepatitis B virus infection. Lancet 384, 2053–2063. https://doi.org/10.1016/s0140-6736(14)60220-8 (2014).
Nayagam, S. et al. Requirements for global elimination of hepatitis B: A modelling study. Lancet Infect. Dis. 16, 1399–1408. https://doi.org/10.1016/s1473-3099(16)30204-3 (2016).
Collaborators, G. H. B. Global, regional, and national burden of hepatitis B, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol. Hepatol. 7, 796–829. https://doi.org/10.1016/s2468-1253(22)00124-8 (2022).
Jeng, W. J., Chen, Y. C., Chien, R. N., Sheen, I. S. & Liaw, Y. F. Incidence and predictors of hepatitis B surface antigen seroclearance after cessation of nucleos(t)ide analogue therapy in hepatitis B e antigen-negative chronic hepatitis B. Hepatology 68, 425–434. https://doi.org/10.1002/hep.29640 (2018).
Kim, G. A. et al. HBsAg seroclearance after nucleoside analogue therapy in patients with chronic hepatitis B: Clinical outcomes and durability. Gut 63, 1325–1332. https://doi.org/10.1136/gutjnl-2013-305517 (2014).
Dusheiko, G., Agarwal, K. & Maini, M. K. New approaches to chronic hepatitis B. N. Engl. J. Med. 388, 55–69. https://doi.org/10.1056/NEJMra2211764 (2023).
Hsu, Y. C. et al. Incidences and determinants of functional cure during entecavir or tenofovir disoproxil fumarate for chronic hepatitis B. J. Infect. Dis. 224, 1890–1899. https://doi.org/10.1093/infdis/jiab241 (2021).
Hadziyannis, S. J., Sevastianos, V., Rapti, I., Vassilopoulos, D. & Hadziyannis, E. Sustained responses and loss of HBsAg in HBeAg-negative patients with chronic hepatitis B who stop long-term treatment with adefovir. Gastroenterology 143, 629-636.e621. https://doi.org/10.1053/j.gastro.2012.05.039 (2012).
Sonneveld, M. J. et al. Probability of HBsAg loss after nucleo(s)tide analogue withdrawal depends on HBV genotype and viral antigen levels. J. Hepatol. 76, 1042–1050. https://doi.org/10.1016/j.jhep.2022.01.007 (2022).
Hall, S. A. L. et al. Discontinuation of nucleot(s)ide analogue therapy in HBeAg-negative chronic hepatitis B: A meta-analysis. Gut 71, 1629–1641. https://doi.org/10.1136/gutjnl-2020-323979 (2022).
Hall, S. A. L. et al. Stopping nucleot(s)ide analogues in non-cirrhotic HBeAg-negative chronic hepatitis B patients: HBsAg loss at 96 weeks is associated with low baseline HBsAg levels. Aliment. Pharmacol. Ther. 56, 310–320. https://doi.org/10.1111/apt.16968 (2022).
Liem, K. S. et al. Limited sustained response after stopping nucleos(t)ide analogues in patients with chronic hepatitis B: Results from a randomised controlled trial (Toronto STOP study). Gut 68, 2206–2213. https://doi.org/10.1136/gutjnl-2019-318981 (2019).
Höner Zu Siederdissen, C. et al. Viral and host responses after stopping long-term nucleos(t)ide analogue therapy in HBeAg-negative chronic hepatitis B. J. Infect. Dis. 214, 1492–1497. https://doi.org/10.1093/infdis/jiw412 (2016).
Berg, T. et al. Long-term response after stopping tenofovir disoproxil fumarate in non-cirrhotic HBeAg-negative patients: Finite study. J. Hepatol. 67, 918–924. https://doi.org/10.1016/j.jhep.2017.07.012 (2017).
Fan, R. et al. Combining hepatitis B virus RNA and hepatitis B core-related antigen: Guidance for safely stopping nucleos(t)ide analogues in hepatitis B e antigen-positive patients with chronic hepatitis B. J. Infect. Dis. 222, 611–618. https://doi.org/10.1093/infdis/jiaa136 (2020).
van Bommel, F. et al. A multicenter randomized-controlled trial of nucleos(t)ide analogue cessation in HBeAg-negative chronic hepatitis B. J. Hepatol. 78, 926–936. https://doi.org/10.1016/j.jhep.2022.12.018 (2023).
Liu, C., Shih, Y. F. & Liu, C. J. Immunopathogenesis of acute flare of chronic hepatitis B: With emphasis on the role of cytokines and chemokines. Int. J. Mol. Sci. https://doi.org/10.3390/ijms23031407 (2022).
Johannessen, A. et al. The Nuc-Stop study: An open-label, randomized trial of different re-start strategies after treatment withdrawal in HBeAg negative chronic hepatitis B patients. J. Hepatol. 78, S1150–S1151. https://doi.org/10.1016/S0168-8278(23)03285-3 (2023).
European Association for the Study of the Liver. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J. Hepatol. 67, 370–398. https://doi.org/10.1016/j.jhep.2017.03.021 (2017).
Rohart, F., Gautier, B., Singh, A. & Lê Cao, K.-A. mixOmics: An R package for ‘omics feature selection and multiple data integration. PLoS Comput. Biol. 13, e1005752–e1005752. https://doi.org/10.1371/journal.pcbi.1005752 (2017).
Yoshio, S. et al. Cytokine and chemokine signatures associated with hepatitis B surface antigen loss in hepatitis B patients. JCI Insight https://doi.org/10.1172/jci.insight.122268 (2018).
Wübbolding, M. et al. Pilot study using machine learning to identify immune profiles for the prediction of early virological relapse after stopping nucleos(t)ide analogues in HBeAg-negative CHB. Hepatol. Commun. 5, 97–111. https://doi.org/10.1002/hep4.1626 (2021).
Hall, S. A. et al. Hepatitis B virus flares following nucleot(s)ide analogue cessation are associated with activation of TLR signalling pathways. J. Infect. Dis. https://doi.org/10.1093/infdis/jiac375 (2022).
Zhong, S., Zhang, T., Tang, L. & Li, Y. Cytokines and chemokines in HBV infection. Front. Mol. Biosci. 8, 805625. https://doi.org/10.3389/fmolb.2021.805625 (2021).
Wang, Y. et al. Predictive value of serum IFN-gamma inducible protein-10 and IFN-gamma/IL-4 ratio for liver fibrosis progression in CHB patients. Sci. Rep. 7, 40404. https://doi.org/10.1038/srep40404 (2017).
Liu, M. et al. CXCL10/IP-10 in infectious diseases pathogenesis and potential therapeutic implications. Cytokine Growth Factor Rev. 22, 121–130. https://doi.org/10.1016/j.cytogfr.2011.06.001 (2011).
Tan, A. T. et al. A longitudinal analysis of innate and adaptive immune profile during hepatic flares in chronic hepatitis B. J. Hepatol. 52, 330–339. https://doi.org/10.1016/j.jhep.2009.12.015 (2010).
Wong, G. L. et al. Serum interferon-inducible protein 10 levels predict hepatitis B s antigen seroclearance in patients with chronic hepatitis B. Aliment. Pharmacol. Ther. 43, 145–153. https://doi.org/10.1111/apt.13447 (2016).
Wiegand, S. B. et al. Soluble immune markers in the different phases of chronic hepatitis B virus infection. Sci. Rep. 9, 14118. https://doi.org/10.1038/s41598-019-50729-5 (2019).
Cheng, X. et al. Hepatitis B virus evades innate immunity of hepatocytes but activates cytokine production by macrophages. Hepatology 66, 1779–1793. https://doi.org/10.1002/hep.29348 (2017).
Barathan, M. et al. Comparative expression of pro-inflammatory and apoptotic biosignatures in chronic HBV-infected patients with and without liver cirrhosis. Microb. Pathog. 161, 105231–105231. https://doi.org/10.1016/j.micpath.2021.105231 (2021).
Wang, H. et al. TNF-α/IFN-γ profile of HBV-specific CD4 T cells is associated with liver damage and viral clearance in chronic HBV infection. J. Hepatol. 72, 45–56. https://doi.org/10.1016/j.jhep.2019.08.024 (2020).
Pauly, M. P. et al. Incidence of hepatitis B virus reactivation and hepatotoxicity in patients receiving long-term treatment with tumor necrosis factor antagonists. Clin. Gastroenterol. Hepatol. 16, 1964-1973.e1961. https://doi.org/10.1016/j.cgh.2018.04.033 (2018).
Rinker, F. et al. Hepatitis B virus-specific T cell responses after stopping nucleos(t)ide analogue therapy in HBeAg-negative chronic hepatitis B. J. Hepatol. 69, 584–593. https://doi.org/10.1016/j.jhep.2018.05.004 (2018).
Wu, J. F. et al. The effects of cytokines on spontaneous hepatitis B surface antigen seroconversion in chronic hepatitis B virus infection. J. Immunol. 194, 690–696. https://doi.org/10.4049/jimmunol.1401659 (2015).
Murphy, K., Weaver, C. T., Berg, L. & Janeway, C. A. Janeway's immunobiology. 10th edition / Kenneth Murphy, Casey Weaver, Leslie Berg; with contribution by Gregory Barton.; International student edition. edn, (W.W. Norton and Company, 2022).
Duan, X. Z. et al. Granulocyte-colony stimulating factor therapy improves survival in patients with hepatitis B virus-associated acute-on-chronic liver failure. World J. Gastroenterol. 19, 1104–1110. https://doi.org/10.3748/wjg.v19.i7.1104 (2013).
Tong, J. et al. Granulocyte colony-stimulating factor accelerates the recovery of hepatitis B virus-related acute-on-chronic liver failure by promoting M2-like transition of monocytes. Front. Immunol. 13, 885829. https://doi.org/10.3389/fimmu.2022.885829 (2022).
Engelmann, C. et al. Granulocyte-colony stimulating factor (G-CSF) to treat acute-on-chronic liver failure: A multicenter randomized trial (GRAFT study). J. Hepatol. 75, 1346–1354. https://doi.org/10.1016/j.jhep.2021.07.033 (2021).
Ghany, M. G. et al. Serum alanine aminotransferase flares in chronic hepatitis B infection: The good and the bad. Lancet Gastroenterol. Hepatol. 5, 406–417. https://doi.org/10.1016/s2468-1253(19)30344-9 (2020).
Chen, C. H. et al. Earlier and higher rate of hepatitis B virus relapse after discontinuing tenofovir versus entecavir in hepatitis B e antigen-positive patients. J. Infect. Dis. 225, 1974–1981. https://doi.org/10.1093/infdis/jiab596 (2022).
Höner Zu Siederdissen, C. et al. Contrasting timing of virological relapse after discontinuation of tenofovir or entecavir in hepatitis B e antigen-negative patients. J. Infect. Dis. 218, 1480–1484. https://doi.org/10.1093/infdis/jiy350 (2018).
Su, T. H. et al. Distinct relapse rates and risk predictors after discontinuing tenofovir and entecavir therapy. J. Infect. Dis. 217, 1193–1201. https://doi.org/10.1093/infdis/jix690 (2018).
Liu, Y. C., Jeng, W. J., Peng, C. W., Chien, R. N. & Liaw, Y. F. Off-tenofovir hepatitis flares in HBeAg-negative patients occur earlier, more frequent and severe than those off-entecavir therapies. Liver Int. 42, 551–560. https://doi.org/10.1111/liv.15140 (2022).
Chen, C.-H. et al. Higher rate of HBsAg loss after discontinuation of tenofovir than entecavir in patients with chronic hepatitis B. Aliment. Pharmacol. Ther. https://doi.org/10.1111/apt.17602 (2023).
Acknowledgements
We express our gratitude to all the study participants. The authors also thank study coordinator Sissel Hafsmo and all study nurses and technicians for invaluable support.
Funding
This study was funded by South-Eastern Norway Regional Health Authority (Grant Nos. 2018092 A. J. and 2021091 A. J.) and Regional Inflammation Research Network (RIRNet), Norway (D.H.R.).
Author information
Authors and Affiliations
Contributions
A.J., D.H.R., H.C.D.A., and O.D. designed the study. A.J., D.H.R., and N.K.B. supervised the study. A.J., D.H.R., E.S., and O.D. included and examined the study participants. D.H.R. and H.C.D.A. performed laboratory analyses. A.J., D.H.R., D.S., H.C.D.A., and M.H. analysed the data. A.J., D.H.R., and M.H. drafted the manuscript. All authors contributed to editing and finalizing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Holmberg, M., Aass, H.C.D., Dalgard, O. et al. Treatment cessation in HBeAg-negative chronic hepatitis B: clinical response is associated with increase in specific proinflammatory cytokines. Sci Rep 13, 22590 (2023). https://doi.org/10.1038/s41598-023-50216-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-50216-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.