Abstract
Study design:
Case series, consecutive sample, survey.
Objectives:
To examine the incidence of spinal cord injuries sustained as a result of falls compared with other causes, and to investigate rehabilitation outcomes between these two groups.
Settings:
Tertiary care, spinal cord injury rehabilitation unit (National Spinal Injuries Center), Stoke Mandeville Hospital, UK.
Methods:
Demographic information and descriptive statistics were examined for individuals sustaining their injury via falls vs non-falls. Statistical analysis investigated rehabilitation outcomes between the groups.
Results:
The etiology of spinal cord injury (SCI) reported is similar to previous findings. Individuals who sustained their SCI as a result of falls and other causes made equal improvements from the start to end of rehabilitation, according to the Needs Assessment Checklist, a clinical measure of individual rehabilitation needs in 10 domains. However, those in the falls group achieved less overall throughout rehabilitation, and this was significant at pre-discharge for the areas of bladder management, mobility and discharge.
Conclusion:
Results highlight the need for specific consideration to be made of the rehabilitation needs of individuals who sustain SCI as a result of a fall, and for these to be addressed in rehabilitation programming.
Similar content being viewed by others
Introduction
In the United Kingdom, the incidence of spinal cord injury (SCI) is estimated to be 1200 each year; with ∼40 000 currently living with this disability.1 While the etiology of SCI is varied, many spinal injuries centers in the United Kingdom have noticed that an increasing proportion of individuals are being admitted as a result of falls.
Many studies have examined the etiology of SCI, but it can be difficult to make a comparison between studies due to differing inclusion criteria. For example, some studies record trampolining accidents as a fall, whereas others would record this as a sporting activity. Results also vary across countries and cultures. For example, in the United States there is a greater number of spinal cord injuries as a result of violence compared with in the United Kingdom.2 Additionally, some studies include non-traumatic spinal cord injuries while others do not. These factors should be taken into consideration when examining reports of the epidemiology and causes of SCI.
One consistent finding, however, is that falls account for a significant proportion of SCIs. For example, a systematic review of the worldwide incidence of SCI revealed that road traffic accidents (RTA) and falls were the most common causes of injury.3 It was also found that in the majority of studies reviewed, there was a higher incidence of traumatic SCI in two particular age groups: those between the ages of 15 and 29, and those over the age of 65.
According to the NSCISC (National Spinal Cord Injury Statistical Center) database,4 spinal cord injuries sustained between 2005 and 2010 resulted from the following causes: RTAs (40.4%), falls (27.9%), violence (15.0%), other (8.4%), sports accidents (8.0%) and unknown (0.1%). Apparelyzed1 report statistics of traumatic injuries only, and revealed falls as the highest cause of SCI with 41.7% of injuries sustained in this way. SCI caused by RTA came second (36.8%), followed by injuries caused by sharp trauma/assault (2.7%), sport (11.6%), knocked over/collision/lifting (4.2%) and trauma non-specific (3.3%). Of those who sustained falls, 12.6% fell a height, 11.7% fell down the stairs, 3.3% jumped, 7.5% fell down and 6.6% were unspecified falls.1
Kennedy et al.5 examined a representative sample of 281 SCI patients, from six specialist centers across Europe. Injury data revealed that the majority of individuals sustained their SCI as a result of a RTA (37.7%), followed by falls (28.9%), sports accidents (19.6%), non-traumatic injuries (6.7%), other (4.6%) and assault (2.5%). Data collected at the National Spinal Injuries Center (NSIC), Stoke Mandeville Hospital (UK) between May 2009 and May 2010 revealed a slightly different pattern of etiology, with non-traumatic injuries and RTAs being the leading causes of SCI, each accounting for 33.6% of injuries, with falls the next most common etiology (18.8%), followed by sport (8%), assault (4%) and other (2%).6
Trends in SCI etiology over the years indicate that RTAs have continued to be the most common cause of SCI, according to data gathered between 1973 and 2010.4 With the exception of the years 1990–1994, when violence was the second most common cause of injury, falls have remained the second highest cause of SCI.4 However, the percentage of SCI recorded as a result of falls has shown a clear increase over the years. This is illustrated in the NSCIC database;4 in 1973–1979, 16.5% of injuries were accounted for by falls, a figure which rose to 20% by 1990–1994, and finally to 27.9% in 2005–2010.
The rising proportion of individuals sustaining SCI as a result of falls has also been documented in the research literature. DeVivo and Chen7 carried out a prospective study of 45 442 patients who were injured between 1935 and 2008, finding that falls are accounting for an increasing proportion of injuries over time. In addition, there are rising numbers of individuals who are affected with high-level tetraplegia, in need of a ventilator, and being discharged to a nursing home, and the mean age at injury was 9 years higher in 2008 compared with in the 1970s.
In a study of Finnish adults over 50 years of age, the number of individuals who suffered an SCI due to a fall was found to increase at an annual rate of 24% between 1970 and 1995,8 a marked pattern that continued with subsequent data collection to 2004.9 The authors noted that demographic changes were insufficient to explain this trend.
Taken together, these findings are significant considering the increasing older adult population,10 and the positive correlation between falls resulting in SCI and age.4 Falls in the elderly are more likely to result in incomplete cervical injuries, life threatening complications, a longer hospital stay and a much increased cost of care.11, 12 This population are also more likely to experience mortality; those over the age of 65 who sustain cervical fractures and SCI have been found to have a mortality rate of 21–30%.13 Despite the significant consequences of SCI caused by a fall, particularly among the elderly, there has been little research examining SCI rehabilitation as a function of falls compared with other causes. Much comparative research into rehabilitation outcome in SCI has focused on coarse distinctions between traumatic and non-traumatic injury, and has typically found that rehabilitation outcomes are similar between these groups. Factors such as age at injury have also been examined.
McKinley et al.14 compared rehabilitation outcome in individuals with traumatic vs vascular SCI, using 10-year prospective data. Groups were matched for age, length of stay and injury completeness. No significant differences were found between vascular and traumatic SCI in functional outcome, as measured by the Functional Independence Measure, length of stay and disposition. Rehabilitation outcome in traumatic and non-traumatic SCI has also been examined as a function of whether patients were admitted to specialist or non-specialist spinal injury centers.15 After controlling for demographic variables, it was found that patients in specialist spinal injury centers made greater progress in rehabilitation in terms of functional outcome, but this difference was only the case for those with traumatic injury etiology.
In another cohort study, individuals who sustained traumatic SCI were divided into two groups: violent etiology (gunshot wound, knife wound or assault), and non-violent etiology (RTA and falls), matched for neurological level of injury.16 Although several demographic differences were noted between the two groups, inpatient rehabilitation outcomes were found not to differ significantly. All individuals reached similar achievement in functional independence and discharge outcomes.
Waters et al.17 examined post-rehabilitation outcomes after SCI caused by RTAs and firearms as a function of various factors, including etiology. It was found that rehabilitation outcomes were strongly affected by disability, completeness of injury and substance abuse after injury. However, etiology and ethnicity did not influence rehabilitation outcomes.
Kennedy et al.18 conducted a comparative analysis of SCI rehabilitation outcomes in several domains in older and younger adults, matched for injury characteristics. It was found that older adults achieved less independence in skin management compared with younger adults. Scivoletto et al.19 also found that patients over 50 years of age achieved fairly good outcomes in rehabilitation, but showed poorer neurologic recovery, significantly less independence in daily living, less independence in bladder and bowel management, and a lower frequency of independent ambulation compared with their younger counterparts. Older age was also associated with increased medical problems. Similarly, Putzke et al.20 found that older individuals with traumatic SCI reported poorer functioning on several domains including functional independence, life satisfaction, perceived physical health and disability; it appears that older age may have a small detrimental effect on SCI rehabilitation outcome, but this seems to be restricted to particular domains of functioning, and does not limit ability to benefit from rehabilitation overall. These findings highlight the need for rehabilitation to address the unique needs of different age groups in rehabilitation programming.
The research above demonstrates that spinal cord injuries caused by falls are common and can have wide-ranging consequences, particularly because individuals in this population tend to be older than individuals who sustain an SCI through other causes. The purpose of the current study is to undertake a comparative analysis of rehabilitation outcomes of individuals who were admitted to the National Spinal Injuries Centre (NSIC, UK) as a result of falls vs other causes, using data collected over an 18-month period. This study aims to investigate the following questions:
-
1)
What is the incidence of SCI as a result of falls compared with other causes in the past 18 months, and do factors such as age, sex and injury characteristics differ between these groups?
-
2)
Is there a difference in rehabilitation outcomes between individuals sustaining their injury as a result of falls compared with other causes?
Materials and methods
Participants
This audit utilized routinely collected data from 356 patients who were admitted to the NSIC between 1 May 2010 and 1 November 2011, for newly acquired traumatic and non-traumatic SCI. In total, 358 patients were admitted in this time period (262 males and 94 females), but two were excluded from this audit because no cause of injury was specified. The mean age of the sample at time of injury was 45.04 years (s.d.=18.52).
Data regarding injury characteristics was available for 304 individuals in the sample, and indicated that complete paraplegic injuries accounted for 7.6% of injuries, incomplete paraplegic injuries 9.8%, complete tetraplegic injuries 25.3% and incomplete tetraplegic injuries 42.7%. Of the 352 individuals for whom data regarding level of injury was available, cervical injuries accounted for 46.1% of injuries, thoracic 39% and lumbar 13.8%. The causes of injury for the total sample were as follows: non-traumatic=35.7%, RTA=27.8%, fall=22.8%, sport=10.4%, assault=2.2%, other=1.1%. Of those who fell, 14.6% of falls were domestic, 5.6% unclassified, 1.7% industrial, 0.6% jumped and 0.03% were self-harm injuries.
Design
Case series, consecutive sample, survey design.
Measures
The Needs Assessment Checklist21 (NAC) was used to measure rehabilitation outcome. This is a routinely used measure at the NSIC to ascertain patients’ needs and abilities, in order to set targets in Goal Planning, the rehabilitation framework utilized at the center.
The NAC covers 10 specific rehabilitation domains: personal health care; activities of daily living; skin management; bladder management; bowel management; mobility; wheelchair; community preparation; psychology and discharge. The NAC is completed by the patient, who rates their degree of independence on a set of behavioral indictors within each domain, using a four-point scale ranging from ‘completely dependent’ to ‘completely independent’. Independence may be physical, or verbal that is, the ability to instruct others to carry out the particular task, depending on functional ability. Scores on each NAC subscale are totaled and the percentage achieved within each is calculated. This information is utilized to tailor rehabilitation, whereby unique behavioral targets are set to progressively help patients to achieve independence in every domain. The NAC has well-established reliability and validity as a clinical measure of rehabilitation outcome.22
Procedure
The sample was collapsed into two groups based on cause of injury (falls vs all other SCI etiology [‘non-falls’]) and rehabilitation outcomes were compared utilizing NAC data. The NAC data were gathered at two time points during rehabilitation; the first NAC administration was after mobilization, and the second administration was just before the patient moving to the pre-discharge ward. NACs were administered by a trained member of the patient’s multi-disciplinary team. Between first and second NAC administration, Goal Planning meetings took place for each patient on a 3-weekly basis, in which patient-centered targets for rehabilitation were continuously reviewed and set, helping patients to progress in their rehabilitation. All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Statistical analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS Inc., Chicago, IL, USA) version 17.0. A Shapiro–Wilk test was first computed to determine the likelihood that the data came from a normal distribution, and revealed that the majority of the data violated the assumption of normality.
Demographic information for individuals in the falls and non-falls groups was examined; frequencies of sex, type of injury and level of injury were computed and compared between groups using χ2 tests, and mean age was compared using the Mann–Whitney test. In order to investigate rehabilitation outcomes for the falls and non-falls groups, achievement scores and first NAC was compared using the Mann–Whitney (two-tailed) test, as was achievement at second NAC. The difference in scores between NAC1 and NAC2 for each group was calculated (improvement), and compared within groups using the Wilcoxon Signed Ranks test, and between groups using the Mann–Whitney (two-tailed) test.
Results
Differences in demographics and injury characteristics between the falls and non-falls groups
In the sample as a whole, 81 patients sustained their SCI as a result of a fall, and 275 patients were injured from other causes. In the falls group, 74.1% were males and 25.9% females, and in the non-falls group 73.5% were males and 26.5% females. This ratio of males to females as a function of etiology was not significant. Mean age at injury was 51.38 years (s.d.=20.63) for falls, and 43.16 years (s.d.=17.45) for non-falls. On average, individuals in the falls group were 8.22 years older than those in the non-falls group, and this difference was statistically significant (U=7482.0, P<0.001).
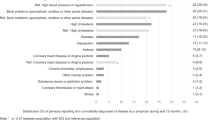
With respect to the level of injury, a higher percentage of individuals in the falls group sustained cervical injuries compared with those in the non-falls group, as shown in Figure 1. The percentage of thoracic injuries was greater in the non-falls group than in the falls group, and there were slightly more lumbar injuries in the falls group. However, these differences in proportion of level of injury as a function of etiology were not significant. The proportion of individuals sustaining different types of injury (complete/incomplete, paraplegia/tetraplegia) as a function of cause of injury is shown in Figure 2, but these differences were not significant.
Percentage achievement at first and second needs assessment
As Figure 1 shows individuals who sustained SCI from a fall have lower scores in the majority of NAC domains at first administration, and lower scores in all domains at second administration. A Mann–Whitney (two-tailed) test revealed that individuals in the falls group achieved significantly less on four domains at first NAC administration: activities of daily living (U=9283.5, P=0.028), skin management (U=8989.0, P=0.016), bladder management (U=8545.0, P=0.003) and wheelchair (U=8847.0, P=0.010), compared with the rest of the SCI population. There was no significant difference between the groups in scores on the remaining NAC subscales.
At second NAC administration, individuals in the falls group achieved significantly poorer rehabilitation outcomes in three domains: bladder management (U=3169.5, P=0.045), mobility (U=3020.0, P=0.016) and discharge (U=2840.5, P=0.004), compared with those in the non-falls group. No significant differences between the groups were evident in the other NAC domains.
Improvements in scores between first and second needs assessment
Figure 3 illustrates that although those in the falls group have poorer achievement in rehabilitation at first and second NAC compared with non-falls, they make comparable improvements over the course of rehabilitation. A Wilcoxon signed ranks test showed that all individuals made significant improvements in rehabilitation according to the difference between NAC1 scores post-mobilization, and NAC2 scores pre-discharge (4.89<Z<10.95, P<0.0001). For both groups, the greatest improvement in rehabilitation was observed in the domains of skin management (39.72% improvement for falls, 37.43% for non-falls) and bowel management (42.74% for falls, 39.33% for non-falls). The smallest improvements were made in psychology (13.07% for falls, 16.78% for non-falls), and physical healthcare (15.15% for falls, 16.08% for non-falls).
A Mann–Whitney (two-tailed) test demonstrated that no significant differences were found in rehabilitation improvements for individuals in the falls vs non-falls groups, with the exception of the community subscale of the NAC. Those who sustained SCI as a result of a fall made significantly less improvement in the community preparation domain of rehabilitation between NAC1 and NAC2 (U=3044.5, P=0.026).
Discussion
This audit revealed that in an 18-month period between May 2010 and November 2011, the incidence of SCI as a result of falls was 22.8%. The leading causes of injury were those of non-traumatic origin (35.7%), followed by RTAs (27.8%), and then falls. Individuals afflicted with SCI caused by a fall were found to make significant gains over the course of rehabilitation, comparable to those injured as a result of other causes. On the whole, however, those in the falls group had more needs to be addressed at rehabilitation commencement, and this pattern remained at the end of rehabilitation, with those in the falls group achieving poorer outcomes across the 10 different domains of rehabilitation measured by the NAC. This poorer outcome before discharge was significant for bladder management, mobility and discharge.
Implications
The present data regarding injury etiology obtained at the NSIC in the past 18 months was compared with that collected at the NSIC the previous year (2009–2010),6 indicating that the proportion of injuries sustained as a result of falls has risen by 4%. This is in accordance with the wider research literature, which has documented an increase in the proportion of SCI as a result of falls over the years, in a range of studies between 1935 and present.7, 8, 9 However, in the present study, the proportion of SCI accounted for by falls is lower than that reported in the European study mentioned earlier, in which 28.9% of injuries were caused by a fall.5 Furthermore, the finding that non-traumatic injury was the primary cause of SCI contrasts with records reporting RTA and falls as the top two causes of injury.4 This could be because the latter studies reported data on traumatic injuries only, but this would not explain the findings in relation to the European study,5 which did include non-traumatic injury data, and the proportion of SCI sustained by non-traumatic etiology was considerably lower than the current figure (35.7%), at 6.7%.
In terms of rehabilitation outcome as a function of etiology, the findings reported here are in partial agreement with previous research, indicating that outcome is independent of injury etiology.14, 16, 17 Individuals in falls and non-falls groups made large and significant improvements across a variety of domains throughout rehabilitation; this suggests that rehabilitation gains were of clinical significance and that on the whole, etiology did not influence ability to progress in rehabilitation. On the other hand, despite the equal improvements in rehabilitation, those who sustained SCI as a result of a fall achieved consistently poorer outcome across the majority of rehabilitation domains measured by the NAC compared with the rest of the SCI population, and had worse outcomes in terms of bladder management, mobility and discharge. This does not concur with the aforementioned research investigating outcome as a function of etiology of SCI more generally, and suggests that whether SCI was caused by a fall in contrast to other causes has an important impact on achievement in inpatient rehabilitation.
One factor that may have mediated the observed poorer outcome for individuals in the falls group is that of age, which was found to be significantly higher in these individuals compared with their counterparts who were not injured by a fall. This would fit with the previous literature finding that older adults generally achieve slightly less across a range of rehabilitation domains at discharge.19, 20 Overall, data gathered at the NSIC, however, in terms of older age,18 and falls etiology as in the present study, worse rehabilitation outcome in these groups is limited to a minority of domains, and overall individuals in all groups (older vs younger; falls vs non-falls) appear to make equal gains in rehabilitation. Those areas where significantly poorer outcomes were observed in the falls group are similar to those in research with older adults. It has been found that, as with individuals sustaining SCI from falls, older adults achieve less independence in bladder management19 and mobility.19, 20 This suggests that the present results may be partly explained in terms of age as opposed to solely falls etiology.
Future research directions
Given that little research has been conducted investigating the effect of specific etiology such as falls on rehabilitation outcome, considering the pertinent consequences for implicated individuals, and for healthcare (for example in terms of length of stay), future research could investigate how clinical practice could be modified to facilitate improved rehabilitation outcome for individuals injured as a result of a fall. This could be done through identifying specific needs of this population and how these may be better addressed to ensure the best possible outcomes for these individuals. Some factors that could be taken into account in future research looking into falls are the causes and height of the falls, medication use and cognitive factors. Another factor that was beyond the scope of the current research but which would be valuable to investigate in future comparative analyses of SCI rehabilitation outcomes in falls vs non-falls, is that of alcohol consumption, which has been found to be linked to risk for fall related injuries in older adults.23
Study limitations
A limitation of this research is that individuals in the falls and non-falls groups were not matched with regard to variables including demographic and injury characteristics. This should not have adversely impacted the results for the variables sex, level and type of injury, as no differences were found between the groups on these factors. However, as the proportion of older to younger adults was different in falls and non-falls groups, with individuals in the falls group being older on average, this may limit the robustness of the conclusions, which can be drawn regarding the effect of falls vs non-falls etiology on SCI rehabilitation outcome. Importantly, however, the present study has highlighted a need for future research in this area, given that SCI caused by a fall had been found to limit the level of achievement and independence in several domains, which is likely to impact an affected individual’s life post-discharge.
Conclusions
This is the first known study to have conducted a comparative analysis of rehabilitation outcomes for individuals who acquired SCI as a result of a fall vs other causes. This is despite the important implications that as a cause of injury, falls are associated with an older age at injury, higher likelihood of incomplete cervical damage and consequent implications for quality of life compared with the rest of the SCI population. This research demonstrates that individuals who sustain SCI caused by falls make similar improvements in rehabilitation compared with those injured from other causes, but their achievement scores consistently lag slightly behind their counterparts. At discharge, poorer outcomes were evident after falls, in the areas of bladder management, mobility and overall discharge independence. This indicates that individuals who acquired SCI from a fall may need greater attention in particular areas of rehabilitation, and for professionals in the multi-disciplinary team to be aware of these unique needs in order to adapt services and ensure that optimum outcomes can be achieved in this group, both in inpatient rehabilitation, and more generally in outpatient services.
References
Apparelyzed [Spinal Cord Injury homepage on the Internet] [cited 2011 Dec 20] Spinal Cord Injury Statistics. Available from: http://www.apparelyzed.com/statistics.html.
Spinal-Injury.net [homepage on the Internet] Causes of Spinal Cord Injury [cited 2011 Dec 20]. Available from: www.spinal-injury.net/causes-of-spinal-cord-injury.html.
Van den Berg ME, Castellote JM, Mahillo-Fernandez I, Pedro-Cuesta J . Incidence of traumatic spinal cord injury in Aragon, Spain (1972-2008). J Neurotrauma 2011; 28: 469–477.
National Spinal Cord Injury Statistical Centre (NSCISC) [homepage on the Internet]. Birmingham, Alabama; 2010 [cited 2011 Dec 20]. Annual Statistical Report, 2010 Complete public Version, from https://www.nscisc.uab.edu/public_content/annual_stat_report.aspx.
Kennedy P, Lude P, Elfström M Cognitive appraisals, coping and psychological outcomes: a multi centre European study. Unpublished report, Department of Clinical Psychology, National Spinal Injuries Centre, Stoke Mandeville Hospital, UK, 2010.
Blakey L Falls Audit (May 2009–May 2010) at the National Spinal Injuries Centre. Unpublished work, Department of Clinical Psychology, NSIC, Stoke Mandeville Hospital, UK 2011.
DeVivo MJ, Chen Y . Trends in new injuries, prevalent cases, and ageing with spinal cord injury. Arch Phys Med Rehabil 2011; 92: 332–338.
Kannus P, Niemi S, Palvanen M, Parkkari J . Continuously increasing number and incidence of fall-induced, fracture-associated, spinal cord injuries in elderly persons. Arch Intern Med 2000; 160: 2145–2149.
Kannus P, Palvanen M, Niemi S, Parkkari J . Alarming rise in the number and incidence of fall-induced cervical spine injuries among older adults. J Gerontol Biol Sci Med Sci 2006; 62: 180–183.
Cohen JE . Human population: the next half century. Science 2003; 302: 1172–1175.
Lovasik D . The older patient with a spinal cord injury. Crit Care Nurs Q 1999; 22: 20–30.
Spivak JM, Weis MA, Cotler JM, Call M . Cervical spine injuries in patients 65 and older. Spine 1994; 19: 2302–2306.
Golob JF, Claridge JA, Yowler CJ, Como JJ, Peerless JR . Isolated cervical spine fractures in the elderly: a deadly injury. J Trauma 2008; 64: 311–315.
McKinley W, Sinha A, Ketchum J, Deng X . Comparison of rehabilitation outcomes following vascular-related and traumatic spinal cord injury. J Spinal Cord Med 2011; 34: 410–415.
New PW, Simmonds F, Stevermuer T . Comparison of patients managed in specialised spinal rehabilitation units with those managed in non-specialised rehabilitation units. Spinal Cord 2011; 49: 909–916.
McKinley W, Cifu D, Keyser-Marcus L, Wilson K . Comparison of rehabilitation outcomes in violent versus non-violent traumatic SCI. J Spinal Cord Med 1998; 21: 32–36.
Waters RL, Adkins RH, Sie I, Cressy J . Postrehabilitation outcomes after spinal cord injury caused by firearms and motor vehicle crash among ethnically diverse groups. Arch Phys Med Rehabil 1998; 79: 1237–1243.
Kennedy P, Evans MJ, Berry C, Mullin J . Comparative analysis of goal achievement during rehabilitation for older and younger adults with spinal cord injury. Spinal Cord 2003; 41: 44–52.
Scivoletto G, Morganti B, Ditunno P, Ditunno JF, Molinari M . Effects on age on spinal cord lesion patients’ rehabilitation. Spinal Cord 2003; 41: 457–464.
Putzke JD, Barrett JJ, Richards JS, DeVivo MJ . Age and spinal cord injury: an emphasis on outcomes among the elderly. J Spinal Cord Med 2003; 26: 37–44.
Kennedy P, Hamilton LR . The needs assessment checklist: a clinical approach to measuring outcome. Spinal Cord 1999; 37: 136–139.
Berry C, Kennedy P . A psychometric analysis of the Needs Assessment Checklist (NAC). Spinal Cord 2002; 41: 490–501.
Grundstrom AC, Guse CE, Layde PM . Risk factors for falls and fall-related injuries in adults 85 years of age and older. Arch Gerontol Geriatr 2012; 54: 421–428.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kennedy, P., Cox, A. & Mariani, A. Spinal cord injuries as a consequence of falls: are there differential rehabilitation outcomes?. Spinal Cord 51, 209–213 (2013). https://doi.org/10.1038/sc.2012.124
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.124
Keywords
This article is cited by
-
The influence of psychological need on rehabilitation outcomes for people with spinal cord injury
Spinal Cord (2023)
-
Epidemiology of traumatic spinal cord injury in Finland
Spinal Cord (2021)