Abstract
Study design:
Our aim was to locate research and communicate the evidence found from scientific studies pertaining to the treatment of neurogenic detrusor overactivity (NDO) in the chronic stage of spinal cord injury (SCI).
Objective:
To address the controversy over the traditional (antimuscarinics) and the ‘new’ treatments for NDO and try to offer an insight on the rationale underlying the development of new drugs such as botulinum toxin (BTX), vanilloids, nociceptin/orphanin FQ. As a final point, to provide information on a new class of cation channels, the Degenerin/Epithelial Na+Channel (Deg/ENaC) Family that could be future targets for the management of NDO.
Setting:
International.
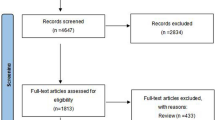
Methods:
Overview of English literature on drug management of NDO.
Results:
Agents that block the ‘efferent’ function of micturition reflex, such as antimuscarinics, are currently first-line therapy for NDO. They reach the highest level of evidence (1a) and grade of recommendation (A). However, many patients and physicians believe that the ‘efferent’ pharmacological management of NDO is not completely satisfactory. Consequently, research is trying to address issues of efficacy, tolerability and convenience of new therapeutic strategies targeting the ‘afferent’ function.
Conclusion:
Antimuscarinic therapy increases the bladder capacity and delays the initial urge to void. However, in some patients they fail to achieve the patient's therapeutic goals. New interesting approaches have been investigated in the last few years. BTX seems to be very promising in treating neurogenic overactive bladder (OAB), but other compounds are now on the horizon.
Similar content being viewed by others
Introduction
Until three decades ago, spinal cord injury (SCI) meant confinement to a wheelchair and a lifetime of medical co-morbidity with severe impairment of quality of life and significant reduction of life expectancy. Most SCI patients develop voiding dysfunction and present symptoms of urgency, frequency and/or urge incontinence. In the past three decades, important advances in the medical and surgical management of acute and chronic SCI have been made.1
Since the ‘90s, the advances in the neurosciences have drawn a lot of attention to the research of changes in micturition reflex function after SCI. The knowledge of physiology and pathophysiology of micturition reflex after trauma allowed the physician to offer effective treatment. It brought to the development of agents aimed at blocking the efferent function of micturition reflex. Antimuscarinic agents are currently the first-line therapy for overactive bladder neurogenic lower urinary tract symptoms (NLUTS). However, antimuscarinics were also shown to act during the storage phase of micturition reflex reducing the afferent input to the central nervous system.2 Consequently, basic science and clinical research is trying to address issues of efficacy, tolerability and convenience of new therapeutic strategies targeting the ‘afferent’ function.
In this overview of literature, we will first present a summary of micturition reflex in normal and pathological conditions. Subsequently, we will focus on the currently available pharmacological armamentarium for the treatment of NLUTS. Finally, we will address the controversy over the traditional (antimuscarinics) and the ‘new’ treatments for neurogenic detrusor overactivity (NDO) and try to offer insight on the underlying rationale of the development of new drugs.
Pathophysiology of micturition reflex
The lower urinary tract serves two main functions: urine storage without leakage (storage phase) and release of urine (voiding phase). These two functions are based on a coordinated interplay of reciprocal actions of central, peripheral autonomic and somatic neuronal pathways, and local peripheral factors (Figure 1).
The figure shows the reciprocal actions of central, peripheral autonomic and somatic neuronal pathways, which regulate the lower urinary tract. CNS, central nervous system; L-R, lateral region; M-R, medial region; N. Onuf, onuf's nucleus; PAG, periaqueductal gray; POA, preoptic area; PS-M, parasympathetic motoneuron; SUS, external striated urethral sphincter. A full color version of this figure is available at the Spinal Cord journal online.
During the storage phase, afferent impulses reach the central nervous system from the bladder and send information to the pons (the organizational hub for micturition). In the pontine tegmentum, imaging and neurophysiologic studies visualized a medial region (M-region), corresponding to Barrington's nucleus or pontine micturition center, which is involved in micturition reflex coordination, and a lateral region (L-region), which suppresses bladder contractions and improves external sphincter muscle activity during the storage phase.3 Several suprapontine centers, that is, basal ganglia, cerebellum, cortex, modulate the micturition reflex by a complex chemical control, which use different ligands (neurotransmitters) and receptors.4
The peripheral neurological control of micturition reflex involves the parasympathetic, sympathetic and somatic peripheral neuronal systems. The parasympathetic system, originating in the spinal cord sacral area (S2-S4) controls bladder contractions. It provides an excitatory input to the bladder through postganglion nerve terminal release of acetylcholine, which excites muscarinic receptors (M2, M3) in the detrusor smooth muscle and leads to its contraction. The sympathetic system, originating in the thoracolumbar cord (Th11-L2), is involved in bladder relaxation and urethral closure through postganglion nerve terminal release of norepinephrine (NE). NE provides an inhibitory input to the bladder, which excites β3 receptors in the detrusor body and leads to bladder relaxation. It also provides an excitatory input to the urethral smooth muscle, which excites α1 receptors in the urethra and leads to urethral closure. The somatic system provides an excitatory input to the striated urethral muscle. Motor neurons along the lateral–ventral horn of the sacral spinal cord (Onuf's nucleus), release acetylcholine, which acts on nicotinic (N) receptors to induce muscle contraction.
In vitro and in vivo experimental and clinical evidences showed that there are many neuronal terminal endings in the lower urinary tract that do not correspond to cholinergic and adrenergic innervation.5 These nerves, known as non-adrenergic–non-cholinergic system, are peptide containing fibers. They consist of small myelinated Ad and unmyelinated C fibers and may have an important role in the regulation of the lower urinary tract functions.5 The non-adrenergic–non-cholinergic system is thought to be ‘silent’ in normal conditions, but becomes active in aging and pathological conditions (that is, NLUTS).6 Over the past years, research has focused on this system to develop new drugs for the treatment of NLUTS and several new pharmacological achievements have been obtained.7 Table 1 summarises the main steps. Finally, Birder8 showed that the urothelial cells exhibit ‘neuronal-like’ properties, similar to mechanosensitive and nociceptive sensory nerves, by release of neuromediators (Figure 2).
The receptor/ligand net in the bladder urothelium. Ach, acetylcholine; ATP, adenosine tri-phosphate; M3, muscarinic receptor type 3; nAChR, nicotinic acetylcholine receptor; NGF, nerve growth factor; NK1, tachykinin receptor type 1; NO, nitric oxide; NOP, nociceptin/orphanin protein receptor; N/OFQ, nociceptin/orphanin FQ; P2x, purinergic receptor type 2x; P2y, purinergic receptor type y; SP, substance P; TrkA, tyrosine kinase receptor; TRPV1, transient receptor protein vanilloid type 1. A full color version of this figure is available at the Spinal Cord journal online.
Most of these systems are ‘silent’ in human beings with intact nervous systems but may become prominent following a neurological disease. Experimental evidence and clinical studies have shown that the reflex pathways, which modulate the micturition in chronic spinal animals and humans, are noticeably different from that of normal ones. In chronic spinal injured patients, the afferent limb of micturition reflex is carried by unmyelinated C fibers whereas in normal controls it goes through myelinated Ad fibers; the suprapontine control is lost and detrusor contraction happens in a reflex modality with dyssynergic contraction of the striated sphincter.9
Pharmacology of NLUTS
Methods are shown in Supplementary Annex 1
A single optimal medical therapy for NLUTS is not yet available, and many physicians believe that the ‘present efferent-based’ pharmacologic management of NDO is not completely satisfactory. We have reviewed the current treatment available as well as the new potential alternative treatments. Definition of evidence is shown in Supplementary Annex 2.
Antimuscarinic receptor antagonist
Currently, antimuscarinic agents (currently known as muscarinic receptor antagonists) are the first-line of choice and the most useful oral medications available. They are a robust established approach to managing NDO (Level of evidence: 1a, Grade of recommendation: A).10 The rationale for treating NDO with antimuscarinic receptor antagonist is based on the fact that detrusor contractions are primarily mediated via muscarinic receptors, specifically subtype M2 and M3. Antimuscarinic agents are used to stabilize the detrusor, reducing its overactivity, making it moderately refractory to the parasympathetic stimulation. It leads to improved bladder compliance, reduction of symptoms, prevention of upper urinary tract damage and improvement of quality of life (Level of evidence: 1a, Grade of recommendation: A). As the patients suffering from NLUTS generally need a higher dose of anticholinergics than the patients with idiopathic detrusor overactivity, early discontinuation of the therapy due to adverse events is a potential drawback (Level of evidence: 1b, Grade of recommendation: A). Several antimuscarinic receptor antagonists have been investigated in the last three decades, and so far five antimuscarinic drugs (oxybutynin, trospium chloride, tolterodine, darifenacin and propiverine) have documented results on treating OAB in neurogenic populations. Oxybutynin chloride,11 tolterodine,12 darifenacin13 and propiverine14 are established effective medical treatments for NDO (Level of evidence: 1a, Grade of recommendation: A). Trospium chloride, a mixed antimuscarinic agent and a smooth muscle relaxant, is also a potential drug for neurogenic bladder management as it was shown to improve cystometric capacity and reduce incontinence episodes.15
These drugs are well tolerated and safe, even during long-term treatment. They have diverse tolerance profiles so that a different antimuscarinic agent may be prescribed if a patient experiences adverse effects or if the therapeutic effect is not sufficient.
Different ways of administration have also been proposed in order to overcome side effects from the oral route. In a selected group of patients transdermal oxybutynin was well tolerated and effective,16 and in other selected patients intravesical oxybutynin was able to abolish the bladder-cooling reflex17 (Level of evidence: 2a, Grade of recommendation: B).
There are other antimuscarinics, which are generally used and approved for the treatment of idiopathic OAB such as solifenacin and fesoterodine. There is scant experience with these compounds in SCI patients. Solifenacin has also been introduced for the management of NDO. Phase III study with solifenacin vs oxybutyninchloride vs placebo has been now completed in SCI patients and the data will be available soon. Fesoterodine and NDO has not been reported in literature. However, there is a trial in SCI patients currently in progress.
One of the most attractive fields of application in neurogenic patients is the combination of different antimuscarinic agents. A study by Amend and colleagues (2008)18 investigated whether a combination of antimuscarinic agents outperforms mono-therapy. Of the 27 patients included, 21 of them suffered from SCI, and they had previously been treated with double-dose antimuscarinic mono-therapy. They were split into three combination treatment groups: (i) tolterodine (8 mg)+oxybutynin (15–30 mg); (ii) trospium chloride (90 mg)+tolterodine (4–8 mg); (iii) oxybutynin (30 mg)+trospium chloride (45–90 mg). After 4 weeks of combination therapy, a significant decrease of incontinence events was observed (from seven to one events per day) and detrusor compliance as well as the bladder capacity improved. A combination of antimuscarinic agents was thus concluded to be an effective treatment strategy in patients who have failed with double-dose anticholinergeric mono-therapy.
Botulinum toxin(BTX)
BTX, a complex protein produced by the anaerobic bacterium, Clostridium botulinum, consists of several serum types (A, B, C, D and so on) and it was originally known only to cause serious, often fatal paralysis after ingestion with contaminated food. The BTX-linked neuromuscular blocking effect is hypothesized to alleviate muscle spasm because of excess neural activity of central origin. Local BTX injections are effective in the treatment of muscular disorders and unlicensed botulinum toxin A (BTXA) has been successfully used to treat NLUTS.19, 20, 21 BTX is thought to cleave SNAP-25, a synaptosome-associated protein, thereby blocking presynaptic acetylcholine release at the neuromuscular junction. This leads to temporary chemodenervation and muscle relaxation. In animal models, BTX inhibits abnormal urothelial release of ATP and calcitonine gene-related peptide, reduces capsaicin-evoked detrusor contractions and inhibits mucosal release of calcitonine gene-related peptide. Parasympathetic transmission inhibition is not the only BTX mechanism of action. It also inhibits substance P release and induces a blockade of mechanisms involved in transient receptor potential vanilloid-1 axonal expression. Apostolidis22 investigated the effect of BTXA therapy on human bladder afferent pathways, finding a progressive decrease in suburothelial fibers expressing P2X3 and transient receptor potential vanilloid-1, which correlates with clinical improvement but finds no change in urothelial sensory-receptor immunoreactivity.23 Clinical results have shown that BTXA is remarkably efficacious in NDO24, 25 when given as a single injection dose of 100–300 U of Botox or of 500–1000 U of Dysport (toxin equivalence is of 1 U Botox to 3.5–5 U Dysport); in an injection volume ranging from 0.1–0.5 ml per injection site. BTXA injection is usually performed using 20–40 evenly distributed intramural inject sites, sparing the trigone. However, two recent studies has reported successful outcomes using a Botox injection with trigone inclusion. Most studies used 300 U Botox, with isolated studies reporting the effects of 100, 150, 200 U. Despite of similar outcomes, the optimal dose has not yet been defined. The clinical benefit of BTXA injection seems to last for a mean of 6–9 months, apparently independently of population and dose. Side effects have been rare till date. Botox injections were repeated at different time intervals in almost all the studies and the efficacy was reported to continue in the majority of patients undergoing repeated injections. Hematuria and pain are the most frequent symptoms soon after injection. Systemic symptoms such as respiratory muscle weakness, extremity weakness and hyposthenia have occasionally been reported, but disappear within 4–5 weeks. Currently BTXA is being tested at phase III in North America and in Europe.26 Recently Del Popolo et al.26 demonstrated the long-term efficacy and safety and high level of patient satisfaction using 500 or 750 IU Dysport in patients who received repeated injections. Although many issues remain open and further research is mandatory, BTXA seems to represent an established safe and effective treatment in patients with SCI.27
Capsaicin-sensitive primary sensory nerves
Recently, the idea of afferent blockade by targeting afferent nerves that control the micturition reflex has gained the trust of urologists as a potential alternative to current drug therapies. The emerging concept is that it would be more desirable to block the micturition reflex that initiates overactive bladder, instead of blocking the contraction of detrusor smooth muscle. The concept of a therapeutic approach through the modulation of the afferent arm of the micturition reflex emerged when the investigators studied the effect of capsaicin on sensory nerves. Capsaicin targets the transient receptor potential vanilloid-1, which is expressed on small-to-medium size afferent neurons (most of C-type but also in a fraction of A-delta type). The acute exposure to capsaicin depolarizes and excites the sensory fibers expressing transient receptor potential vanilloid-1 receptors. This excitation is followed by a refractory period. The repeated, long-term, high-dose exposure to capsaicin desensitizes and ultimately damages the peripheral terminals, which become unresponsive. Desensitization is ‘a long lasting reversible suppression of sensory nerve activity and it is dependent on dose, time of exposure and interval between consecutive expositions’.6
The proof of concept that an inhibitory modulation of urinary bladder afferent nerves could achieve a therapeutic benefit in the treatment of bladder overactivity was obtained through the intravesical instillation of repeated low-concentration doses or single high-concentration doses of capsaicin. De Ridder et al.28 reported that repeated instillations of intravesical capsaicin were effective in approximately 80% of patients with bladder overactivity due to SCI and the beneficial effect lasted 3–5 years. At the end of the 1990s, Lazzeri et al.29 questioned the efficacy and the safety of capsaicin for management of detrusor hyperreflexia. Petersen et al.30 demonstrated in a placebo-controlled crossover study that intravesical treatment with capsaicin did not show beneficial effects on detrusor hyperreflexia and produced significant reactive changes in the bladder mucosa. Finally, Lazzeri et al.31 found that 12.96% of patients reported a significant episode of autonomic dysreflexia during the capsaicin instillation, 35.18% presented rhythmic detrusor contractions causing the leakage of 96% of patients with incomplete spinal lesion and bladder sensation reported a warm/burning/painful sensation. De Seze et al.32 found that the side effects were due not to the capsaicin itself, but to alcohol (the vehicle), which was used sometimes at the concentration of 30%. In their work, capsaicin in glucidic acid was equally effective with fewer side effects. As capsaicin was not a licensed agent its use was abandoned and replaced with pharmaceutically prepared resiniferatoxin (RTX). RTX is an ultra potent capsaicinoid obtained from a cactus species of the genus Euphorbia, Euphorbia resinifera. It is a thousand times more effective than capsaicin. Following early positive reports of its effectiveness in both NDO and idiopathic detrusor overactivity, clinical trials in Europe and the United States were initiated to examine the efficacy of the agent in both groups of patients.33, 34 The efficacy of RTX was demonstrated in 2002 by Giannantoni et al.35 in patients with neuropathic bladder secondary to SCI. RTX was shown to improve urodynamic parameters in patients with neurogenic bladder when compared with capsaicin.
Recently, 54 patients with detrusor overactivity who were refractory to anticholinergics were randomly treated with 4 weekly intravesical instillations of 10 nM RTX36 or vehicle. Three months after the treatment cycle a significantly higher percentage of patients receiving RTX had excellent and improved results; treatment remained effective at 6 months in 50% of patients. The authors concluded that multiple intravesical instillations of 10 nM RTX improved incontinence in patients with OAB. There was a lot of interest in these drugs, but no natural or synthetic vanilloid receptor agonist/antagonists are currently on the market. Although chemical denervation, by capsaicin or RTX, was proved to work in some setting, it remains an experimental alternative approach to the management of neurogenic OAB.
Nociceptin/Orphanin FQ—NOP receptor system
About 10 years ago, naturally occurring heptadecapeptide nociceptin/orphanin FQ (N/OFQ) was identified as the endogenous ligand of a previously orphan G-protein-coupled receptor now named N/OFQ peptide receptor. At peripheral levels, N/OFQ exerts potent inhibitory effects on primary afferent bladder fibers. A preliminary report and a subsequently randomized, placebo-controlled, double-blinded study demonstrated that intravesical instillation of 1 μM N/OFQ solution produces an acute inhibitory effect on the micturition reflex in humans.37, 38 In patients with NDO, Lazzeri et al.39 observed daily intravesical instillation of 1 mg of N/OFQ (but not placebo) is associated throughout the 10 day instillation period with less frequent incontinence episodes, increased bladder capacity and improved urodynamic parameters. Malaguti et al.40 performed the neurophysiological assessment of the nociceptive flexion reflex (NFR-RIII) in four healthy subjects and in five patients with lower urinary tract symptoms to investigate the N/OFQ neuronal site and functional mechanism of action. N/OFQ seems to selectively inhibit vesical sensory innervation in patients with lower urinary tract symptoms as it exerts a tonic inhibitory modulation of the nociceptive reflex, which is mediated by descending pathways. In healthy subjects N/OFQ modulation of the nociceptive reflex is not functionally active. These findings seem to provide evidence that N/OFQ and C-fibers are involved in the pathophysiology of lower urinary tract symptoms and make them attractive targets for new therapies.
The degenerin/epithelial Na+ channel (Deg/ENaC) family
The Deg/ENaC family represents a new class of cation channels that was discovered at the early 1990s.41 This cationic channel family is characterized by amiloride sensitivity, and is either constitutively active or activated by mechanical stimuli, and/or by ligands such as peptides or protons. Recent studies on these channels have implicated them in various sensory modalities, including the lower urinary tract. It has been reported that the Epithelial Na+ Channel (ENaC) expressed in the lower urinary tract epithelia.42 In rabbit bladder epithelium, ENaC is mechanosensitive, having the ability to change their sodium transport properties following changes in the hydrostatic pressure. The basal ATP release from the rabbit bladder epithelium is altered by amiloride, a blocker of ENaC.43 Intravesical instillation of amiloride reduces the frequency of reflex voiding during bladder filling in anesthetized rats, and stretch-evoked ATP release from bladder strips is largely diminished by amiloride.42 These indicate that ENaC expressed in the bladder epithelium is implicated in the mechanosensory transduction by controlling stretch-evoked ATP release. In the human bladder, the expression level of ENaC is extremely low, but it is markedly up regulated in SCI men (paraplegics) (del Popolo-Lazzeri, personal observation) and its expression level could correlate significantly with storage urinary symptoms.
The acid-sensing ion channel (ASIC), an H+-gated subgroup of the Deg/ENaC family, are encoded by three different subunit genes, ASIC1, ASIC2 and ASIC3, and the subunits form homo- and hetero-multimeric channels, which differ in their pH sensitivity and other pharmacological properties.44 In the central and peripheral nervous system, ASICs have emerged as key receptors for extracellular protons, and recent studies could suggest diverse roles for these channels in the physiology of mechanosensation and the pathophysiology of lower urinary tract pain.45 ASICs, especially ASIC1 and ASIC2, are abundantly expressed in the urothelium and detrusor muscle of mouse bladder.46 ASIC1 is a dominant subunit in the bladder mucosa, and both ASIC1 and ASIC2 are expressed in the bladder muscle. The expressions of ASIC2 and ASIC3 in the urothelium and suburothelial nerve plexus increase in cyclophospamide-induced cystitis, whereasASIC1 expression is not altered. Recent studies in the rat suggested that acid-induced Ca2+ influx and ATP release in the urothelium are partly attributed to ASIC activation.47 Roles of each ASIC subunit in sensory function are not well understood at present. So far nobody has investigated its expression in SCI patients and its changes after treatments, but these new channels might represent an attractive target for future drugs.
Conclusion
The neurogenic bladder has always represented the most dramatic dysfunction after SCI. Study of the mechanisms for central control and the complex structure of bladder wall has led to remarkable innovations in the treatment of detrusor overactivity. Thanks to early use, the development of inhibitors of detrusor contraction, mainly with efferent action, has improved the outcome of SCI patients. The new target for treatment is in the urothelium, therefore opening up new ways of treatment in the afferent pathway. Neurophysiological achievements seem to support a new hyper-afferent activity as the main changes in neurogenic bladder.7 Theoretically, it should be possible to delay the reflex voiding, increasing bladder capacity without interfering with the contractile phase during bladder emptying.
Antimuscarinic agents remain the first-line of choice for pharmacological treatment of neurogenic OAB. Antimuscarinic therapy increases bladder capacity and delays the initial urge to void. However, these agents fail to achieve the therapeutic goals in some patients and new interesting approaches have been investigated in the last few years. BTX seems to be very promising in treating neurogenic OAB, but other compounds are on the horizon. Newer agents and their possible applications in NDO, for example, the beta-3 agonists, centrally acting drugs such as amitriptyline and gabapentin, neurokinin receptor antagonists, PDE5 inhibitors and alpha blockers, could be considered.
Transition of promising basic science therapeutic principles to clinical practice are welcome, and emphasis on the creation of additional strategy mechanisms to provide an international trial infrastructure are needed. Without this infrastructure, basic science advances will only remain promising. SCI will obviously need multiple therapeutic modalities. However, physicians do play a key role in the management of lower urinary tract disease.
References
Go BK, DeVivo MJ, Richards JS . The epidemiology of spinal cord injury. In: Stover SI, DeLisa JA, Whiteneck GC (eds). Spinal Cord Injury: Clinical Outcomes from the Model Systems. Aspen Publishers: Gaithersburg, 1995, pp 21–51.
Andersson KE . Antimuscarinics mechanisms and the overactive detrusor: an update. Eur Urol 2011; 59: 377–9.
Blok BFM, Willemsen TM, Holstege G . A PET study on brain control of micturition in humans. Brain 1997; 120: 111–112.
Kuhtz-Buschbeck JP, Van Der Horst C, Pott C, Wolff S, Nabavi A, Jansen O et al. Cortical representation of the urge to void: a functional magnetic resonance imaging study. J Urol 2005; 174: 1477–1481.
Maggi CA, Meli A . The sensory efferent function of capsaicin-sensitive neurons. Gen Pharmac 1988; 19: 1–43.
Maggi CA, Meli A . The role of neuropeptides in the regulation of micturition reflex. J Auton Pharmacol 1986; 6: 133–162.
Lazzeri M, Spinelli M . The challenge of overactive bladder therapy: alternative to antimuscarinic agents. Int Braz J Urol 2006; 32: 620–630.
Birder L . Role of the urothelium in bladder function. Scand J Urol Nephrol Suppl 2004; 215: 48.
de Groat WC, Kawatani M, Hisamitsu T, Cheng CL, Ma CP, Thor K et al. Mechanisms underlying the recovery of urinary bladder function following spinal cord injury. J Auton Nerv Syst 1990; 30 (Suppl): 571–577.
Stöhrer M, Blok B, Castro-Diaz D, Chartier-Kastler E, Del Popolo G, Kramer G et al. EAU guidelines on neurogenic lower urinary tract dysfunction. Eur Urol 2009; 56: 81–88.
Stöhrer M, Murtz G, Kramer G, Schnabel F, Arnold EP, Wyndaele JJ . Propiverine compared to oxybutynin in neurogenic detrusor overactivity—results of a randomized, double blind, multicenter clinical study. Eur Urol 2007; 51: 235–242.
Reddy PP, Borgstein NG, Nijman RJM, Ellsworth PI . Longterm efficacy and safety of tolterodine in children with neurogenic detrusor overactivity. J Pediatr Urol 2008; 4: 428–433.
Novartis Pharmaceuticals Corporation. Darifenacin phase III studies. Data on file (Summary of Clinical Efficacy, EMEA version May 2003, sections 2, 7, 3, 2, 7, 4 2, 7, 3 and 2, 7, 4).
Madersbacher H, Mürtz G, Alloussi S, Domurath B, Henne T, Körner I et al. Propiverine vs oxybutynin for treating neurogenic detrusor overactivity in children and adolescents: results of a multicentre observational cohort study. BJU Int 2009; 103: 776–781.
Stöhrer M, Bauer P, Giannetti BM, Richter R, Burgdörfer H, Mürtz G . Effect of trospium chloride on urodynamic parameters in patients with detrusor hyperreflexia due to spinal cord injuries. A multicentre placebo controller double-blind trial. Urol Int 1991; 47: 138–143.
Kennelly MJ, Lemack GE, Foote JE, Trop CS . Efficacy and safety of oxybutynin transdermal system in spinal cord injury patients with neurogenic detrusor overactivity and incontinence: an open-label, dose-titration study. Urology 2009; 74: 741–745.
Van Meel TD, De Wachter S, Wyndaele JJ . The effect of intravesical oxybutynin on the ice water test and on electrical perception thresholds in patients with neurogenic detrusor overactivity. Neurourol Urodyn 2010; 29: 391–394.
Amend B, Hennenlotter J, Schäfer, Horstmann M, Stenzl A, Sievert KD . Effective treatment of neurogenic detrusor dysfunction by combined high-dose antimuscarinics without increased side-effects. Eur Urol 2008; 53: 1021–1028.
Schurch B, Stöhrer M, Kramer G, Schmid DM, Gaul G, Hauri D . Botulinum-A toxin for treating detrusor hyperreflexia in spinal cord injured patients: a new alternative to anticholinergic drugs? Preliminary results. J Urol 2000; 164: 692–697.
Schurch B, de Seze M, Denys P, Chartier-Kastler E, Haab F, Everaert K et al. Botulinum toxin A is a safe and effective treatment for neurogenic urinary incontinence: results of a single treatment, randomized, placebo controlled 6-month study. J Urol 2005; 174: 196–200.
Reitz A, Stohrer M, Kramer G, Del Popolo G, Chartier-Kastler E, Pannek J et al. European experience of 200 cases treated with botulinum-A toxin injections into the detrusor muscle for urinary incontinence due to neurogenic detrusor overactivity. Eur Urol 2004; 45: 510–515.
Apostolidis A, Popat R, Yiangou Y, Cockayne D, Ford AP, Davis JB et al. Decreased sensory receptors P2X3 and TRPV1 in suburothelial nerve fibers following intradetrusor injections of botulinum toxin for human detrusor overactivity. J Urol 2005; 174: 977–983.
Roosen A, Datta SN, Chowdhury RA, Patel PM, Kalsi V, Elneil S et al. Suburothelial myofibroblasts in the human overactive bladder and the effect of botulinum neurotoxin type A treatment. Eur Urol 2009; 55: 1440–1448.
Patel AK, Patterson JM, Chapple CR . Botulinum toxin injections for neurogenic and idiopathic detrusor overactivity: a critical analysis of results. Eur Urol 2006; 50: 684–709.
Kalsi V, Apostolidis A, Popat R, Gonzales G, Fowler CJ, Dasgupta P . Quality of life changes in patients with neurogenic versus idiopathic detrusor overactivity after intradetrusor injections of botulinum neurotoxin type A and correlations with lower urinary tract symptoms and urodynamic changes. Eur Urol 2006; 49: 528–535.
Del Popolo G, Filocamo MT, Li Marzi V, Macchiarella A, Cecconi F, Lombardi G et al. Neurogenic detrusor overactivity treated with English botulinum toxin A: 8-year experience of one single centre. Eur Urol 2008; 53: 1013–1020.
Lazzeri M . Botulinum toxin A and lower urinary tract symptoms: non multa, sed multum (not many, but much). Eur Urol 2009; 55: 59–61.
De Ridder D, Chandiramani V, Dasgupta P, Van Poppel H, Baert L, Fowler CJ . Intravesical capsaicin as a treatment for refractory detrusor hyperreflexia: a dual center study with long-term follow-up. J Urol 1997; 158: 2087–2092.
Lazzeri M, Spinelli M, Beneforti P, Zanollo A, Turini D . Urodynamic assessment during intravesical instillation of capsaicin for the treatment of refractory detrusor hyperreflexia. Spinal Cord 1999; 37: 440–443.
Petersen T, Nielsen JB, Schroder HD . Intravesical capsaicin in patients with detrusor hyperreflexia: a placebo-controlled cross-over study. Scand J Urol Nephron 1999; 33: 104–110.
Lazzeri M, Spinelli M, Zanollo A, Turini D . Intravesical vanilloids and neurogenic incontinence: ten years experience. Urol Int 2004; 72: 145–149.
de Seze M, Wiart L, de Seze MP, Soyeur L, Dosque JP, Blajezewski S et al. Intravesical capsaicin versus resiniferatoxin for the treatment of detrusor hyperreflexia in spinal cord injured patients: a double-blind, randomized, controlled study. J Urol 2004; 171: 251–255.
Lazzeri M, Beneforti P, Turini D . Urodynamic effects of intravesical resiniferatoxin in humans: preliminary results in stable and unstable detrusor. J Urol 1997; 158: 2093–6.
Lazzeri M, Spinelli M, Beneforti P, Zanollo A, Turini D . resiniferatoxin for the treatment of detrusor hyperreflexia refractory to capsaicin in patients with chronic spinal cord diseases. Scand J Urol Nephrol 1998; 32: 331–334.
Giannantoni A, Di Stasi SM, Stephen RL, Navarra P, Scivoletto G, Mearini E et al. Intravesical capsaicin versus resiniferatoxin in patients with detrusor hyperreflexia: a prospective randomized study. J Urol 2002; 167: 1710–1714.
Peng CH, Kuo HC . Multiple intravesical instillations of low-dose resiniferatoxin in the treatment of refractory interstitial cystitis. Urol Int 2007; 78: 78–81.
Lazzeri M, Calò G, Spinelli M, Guerrini R, Beneforti P, Sandri S et al. Urodynamic and clinical evidence of acute inhibitory effects of intravesical nociceptin/orphanin FQ on detrusor overactivity in humans: a pilot study. J Urol 2001; 166: 2237–2240.
Lazzeri M, Calò G, Spinelli M, Guerrini R, Salvadori S, Beneforti P et al. Urodynamic effects of intravesical nociceptin/orphanin FQ in neurogenic detrusor overactivity: a randomized, placebo-controlled, double-blind study. Urology 2003; 61: 946–950.
Lazzeri M, Calo G, Spinelli M, Malaguti S, Guerrini R, Salvadori S et al. Daily intravesical instillation of 1 mg nociceptin/orphanin FQ for the control of neurogenic detrusor overactivity: a multicenter, placebo controlled, randomized exploratory study. J Urol 2006; 176: 2098–2102.
Malaguti S, Spinelli M, Citeri M, Lazzeri M . Nociceptin/Orphanin FQ (N/OFQ) modulates the bladder pain in humans. Neurophysiological evidence by nociceptive flexion (RIII) reflex analysis. Eur Urol (Suppl) 2007; 6: 167.
Kellenberger S, Schild L . Epithelial sodium channel/degenerin family of ion channels: a variety of functions for a shared structure. Physiol Rev 2002; 82: 735–767.
Du S, Araki I, Mikami Y, Zakoji H, Beppu M, Yoshiyama M et al Amiloride-sensitive ion channels in urinary bladder epithelium involved in mechanosensory transduction by modulating stretch-evoked adenosine triphosphate release. Urology 2007; 69: 590–595.
Ferguson DR, Kennedy I, Burton TJ . ATP is released from rabbit urinary bladder epithelial cells by hydrostatic pressure changes-a possible sensory mechanism? J Physiol 1997; 505: 503–511.
Kellenberger S, Schild L . Epithelial sodium channel/degenerin family of ion channels: a variety of functions for a shared structure. Physiol Rev 2002; 82: 735–767.
Wemmie JA, Price MP, Welsh MJ . Acid-sensing ion channels: advances, questions and therapeutic opportunities. Trends Neurosci 2006; 29: 578–586.
Kobayashi H, Yoshiyama M, Zakoji H, Takeda M, Araki I . Sex differences in expression profile of acid-sensing ion channels in the mouse urinary bladder: a possible involvement in irritative bladder symptoms. BJU Int 2009; 104: 1746–1751.
Corrow K, Girard BM, Vizzard MA . Expression and response of acid-sensing ion channels (ASICs) in urinary bladder to cyclophosphamide (CYP)-induced cystitis. Am J Physiol Renal Physiol 2010; 298: F1130–F1139.
Acknowledgements
We would like to thank Amy Sussman, who revised the linguistic style of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Spinal Cord website
Supplementary information
Rights and permissions
About this article
Cite this article
del Popolo, G., Mencarini, M., Nelli, F. et al. Controversy over the pharmacological treatments of storage symptoms in spinal cord injury patients: a literature overview. Spinal Cord 50, 8–13 (2012). https://doi.org/10.1038/sc.2011.110
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.110
Keywords
This article is cited by
-
Long-Term Urologic Evaluation Following Spinal Cord Injury
Current Bladder Dysfunction Reports (2016)
-
The possible role of percutaneous tibial nerve stimulation using adhesive skin surface electrodes in patients with neurogenic detrusor overactivity secondary to spinal cord injury
International Urology and Nephrology (2015)
-
Are oxybutynin and trospium efficacious in the treatment of detrusor overactivity in spinal cord injury patients?
Spinal Cord (2014)
-
Neurogenic Bladder: from Diagnosis to Management
Current Urology Reports (2014)
-
OnabotulinumtoxinA (Botox®): A Review of its Use in the Treatment of Urinary Incontinence in Patients with Multiple Sclerosis or Subcervical Spinal Cord Injury
Drugs (2014)