Abstract
Study design:
The purpose of this study was to explore the changes in pelvic floor muscle tension at different times after suprasacral spinal cord injury (SS) and sacral cord injury (SC), and learn more about pelvic floor dysfunction (PFD) after spinal cord injury (SCI).
Method:
A total of 70 healthy female Sprague–Dawley (SD) rats, weighing between 250 and 280 g, were randomly divided into seven groups with 10 rats in each group, which included five SS groups (3 days and 2, 4, 8 and 12 weeks after injury), one SC group (4 weeks after injury) and one normal group. Muscle tension, including muscle compliance, and contraction activity elicited using electrostimulation under two initial lengths were measured at different time points.
Results:
(1) Muscle compliance decreased within 4 weeks in the SS group (P>0.05), began to increase at 8 weeks (P<0.05) and reached the peak at 12 weeks, which were all lower than the normal level; (2) contraction activity under both initial lengths tended to decrease within 4 weeks, peak at 8 weeks (P<0.05) and decline again at 12 weeks , which were all lower than that of the normal group as well; and (3) the SC group showed similar compliance with the normal group (P>0.05) and less contraction activity when compared with other SS groups (P<0.05).
Conclusion:
Measurement for the compliance and contraction activity of pubococcygeus indicates the changes from decreasing to increasing after suprasacral cord injury, and similar compliance combined with rather low contraction activity compared with the normal group after sacral cord injury, both of which are in accordance with PFD after spinal cord injury.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a serious central neurological disorder with incurable complications, such as paralysis, pain, spasm and dysfunction, especially in excretory function, which hinder patients from partaking in social activities in a normal manner. Much effort has been made to reconnect the impaired spinal cord, including stem cell transplant,1, 2, 3 nerve transferring,4 functional electrical stimulation5 and brain–computer interface,6 which has brought much hope for their recovery. However, much more work needs to be carried out to accomplish complete recovery of distal spinal cord; therefore, trying to protect the organ and tissue below the injury level, especially treating pelvic floor dysfunction (PFD), seems to be rather important.
A few studies on PFD after suprasacral cord injury have reported on abnormal muscle tension; however, incontience, constipation and sexual function disorder, as shown in PFD, were closely related to the abnormality of pelvic floor tension. Increased external sphincter tension was related to detrusor-sphincter dyssynergia; spasm of levator ani leads to high resistance for defecation7 and constipation; and abnormal tension in erector clitoridis tends to cause mentulagra and prolonged erection.8 We believe that muscle tension could have an important role in the normal function and dysfunction of the pelvic floor. For the treatment and rehabilitation of PFD after SCI, the first step to be taken is the clarification of muscle tension and its changes.
Our research aims to explore the changes in pubococcygeus tension and its contraction activity on Sprague–Dawley (SD) rats at different times after SCI, and to compare the differences at 4 weeks after injury between suprasacral cord injury (SS) and sacral cord injury (SC) to provide more evidence for research on PFD after SCI.
Materials and methods
A total of 70 healthy adult SD female rats, weighing between 250 and 280 g, were fed for 1 week before they were used as spinal cord injury models.
Spinal cord injury models
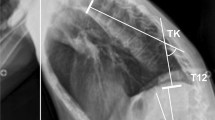
To anesthetize SD rats, 4% chloral hydrate was intraperitoneally injected into their abdominal cavity (300 mg kg–1). The rat was then fixed by limbs and head on the operation table in a prone position. Locating the T9–T10 (SC group at L3–4) spinous process according to the T2 level, using an operating microscope, the spinous process and vertebral plate were excisioned. The spinal cord was gently pulled out around the dura through the anterior part of the vertebral canal using medullary groove while protecting the vessel in the vertebral canal. The blood flow from the incisions to the spinal cord and its dura was simultaneously stanched using microscissors, and hemostasis was attained locally using jelly sponge and bipolar electrocoagulation if necessary. After the operation, the rats were placed in single cages, kept warm and swiftly injected with 5% GNS 5 m1 subcutaneously. Forage (5 g) and penicillin (0.25 ml) were given to each rat twice a day after they recovered from anesthesia 8 h later. Urine was expressed manually every 8 h per day for 4 weeks until the neurogenic bladder was formed (and for 1 week in the SC group).
Apparatus
Creature function measurement system BL-420F (Taimeng, Chengdu, China) was used to measure muscle tension, and data were shown through a computer screen in real time. A steel hood connected the muscle to force sensing, which was used to input the muscle tension signal into the system.
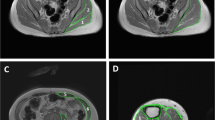
Locating the pelvic floor muscle
To anesthetize SD rats, 4% chloral hydrate was intraperitoneally injected into the abdominal cavity (300 mg kg–1), and the rats were fixed by limbs and head onto the operation table in a supine position. After preparing the skin along the pelvic outlet in the perineal region, skin of approximately 1 cm to the anus lateral margin was sheared using curved scissors, subcutaneous tissue was bluntly dissected using hemostatic forceps and the pubococcygeus was located. After the connective tissue behind it was continually dissected, this muscle, which was approximately 1 cm in diameter and shaped in the form of a circular cylinder, was exposed (see Figure 1).
Measurement of muscle tension in vivo
The muscle was isolated from deep connective tissue, a steel hook was used to link the muscle to force sensing and an inelastic suture silk of approximately 10 cm was used to connect them, which is parallel to the horizontal plane. Tonic data could be viewed on the screen in real time.
The preload was modulated to 1 g on the suture silk for 3 s, and the silk was dragged at a certain speed for 0.5 cm s–1 for 1 s. The tonic on the suture silk was observed and recorded as muscle compliance.
After 5 min, two acupuncture needles were pricked into the muscle belly, which linked the electric current output interface. The electricity parameter was set: constant, square wave, 10 Hz; 50 ms; 3 V. The precondition set was the same as the compliance part of 1 g preload; thereafter, electrical stimulation was administered for 3 s to observe the tonic change. After 3 min, the preload was changed by dragging the suture silk approximately 0.5 cm s–1 for 3 s, and then electrical stimulation was administered on the muscle and tension changes were recorded. This was regarded as muscle contraction activity (see Figures 2 and 3).
Statistical method
One-way analysis of variance was used to compare the pre- and postresults, and the difference between groups was analyzed using the Tukey method in multiple comparisons. The significance level was set as 0.05.
Statement of ethics
The animal experiments were authorized by the animal ethics committee of Capital Medical University in Beijing, China, and license was obtained for animal feeding and experiments.
Results
Muscle compliance and contraction activity were measured at different time points (3 days, and 2, 4, 8 and 12 weeks) after suprasacral cord injury and 4 weeks after sacral cord injury. Both compliance and contraction activity resulted in changes in tension, from peak value to initial value. Contraction activity included tension changes under optimal initial length and prolonged length. All results are shown in Table 1.
Compliance
Compliance is used to evaluate the physical traits of the muscle. In this study, we found that muscle compliance tended to decrease within 4 weeks (P>0.05), whereas 4 weeks later, compliance obviously increased (P<0.05) and reached maximal value at week 8. The results of different time points and different levels are shown in Tables 2 and 3.
Contraction activity
Contraction activity under optimized initial length and prolonged length showed similarities: tension changes tended to decrease within 4 weeks and increased 4 weeks later, peaked at week 8 and decreased to some extent at week 12, which were lower than those of the normal group. The SC group showed a much lower value under both lengths than did the normal group (Tables 4, 5, 6 and 7).
Discussion
Spinal shock after SCI is always accompanied by hypotonia of striated muscle in the pelvic floor that is innervated by spinal conus, but when the spinal shock passes, muscle tension tends to increase gradually with functional recovery of the caudal spinal cord, even to clasp-knife rigidity in the extremity, which is regarded as spastic paralysis.
Until now, few researches about pelvic floor muscle tension after SCI have been reported. Most studies on the pelvic floor muscle focus on bulbospongiosus and ischiocavernosus related to sexual dysfunction after SCI,8 whereas no systematic researches on the levator ani muscle have been reported. Actually, levator ani muscle has an important role in puborectum angular shaping, urination and defecation controlling. Spasms of levator ani and urethrae external sphincter tend to induce bladder outlet obstruction, relating to detrusor-sphincter dyssynergia, and abnormal pelvic floor tension hinder defecation, cause constipation and even autonomic dysreflexia.
Using a rat model of SCI at different time points, this research shows the tension traits of pubococcygeus for a better understanding of PFD after SCI. Muscle fibers can obtain two kinds of load in in vivo and experimental conditions. One is the preload, which is set before muscle contraction and makes the muscle maintain a certain length before contraction; this length is also called the initial length. Another load is the afterload, which is set on fiber after muscle contraction, and will hinder muscle fiber shortening during contraction. It is generally believed that muscle tension is related to (preload) initial length, afterload and contractibility of the muscle itself. When the pre- and postload is maintained, tension changes should be caused only by changes in muscle contractibility. In this study, we set up preload at 1 g and treated it as the optimal initial length, and extended the muscle fiber in the same speed for the same length to standardize the afterload. Under this condition, we believe that all tension changes are caused by the different contractibility activities of the muscle itself.
Ditunno9 proposed a four-phase theory for spinal shock.9 Phase I is characterized by a complete loss or weakening of all reflexes below the SCI, which lasts for 1 day. Phase II occurs over the next 2 days, and is characterized by the return of some polysynaptic reflexes below the SCI, such as the bulbocavernosus reflex. Phases III and IV are characterized by hyperreflexia or abnormally strong neural reflexes, usually produced by minimal stimulation. In phase I, neurons that are distal to the injury level lose the basal level of excitatory from the brain and become hyperpolarized, and therefore less responsive to stimuli. In phase II, restoration of reflexes is polysynaptic in nature, which relates to hypersensitivity of reflex muscles after denervation, and more receptors for neurotransmitters are expressed. During phases III and IV, interneurons and lower motor neurons below the SCI begin sprouting, attempting to reestablish synapses. In this study, the pelvic floor muscle is innervated by the pudendal nerve, which belongs to the mono- and polysynaptic reflex. Muscle tension tends to rise obviously after 4 weeks, and continues to increase at 8 and 12 weeks, which is consistent with the theory of Ditunno.9 As the period between 4 and 8 weeks is a little longer, it may be more persuasive to observe the tension at weeks 5 and 6.
Muscle compliance is a kind of physical trait, and muscle mechanics should include muscle response after electrical stimulation to indicate its physiological or contraction activity. To observe the muscle contraction activity at different time points after SCI, this research designed electrical stimulation under two initial lengths. Electrical stimulation can be commonly divided into single stimulus and continued stimulus, in which the continued mode is closer to normal conditions. After the pilot study, 10 Hz and 3 V electrical stimulation has been proven to induce the pubococcygeus complete tetanus, which is most similar to the normal mode of muscle contraction. In this research, contraction activity under both initial lengths is found to decrease gradually within 4 weeks, which is thought to be related to hyperpolarization of the motor neuron and therefore less responsive to stimuli.9 Besides that, lack of trophic action may be another reason for the decrease in contraction activity in the spinal shock period. However, the 8-week contraction activity under the two lengths indicates significant increment compared with the normal level, which is in accordance with muscle compliance results. The sprouting of interneurons and lower motor neurons below the SCI to re-establish synapses is believed to be the main reason, and stimulation irritates the muscle and produces its contraction. However, at week 12, contraction activity under both lengths decreases, which is different from compliance results, and monosynaptic hyperreflexia and changes in the muscle itself may be the other reason. In our research, the morphological part has proved that desmoplasia and breakage of sarcomere at week 12 are worse than those at week 8. Another reason for this could be that serious hyperplasia of connective tissue decreases both muscle compliance and contraction activity.
After suprasacral injury, α-motoneuron reflex circle innervating the pelvic floor muscle maintains its integrity for the muscles to get trophic action from the neural system to some extent and not show obvious atrophy. However, sacral cord injury, either anterior horn cell or nerve root injury, is a direct injury to lower motoneurons, resulting in serious muscle atrophy that leads to loss of neural trophic action. In this research, the difference in compliance between the SS and SC groups at 4 weeks was compared, and compliance of the SC group was a little higher than that of the SS group (P>0.05). It is estimated that the higher compliance is related to the hyperplasticity of connective tissue. Compliance is merely a kind of indication of the physical trait, and not enough to explain muscle physiological changes; therefore, combining muscle contraction activity results was more meaningful.
Contraction activity in the SS group under both lengths was much higher than that in the SC group. But contraction activity in the SC group was very little, especially in the optimized initial length. Loss of trophic action from the neural system must be an important reason, and serious dissolved sarcomere and hyperplasia connective tissue in muscle itself should be another aspect.
For the study of PFD, it is valuable to learn the trait of the pelvic floor muscle. This research pertains to the compliance and contraction activity of the pelvic floor muscle, which makes us realize the changes in muscle in the pelvic floor, combined with PFD. In the clinical treatment of PFD, the effective method to modify the pelvic floor muscle would be an important option for SCI patients.
References
Dasari VR, Spomar DG, Li L, Gujrati M, Rao JS, Dinh DH . Umbilical cord blood stem cell mediated downregulation of fas improves functional recovery of rats after spinal cord injury. Neurochem Res 2008; 33: 134–149.
Coutts M, Keirstead HS . Stem cells for the treatment of spinal cord injury. Exp Neurol 2008; 209: 368–377.
Bambakidis NC, Butler J, Horn EM, Wang X, Preul MC, Theodore N et al. Stem cell biology and its therapeutic applications in the setting of spinal cord injury. Neurosurg Focus 2008; 24: E20.
Keith MW, Kilgore KL, Peckham PH, Wuolle KS, Creasey G, Lemay M . Tendon transfers and functional electrical stimulation for restoration of hand function in spinal cord injury. J Hand Surg [Am] 1996; 21: 89–99.
Kirsch R . Development of a neuroprosthesis for restoring arm and hand function via functional electrical stimulation following high cervical spinal cord injury. Conf Proc IEEE Eng Med Biol Soc 2005; 4: 4142–4144.
Turner JA, Lee JS, Martinez O, Medlin AL, Schandler SL, Cohen MJ . Somatotopy of the motor cortex after long-term spinal cord injury or amputation. IEEE Trans Neural Syst Rehabil Eng 2001; 9: 154–160.
Shafik A . The role of the levator ani muscle in evacuation, sexual performance and pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct 2000; 11: 361–376.
Nout YS, Schmidt MH, Tovar CA, Culp E, Beattie MS, Bresnahan JC . Telemetric monitoring of corpus spongiosum penis pressure in conscious rats for assessment of micturition and sexual function following spinal cord contusion injury. J Neurotrauma 2005; 22: 429–441.
Ditunno JF, Little JW, Tessler A, Burns AS . Spinal shock revisited: a four-phase model. Spinal Cord 2004; 42: 383–395.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lu, Z., Li, J., Liao, L. et al. Changes in pubococcygeus muscle tension in the pelvic floor of rats after spinal cord injury. Spinal Cord 48, 464–469 (2010). https://doi.org/10.1038/sc.2009.169
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.169