Abstract
Study design:
Case report.
Objective:
Complications in spinal cord injury (SCI) are a challenging problem for the patients and often difficult to manage. Three cases of spondylodiscitis, localized at the lumbosacral junction in long-term paraplegic patients are presented.
Setting:
Spinal Cord Injury Center, Orthopaedic University Hospital Heidelberg, Heidelberg, Germany.
Clinical presentation:
In all three cases, neurological deterioration (ASIA A) was caused by a secondary compression of the spinal cord at the lumbosacral spine. Increase of spasticity and pain, atonic bladder and sphincter function accompanied by vegetative symptoms were present in all patients. Microbiological analysis of the sacral area showed coagulase negative staphylococcus in two cases, whereas in one case no microorganism was found. The diagnosis was made by MRI of the whole spine and surgical treatment was required. At follow-up (6 months), patients showed no AIS (ASIA Impairment Scale) changes.
Conclusion:
If neurological deterioration occurs, spondylodiscitis should be ruled out in paraplegic individuals. The therapeutic goal is to achieve emergent decompression of the spinal cord and to administrate adequate antibiotic therapy to avoid a neurologically complete situation.
Similar content being viewed by others
Introduction
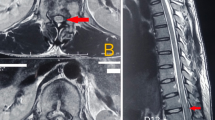
Spondylodiscitis is the third most common bone infection in adults with preferential site at the lumbar spine. Primary focus of infection constitutes decubitus ulcers, urogenital infections, pulmonary infections, endocarditis or catheter-associated infections.1 Urogenic inflammation causing spondylodiscitis are often underestimated in their frequency of occurrence and severity of symptoms.2 Decubitus ulcers and urogenital infections are the most common complications in paraplegic patients and associated with severe problems for the patient and his environment.3 We report the unspecific clinical picture and the course of spondylodiscitis at the lumbosacral spine in three chronic incomplete paraplegic patients, who were treated at our institution from 2000 to 2007 (Figures 1 and 2).
(a) Incomplete sensorimotor paraplegia below T3 after traumatic T2–3 fracture 27 years ago. (b) CT shows pseudarthrosis L5/S1 with osteolytic zones at the lumbosacral area. (c) Scintigraphy with enhancement at the pelvis and lumbar spine. (d) Postoperative formation of seroma ( → ) after dorsal stabilization S1/2 using autograft from the iliac crest.
Case report
This study shows three chronically initially incomplete paraplegic patients who developed lumbosacral spondylodiscitis as a possible long-term complication (Table 1). Patients had been paraplegic for 12–27 years and comorbidities associated with paraplegia constituted decubitus, periarticular ossifications, refluxnephropathy, recurrent urogenital infections and ascending syringomyelie. In all cases neurological deterioration (ASIA A) was caused by an additional compression of the cauda equina. An increase in spasticity and pain, vegetative symptoms, an emerging atonic bladder and atonic sphincter tonus was noted. Laboratory examination showed normal leukocytes and elevated CRP in two cases. Fever was evident in one case. In two cases coagulase negative staphylococcus was isolated and in one case no microorganism was found. Coagulase negative staphylococcus was confirmed in the biopsy of affected bony structures or tissue in each of the two cases (case 1 and 2).
Spondylodiscitis with a paravertebrally located abscess formation was diagnosed with MRI of the whole spine in all patients. Surgical treatment via posterior approach was carried out in all three cases, whereas the posterior and anterior structures (case 1: osteodiscectomy S1/2, case 2: vertebra L5/S1 and discectomy L5/S1, case 3: complete resection of the os sacrum) were removed and drainage of the para- and praevertebral abscess was performed. The patients reported on improvement of pain and were mobilized in the wheelchair. Antibiotic medication was continued for 12 weeks postoperatively. At follow-up after 6 months the ASIA Impairment Scale remained unchanged. No further relapse of spondylodiscitis had been noted.
Discussion
Malignant tumours (skin and bladder tumours), pulmonary, cardiovascular and urogenital diseases are common causes of deaths in long-term paraplegic patients.3 Frequent and alternating antibiotic therapies can aggravate immunosuppression and select for resistant microorganisms. Furthermore, malnutrition, nicotin abusus and intestinal dysfunction in paraplegic patients result in an increased sensitivity to complications.4 Chronical skin lesions result in a loss of proteins, electrolytes and general immunosuppression. Furthermore, bacteria can easily contaminate the adjacent bony structures of the spine or the hip. Without an adequate treatment of the potential infectious focus, a vicious circle may lead to infection or even seeding. Spondylodiscitis is a rare disease with unspecific primary symptoms. For this reason therapy often starts after a certain delay.5 The large spectrum of possible differential diagnosis in paraplegic patients is a medical challenge because of vegetative unspecific symptoms. Similar to non-paraplegic patients the isolation of a microorganism is still a problem with regard to frequent and alternating antibiotic therapy.
Coagulase negative staphylococcus has less virulent factors than staphylococcus aureus and often comes across immunocompromised patients.
In paraplegic patients we recommend MRI of the whole spine to rule out possible differential diagnosis like tumours, syringomyelie or tethered cord syndrome (Table 2).
If acute neurological deterioration in paraplegic patients occurs, spondylodiscitis as a rare, but possible differential diagnosis should be excluded. The therapy is in accordance to the approach in normal patients including dorsal decompression of the spinal canal, ventral drainage of the infectious focus and dorso (ventral) stabilization. In cases of complete affection of the os sacrum, resection can be indicated. Concomitant adequate antibiotic therapy is obligatory.
Conflict of interest
The authors declare no conflict of interest.
References
Huttner B, Opravil M . Die infektiöse Spondylitis. Z Rheumatol 2006; 65: 7–11.
Renker EK, Möhring K, Abel R, Carstens C, Wiedenhöfer B, Lehner B et al. Urogenic spondylodiscitis. Orthopade 2009; 38: 355–364.
Frankel HL, Coll JR, Charlifue SW, Whiteneck GG, Gardner BP, Jamous MA et al. Long-term survival in spinal cord injury: a fifty year investigation. Spinal Cord 1998; 36: 266–274.
McKinley W, Jackson A, Cardenas D, DeVivo M . Long-term medical complications after traumatic spinal cord injury: A regional model system analysis. Arch Phys Med Rehabil 1999; 80: 1402–1409.
Asamoto S, Doi H, Kobayashi N, Endoh T, Sakagawa H, Iwanaga Y et al. Spondylodiscitis: diagnosis and treatment. Surg Neurol 2005; 64: 103–108.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Putz, C., Akbar, M., Wiedenhöfer, B. et al. Clinical presentation of spondylodiscitis as a long-term complication in incomplete paraplegia: a report of three cases. Spinal Cord 48, 779–782 (2010). https://doi.org/10.1038/sc.2009.154
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.154