Abstract
Background:
Pressure ulcers (PUs) are a common complication following a spinal-cord injury (SCI). Good prevention requires identifying the individuals at risk for developing PUs. Risk assessment scales used nowadays were designed on pathophysiological concepts and are not SCI-specific. Recently, an epidemiological approach to PU risk factors has been proposed to design an SCI-specific assessment tool. The first results seem quite disappointing, probably becuase of the level of evidence of the risk factors used.
Objective:
To determine PU risk factors correlated to the patients with SCI, medical care management during the acute as well as in the rehabilitation and chronic stages. This first part focuses on identifying the risk factors during the acute and rehabilitation stages.
Materials and methods:
Systematic review of the literature.
Results:
Six studies met our inclusion criteria. The risk factors during the acute stage of an SCI are essentially linked to care management and treatment modalities. There is insufficient evidence to make a recommendation on medical risk factors, except for low blood pressure on admission to the Emergency Room, with a moderate level of evidence. Regarding the rehabilitation stage, no study was deemed relevant.
Discussion and conclusions:
Additional observational studies are needed, for both the acute and rehabilitation stages, to improve this level of evidence. However, this systematic review unveiled the need for a carefully assessed t care management and the related practices, especially during the acute stage of an SCI.
Similar content being viewed by others
Introduction
Acute spinal-cord injury (SCI) is a traumatic event that can quickly affect the patient's vital prognosis. In the two decades following World War II, emergency medicine and intensive medical care have improved vastly with a positive impact on the vital prognosis for an acute SCI injury. The patient's life expectancy increased along with the development of physical medicine and rehabilitation, allowing a better management of urinary and sphincter disorders.1, 2
Pressure ulcers (PUs) are now the most common complication for patients with SCI,3, 4 despite the large number of recommendations available5, 6 for information and prevention, and the technological progresses made for preventing and treating PU. PU has become the second cause of rehospitalization after an SCI,7 with estimated annual costs amounting to 1.4 billion dollars in the United States.8
To set up a PU prevention programme for the SCI population, we need to assess correctly the PU risk factors to identify the patients who could benefit from an intensive prevention training programme on PU management.
The main risk assessment scales used in hospitals or for the chronic group (at home) are the Braden, Norton and Waterlow scales. These scales were designed 20–30 years ago on the basis of the following main pathophysiological PU factors: pressure, friction, shearing, incontinence, nutrition and immobility. They identified at-risk patients within a heterogeneous population of hospitalized patients. The results collected from the patients with SCI are more limited, all patients being labelled ‘at risk’ for developing PUs.9
Salzberg et al.10, 11, 12 reviewed the PU risk factors using an epidemiological approach to the pathophysiological factors. For this, they differentiated different successive stages of the medical care for the patients with SCI to identify the specific risk factors for this population. This led to the design of a risk assessment scale for acute SCI (SCIPUS-A), and one for chronic SCI (SCIPUS). Since their original publication, the metrological values of these two scales have not been sufficiently tested to set clinical practice recommendations.13 Furthermore, an independent study reports no significant differences between SCIPUS-A, Braden, Norton and Waterlow scales for acute SCI.14 Since then, new epidemiological studies focusing on patients with SCI have brought up new additional risk factors15 that can probably explain the lack of validity
The main objective of this systematic literature review is to determine the current state of knowledge on PU risk factors for the successive stages of the medical care for the patients with SCI.
In this review, we will deal with the risk factors observed during the acute and rehabilitation stages of an SCI.
Materials and methods
The methodology used for our review was conducted according to the recommendations from the Cochrane Library.16
Inclusion criteria
Cross-sectional, case–control and cohort studies are included in this review. Basic research, case reports and case series have been excluded. Only articles assessing potential PU risk factors in patients with SCI have been kept. There were no language restrictions.
The group studied must be made up of patients with SCI, paraplegics or tetraplegics, at the acute or chronic SCI stages, at home or in the hospital, regardless of the aetiology. Studies on the basis of groups not exclusively made up of patients with SCI were excluded, similar to studies focusing on SCI patients with a PU, but without a control group.
The presence of PU was the ‘PU’ variable taken into account. We assessed whether the evaluation was a clinical one, through a questionnaire or directly from the patient's medical records and the PU classification used.
There was no restriction as to the type of risk factor studied.
Bibliographical research strategy
We have searched the following databases between the start date (listed next to the name of the database) and March 2008: Medline (1966), Embase (1980), Pascal (1990) and Reedoc (1977). The research keywords were either terms extracted from the thesaurus (Mesh Dictionary for Medline) or terms appearing in the text or in the title (free words). They were combined in as many stages as necessary with the use of the connector words ‘and’, ‘or’ and ‘except’ (see Appendix 1).
Several Grey Literature databases were searched as well, such as the British Columbia Environmental and Occupational Health Research Network, The New York Academy of Medicine and UNM Health Sciences Library.
We also did a manual review of journals available in our University Library that routinely publishes articles on paraplegia or PU (Paraplegia, 1977–1978 and 1983–996; Spinal Cord, -1997–2008, Archives of Physical Medicine and Rehabilitation, 1980–2008; American Journal of Physical Medicine, 1980–1987; American Journal of Physical medicine and Rehabilitation, 1988–1995; Annales de Réadaptation et de Médecine Physique, 1983–2008 and Topics in Spinal Cord Medicine, 1995–2008; Wounds, 1995–2008; Journal of Wound Care, f1999–2008 and Advances in Skin and Wound Care, 2001–2008).
We reviewed the bibliographical references of the selected articles and the literature reviews on this topic.
There were no language restrictions in the bibliographical research.
Review process
Selection of articles
At the first reading, the titles and abstracts allowed us to select potentially eligible studies by discarding non-relevant articles.
Second, all potentially eligible studies were examined thoroughly and selected on the basis of previously established inclusion criteria. The selection of articles was carried out by one reader (AG).
Data extraction and methodological quality evaluation
The studies meeting the inclusion criteria were analysed by two readers (AG and AD), using a standardized reading tool as described by Macfarlane et al.17 This reading tool included study type, selected population, data collecting mode, definition of the analysed variables, statistical analysis used, and results and bias. The criteria were scored ‘yes’ or ‘no’ or ‘unable to determine.’ Positively scored criteria were added to reach a total quality score. Quality score results were expressed as percentages of the total attainable score. Data extraction and quality assessment were not conducted with blinded details and results, as there is no evidence that blinding leads to a decrease in bias for a systematic review.18 Afterwards, the two readers compared their evaluations and discussed any discrepancies or conflict of opinion.
Data analysis and level of evidence staging
The studies were grouped into three batches according to the SCI stage. The first batch for the acute stage (acute SCI), defined as the stage before the patient's admission into a rehabilitation centre (prehospital care, neurosurgery or emergency care). The second batch for the physical medicine and rehabilitation stage, once the patients are in a rehabilitation centre, and finally the last batch for patients with SCI who returned home (chronic stage).
Then the different factors were grouped together by themes and the level of evidence was discussed, on the one hand, regarding the type of study (in ascending order by level of evidence: cross-sectional study, case–control study, historical cohort study and prospective cohort study), and on the other hand, according to the quality assessment established for each study. A factor was deemed ‘PU relevant,’ when a statistical link was established in a cross-sectional study. A factor was labelled as ‘potential risk factor,’ when a correlation was made from a case–control or cohort study with univariate analysis and ‘risk factor’ with multivariate analysis.
We sum up the level of scientific evidence by using a three-level scoring system used earlier for systematic reviews of risk factors:19
-
Strong evidence (level 1): provided by generally consistent findings in multiple high-quality studies.
-
Moderate evidence (level 2): provided by generally consistent findings in one high-quality study and one or more low-quality studies, or in multiple low-quality studies.
-
Insufficient evidence (level 3): only one study available or inconsistent findings in multiple studies.
Results
Bibliographical research results
The data examination included 820 references (Figure 1). The initial analysis based on titles and abstracts included 40 articles. The analyses of the reference lists allowed us to add two more articles. The second analysis based on full texts excluded 20 articles.
Among the 22 studies, six focused on the acute stage (prehospital, emergency or neurosurgery care), two were carried out during the rehabilitation stage and 14 focused on the chronic stage (patients at home).
Characteristics of the excluded studies
Among the excluded studies, two were irrelevant and20, 21 seven were on the basis of basic research.22, 23, 24, 25, 26, 27 In one study, the population was not SCI exclusive,10 and three other studies focused on SCI patients with PU.28, 29, 30 Three studies were descriptive, without any PU-related factors.31, 32, 33 The last three excluded studies were an overview of PUs in patients with SCI,34 a validation of a risk assessment scale35 and a preliminary report of a case study already included in our review.36
Potential risk factors or PU-associated risk factors during the acute stage
A literature analysis included six studies dealing with this acute stage (Table 1). Among these six studies, one was a cohort study and five were historical cohort studies. The quality assessment mean score was 60.7% (E=35.7–85.7). The number of patients included ranges from 39 to 54937, 38 with a total number of 1061 patients. The studies that included the largest number of patients also had the lowest quality assessment score.
Pressure ulcers were clinically and directly evaluated in one study,37 and indirectly evaluated by data extraction from the patients' medical records in four other studies.12, 14, 38, 39 Curry et al.40 do not clearly state the modalities used for accessing the data, but they were probably extracted from the medical records.
The literature search found 26 studied risk factors that can be classified as following:
Sociodemographic factors
Age at time of the accident was taken into account in four studies,12, 14, 37, 39 and is not related to the onset of PUs with a strong level of evidence (Table 2). Sex: there was support to include sex as a risk factor, as separate studies have shown it to be important for women39 and men.14 Quality assessment is comparable; the level of evidence is insufficient for this factor. Ethnicity was taken into account in one study12 and was associated with PU. The level of evidence is insufficient.
Neurological factors
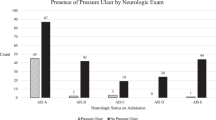
The transversal extension of the spinal-cord lesion has been evaluated in four studies12, 14, 39, 40 and is associated twice with PU onset.12, 14 The level of evidence is insufficient to qualify this factor as a risk factor. The vertical extension of the spinal-cord lesion, evaluated by the ASIA motor index,37 is not associated with PU. The level of evidence is insufficient. The neurological level (paraplegia or tetraplegia)12, 14, 38, 39, 40 is not correlated with PU onset, and cannot be considered as a risk factor. The level of evidence is strong.
Functional factors
The mobility status (in bed, in a wheelchair or walking) has been evaluated in a historical cohort study,12 and is correlated to the onset of a PU. This same study assessed the patient's mobility status with a significant correlation. There is an important measurement bias on this variable—the evaluation was retrospective and quantified the patient's mobility status in bed only from the data collected in the patient's medical records based on the comments of nurses. These are two risk factors with an insufficient level of evidence (level 3).
Clinical factors
The presence of another trauma injury to the bones or internal organs,14, 37 as well as smoking, is not considered as PU-related factor during this acute stage (Table 3). The level of evidence is moderate (level 2).
A history of lung disease is a risk factor found in a historical cohort study, but the results are confusing. Patients with a history of chronic lung disease tend to develop PU at a later stage than those with no history of lung disease. No other study has taken this factor into account, and the level of evidence is insufficient (level 3). The same study has evaluated several factors such as moisture (urines and faeces) or mental status with major measurement bias due to the data collection mode described above. These two factors could be labelled as risk factors, but the level of evidence is insufficient (level 3).
Urinary incontinence is reported in several studies as a potential risk factor; however, a good quality cohort study, but with a univariate analysis, finds no correlation, whereas a historical cohort study with multivariate analysis found a correlation between urinary incontinence and PUs.
Low blood pressure on arrival at the emergency room (ER) is linked to the onset of PU in a high quality cohort study. The level of evidence is moderate (level 2).
Biological factors
Hemodynamic and cardiorespiratory variables (complete blood count, arterial blood gas measurement and pulse oxymetry) are not correlated to PUs.12, 37 Thus, they are not PU risk factors (level 2).
The results regarding malnutrition seem discordant: a cohort study finds no correlation between 72-h prealbumin levels and the onset of a PU; on the other hand, another historical cohort study finds a correlation between the decrease of albumin levels during the first week and the onset of PU. We can consider, in fact, that malnutrition, with a variation in the albumin levels, is a risk factor for developing a PU with an insufficient level of evidence (level 3), and a 72-h prealbumin level monitoring is too early to detect a potential malnutrition.
The initial creatinaemia is a risk factor found in a historical cohort12 with a significant statistical difference (0.98 vs 1.12 mg l−1), but it is clinically non-significant because these levels are within the normal biological range.
Medical care management factors
The ER transfer time and the distance covered between the injury site and the ER, as well as the use of a long spine board during the prehospitalization acute stage, are all associated with the onset of PU with a moderate level of evidence (level 2; Table 4). The incidence of PU increases significantly beyond the 6 h.37, 40
Time spent in the neurosurgery ward is also a PU-related risk factor, especially after 15 days.14 Therapeutic gestures, such as vertebral osteosynthesis and tracheotomy, are also PU-related risk factors.14 These three factors are qualified as potential risk factors (univariate analysis), with an insufficient level of evidence (level 3).
PU-related or potential risk factors during the rehabilitation stage
Only two studies41, 42 were carried out within a rehabilitation centre. These studies included patients hospitalized for an initial rehabilitation stay for their SCI as well as patients being rehospitalized for a PU. As our initial hypothesis was that risk factors varied according to the different stages of their medical care, we considered that patients being rehospitalized for PU depended on the at-home risk factors, and as it was a major selection bias, we discarded these two studies.
Discussion
Our goal for this first part of our systematic literature review was to assess the PU risk factors for the acute and rehabilitation stages of SCI.
During the acute stages of an SCI (acute SCI), pre-hospital care and neurosurgery care, the risk factors do not appear to be related to the clinical variables. Medical care management (duration of stay in the neurosurgery ward and time spent on a long spine board ) appears to have an unsuspected impact on the onset of a PU.
Among the clinical variables studied, arterial low blood pressure can be considered as a potential risk factor, with a moderate level of evidence. It is also a known PU risk factor in the elderly population,43 with, as pathophysiological support, tissue hypoperfusion. The patient's nutritional state and urinary incontinence are also known as PU risk factors44, 45 and are found in the main PU risk assessment scales. The lack of a statistical link between PU and urinary incontinence during the acute SCI stage can be explained by the systematic urinary catheterization on admission to the ER. Furthermore, the causal relationship between urinary incontinence and PUs has been argued lately:46 urinary incontinence might be a telltale sign for other risk factors, such as the loss of autonomy in elderly persons. Malnutrition is an epidemiological risk factor with an insufficient level of evidence (level 3). It is a complication of acute SCI, with an average loss of 3.3 kg during the first 4 weeks,47 and treating this malnutrition reduces the risk of developing a PU or speeds up its healing.48
The SCI neurological level (paraplegia or tetraplegia) is not a PU risk factor with a strong level of evidence, meaning that paraplegic patients have the same rate of PU incidence that tetraplegic patients do in the acute stage of their SCI. This is probably related to the high incidence of early immobilization and vertical stabilization for acute SCI patients, regardless of their neurological level.
As for prehospital medical care management, immobility as well as the relationship between interface pressure and the length of immobilization time seems to be the main pathophysiological support49, 50 for the identified risk factors (using a hard surface such as a long spine board, the time period between the initial injury and the patient's admission to the ER as well as the distance travelled between the injury site and the ER). The use of this type of equipment has been criticized recently. It should not be systematically used, because it is a source of discomfort and pain and can lead to PUs.51
Some risk factors (moisture, incontinence, mobility status, mental status and nutrition) present a measurement bias that is taken into account when interpreting the results.
The medical care-related risk factors that are identified during the patient's hospital stay before their transfer to the physical medicine and rehabilitation centre should be interpreted with caution. In fact, the relationship between the time spent in the neurosurgery ward, a vertebral osteosynthesis and the length of immobilization time have already been described for the patient with SCI, and it seems that the sooner the patient is surgically stable, the shorter will be the hospital stay and immobilization time.52, 53 Performing a tracheotomy should probably not be regarded as a risk factor per se, but rather as a marker for the severity of the patient's clinical state. Other therapeutic actions, such as wearing a neck brace during the acute stage of polytrauma, have been associated with the onset of PU,54 but no study is SCI-specific for this variable.
No study has been conducted within a rehabilitation centre on the basis of a homogeneous SCI population—that is,: excluding patients rehospitalized for PU—thus not allowing us to assess PU risk factors during this rehabilitation stage. The PU incidence in SCI rehabilitation centres is probably quite low, as the prevalence of PU upon admission in a rehabilitation centre is around 30%, which drops to 2% when patients leave the centre.14 There are very few studies on the subject, and the real impact of this phenomenon remains unclear.
The level of evidence for the risk factors involved in this review is low, taking into account the dearth of studies and the retrospective nature of most of them (historical cohorts). No study reported the relative risk or the odds ratio. Furthermore, the confusion impact between the various risk factors has not been clearly established (vertebral osteosynthesis, length of hospitalization time, tracheotomy and so on), and this could be the focus of some additional studies.
The current risk-assessment scales have a limited impact on patient with SCI, as they systematically attribute the same risk level to each patient,9 without differentiating patients with SCI, who will develop a PU from those who will not. This might be due to the contents of the scales with relevant physiological factors but irrelevant epidemiological ones for the SCI population. Risk-assessment scales, such as SCIPUS-A,12 were designed with an epidemiological approach but based on an historical cohort, thus leading to major measurement bias on some variables (moisture and activity level). This probably explains the limited predictive value of this scale in prospective studies, with results that can be compared to the classic scales.14 Furthermore, the risk factors that we found were correlated to the care management, but were not accounted for by the authors, and this could probably increase the predictive value of their risk assessment scales.
Study limitations
Several critical comments can be made on the methodology.
We abided by the Cochrane recommendation for the number of databases used for our literature search. We were not able to access some nursing-specific databases, such as the CINHAL database. We partly overcame this bias by a manual search.
The keywords used have been mostly selected from each database's thesaurus and compiled in a systematic manner according to the Cochrane recommendations.16 The PU and SCI topics did not raise any nosological issues in the bibliographical research. The risk factors topic required a wider array of keywords, thus explaining the large number of articles found during the initial search.
It is generally recommended, in order to increase the exhaustiveness of the bibliographical search, to analyse the references of the selected articles as well as to proceed with a manual review of the journals most likely to deal with the topic.16, 55 The references analysis of the selected articles and manual review unveiled three additional articles, which seems to be quite satisfactory in regards to the 22 articles retained. Finally, we did not follow the Cochrane recommendations for assessing the level of evidence, because the Cochrane scoring system always gives a low level of evidence to observational studies regardless of their quality.
Perspectives
The results of this systematic review of the literature demonstrate that the main risk factors during the acute SCI stage are correlated to both medical variables and the patient's medical care management. Thus, from prehospital medical care to, discharge from the surgery ward, the focus is on the patient's vital functions and spinal-cord stabilization as well as on preventing further spinal complications. If the various players are well aware of the PU risk in patients with SCI and usually implement specific prevention measures, they might not be aware of the potential negative impact of the therapeutic modes and length of immobilization. The level of evidence for care-related factors is better than that for medical factors, but it is mostly insufficient and requires additional prospective observational studies. There are no epidemiological investigations for risk factors during the rehabilitation stage, and we have noticed the lack of observational studies as well.
Conclusion
The objective of this literature review was to assess the PU risk factors during the acute and rehabilitation stages of a SCI. Risk factors during the acute stage are essentially related to the modalities of the patient's medical care management. The level of evidence for medical factors is mostly insufficient, except for low blood pressure on admission to the ER. Additional observational studies are needed, both for the acute and rehabilitation stages, to improve this level of evidence. Finally, this study allowed us to analyse the medical care organization and management of the PU risk during the acute SCI stage.
References
Frankel HL, Coll JR, Charlifue SW, Whiteneck GG, Gardner BP, Jamous MA et al. Long-term survival in spinal cord injury: a fifty year investigation. Spinal Cord 1998; 36: 266–274.
Yeo JD, Walsh J, Rutkowski S, Soden R, Craven M, Middleton J . Mortality following spinal cord injury. Spinal Cord 1998; 36: 329–336.
Johnson RL, Gerhart KA, McCray J, Menconi JC, Whiteneck GG . Secondary conditions following spinal cord injury in a population-based sample. Spinal Cord 1998; 36: 45–50.
Whiteneck GG, Charlifue SW, Frankel HL, Fraser MH, Gardner BP, Gerhart KA et al. Mortality, morbidity, and psychosocial outcomes of persons spinal cord injured more than 20 years ago. Paraplegia 1992; 30: 617–630.
Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Pressure ulcer prevention treatment following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med 2001; 24 (Suppl 1): S40–S101.
Whitney J, Phillips L, Aslam R, Barbul A, Gottrup F, Gould L et al. Guidelines for the treatment of pressure ulcers. Wound Repair Regen 2006; 14: 663–679.
Cardenas DD, Hoffman JM, Kirshblum S, McKinley W . Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil 2004; 85: 1757–1763.
Fuhrer MJ, Garber SL, Rintala DH, Clearman R, Hart KA . Pressure ulcers in community-resident persons with spinal cord injury: prevalence and risk factors. Arch Phys Med Rehabil 1993; 74: 1172–1177.
Wellard S, Lo SK . Comparing norton, braden and waterlow risk assessment scales for pressure ulcers in spinal cord injuries. Contemp Nurse 2000; 9: 155–160.
Salzberg CA, Byrne DW, Cayten CG, Kabir R, van Niewerburgh P, Viehbeck M et al. Predicting and preventing pressure ulcers in adults with paralysis. Adv Wound Care 1998; 11: 237–246.
Salzberg CA, Byrne DW, Cayten CG, van Niewerburgh P, Murphy JG, Viehbeck M . A new pressure ulcer risk assessment scale for individuals with spinal cord injury. Am J Phys Med Rehabil 1996; 75: 96–104.
Salzberg CA, Byrne DW, Kabir R, van Niewerburgh P, Cayten CG . Predicting Pressure Ulcers during initial hospitalization for Acute Spinal Cord Injury. Wounds 1999; 11: 45–57.
Mortenson WB, Miller WC . A review of scales for assessing the risk of developing a pressure ulcer in individuals with SCI. Spinal Cord 2008; 46: 168–175.
Ash D . An exploration of the occurrence of pressure ulcers in a british spinal injuries unit. J Clin Nurs 2002; 11: 470–478.
Chen Y, Devivo MJ, Jackson AB . Pressure ulcer prevalence in people with spinal cord injury: age-period-duration effects. Arch Phys Med Rehabil 2005; 86: 1208–1213.
Green S, Higgins J . Cochrane Handbook for Systematic Reviews of Interventions 4.2.5. In: http://www.cochrane.org/resources/handbook/, May 2005.
Macfarlane TV, Glenny AM, Worthington HV . Systematic review of population-based epidemiological studies of oro-facial pain. J Dent 2001; 29: 451–467.
Irwig L, Tosteson AN, Gatsonis C, Lau J, Colditz G, Chalmers TC et al. Guidelines for meta-analyses evaluating diagnostic tests. Ann Intern Med 1994; 120: 667–676.
Hoogendoorn WE, Van Poppel MN, Bongers PM, Koes BW, Bouter LM . Systematic review of psychosocial factors at work and private life as risk factors for back pain. Spine 2000; 25: 2114–2125.
Charlifue S, Lammertse DP, Adkins RH . Aging with spinal cord injury: changes in selected health indices and life satisfaction. Arch Phys Med Rehabil 2004; 85: 1848–1853.
Garber SL, Rintala DH . Pressure ulcers in veterans with spinal cord injury: a retrospective study. J Rehabil Res Dev 2003; 40: 433–441.
Alexander LR, Spungen AM, Liu MH, Losada M, Bauman WA . Resting metabolic rate in subjects with paraplegia: the effect of pressure sores. Arch Phys Med Rehabil 1995; 76: 819–822.
Mawson AR, Siddiqui FH, Connolly BJ, Sharp CJ, Summer WR, Biundo Jr JJ . Sacral transcutaneous oxygen tension levels in the spinal cord injured: risk factors for pressure ulcers? Arch Phys Med Rehabil 1993; 74: 745–751.
Rodriguez GP, Claus-Walker J . Biochemical changes in skin composition in spinal cord injury: a possible contribution to decubitus ulcers. Paraplegia 1988; 26: 302–309.
Rodriguez GP, Claus-Walker J, Kent MC, Garza HM . Collagen metabolite excretion as a predictor of bone- and skin-related complications in spinal cord injury. Arch Phys Med Rehabil 1989; 70: 442–444.
Rodriguez GP, Garber SL . Prospective study of pressure ulcer risk in spinal cord injury patients. Paraplegia 1994; 32: 150–158.
Scivoletto G, Fuoco U, Morganti B, Cosentino E, Molinari M . Pressure sores and blood and serum dysmetabolism in spinal cord injury patients. Spinal Cord 2004; 42: 473–476.
Lehman CA . Risk factors for pressure ulcers in the spinal cord injured in the community. SCI Nurs 1995; 12: 110–114.
Lloyd EE, Baker F . An examination of variables in spinal cord injury patients with pressure sores. SCI Nurs 1986; 3: 19–22.
Thiyagarajan C, Silver JR . Aetiology of pressure sores in patients with spinal cord injury. Br Med J (Clin Res Ed) 1984; 289: 1487–1490.
Chen D, Apple Jr DF, Hudson LM, Bode R . Medical complications during acute rehabilitation following spinal cord injury—current experience of the Model Systems. Arch Phys Med Rehabil 1999; 80: 1397–1401.
Gunnewicht BR . Pressure sores in patients with acute spinal cord injury. J Wound Care 1995; 4: 452–454.
Hammond MC, Bozzacco VA, Stiens SA, Buhrer R, Lyman P . Pressure ulcer incidence on a spinal cord injury unit. Adv Wound Care 1994; 7: 57–60.
Sheerin F, Gillick A . Early pressure ulcer development in spinal cord injured patients. Emerg Nurse 2004; 12: 34–38.
New PW, Rawicki HB, Bailey MJ . Nontraumatic spinal cord injury rehabilitation: pressure ulcer patterns, prediction, and impact. Arch Phys Med Rehabil 2004; 85: 87–93.
Linares HA, Mawson AR, Suarez E, Biundo JJ . Association between pressure sores and immobilization in the immediate post-injury period. Orthopedics 1987; 10: 571–573.
Mawson AR, Biundo Jr JJ, Neville P, Linares HA, Winchester Y, Lopez A . Risk factors for early occurring pressure ulcers following spinal cord injury. Am J Phys Med Rehabil 1988; 67: 123–127.
Richardson RR, Meyer Jr PR . Prevalence and incidence of pressure sores in acute spinal cord injuries. Paraplegia 1981; 19: 235–247.
Sheerin F, Gillick A, Doyle B . Pressure ulcers and spinal-cord injury: incidence among admissions to the Irish national specialist unit. J Wound Care 2005; 14: 112–115.
Curry K, Casady L . The relationship between extended periods of immobility and decubitus ulcer formation in the acutely spinal cord-injured individual. J Neurosci Nurs 1992; 24: 185–189.
Lamid S, El Ghatit AZ . Smoking, spasticity and pressure sores in spinal cord injured patients. Am J Phys Med 1983; 62: 300–306.
Vidal J, Sarrias M . An analysis of the diverse factors concerned with the development of pressure sores in spinal cord injured patients. Paraplegia 1991; 29: 261–267.
Schubert V . Hypotension as a risk factor for the development of pressure sores in elderly subjects. Age Ageing 1991; 20: 255–261.
Bansal C, Scott R, Stewart D, Cockerell CJ . Decubitus ulcers: a review of the literature. Int J Dermatol 2005; 44: 805–810.
Clark M, Schols JM, Benati G, Jackson P, Engfer M, Langer G et al. Pressure ulcers and nutrition: a new European guideline. J Wound Care 2004; 13: 267–272.
Krause T, Anders J, von Renteln-Kruse W . [Urinary incontinence as a risk factor for pressure sores does not withstand a critical examination]. Pflege 2005; 18: 299–303.
Laven GT, Huang CT, DeVivo MJ, Stover SL, Kuhlemeier KV, Fine PR . Nutritional status during the acute stage of spinal cord injury. Arch Phys Med Rehabil 1989; 70: 277–282.
Stratton RJ, Ek AC, Engfer M, Moore Z, Rigby P, Wolfe R et al. Enteral nutritional support in prevention and treatment of pressure ulcers: a systematic review and meta-analysis. Ageing Res Rev 2005; 4: 422–450.
Keller BP, Lubbert PH, Keller E, Leenen LP . Tissue-interface pressures on three different support-surfaces for trauma patients. Injury 2005; 36: 946–948.
Lovell ME, Evans JH . A comparison of the spinal board and the vacuum stretcher, spinal stability and interface pressure. Injury 1994; 25: 179–180.
Vickery D . The use of the spina l board after the pre-hospital phase of trauma management. Emerg Med J 2001; 18: 51–54.
Campagnolo DI, Esquieres RE, Kopacz KJ . Effect of timing of stabilization on length of stay and medical complications following spinal cord injury. J Spinal Cord Med 1997; 20: 331–334.
Wang D, Teddy PJ, Henderson NJ, Shine BS, Gardner BP . Mobilization of patients after spinal surgery for acute spinal cord injury. Spine 2001; 26: 2278–2282.
Morris CG, McCoy EP, Lavery GG . Spinal immobilisation for unconscious patients with multiple injuries. Bmj 2004; 329: 495–499.
Suarez-Almazor ME, Belseck E, Homik J, Dorgan M, Ramos-Remus C . Identifying clinical trials in the medical literature with electronic databases: MEDLINE alone is not enough. Control Clin Trials 2000; 21: 476–487.
Acknowledgements
We thank the Fondation Paul Bennetot for their research funding as well as Christine Gilbert for her precious bibliographical research, Frank Dreyer for his help with the results and Bénédicte Clément for her translation.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
Keywords used for the literature database research
1. Spinal-cord injury
2. Spinal-cord injuries
3. Spinal-cord disease
4. parapleg*
5. tetrapleg*
6. #1 OR #2 OR #3 OR #4 OR #5
7. Pressure sore
8. decubitus sore
9. pressure ulcer
10. decubitus ulcer
11. bedsore
12. #7 OR #8 OR #9 OR #10 OR #11
13. risk
14. risk factor
15. risk assessment
16. epidemiology
17. case–control studies
18. follow-up studies
19. prospective studies
20. aetiology
21. causality
22. causation
23. relative risk
24. Odd ratio
25. #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24
26. #6 AND #12 AND #25
Rights and permissions
About this article
Cite this article
Gélis, A., Dupeyron, A., Legros, P. et al. Pressure ulcer risk factors in persons with SCI: part I: acute and rehabilitation stages. Spinal Cord 47, 99–107 (2009). https://doi.org/10.1038/sc.2008.107
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.107
Keywords
This article is cited by
-
Development of the spinal cord injury pressure sore onset risk screening (SCI-PreSORS) instrument: a pressure injury risk decision tree for spinal cord injury rehabilitation
Spinal Cord (2021)
-
Factors affecting adherence to behaviours appropriate for the prevention of pressure injuries in people with spinal cord injury from Malaysia: a qualitative study
Spinal Cord (2021)
-
Epidemiological characteristics and early complications after spinal cord injury in Former Yugoslav Republic of Macedonia
Spinal Cord (2020)
-
Severe pressure ulcers requiring surgery impair the functional outcome after acute spinal cord injury
Spinal Cord (2020)
-
A latent structural equation model of risk behaviors and pressure ulcer outcomes among people with spinal cord injury
Spinal Cord (2017)