Abstract
Patients with complex congenital heart disease (CCHD) may pose a serious threat to the mother-infant safety. This study intends to explore the influencing factors for adverse pregnancy outcomes in the CCHD population. Totally 108 CCHD patients who terminated pregnancy from January 2013 to January 2023 were recruited. We collected clinical data during the pregnancy from electronic medical records. Among them, 45 patients had adverse pregnancy outcomes (41.7%) and no patient died. 5 patients with no newborn. The incidence rate of adverse pregnancy outcomes was significantly higher in patients with brain natriuretic peptide (BNP) > 100 pg/mL (OR: 2.736; 95%CI: 1.001–7.481, p = 0.049) and hypoxemia (OR: 15.46; 95%CI: 1.689–141.512, p = 0.015) and without undergoing cardiac surgical correction (OR: 3.226; 95%CI: 1.121–9.259, p = 0.03). It was confirmed by propensity score matching that no cardiac surgical correction was an independent risk factor. Maternal patients without undergoing cardiac surgical correction had poorer NYHA cardiac function (p = 0.000) and were more prone to heart failure (p = 0.027), hypoxemia (p = 0.042), pulmonary arterial hypertension (p = 0.038) and postpartum hemorrhage (p = 0.016). Moreover, these patients had prolonged Surgical Intensive Care Unit (SICU) stay (p = 0.000) and significantly higher risk of premature delivery (p = 0.005), low birth weight (p = 0.018), infection and asphyxia (p = 0.043). Corrective cardiac surgery in patients with CCHD before pregnancy significantly reduces the incidence of adverse pregnancy outcomes.
Similar content being viewed by others
Introduction
The number of pregnancies in women with complex congenital heart disease (CCHD) has increased over the past decades and is expected to rise further in the coming years1. The severe abnormalities of cardiac structure and hemodynamic changes during pregnancy of CCHD patients bring greater challenges to the cardiovascular system2. Due to the increases in the maternal blood volume, cardiac output, oxygen consumption and heart rate during pregnancy, the patients may develop heart failure, malignant arrhythmia and other serious complications at any time, leading to high mortality and extremely high risk of perinatal adverse pregnancy outcomes3. According to a study by the European Registry of Pregnancy and Cardiac Disease (ROPAC), only 40% of CCHD patients have no adverse pregnancy outcomes, and maternal events and fetal events occur in about 36% and 43% of them, respectively4. Recent studies have shown that brain natriuretic peptide (BNP), low oxygen saturation, pulmonary arterial hypertension and other risk factors can significantly affect the pregnancy outcome of the CCHD population5,6. At present, the pre-pregnancy assessment, pregnancy management and reduction of the incidence of adverse pregnancy outcomes in this population are one of the focuses of attention.
Currently, numerous advancement have been made for the patient suffering from CCHD during pregnancy, which significantly improve the outcomes7. In particular, CCHD surgical techniques have improved8, but there is still a lack of evidence whether surgery can improve the prognosis of pregnant women with CCHD. This study intends to explore the influencing factors for adverse pregnancy outcomes in the CCHD population, so as to further improve the clinical management and intervention of the disease, and provide guidance for obtaining favorable pregnancy outcomes.
Methods
Patients
This study includes pregnant women with CCHD who were hospitalized in Beijing Anzhen Hospital from January 2013 to January 2023. In 2018, the American Heart Association proposed the AP classification of congenital heart disease, i.e., Anatomy + Physiological stage, to assess the complexity of congenital heart disease, in which all IA-IIID grades can be classified as CCHD: including types such as Tetralogy of Fallot, corrected transposition of the great arteries, complete transposition of the great arteries, Ebstein’s anomaly, single ventricle, and severe valvular anomalies9.
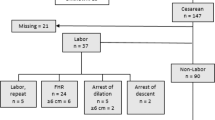
Inclusion criteria were as follows: (1) Pregnant women with CCHD; (2) those who terminated pregnancy at <28 weeks for cardiac reasons and for all reasons at ≥28 weeks. Exclusion criteria were as follows: (1) Patients with incomplete data; (2) those who terminated pregnancy for non-cardiac reasons at <28 weeks. A total of 108 eligible patients were included.
The study protocol was approved by the ethics committees or institutional review boards of the Beijing Anzhen Hospital. All clinical procedures fulfilled the tenets of the Declaration of Helsinki. All participants were informed about the study’s purpose, risks, and benefits and gave informed consent for this study. Supplementary Fig. 1 shows the flowchart of the current study scheme.
Prognostic variables
The data related to pregnancy were mainly collected prior to delivery, including maternal CCHD type, age, parity, length of SICU stay, NYHA cardiac function class, mode of delivery, history of cardiac surgery, postpartum hemorrhage, arrhythmia, valvular regurgitation, Eisenmenger, heart failure, neonatal Apgar score, birth weight, gestational age at birth, neonatal malformation, neonatal complications (neonatal infection, asphyxia, hyperbilirubinemia, arrhythmia), echocardiographic indicators (ejection fraction, pulmonary arterial pressure, valvular regurgitation), BNP, hemoglobin, and SPO2.
Adverse pregnancy outcomes
The adverse pregnancy outcomes include adverse maternal outcomes and adverse neonatal outcomes. Adverse maternal outcomes were defined as having any of the following conditions. Termination of pregnancy was characterized by a gestational age of delivery <37 weeks. Postpartum hemorrhage was defined as blood loss of more than 500 ml after vaginal delivery or more than 1000 ml after cesarean section10. Miscarriage was identified as the spontaneous loss of pregnancy before 28 weeks of gestation. Arrhythmia was characterized by irregular heartbeats detected during pregnancy through electrocardiogram (ECG). Admission to the Surgical Intensive Care Unit (SICU) was necessitated by severe complications such as severe infection11. Heart failure was defined as a cardiac ejection fraction less than 50% accompanied by symptoms such as dyspnea12. Adverse neonatal outcomes included conditions such as low birth weight, defined as a birth weight of ≤2500 grams. Neonatal infection was diagnosed based on clinical signs and laboratory findings indicative of infection, such as fever, lethargy, and positive blood cultures. Neonatal asphyxia was defined by an Apgar score of less than 8 at 5 min, indicating difficulty in establishing adequate breathing at birth. Neonatal malformations were congenital abnormalities detected in the newborn through clinical examination or imaging studies. Any combination or single occurrence of the above outcomes in the same patient was counted as one adverse pregnancy outcome.
Statistical analysis
SPSS25.0 software was used for data analysis. Measurement data were compared between the two groups by t-test. Enumeration data were expressed as [n(%)], and compared between the two groups by chi-square test or Fisher’s exact probability test. Multivariate Logistic regression analysis was performed on statistically significant variables in univariate analysis (BNP > 100 pg/mL, without a history of cardiac surgery, cardiac function, pulmonary arterial pressure, and hypoxemia). The propensity score matching method was used to reduced selection bias introduced by using a non-randomized design. The following variables were used to compute the propensity score for each patient: age, BNP, Hypoxemia, NYHA Cardiac function class, Arrhythmia, Hemoglobin, ejection fraction and PAP. p < 0.05 was considered statistically significant. Using Graphpad Prism for Statistical Mapping. R software was used for data visualization.
The propensity score matching method was used to reduced selection bias introduced by using a non-randomized design. The following variables were used to compute the propensity score for each patient: age, BNP, hypoxemia, NYHA Cardiac function class, arrhythmia, hemoglobin, ejection fraction and PAP. Confounding bias due to unknown factors cannot be completely excluded with this study design.
Results
The general characteristics of the study population
In this study, the average age of the 108 CCHD patients was 29 ± 4 years. Most patients had good cardiac function (87%). Among the pregnant women, 31.5% had elevated BNP levels (>100), indicating potential cardiac stress. The mode of delivery was predominantly cesarean section (86.4%). Baseline information on the 108 pregnant women with complex pre-centers is shown in Table 1.
The adverse pregnancy outcome
The average gestational age at termination of pregnancy was 36 ± 4 weeks. There were 5 cases of miscarriage (4.63%), with no maternal mortality events reported. Their primary mode of delivery was cesarean section (86.4%), with a few newborns presenting complications (6.81%). Maternal outcomes in Table 2 and neonatal outcomes in Table 3.
The adverse outcomes in different types of CCHD
The types of CCHD included tetralogy of Fallot, congenitally corrected transposition of the great arteries, complete transposition of the great arteries, Ebstein’s anomaly, single ventricle, double outlet of the right ventricle, aortic stenosis, and pulmonary stenosis (Table 4). Among them, tetralogy of Fallot accounts for the majority (67.59%), followed by transposition of the great arteries (18.52%). Complete transposition of the great arteries and double outlet of the right ventricle have the highest incidence of adverse pregnancy outcomes (100%).
The adverse outcomes in different patients with or without surgery
We analyzed the adverse outcomes in different patients with or without surgery. We found that the incidence of adverse outcomes in patients after cardiac surgery (32.88%) was significantly lower than that in patients without surgery (60%) (p < 0.001). Detailed results are shown in Table 5.
Factors associated with adverse outcomes
According to the presence or absence of adverse pregnancy outcomes, the pregnant patients with CCHD were divided into two groups. The incidence rate of adverse pregnancy outcomes was significantly higher in patients with BNP > 100 pg/mL (p = 0.014), hypoxemia (p = 0.001), NYHA cardiac function class ≥III (p = 0.001) and elevated pulmonary arterial pressure (p = 0.007), and without undergoing cardiac surgical correction (p = 0.004) in both groups (Table 6). There were no statistically significant differences in age, arrhythmia, gravidity and parity, Hb and EF between the two groups (p > 0.05).
The results of univariate analysis showed that BNP > 100 pg/mL, no cardiac surgical correction, NYHA cardiac function class ≥III, elevated pulmonary arterial pressure and hypoxemia were all risk factors for adverse pregnancy outcomes (p < 0.05). Then they were incorporated into the multivariate logistic regression analysis. It was found that BNP > 100 pg/mL (OR: 2.736; 95%CI: 1.001–7.481, p = 0.049), no cardiac surgical correction (OR: 3.226; 95%CI: 1.121–9.259, p = 0.03) and hypoxemia (OR: 15.46; 95%CI: 1.689–141.512, p = 0.015) were independent risk factors for adverse pregnancy outcomes (Fig. 1).
Association of cardiac surgical correction and adverse pregnancy outcomes
In order to make the baseline information consistent between the two groups with and without cardiac surgical correction, we chose the propensity score matching method. This approach was used to further investigate the independent impact of preoperative refinement of cardiac corrective surgery on adverse pregnancy outcomes in patients with complicated congenital heart disease.
In the unmatched data, there were 75 individuals in the group who underwent cardioversion before pregnancy and 33 individuals in the group who did not. After propensity score matching, we obtained 33 pairs of matched data. One-way analyses of the matched variables were conducted again, showing no statistically significant differences in the remaining baseline information, confirming that the match was established (Table 7).
We performed a univariate analysis of all matched patients (66 in total) grouped according to whether or not an adverse pregnancy outcome occurred, and the results showed that whether or not cardiac corrective surgery was performed had a significant and independent effect on pregnancy outcome (p = 0.001) (Table 8).
Basic data of pregnant patients with CCHD were compared with and without cardiac surgical correction. The results revealed that there were statistically significant differences between the two groups in gestational age at termination of pregnancy (p = 0.005), length of SICU stay (p = 0.000), pulmonary arterial pressure (p = 0.038), Hb (p = 0.018), SPO2 (p = 0.042), cardiac function (p = 0.000), incidence of heart failure (p = 0.027), and postpartum hemorrhage (p = 0.016). Patients without undergoing cardiac surgical correction had significantly higher rate of premature delivery, pulmonary arterial pressure, Hb and incidence of heart failure, significantly longer length of SICU stay, significantly lower SPO2, and significantly poorer cardiac function than those undergoing cardiac surgical correction. The delivery mode had no statistically significant difference between the two groups (p > 0.05), mainly cesarean section (CS) rather than vaginal delivery (VD). There were 27 cases (93.1%) and 63 cases (85.1%) of CS among patients without undergoing cardiac surgical correction and undergoing cardiac surgical correction, respectively (Table 9). No statistically significant differences were found between the two groups in age, parity, EF, BNP, and incidence of Eisenmenger syndrome and arrhythmia (p > 0.05). Taken together, these data suggest that not having cardiac surgery before pregnancy is a risk factor, which also correspond to the odds ratio (3.226) as shown in Fig. 1.
There were 103 live births in the two groups. The two groups had significant differences in the birth weight (p = 0.018), and incidence of neonatal complications (infection, asphyxia) (p = 0.043) (Table 10). Specifically, the incidence of low birth weight, asphyxia, infection and postpartum hemorrhage in patients without undergoing cardiac surgical correction was significantly higher than that in patients undergoing cardiac surgical correction.
Among the 103 neonates, there were 4 (3.9%) neonatal infections, 3 (2.9%) neonatal asphyxia, 1 (1.0%) neonatal cardiac arrhythmia, and 26 neonates with a birth weight of <2500 g, including 2 very-low-birth-weight infants (1230 g and 1160 g) and 1 very-low-birth-weight infant (980 g), all born prematurely at 30 weeks. The mothers of these three children had one case of heart failure and two cases of concomitant severe pulmonary hypertension.
Discussion
Pregnancy is a major life event for almost every woman. However, for women with CCHD pregnancy is associated with additional risks and deserves special attention13. This study evaluates the possible influencing factors for pregnancy outcomes of patients with CCHD, and the high-risk factors for adverse pregnancy outcomes were searched to predict the occurrence of adverse pregnancy outcomes to a certain extent. After analyzing 108 CCHD patients, we found that BNP, history of cardiac surgical correction, NYHA cardiac function class, pulmonary arterial pressure, and hypoxemia were associated with adverse events. After multivariate adjustment, BNP, history of cardiac surgical correction, and hypoxemia remained associated with adverse events. Patients who did not undergo cardiac surgery had a higher incidence of adverse pregnancy outcomes. Propensity score matching analysis further confirmed the independent effect of cardiac surgery on improving pregnancy outcomes. Patients who did not undergo cardiac surgery had significantly higher rates of preterm birth, pulmonary arterial pressure, heart failure, postpartum hemorrhage, and longer SICU stays. Additionally, these patients had significantly increased rates of low birth weight, asphyxia, and infection in newborns compared to the surgery group.
CCHD is a progressive congenital disease, and the opportunity for surgery may be eventually lost. Patients with CCHD have far inferior cardiovascular adaptability to the population with normal cardiac function, and are faced with serious threats brought about by the unique hemodynamic changes during pregnancy. A German study involving 4015 CHD patients found that, compared to a healthy control group, the incidence of stroke, heart failure, and arrhythmia during pregnancy was significantly higher. As the complexity of CHD increased, the incidence of adverse maternal and fetal outcomes also rose. However, the risk factors remain unclear14. Previous studies have shown that high-risk factors for adverse cardiovascular events in patients with congenital heart disease (CHD) include NYHA Class III-IV heart function and heart failure15,16. Several studies have shown that a high BNP concentration (>100 pg/mL) is associated with adverse cardiovascular events and adverse maternal-infant outcomes, and BNP currently serves as a negative predictor of adverse events, consistent with the findings in this study17. Our study has reached similar conclusions.
Shuenn-Nan et al. argued that the incidence of pulmonary arterial hypertension is up to 49.9% in the CCHD population by the age of 40 years, and Asian CCHD patients with pulmonary arterial hypertension have a higher incidence of adverse events than those without pulmonary arterial hypertension5 In this study, the pulmonary arterial pressure in patients who had undergone cardiac surgical correction before pregnancy was significantly lower than that in patients without undergoing cardiac surgical correction. Therefore, cardiac surgical correction before pregnancy in patients with CCHD is beneficial to delaying the progression of pulmonary arterial hypertension, but has less significant effect on adverse pregnancy outcomes. Considering the small sample size, the significance of cardiac surgical correction remains to be determined by more prospective studies.
Among the 108 patients in this study, the incidence of adverse maternal and neonatal outcomes significantly decreased among those who underwent cardiac surgery. Wang et al.18 found that cardiac surgical correction before pregnancy in CCHD patients can effectively relieve cardiac dysfunction, improve oxygen saturation, and reduce the incidence of perinatal complications, achieving better pregnancy outcomes in most patients, consistent with the results of this study. However, patients are still at risk at any time after surgery, and adequate risk assessment is required before pregnancy, regardless of the presence or absence of residual cardiac disease18.
Patients with CHD often require multiple surgeries, and the timing of surgical intervention should be determined within the context of each patient’s life cycle. Since repeat cardiac surgery is high-risk, the decision to perform surgery must be made with caution, especially in young women of childbearing age. Surgery is usually not performed if residual disease is mild or if pregnancy is tolerable.
For patients with CCHD, surgery usually cannot completely resolve the problem. Although surgery can significantly improve heart structure and function, residual cardiac lesions and long-term complications may still persist. Hemodynamic changes during pregnancy can exacerbate the condition of patients with CCHD. Among these patients, there are currently three common postoperative statuses: post-radical tetralogy of Fallot (TOF), post-arterial switch transposition of the great arteries (TGA), and functional univentricularity after Fontan. For post-radical TOF, long-term complications mainly include residual pulmonary regurgitation, right ventricular dilatation, ventricular dysfunction, and cardiac arrhythmia. Pregnancy may exacerbate these complications but is generally well-tolerated by most patients19. For post-arterial switch TGA, long-term complications include anatomical stenosis of the reconstructed great vessels and coronary dysfunction. Pregnancy may lead to neoaortic root dilatation, aortic regurgitation, and myocardial ischemia of coronary origin. Studies have shown that pregnancy is better tolerated in postoperative women. The prognosis for mother and child is extremely poor in those with severely reduced pulmonary blood flow or combined with severe pulmonary vascular disease20. In the case of functional univentricularity after Fontan, pregnancy is not recommended for patients with ventricular dysplasia, cyanosis, or mitral valve closure insufficiency. The prognosis for mothers and infants is poorer in patients with severely diminished pulmonary blood flow or comorbid severe pulmonary vascular disease21. Our study confirms that the incidence of adverse events is lower in patients with CCHD who have undergone cardiac surgery. Pregnancy outcomes are better for patients who have undergone surgery for TOF or TGA. However, pregnancy outcomes remain poor for patients with univentricularity after surgery.
In our study, there were 95 cases (88%) of pregnancy termination via surgery, with 75 of them due to cardiac intolerance. A previous study reported a CS rate of 44.8% for CCHD. The likely reason for the discrepancy is the different patient composition, as highly CCHD patients only accounted for 11.4% in that study. Previous studies have shown that significant haemodynamic fluctuations in pregnancy are associated with susceptibility to cardiovascular events22,23. Transvaginal delivery is highly susceptible to heart failure24. The American Heart Association’s stated that VD with adequate analgesia, supplemented by assisted labor, should be selected whenever possible, and CS should be selected according to obstetric indications7. Currently, there is no uniform clinical standard for the mode of delivery of patients with CCHD, which should be based on the patient’s cardiac condition25.
In addition to pregnancy risk, the offspring outcome of pregnant women with heart disease has also become the focus of current research in China and foreign countries. According to the National Birth Defects Prevention Network (NBDPN), birth defects occur in approximately 3–5% of newborns26. CHD is the most common birth defect, and its genetic mechanism remains to be fully understood. It is currently known that chromosomal abnormalities, copy number variations, and genetic defects occur in about 8–12%, 3–25% and 3–5% of patients with CHD, which may be inherited to their offspring. Therefore, it is recommended that women with CCHD undergo genetic testing before pregnancy. Studies have shown that 3–20% of patients with CHD can pass on the defect to their offspring, and such a risk of female patients is about twice that of male patients27. The proportion of newborns with birth defects was similar to that in the total population, but the proportion of newborns with CHD was significantly lower. However, this warrants further investigation. According to the ROPAC, the number of pregnant women with heart disease has increased significantly worldwide over the past five decades, and CCHD accounts for 20% of patients with CHD (66%), mostly with class III-IV cardiac function according to the modified World Health Organization (WHO) classification4. Such patients still have greater maternal and fetal risks during pregnancy, so close monitoring before, during and after pregnancy is required, and delivery plans should be formulated in advance to avoid as much as possible adverse outcomes such as maternal malignant arrhythmia, heart failure, fetal growth restriction and premature delivery28. To sum up, pregnancy is not recommended for CCHD patients with BNP > 100 pg/mL, no cardiac surgical correction and hypoxemia, and cardiovascular disease should be corrected first before pregnancy to obtain better maternal-fetal outcomes.
There are several limitations to this study. First, the patients were from a single cardiac center, and the cases span a long period during which surgical treatment levels have progressed. It is impossible to exclude data deviations caused by differences in surgical techniques at different centers and in different years. Second, due to the long case duration and changes in patient contact information, complete follow-up information was not obtained, limiting the exploration of long-term prognosis. A large number of prospective studies are still needed. Third, considering the small sample size, the use of propensity score matching may introduce confounding bias, and the significance of cardiac surgical correction needs to be confirmed by more prospective studies.
In conclusion, in this study we find the occurrence of adverse pregnancy outcomes is associated with BNP > 100 pg/mL, hypoxemia, NYHA cardiac function class ≥III, no cardiac surgical correction and elevated pulmonary arterial pressure, and BNP > 100 pg/mL, hypoxemia and no cardiac surgical correction are independent risk factors for adverse pregnancy outcomes. Cardiac surgical correction before pregnancy in CCHD patients is associated with reduced risk of deterioration of cardiac function, heart failure, hypoxemia, anemia, pulmonary arterial hypertension, premature delivery, postpartum hemorrhage, low birth weight and neonatal complications (infection, asphyxia) as well as the length of SICU stay.
References
van Hagen, I. M. & Roos-Hesselink, J. W. Pregnancy in congenital heart disease: risk prediction and counselling. Eur. Heart J. 88, 228–236 (2021).
Bravo-valenzuela, N. J., Peixoto, A. B. & Araujo Júnior, E. Prenatal diagnosis of congenital heart disease: a review of current knowledge. Indian Heart J. 70, 150–164 (2018).
Conti, E. et al. Pregnancy arrhythmias: management in the emergency department and critical care. J. Clin. Med. 13, 1095 (2024).
Avila, W. S. et al. Pregnancy in women with complex congenital heart disease. a constant challenge. Arq. Bras. Cardiol. 113, 1062–1069 (2019).
Chiu, S. et al. Pulmonary hypertension in adult congenital heart disease in Asia: a distinctive feature of complex congenital heart disease. J. Am. Heart Assoc. 11, e022596 (2022).
Van Den Bosch, E. et al. Associations between blood biomarkers, cardiac function and adverse outcome in a young tetralogy of Fallot cohort. Int. J. Cardiol. 361, 31–37 (2022).
Canobbio, M. M. et al. Management of pregnancy in patients with complex congenital heart disease: a scientific statement for healthcare professionals from the American Heart Association. Circulation 135, e50–e87 (2017).
Pettitt, T. W. Quality improvement in congenital heart surgery. NeoReviews 21, e179–e192 (2020).
Warnes, C. A. et al. Task Force 1: the changing profile of congenital heart disease in adult life. J. Am. Coll. Cardiol. 37, 1170–1175 (2001).
Giouleka, S. et al. Postpartum hemorrhage: a comprehensive review of guidelines. Obstet. Gynecol. Surv. 77, 665–682 (2022).
Laibl, V. & Sheffield, J. The management of respiratory infections during pregnancy. Immunol. Allergy Clin. North Am. 26, 155–172 (2006).
Bright, R. A., Lima, F. V., Avila, C., Butler, J. & Stergiopoulos, K. Maternal heart failure. J. Am. Heart Assoc. 10, e021019 (2021).
Ramage, K., Grabowska, K., Silversides, C., Quan, H. & Metcalfe, A. Association of adult congenital heart disease with pregnancy, maternal, and neonatal outcomes. JAMA Netw. Open 2, e193667 (2019).
Lammers, A. E. et al. Maternal and neonatal complications in women with congenital heart disease: a nationwide analysis. Eur. Heart J. 42, 4252–4260 (2021).
Grewal, J., Silversides, C. K. & Colman, J. M. Pregnancy in women with heart disease. Heart Fail. Clin. 10, 117–129 (2014).
Goldstein, S. A., Sorenson, L., Chapa, J. B. & Krasuski, R. A. Pregnancy in a woman with congenitally corrected transposition of the great arteries. Cleve. Clin. J. Med. 88, 228–236 (2021).
Tanous, D. et al. B-type natriuretic peptide in pregnant women with heart disease. J. Am. Coll. Cardiol. 56, 1247–1253 (2010).
Li, Yan et al. Analysis of perinatal outcomes in pregnant women with complex congenital heart disease. J. Clin. Cardiol. 34, 1112–1115 (2018).
Sugimoto, A. et al. Contemporary surgical management of complete atrioventricular septal defect with tetralogy of Fallot in Japan. Gen. Thorac. Cardiovasc. Surg. 70, 835–841 (2022).
Stoll, V. M. et al. Pregnancy outcomes in women with transposition of the great arteries after an arterial switch operation. JAMA Cardiol. 3, 1119 (2018).
McNamara, J. R., McMahon, A. & Griffin, M. Perioperative Management of the Fontan Patient for Cardiac and Noncardiac Surgery. J. Cardiothorac. Vasc. Anesth. 36, 275–285 (2022).
Kearney, K., Zentner, D. & Cordina, R. Management of maternal complex congenital heart disease during pregnancy. Curr. Heart Fail. Rep. 18, 353–361 (2021).
Kuate Defo, A. & Daskalopoulou, S. S. Alterations in vessel hemodynamics across uncomplicated pregnancy. Am. J. Hypertens. 36, 183–191 (2023).
Cutshall, A., Gourdine, A., Bender, W. & Karuppiah, A. Trends in outcomes of pregnancy in patients with congenital heart disease. Curr. Opin. Anaesthesiol. 36, 35–41 (2023).
Mok, T. et al. Delivery timing and associated outcomes in pregnancies with maternal congenital heart disease at term. J. Am. Heart Assoc. 11, e025791 (2022).
Mai, C. T. et al. Coronary artery bypass grafting versus percutaneous coronary intervention in end‐stage kidney disease: A systematic review and meta‐analysis of clinical studies. Curr. Opin. Cardiol. 959, 32–38 (2023).
Nees, S. N. & Chung, W. K. Genetic basis of human congenital heart disease. Cold Spring Harb. Perspect. Biol. 12, a036749 (2020).
Stephens, E. H., Bonnichsen, C. R. & Rose, C. H. Maternal and fetal outcomes in women with congenital heart disease. J. Cardiothorac. Vasc. Anesth. 36, 3685–3686 (2022).
Acknowledgements
The authors express their gratitude to all participants and healthcare professionals who selflessly supported this research. The authors did not receive any additional funding to support this research.
Author information
Authors and Affiliations
Contributions
J.G. collected and analyzed data, J.Z. wrote comments and edited them. All authors have contributed to the editorial changes of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gu, J., Zhao, H. & Zhang, J. Pregnancy outcomes among patients with complex congenital heart disease. npj Cardiovasc Health 1, 20 (2024). https://doi.org/10.1038/s44325-024-00022-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44325-024-00022-w