Abstract
Background
Stanford type B-acute aortic dissection (type B-AAD) is often life-threatening without invasive surgery. Multilineage-differentiating stress enduring cell (Muse cells), which comprise several percent of mesenchymal stem cells (MSCs), are endogenous pluripotent-like stem cells that selectively home to damaged tissue and replace damaged/apoptotic cells by in-vivo differentiation.
Methods
Mortality, aortic diameter expansion, cell localization, cell differentiation, and inflammation of the dissected aorta were evaluated in type B-AAD model mice intravenously injected with human-Muse cells, -elastin-knockdown (KD)-Muse cells, -human leukocyte antigen-G (HLA-G)-KD-Muse cells, or MSCs, all without immunosuppressant.
Results
Here, we show the Muse (50,000 cells) group has a lower incidence of aortic rupture and mortality of AAD compared with the MSC-50K (50,000 human-MSCs) and vehicle groups. Spectrum computed tomography in-vivo dynamics and 3-dimensional histologic analyses demonstrate that Muse cells more effectively home to the AAD tissue and survive for 8 weeks in the Muse group than in the MSC-750K (750,000 human-MSCs containing 50,000 Muse cells) group. Homing of Muse cells is impeded in the HLA-G-KD-Muse (50,000 cells) group. Differentiation of homed Muse cells into CD31(+) and alpha-smooth muscle actin (+) cells, production and reorganization of elastic fibers in the AAD tissue, and suppression of diameter expansion are greater in the Muse group than in the MSC-750K and elastin-KD-Muse (50,000 cells) groups.
Conclusions
Intravenously administered Muse cells reconstruct the dissected aorta and improve mortality and diameter enlargement rates. Moreover, small doses of purified Muse cells are more effective than large doses of MSCs. HLA-G is suggested to contribute to the successful survival and homing of Muse cells.
Plain language summary
Acute aortic dissection (AAD) is a serious disease in which the largest artery in the body, called the aorta, enlarges and ruptures. Surgery is often required to prevent death. Cells called Muse cells have been injected into people during clinical trials to treat other diseases. In this study, we injected Muse cells into mice with dissected aorta. The cells accumulated in damaged parts of the aorta and strengthened the structure of the aorta, reducing the number of mice that died. If further research shows this treatment works in humans, this could enable AAD to be treated without surgery and potentially improve the treatment and survival of people with AAD.
Similar content being viewed by others
Introduction
Acute aortic dissection (AAD) is a common, life-threatening disease that occurs with chest pain and/or back pain, mainly related to high blood pressure. AAD begins with a tear (entry) in the intima of the aortic wall and progresses into the media, forming the original aortic lumen (true lumen) and a newly created wall lumen (false lumen), and is associated with inflammation of the aortic tissue1,2,3,4. AAD is classified into two types5; Stanford type A-AAD (Stanford A-AAD), which involves the ascending aorta, requires emergent surgery to place a prosthetic vascular graft because the prognosis is generally poor; Stanford type B-AAD (Stanford B-AAD) that does not involve the ascending aorta but extends distal to the aortic arch is usually treated conservatively for avoiding surgical risks if there are no complications6,7. However, in Stanford B-AAD, the vulnerable dissected aorta often dilates over time and develops an aneurysmal transformation, increasing the risk of rupture8, which ultimately leads to significant mortality. This requires highly invasive surgery with the risk of serious complications such as spinal cord infarction9. Thoracic endovascular aortic repair (TEVAR), a surgical treatment intended to close the entry that connects the true lumen and false lumen, in the acute phase may improve mortality and aneurysmal changes during the chronic phase10, while this treatment includes risk of complications. In other words, there is no debate that emergency surgery is necessary for Stanford A-AAD, while surgery for the acute phase of Stanford B-AAD remains controversial. We focused on Stanford type B-AAD, expecting to avoid surgery in the chronic phase through structural strengthening of the dissected aorta in the acute phase by cell-based therapy.
Multilineage-differentiating stress enduring (Muse) cells that reside in the bone marrow (BM), peripheral blood, organ connective tissues, and umbilical cord are collectable as cells positive for the pluripotent surface marker stage-specific embryonic antigen (SSEA)−3 and are stress-tolerant11,12,13,14. They are also obtainable as stage-specific embryonic antigen-3 (SSEA-3)-positive cells as several percent of MSCs11,12,13,14. Muse cells are non-tumorigenic as they are endogenous to the body, and are stress tolerant with a high capacity for repairing DNA damage11,15,16. They exert anti‐inflammatory, anti‐apoptotic, anti-fibrosis and trophic effects by producing cytokines including vascular endothelial growth factor and matrix metalloproteinase-2/917,18,19. Muse cells exhibit pluripotent-like properties; i.e., expression of the pluripotent stem cell markers, differentiate into triploblastic-lineages from a single cell and exhibit self-renewability11,20.
Studies in which Muse cells were systemically administered in animal disease models of acute myocardial infarction, stroke, liver cirrhosis, chronic kidney injury, epidermolysis bullosa, and aortic aneurysm revealed unique features of Muse cells17,18,19,21,22,23. They express sphingosine-1-phosphate (S1P) receptor 2 and selectively home to the site of damaged tissue after intravenous injection by sensing S1P, produced in damaged cells by phosphorylating the cell membrane component sphingosine19,24. Therefore, intravenous drip is the main delivery method for clinical application and surgical operation is not required in many cases. Following engraftment in damaged tissue, Muse cells phagocytose damaged cells, recycle signals and factors derived from damaged cells, and differentiate into the same cell type as the damaged cells in a short time period to replace damaged/apoptotic cells and repair the tissue25. Therefore, Muse cells do not require gene induction or differentiation manipulation prior to clinical use. Notably, Muse cells possess a specific immune privilege and thus intravenously injected allogeneic/xenogeneic-Muse cells are able to escape from immunologic attack and survive as functional cells in the host tissue for more than 6 months and ~7 weeks in allogenic and xenogeneic systems, respectively, even without HLA-matching test or immunosuppression17,19.
Clinical trials have been initiated to evaluate the safety and efficacy of intravenously administered donor-derived allogeneic Muse cells without HLA matching or immunosuppression for the treatment of stroke, acute myocardial infarction, epidermolysis bullosa, amyotrophic lateral sclerosis, traumatic spinal cord injury, perinatal hypoxic ischemic encephalopathy, and COVID19- acute respiratory distress syndrome, under the approval of regulatory authorities (Japan Pharmaceutical Information Center-Clinical Trials Information; JapicCTI-183834, 184103, 184563, and 194841). The safety and efficacy of Muse cell treatment for acute myocardial infarction, epidermolysis bullosa and subacute ischemic stroke were recently reported26,27,28.
In the present study, we examine the effectiveness and mechanisms of action of intravenously injected human Muse cells in a conventional mouse Stanford B-AAD model without immunosuppression. As a result, Muse cells reconstruct the dissected aorta and improve diameter expansion rates and mortality.
Methods
Human-Muse cells and -MSCs
Human BM-derived MSCs, checked to be negative for mycoplasma contamination using MycoAlert® Mycoplasma Detection kit by the supplier (PT-2501, Lonza, Basel, Switzerland; obtained with informed consent from donors), were used as the source of Muse (SSEA-3(+) cells) and non-Muse MSCs (cells other than Muse cells in MSCs [SSEA-3(-)]), as previously reported11,29. Human BM-MSCs were cultured at 37 °C and 5% CO2 in low glucose Dulbecco’s Modified Eagle Medium (10567, Thermo Fisher Scientific, Waltham, MA) with 10% (vol/vol) fetal bovine serum (FBS); HyClone (SH30910.03, GE Healthcare, Chicago, IL) and 0.1 mg/mL kanamycin (15160-054, Thermo Fisher Scientific). For collection of Muse and non-Muse MSCs, eighth-passage MSCs were incubated with rat anti-SSEA antigen-3 (SSEA-3) IgM antibody (1:1000; 330302, BioLegend, San Diego, CA) as the primary antibody (rat IgM isotype control antibody,1:1000; 400801, BioLegend), fluorescein isothiocyanate (FITC)-conjugated goat anti-rat IgM antibody (1:100; 112-095-075, Jackson ImmunoResearch Laboratories, Inc., West Grove, PA) as the secondary antibody, and anti-FITC MicroBeads (1:50; Miltenyi Biotec Inc, Auburn, CA) as the tertiary antibody. MSCs were then separated into anti-FITC(+) and anti-FITC(−) cell fractions by magnetic-activated cell sorting (MACS) (autoMACS Pro Separator, Miltenyi Biotec Inc, Auburn, CA) and the FITC(+) cell fraction was used for the Muse cells injection group. Analysis by FACS (BD FACS Aria II, Becton Dickinson, Franklin Lakes, NJ) revealed that human BM-MSCs contained 5.0 ± 0.9% SSEA-3(+)-Muse cells (Fig. S1). The FITC(+) cell fraction sorted by MACS contained 76.5 ± 6.0% SSEA-3(+)-Muse cells (Fig. S1). Therefore, SSEA-3(+)-Muse cells were enriched from ~5% to ~76% by MACS. To give a specific example, 750,000 MSCs contain approximately 5% SSEA-3(+) cells ( = Muse cells), and a group of 50,000 MSCs sorted by MACS contains approximately 76% SSEA-3(+) cells ( = Muse cells). In other words, the number of Muse cells administered to the 750,000 MSCs injection group and the Muse cells injection group described below is almost the same. The SSEA-3(-) cell fraction was isolated by fluorescence activated cell sorting (FACS) and used as non-Muse MSCs (Fig. S1).
GFP-Muse cells and -MSCs
For histologic analysis, Muse cells and MSCs were labeled with green fluorescent protein (GFP) using lentivirus. For preparation of GFP-labeled Muse cells, human BM-MSCs were introduced with vectors below. For lentivirus production, pMD2G, pCMV deltaR8.74, and pWPXL-GFP were transfected into LentiX-293T packaging cells (Takara Bio Inc, Shiga, Japan) using Lipofectamine 2000 (Thermo Fisher Scientific, MA, USA). After 3 days, the viral supernatant was collected, centrifuged, and filtered through a 0.45-µm filter. For Muse cell sorting, GFP-labeled human BM-MSCs were incubated with rat anti SSEA-3 antibody (1:1000; BioLegend) detected by allophycocyanin-conjugated anti-rat IgM (1:100; Jackson ImmunoResearch) in the antibody diluents and sorted by FACSAriaII11. GFP(+) cells (GFP-MSCs) and GFP(+)/SSEA-3(+) double-positive cells (GFP-Muse cells) were sorted by FACS. To collect GFP-Muse cells, GFP-MSCs were incubated with rat anti-SSEA-3 IgM antibody (1:1000; 330302, BioLegend) as the primary antibody and allophycocyan-conjugated goat anti-rat IgM antibody (1:100; 112-136-075, Jackson ImmunoResearch Laboratories) as the secondary antibody.
HLA-G gene knockdown-Muse cells
HLA-G shRNA lentiviral particles (sc-42920-V, Santa Cruz Biotechnology Inc, Dallas, TX) and control shRNA lentiviral particles (sc-108080, Santa Cruz Biotechnology Inc) were introduced into Akaluc-MSCs and Muse cells were sorted by FACS as SSEA-3(+) cells to obtain HLA-G KD-Muse cells and shRNA control-Muse cells, respectively. The HLA-G protein expression level in JEG3 cells at the 5th and 10th passages was examined to assess the effect of HLA-G shRNA lentiviral particles. JEG3 cells (92120308, European Collection of Authenticated Cell Cultures (ECACC), Porton Down, England) were checked and found to be negative for mycoplasma contamination using PCR by the supplier. HLA-G shRNA lentiviral particles were introduced into JEG3 (HLA-G KD-JEG3). Protein extraction and Western blotting were performed as reported previously19. The primary antibody for HLA-G was mouse anti-human HLA-G IgG1 antibody (1:200, overnight; 557577, BD) and the secondary antibody was goat anti-mouse IgG-HRP antibody (1:5000, 1 h; 115-035-071, Jackson ImmunoResearch Laboratories). The primary antibody for ACTB (β-actin) was mouse anti-beta actin IgG1 antibody (1:10000, overnight; ab6276, abcam) and secondary antibody was goat anti-mouse IgG-HRP antibody (1:5000, 1 h; 115-035-071, Jackson ImmunoResearch Laboratories). Expression of HLA-G in HLA-G KD-JEG3 was suppressed in comparison to naïve JEG3 (Fig. S2a, b). Relative expression (HLA-G/ACTB) of HLA-G KD-JEG3 was 48.2% at the fifth passage and 37.7% at the tenth passage of naïve JEG3 (Fig. S2c). Then, HLA-G gene expression level in HLA-G KD-Muse cells and shRNA control-Muse cells was quantified by digital droplet polymerase chain reaction (ddPCR). Total RNA was extracted from cells and purified using an RNA purification kit (NucleoSpin RNA XS, Takara Bio). First-strand cDNA was synthesized by SuperScript III reverse transcriptase (Thermo Fisher Scientific). PCR was performed using a predesigned primer (HLA-G, Hs03045108_m1, Thermo Fisher Scientific). DNA was amplified using a ddPCR QX100 system (Bio-Rad Laboratories Inc, Hercules, CA) and quantified by QuantaSoft (Ver.1.7, Bio-Rad Laboratories Inc). Tenth-passage HLA-G KD-Muse cells and shRNA control-Muse cells were incubated with interferon gamma (100 ng/ml, 17001, Sigma-Aldrich) for stimulating the expression of HLA-G for 3 days. The ddPCR results confirmed that the HLA-G gene expression was decreased by 44.3% in HLA-G KD-Muse cells compared with that in shRNA control-Muse cells (P = 0.0036) (Fig. S2d). HLA-G expression in Muse cells was also assessed by FACS. Eleventh-passage MSCs and HLA-G KD-MSCs after incubation with interferon gamma (100 ng/ml, 17001, Sigma-Aldrich) for 3 days were incubated with rat anti-SSEA antigen-3 (SSEA-3) IgM antibody (1:1000; 330302, BioLegend) as the primary antibody [rat IgM isotype control antibody (1:1000; 400801, BioLegend)], FITC-conjugated goat anti-rat IgM antibody (1:100; 112-095-075, Jackson ImmunoResearch Laboratories) as the secondary antibody, and mouse anti-HLA-G IgG2a antibody (1:50; 557577, BD) as the primary antibody [mouse IgG2a isotype control antibody (1:50, 400201, BioLegend)], APC-conjugated goat anti-mouse IgG antibody (1:100; 115-136-146, Jackson ImmunoResearch Laboratories) as the secondary antibody. HLA-G expression was 69.7 ± 3.7% in naïve Muse cells while that was 8.8 ± 2.2% in HLA-G KD-Muse cells (Fig. S2e).
Elastin gene knockdown-Muse cells
Elastin shRNA lentiviral particles (sc-43360-V, Santa Cruz Biotechnology Inc) and control shRNA lentiviral particles (sc-108080, Santa Cruz Biotechnology Inc) were introduced into human BM-MSCs and Muse cells were sorted as SSEA-3(+) cells by FACS to collect Elastin KD-Muse cells and shRNA-control Muse cells. The elastin gene expression level was quantified by ddPCR. Total RNA was extracted from Muse cells and purified using an RNA purification kit (NucleoSpin RNA XS, Takara Bio). First-strand cDNA was synthesized by SuperScript III reverse transcriptase (Thermo Fisher Scientific). PCR was performed using a predesigned primer (elastin, Hs00355783_m1, Thermo Fisher Scientific). DNA was amplified using a ddPCR QX100 system (Bio-Rad Laboratories Inc) and quantified by QuantaSoft (Ver.1.7, Bio-Rad Laboratories Inc).
Induction of Stanford B-AAD model and analysis of model mice
The Animal Care and Use Committee of Tohoku University Graduate School of Medicine (Sendai, Japan) approved all the animal experiments in the present study (No. 2018-157) before the start of the experiments. Mice were housed in rooms of the animal experiment facility at Tohoku University Graduate School of Medicine maintained at 22 °C and 50% humidity under cycle 12 h dark/12 h light and provided standard food and water. Five mice were housed in one cage. The acclimatization period of mice was 1 week. Animal experiments were conducted from July 24, 2018 to October 2, 2021. Approximately 10 mice were used in the experiment per week. The experimenters, laboratories, laboratory animal suppliers, and equipment used were all the same to minimize potential confounding factors.
AAD-model making
Male 4-week-old wild-type mice (C57BL/6NCrS1c, Japan SLC, Inc., Hamamatsu, Japan) were used. Stanford B-AAD model mice were created according to the previously described method with minor modifications30,31. Only male mice were used in this study to exclude the effect of the estrous cycle, following previous studies30,31. In the previous method, model mice died 30% within 24 h and 70% within 48 h after onset of the dissection due to aortic rupture, and the survival rate after 2 weeks remained unknown30,31. In this study, the start time of β-aminopropionitrile fumarate salt (BAPN; A3134, MilliporeSigma, St. Louis, MO) supply was delayed from 3 weeks to 4 weeks after birth, and the human angiotensin II (Ang II; 4001-v, Peptide Institute, Inc., Osaka, Japan) administration period was shortened from 72 h to 24 h to reduce mortality. These modifications successfully reduced the mortality rate up to 20% within 24 h after onset of the dissection, and animals could survive for up to 8 weeks, enabling us to evaluate the dissected aorta until the subacute stage. Eventually, mice were fed a regular diet and drinking water containing BAPN (1 g/kg/d) for 4 weeks, an osmotic mini pump (Alzet 2001D, DURECT Corporation, Cupertino, CA) filled with Ang II was implanted subcutaneously in the back skin under anesthesia (4.0% isoflurane) and Ang II was continuously administered (1 μg/kg/min) for 24 h to induce Stanford B-AAD (Fig. 1a). Saline was administered instead of Ang II for the sham group. Incision of the skin (1 cm) and underlying tissues (3 cm) was performed for mini pump implantation. The skin incision was closed with 2 needle sutures using 4-0 nylon thread. Mice may die due to aortic rupture during the experiment. In particular, the risk of death due to dissected vessel wall rupture is high during 24 h after administration of Ang II, and careful observation is required. If the aorta ruptures, the mouse dies almost instantly, but the mouse does not die, and its ADL (Activities of Daily Living) is severely impaired, such as being unable to move or eat, and there are signs of death. If this is observed, euthanasia is judged to be appropriate as a humane endpoint.
a The outline of this study. Stanford B-AAD develops within 24 hours of starting Ang II (▲) administration after taking BAPN (△) for 4 weeks. Twenty-four hours after the administration of Ang II, the mice were randomly assigned to the following 4 groups: Mice received 0.2 ml saline containing either 50,000 Muse cells (Muse group), 50,000 MSCs (MSC-50K group), 750,000 MSCs that contain the same number of Muse cells as the Muse group, according to the calculations described in the “Human-Muse cells and -MSCs” paragraph in the Methods section (MSC-750K group), no cells (vehicle group) and underwent CT imaging (♦). Cells were administered (●) intravenously immediately after CT imaging. BAPN: β-aminopropionitrile fumarate salt. Ang II: angiotensin II. AAD: acute aortic dissection. MSC: mesenchymal stem cells. b Descending aortas with or without AAD from 16-weeks-old mice. Upper: the sham group (mice without AAD) as control. Lower: Stanford B-AAD model at 8 weeks after AAD onset. Left: contrast-enhanced CT, insets: short axis image of the descending aorta. There are 2 cavities in the AAD aorta, the true lumen (circle) and false lumen (asterisk) Right: Elastica-Masson staining of the aorta (low magnification). Higher magnification images of the boxed area are displayed. The cavity surrounded by continuous elastic fiber is the true lumen (circle). The false lumen is indicated by an asterisk. Scale bar: 200 μm (low magnification), 20 μm (high magnification). c Survival rate of the vehicle group (AAD mice administered with no cells) (n = 30), MSC-50K group (AAD mice administered with 50,000 mesenchymal stem cells) (n = 10), MSC-750K group (AAD mice administered with 750,000 mesenchymal stem cells) (n = 31) and Muse group (AAD mice administered with 50,000 Muse cells) (n = 34). Animals were killed at 8 weeks after cell administration. *P < 0.05. The vehicle group vs the MSC-50K group: P = 0.75 by log rank test and P = 0.70 by Wilcoxon test, the vehicle group vs the MSC-750K group: P = 0.18 by log rank test and P = 0.12 by Wilcoxon test, the vehicle group vs the Muse group: P = 0.014 by log rank test and P = 0.013 by Wilcoxon test, the MSC-50K group vs the MSC-750K group: P = 0.19 by log rank test and P = 0.12 by Wilcoxon test, the MSC-50K group vs the Muse group: P = 0.012 by log rank test and P = 0.010 by Wilcoxon test, the MSC-750K group vs the Muse group: P = 0.24 by log rank test and P = 0.32 by Wilcoxon test. d Macroscopic observation of the aorta at 8 weeks after cell administration. Bidirectional arrows indicate the dissected area. Scale bar: 5 mm. e Contrast-enhanced CT images. The dissected aorta dilated over time. The diameter was assessed by CT (short axis) at each time-point. White bars indicate the maximum minor-axis diameter of the dissected aorta. f Ratio of the dissected aortic diameter. The dilation ratio of the dissected aorta at 4 and 8 weeks after cell administration was calculated as the ratio to that on the first day of dissection. All groups were n = 10. The dilation ratio at 4 weeks; the Sham group vs the Vehicle group: P = 0.0010, the Sham group vs the MSC-750K group: P = 0.0010, the Sham group vs the Muse group: P = 0.0034, the Vehicle group vs the MSC-750K group: P = 0.14, the Vehicle group vs the Muse group: P = 0.0010, the MSC-750K group vs the Muse group: P = 0.014. The dilation ratio at 8 weeks; the Sham group vs the Vehicle group: P = 0.0010, the Sham group vs the MSC-750K group: P = 0.0010, the Sham group vs the Muse group: P = 0.0031, the Vehicle group vs the MSC-750K group: P = 0.041, the Vehicle group vs the Muse group: P = 0.0010, the MSC-750K group vs the Muse group: P = 0.0021. *P < 0.05; **P < 0.01 by log rank test and Wilcoxon test (c) and Steel–Dwass test (f). The boxplot indicates the interquartile range (top: the third quartile; bottom: the first quartile) with the whiskers extending to the most extreme points within 1.5 times the interquartile range (outliers beyond 1.5 times the interquartile range are also shown) and with a horizontal line and cross mark respectively indicating the median and mean (f).
Contrast-enhanced CT
Animals were anesthetized with 0.01 ml per mouse body weight (g) of a mixture of 0.75 mg medetomidine hydrochloride (Domitor, Orion Corporation, Espoo, Finland), 10 mg midazolam (Dormicum, Maruishi Pharmaceutical Co. Ltd, Osaka, Japan), and 12.5 mg butorphanol tartrate (Bettlefar, Meiji Seika Pharma Co. Ltd, Tokyo, Japan) in 25 ml saline and the osmotic mini pump was removed. Contrast-enhanced computed tomography (CT) was performed using CT equipment designed for animal experiments (Latheta LCT-200, Hitachi, LTD, Tokyo, Japan). Iomeprol (Iomeron, Eisai Co. Ltd, Tokyo, Japan), a contrast agent for CT imaging, was injected intravenously at a rate of 0.4 ml/h/body weight (g) using a syringe pump. The contrast agent was continuously injected for 2.5 min starting 1 min prior to the initiation of imaging without washing out the agent during imaging of the aorta.
Stanford B-AAD was diagnosed by confirming the presence of 2 cavities in the aorta other than the ascending aorta on multiple short axis images of contrast-enhanced CT. All CT images used for this study were provided in the repository32 URL: https://www.scidb.cn/en/detail?dataSetId=f1b7da634c334aaca05609c88740d65b. The diameter of the dissected aorta was assessed as the maximum minor-axis diameter of the thoracic aorta in the area of distal left subclavian artery bifurcation to the proximal diaphragm. The diameter of the dissected aorta was measured within 24 h after AAD induction (before cell injection), as well as at 4 and 8 weeks after cell injection (Fig. 1a). Osirix software (MD ver.5.8.2, Pixmeo SARL, Switzerland) was used to measure the aortic diameter.
Cell Infusion
After Ang II administration, mice were divided randomly into 4 groups before CT imaging to avoid bias depending on the difference in the aortic diameters. Experimenter MT was aware of the group assignment in subsequent stages of the experiment, but the other experimenters were not. Cells were intravenously administered immediately after the CT imaging (Fig. 1a). The treatment procedure after diagnosis using CT images is consistent with actual clinical procedures. Mice received 0.2 ml saline containing either 50,000 Muse cells (Muse group, n = 10), 50,000 MSCs (MSC-50K group, n = 10), 750,000 MSCs that contain the same number of Muse cells as the Muse group, according to the calculations described in the “Human-Muse cells and -MSCs” paragraph in the Methods section (MSC-750K group, n = 10), no cells (vehicle group, n = 10). Wild-type mice without AAD (sham group, n = 10) were also prepared. Mice that died by aortic rupture before the first CT scan, that develop Stanford type A-AAD, that did not develop AAD or that with a thrombosed false lumen were all excluded.
Sample size calculation
The minimum sample size (n) for detecting a difference in diameter enlargement of the dissected aorta between any two groups can be calculated using n = 2(Zα/2 + Zβ)2 (σ/δ)2. Z is a standardized value in a standard normal distribution. If we set α = 0.05 (significance level is 5%), then Zα/2 = 1.96. If we set β = 0.2 (power (1-β) is 80%), then Zβ = 0.84. σ is the standard deviation of diameter expansion ( = 8%). δ is the mean difference in diameter expansion (hypothesized to be 10%). By using the equation, the minimum sample size was expected to be 10 mice.
Sample size
A total of 330 mice were used in this study. Twenty-six mice were used as the sham group, and 304 were given BAPN. Of the 304 mice, 51 mice died from aortic rupture, and the 253 surviving mice received Ang II. Of the 253 mice, 56 mice died within 24 hours of starting Ang II administration due to rupture due to aortic dissection, 10 mice developed into Stanford A-AAD, 4 mice did not develop dissection, and 3 mice developed dissection with thrombosed false lumen. Consequently, the remaining 180 surviving Stanford B-AAD mice were assigned to either the Muse (n = 55), Elastin KD-Muse (n = 12), HLA-G KD-Muse (n = 3), non-Muse (n = 3), MSC-50K (n = 10), MSC-750K (n = 49), or vehicle groups (n = 48). Mice after treatment were not excluded from data acquirement.
Sample collection
In this study, all measurements were taken from distinct samples and the same sample was not measured repeatedly.
Survival rate
Overall survival of AAD model mice was monitored for 8 weeks after cell injection. The target animals were confined to those observed for over 4 weeks. Mice killed within 2 weeks of examination were excluded from the survival rate. At the same time, mice used for IVIS Spectrum CT described below were also excluded from the survival rate because the effect of Akaluc-transduction on the life span was unknown.
In vivo dynamics of injected cells
Lentivirus containing Venus-Akaluc was introduced into human BM-MSCs. In brief, Akaluc/pcDNA3, provided by Satoshi Iwano33, was inserted into a vector to construct pWPXL. pWPXL-Venus-Akaluc, pMD2G, and pCMV deltaR8.74 were transfected into LentiX-293T cells (TaKaRa Bio Inc, Shiga, Japan) using Lipofectamine 2000 (Thermo Fisher Scientific). After 3 days, the supernatant was collected, centrifuged, and filtered through a 0.45-µm filter before introducing into MSCs. Then, Venus-positive cells (Akaluc-MSCs) and Venus(+)/SSEA-3(+) double-positive cells (Akaluc-Muse cells) were sorted by FACS. To collect Akaluc Muse cells, Akaluc-MSCs were incubated with rat anti-SSEA-3 IgM antibody (1:1000; BioLegend) as the primary antibody and allophycocyan-conjugated goat anti-rat IgM antibody (1:100; Jackson ImmunoResearch Laboratories) as the secondary antibody. Cells were intravenously injected at 24 h after AAD induction. Mice were divided randomly into 3 groups and received 0.2 ml saline containing either; 1) 50,000 Akaluc-Muse cells (Akaluc-Muse group), 2) 750,000 Akaluc-MSCs (Akaluc-MSC-750K group), and 3) no cells (vehicle group). Three mice were used for each group at each time-point. For HLA-G KD-Muse group, mice received an injection of 50,000 HLA-G shRNA-Akaluc-Muse cells (described below) in 0.2 ml saline (HLA-G KD-Muse group) and inspected by IVIS Spectrum CT at 1 week. Three mice were used the HLA-G KD-Muse group.
Contrast-enhanced CT images of the mice were obtained before IVIS imaging to confirm the site of the aortic dissection (Fig. S3). CT images used for this study were provided in the repository32 URL: https://www.scidb.cn/en/detail?dataSetId=f1b7da634c334aaca05609c88740d65b. Localization of Muse cells and MSCs was assessed by IVIS Spectrum CT (Perkin Elmer, Waltham, MA) at 1, 4, and 8 weeks after cell injection. Mice were killed by an overdose of isoflurane and organs were removed 1 h after intravenous injection of 0.2 ml of 15-mM AkaLumine-HCl, an artificial substrate. Images of each organ were taken by IVIS within 1 h after immersion in 2 ml of 0.5-mM AkaLumine-HCl. Local distribution of Muse cells and MSCs was assessed on the basis of average radiance (photons/s/cm2/Sr; mean of organ surface luminance) and signal strength was assessed by Total Flux (photons/s; light intensity). Living Image software (ver.4.5, PerkinElmer, Waltham, MA) was used for quantification. The value of the total flux of each organ in the Akaluc-Muse and Akaluc-MSC-750K groups was obtained by subtracting the total flux (autofluorescence) of each organ in the vehicle group.
Histologic assessment
Cells were intravenously injected within 24 h after induction of AAD. Mice were divided into 2 groups: 1) 50,000 GFP-Muse cells in 0.2 ml saline (GFP-Muse group), and 2) 750,000 GFP-MSC in 0.2 ml saline (GFP-MSC-750K group). Three animals were used for each group.
Mice were killed by an overdose of isoflurane anesthesia and perfused transcardially (right ventricle) with 4% paraformaldehyde in phosphate buffered saline (PBS). The whole aorta from the ascending to the terminal aorta was dissected out, divided into 8 pieces, and embedded in OCT compound (Sakura Finetek USA, Inc, Torrance, CA). Cryo-sections (6 μm) for fluorescent immunostaining were cut using a microtome cryostat (Leica, Wetzlar, Germany). The whole aorta was embedded in paraffin (Tissue-Tek VIP 5 Jr, Sakura Finetek Japan Co. Ltd, Tokyo, Japan). Cross-sections (3 μm) for Elastica-Masson staining and immunostaining were cut using a microtome (Retoratome REM-710, Yamato Kohki Industrial Co. Ltd, Saitama, Japan).
Cryo-sections were double stained by first incubating with 2 primary antibodies, mouse anti-αSMA (alpha smooth muscle actin) IgG antibody (1:200; MS-113, Thermo Fisher Scientific) and rabbit anti-GFP IgG antibody (1:500; MBL598, Medical & Biological Laboratories Co., Ltd, Nagoya, Japan), and then washed and incubated with 2 secondary antibodies Alexa Fluor 680-conjugated donkey anti-mouse IgG antibody (1:500; A10038, Thermo Fisher Scientific) and Alexa Fluor 594-conjugated donkey anti-rabbit IgG antibody (1:500; 711-586-152, Jackson ImmunoResearch Laboratories). Another double staining was performed with goat anti-CD31 IgG antibody (1:50; sc-1506, Santa Cruz Biotechnology Inc) and rabbit anti-GFP IgG antibody (1:500), followed by incubation with 2 secondary antibodies, Alexa Fluor 647-conjugated donkey anti-goat IgG antibody (1:500; 705-606-147, Jackson ImmunoResearch Laboratories) and Alexa Fluor 594-conjugated donkey anti-rabbit IgG antibody (1:500; 711-586-152, Jackson ImmunoResearch Laboratories). The double-positive cells were quantified by the cell number per unit total intimal and medial area and were calculated as the average of 5 sections. An A1 Laser confocal microscope (Nikon, Tokyo, Japan) was used for observation.
CD45 immunostaining was performed for leukocyte infiltration by using the Muse, MSC-750K and vehicle groups. Paraffin sections were stained with anti-mouse CD45 rat IgG2b antibody (1:10; 550539, BD Pharmingen, San Diego, CA), followed by horseradish peroxidase (HRP)-conjugated donkey anti-rat IgG antibody (1:500; 712-036-153, Jackson ImmunoResearch Laboratories, Inc.). Sections were incubated with 3,3’-DAB (o49-22831, FUJIFILM Wako Pure Chemical Corporation, Osaka, Japan) for detecting HRP. Positive cells were counted per dissected aortic area and the mean of 5 areas from each sample was calculated. A BX53 Microscope (Olympus, Tokyo, Japan) was used for observation.
Light sheet analysis
The dissected aorta was assessed by three-dimensional (3D) staining and imaging. The aortic samples of the GFP-Muse group at 2 weeks were prepared in the same way as for histologic assessment. The aortic samples fixed by 4% paraformaldehyde in PBS were washed in PBS for 10 min and then incubated in depigmentation solution34 (16%(v/v) dimethyl sulfoxide (DMSO), 16%(v/v) H2O2 in PBS) with rotation overnight at room temperature. After washing 3 times at room temperature for 20 min in PBS, the samples were treated with antigen retrieval solution34 (4%[w/v] sodium dodecyl sulfate in 200 mM borate) at 54 °C overnight. Following 3 days of reaction with goat anti-GFP IgG antibody (Abcam, ab6673, 1:100) in antibody reaction solution (10%(w/v) FBS, 0.02%(w/v) sodium azide, 1% (w/v) bovine serum albumin, 0.2% (v/v) Triton X-100 and 5% (v/v) DMSO in PBS), the samples were washed with PBS. The samples were further reacted with Alexa Fluor 488 Anti-Goat IgG (Jackson ImmunoResearch, 705-545-003, 1:200) and propidium iodide (Invitrogen, P3566) then washed with PBS. Finally, the samples cleared by CUBIC-R + 35 were embedded in small glass tubes with agarose and imaged using a light sheet microscope, MuVi-SPIM CS (Luxendo, Heidelberg, Germany). The images were processed with an Image Processor (Luxendo, v3.5.0) and then visualized by Imaris software (Bitplane, v9.5.1).
Assessment for elastic fibers
To identify elastic fibers, Elastica-Masson staining was performed and a BX53 Microscope (Olympus, Tokyo, Japan) was used for observation. The aortic neointimal and medial elastin content was quantified on the basis of the percent area of the elastin compared with the total neointimal and medial areas, which was calculated as the mean of the 5 pieces from each of the aortic samples, as described previously23,36. The quantification was performed as follows: color images of the Elastica-Masson staining were deconvolved (Figs. S4–1) and the aortic adventitia was excluded (Figs. S4–2), leaving the neointima and media (Figs. S4–1 red color part). After adjusting the color threshold of the elastic fibers, the elastin content was distinguished (Fig. S4–4 red color part). The calculation (area of (4) red color parts) / (area of (3) red color parts) ×100 represented the percent of elastin area in the neointima and media. Image J software (ver.1.52, National Institutes of Health, Bethesda, MD, https://imagej.net/Citing) was used.
In addition to the Muse and MSC-750K groups, elastin KD-Muse cells and shRNA-control Muse cells were prepared. The latter two groups received intravenous injection of 50,000 cells in 0.2 ml saline within 24 h after induction of AAD. Ten mice were used for this group.
Transmission electron microscopy
The Muse and vehicle groups, as well as the aorta from intact animals (intact group) were prepared. All procedures were performed as described previously37. In brief, under ether anesthesia, animals were perfused through the initial portion of the aorta with 300 ml of 2.5% glutaraldehyde and 2% paraformaldehyde in 0.1 M phosphate buffer (pH 7.4), and then the aorta was dissected out. After washing and subsequent postfixation in phosphate-buffered 1% OsO4 (pH 7.4), dehydration in an ascending series of ethanol solutions and passage through propylene oxide, the blocks were embedded in EPON 812. Thin sections were stained in lead and uranyl salt solutions.
Measurement of S1P levels
One day after cell injection, the peripheral blood and aortic tissues were collected. The blood was infused into a heparinized tube and centrifuged at 1200 g for 15 min at 4 °C. The supernatant was used as plasma. After blood collection, model mice were killed by an overdose of isoflurane anesthesia and aortic tissue ( ~ 20 mg) was dissected out. The tissue samples were homogenized with homogenizing buffer (RIPA buffer, protease inhibitor [cOmplete Mini EDTA-free, Roche Diagnostics GmbH, Mannheim, Germany], phosphatase inhibitor [PhosSTOP, Roche]) on ice and centrifuged at 10,000 g for 10 min at 4 °C. The homogenate supernatant was used. Lipid was extracted from 50 µl of plasma or homogenate supernatant using 500 µl of methanol containing 50 pmol of internal standards (C17-S1P, Avanti Polar Lipids, Alabaster, AL). S1P was analyzed by reverse-phase high-pressure liquid chromatography using an L-column 3 C18 column (2 µm, 2.0 × 50 mm; Chemicals Evaluation and Research Institute, Tokyo, Japan) coupled with a QTRAP5500 mass spectrometer (Sciex Inc., Framingham, MA). A binary gradient consisting of solvent A (acetonitrile:methanol:water, 1:1:3, v/v/v, containing 5 mM ammonium acetate and 1% formic acid) and solvent B (2-propanol containing 5 mM ammonium acetate and 1% formic acid) was used. The gradient profile was as follows: 0–5 min, 95% A; 5–16 min, 5–95% B linear gradient; 16–20 min, 95% B. The flow rate was 0.2 ml/min, and the column temperature was 40 °C. S1Ps were detected in multiple reaction monitoring mode as follows: S1P (380.2 → 264.2) and C17-S1P (366.2 → 250.2) in positive ion mode. Lipids were quantified using MultiQuant version 2.0 (Sciex) and normalized against the internal standard. The protein concentration (μg/mL) was measured using a Bradford protein assay (Thermo Fisher Scientific). The S1P level of the homogenate supernatant was expressed as nanograms per milligram total protein. Three samples were analyzed for each group.
Migration assay toward AAD tissue
Mice were killed 1 day after induction of AAD by an overdose of isoflurane anesthesia. The AAD tissue (~20 mg) was dissected and plated onto a 6-well Boyden chamber (ThinCert 6-Well Plate insert, 8.0 μm, Greiner Bio-One International GmbH, Kremsmunster, Austria) in Dulbecco’s Modified Eagle Medium supplemented with 10% FBS and kanamycin. Non-Muse MSCs (~712,000 cells) were plated onto 6-well plate dishes with the same medium as the insert plate. Dissected aortic tissue and non-Muse MSCs were co-cultured for 24 h. Aortic tissue was then homogenized for measurement of S1P in the supernatant, as described above.
Statistics and reproducibility
Sample size (n) and data were shown in each figure and supplementary data. Statistical analyses were performed using JMP Pro 17 software (SAS Institute Inc., Cary, NC). Comparison of 2 groups was performed using Student t-test. The comparison of three or more groups was performed by using Steel–Dwass test. The statistical tests were two-sided. Continuous variables are expressed as mean ± standard deviation (SD). A p-value of less than 0.05 was considered significant.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Mortality rate, aortic diameter dilation and in vivo-dynamics of injected cells in the Stanford B-AAD mouse
Human Muse cells were collected from human BM-MSCs as SSEA-3(+) by magnetic-activated cell sorting as described previously (Fig. S1)21,23. Stanford type B-AAD model mice were created according to the previously described method with minor modifications30,31. Male 4-week-old mice (C57BL/6NCrS1c) were supplied with drinking water containing β-aminopropionitrile fumarate salt (BAPN) for 4 weeks, and then human angiotensin II (Ang II) was continuously administered by an osmotic mini pump implanted subcutaneously in the back skin for 24 h. The sham group received saline instead of Ang II.
Approximately 20% of AAD model mice died within 24 h after Ang II administration. The dissection of those mice clarified that almost all of the deaths were due to the rupture of the dissected thoracic aorta. Survived mice exhibited Stanford B-AAD in contrast-enhanced computed tomography (CT) imaging. Aortic dissection was also confirmed by macroscopic observation to have started at the distal site of the left subclavian artery extending to the descending thoracic and abdominal aorta, ranging from the level of the left ventricle to the renal artery bifurcation. Contrast-enhanced CT within 24 h after onset showed false lumen patency in almost all AAD model mice (Fig. 1b). Elastica-Masson staining confirmed the dissection of the aortic wall at the media, separating the aorta into 2 cavities (Fig. 1b).
Mice confirmed to have Stanford type B-AAD by CT scan were divided randomly into 4 groups and received 0.2 ml saline containing either 50,000 Muse cells (Muse group, n = 10), 50,000 MSCs (MSC-50K group, n = 10), 750,000 MSCs that contain the same number of Muse cells as the Muse group (MSC-750K group, n = 10), no cells (vehicle group, n = 10). The average diameter of the dissected aorta did not differ significantly among the groups (Fig. S5).
Survival rate was examined for up to 8 weeks after cell injection in each group by the Kaplan-Meier method. The mortality rate at 8 weeks was the lowest in the Muse group (8.8%), followed by the MSC-750K (19.4%) and vehicle (33.3%) groups, and the highest in the MSC-50K group (40.0%) (Fig. 1c). The better survival rate in the Muse group compared with the other groups was due to the avoidance of ruptures of the dissected aorta. The odds ratio for death was 5.17 (95% CI: 1.26–21.11, P = 0.022) between the vehicle and Muse groups, and 6.89 (95%CI: 1.22–38.99, P = 0.029) between the MSC-50K and Muse groups. No significant difference was detected between the MSC-750K and Muse, the vehicle and MSC-750K or the vehicle and MSC-50K groups. Because the MSC-750K group had better survival than the MSC-50K group and the data of the MSC-50K group was close to that of the vehicle group (P = 0.20) (Fig. 1c), the MSC-750K group was selected as representative of the two MSC groups in subsequent experiments.
Macroscopic observation of the dissected aorta at 8 weeks confirmed the dissected area of the aorta in the vehicle, MSC-750K, and Muse groups (Fig. 1d). In contrast-enhanced CT was used to measure the diameter of the dissected aorta on the day of dissection (before cell injection, 0 day), 4 and 8 weeks after cell injection (Fig. 1e). The expansion rate of the dissected aortic diameter was calculated as the ratio to that on day 0 (Fig. 1f). At 4 weeks, the dilation ratio of the aortic diameter was 1.23 ± 0.10 times larger in the vehicle group; 1.15 ± 0.10 times in the MSC-750K group, 1.05 ± 0.02 times in the Muse group, and 1.00 ± 0.03 times in the sham group. At 8 weeks, the dilation ratio of the aortic diameter was 1.36 ± 0.07, 1.23 ± 0.11, 1.09 ± 0.02 and 1.02 ± 0.03 times larger in the vehicle, MSC-750K, Muse and sham groups (Fig. 1f). In both 4 and 8 weeks, statistical significances were seen between the vehicle and Muse/sham groups, and between MSC-750K and Muse/sham groups. Therefore, the Muse group showed statistically meaningful improvement of the aortic diameter increase compared to the vehicle and MSC-750K groups. However, the aortic diameter in the Muse group was consistently larger than the sham group (p < 0.01) at 4 and 8 weeks. In 8 weeks, the statistical significance was seen between the vehicle and MSC-750K groups (Fig. 1f).
Venus-Akaluc GFP-labeled cells were intravenously injected 24 h after the onset of AAD and the in vivo dynamics of injected cells were evaluated. The vehicle group was used to define the baseline level at each time-point. Contrast-enhanced CT images were obtained before IVIS imaging to confirm the site of the aortic dissection (Fig. S3). CT images used for this study were provided in the repository32 URL: https://www.scidb.cn/en/detail?dataSetId=f1b7da634c334aaca05609c88740d65b.
In the Muse group, the signal in the aorta was detectable in the area ranging from the distal aortic arch where the dissection started to the descending aorta, including the upper abdominal aorta at 1, 4, and 8 weeks (Fig. 2a, c, e), and the overall signal gradually increased according to the time point. The signal in the lung and other organs was consistently under the detection limit at 1, 4, and 8 weeks, except in the femoral and tibial bones with weaker signal than that in the aorta only at 1 week (Figs. 2a, c, e, S6).
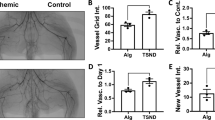
Luminosity (photons/s/cm2/Sr; mean of organ surface luminance) of the aorta with Stanford B acute aortic dissection (AAD), lung, and bone (femoral and tibial) was measured by IVIS Spectrum CT at 1 week (a), 4 weeks (c), and 8 weeks (e) after cell administration in the Muse group (AAD mice administered with Venus-Akaluc GFP-labeled 50,000 Muse cells), MSC-750K group (AAD mice administered with Venus-Akaluc GFP-labeled 750,000 mesenchymal stem cells) and HLA-G KD-Muse group (AAD mice administered with Venus-Akaluc GFP-labeled HLA-G gene knockdown-50,000 Muse cells). Images of other organs at 1 week is shown Fig. S6. Total luminosity (photons/s) of each organ at 1 week (b), 4 weeks (d), and 8 weeks (f) after cell administration is shown. All groups were n = 3. Total luminosity of Aorta at 1 week; the Muse group vs the MSC-750K group: P = 0.19, the Muse group vs the HLA-G KD-Muse group: P = 0.19, the MSC-750K group vs the HLA-G KD-Muse group: P = 0.19. Total luminosity of Lung at 1 week; the Muse group vs the MSC-750K group: P = 0.15, the Muse group vs the HLA-G KD-Muse group: P = 1.00, the MSC-750K group vs the HLA-G KD-Muse group: P = 0.15. Total luminosity of Bone at 1 week; the Muse group vs the MSC-750K group: P = 0.90, the Muse group vs the HLA-G KD-Muse group: P = 0.19, the MSC-750K group vs the HLA-G KD-Muse group: P = 0.39. Total luminosity of Aorta at 4 weeks; the Muse group vs the MSC-750K group: P = 0.0073. Total luminosity of Aorta at 8 weeks; the Muse group vs the MSC-750K group: P = 0.015. *P < 0.05; **P < 0.01 by Steel–Dwass test (b) and t-test (d, f). The error bars are expressed as standard deviation (SD).
In the MSC-750K group, the signal in the aorta was significantly lower than that in the Muse group (Fig. 2a, c, e). At 1 week, the lung exhibited the highest signal among all the organs and the femoral/tibial bones exhibited signals comparable to that in the aorta at 1 week, but all of those became under the detection limit at 4 and 8 weeks (Fig. 2a, c, e).
Muse cells are reported to express HLA-G, associated with immune tolerance in the placenta19. We generated HLA-G shRNA-Akaluc-Muse cells to knock down HLA-G expression (HLA-G KD-Muse cells) (Fig. S2), and examined the in vivo-dynamics at 1 week. In the Muse group, the signal of the aorta (1461 ± 128 p/s) was higher than that of the bone (793 ± 121 p/s), whereas, in the HLA-G KD-Muse group, those of the aorta (245 ± 111 p/s) and bone (257 ± 124 p/s) were close to each other and were both lower than that of the aorta of the Muse group (Fig. 2a, b). However, there was no statistically significant difference in the aorta signals among the Muse, MSC-750K, and HLA-G KD-Muse groups or between the signals of the aorta and bone in both the Muse and HLA-G KD-Muse groups, respectively (Fig. 2a, b).
Comparison of the total light intensity of Akaluc-GFP Venus in each organ revealed that the signals in the aorta were not statistically significantly different among the 3 groups at 1 week (P = 0.19 for each) (Fig. 2b). The ratio in the aorta between the Muse and MSC-750K groups was 3.85 times (P < 0.01) at 4 weeks and the ratio was maintained at 3.68 times (P < 0.05) at 8 weeks (Fig. 2d, f). In the lung, the signal was only detectable in the MSC-750K group and not in the Muse and HLA-G KD-Muse groups at 1 week (both at P < 0.05). No significant difference was detected in the lower limb bones between the Muse and MSC-750K groups (P = 0.49), but was 3.09 times lower in the HLA-G KD-Muse group (P < 0.05) than in the Muse group at 1 week (Fig. 2b, d, f).
In vivo-differentiation and elastin production of injected cells
GFP-labeled cells were used for histologic analysis. The ratio of α-smooth muscle actin (SMA; smooth muscle cell marker)(+) among GFP(+) cells in the media of the Muse group aorta was 53.7 ± 7.2%, 5.32 times more than that of the MSC-750K group aorta (10.1 ± 1.9%) at 2 weeks (P < 0.001). A similar trend was seen at 4 and 8 weeks; 3.74 times higher in the Muse group than in the MSC-750K group at 4 weeks (P < 0.01), and 4.04 times higher in the Muse group than in the MSC-750K group at 8 weeks (P < 0.01) (Fig. 3a). The number of GFP(+)/α-SMA(+) cells per area (mm2) in the media in the Muse group had 5.35 times more than that in the MSC-750K group at 2 weeks (P < 0.05). At 4 weeks, the Muse group had 5.68 more of these cells than the MSC-750K group (P < 0.001), and the ratio between the 2 groups increased to as high as 6.93 at 8 weeks (P < 0.001) (Fig. 3b). An example of GFP + /α-SMA+ in the media in the Muse group at 4 weeks is shown in Fig. 3c.
a Ratio of GFP(+)/alpha smooth muscle actin (αSMA)(+) cells to the total GFP(+) cells in the media of the aorta with Stanford B acute aortic dissection (AAD) in the Muse group (AAD mice administered with GFP-labeled 50,000 Muse cells) and MSC-750K group (AAD mice administered with GFP-labeled 750,000 mesenchymal stem cells). The Muse group vs the MSC-750K group at 2 weeks: P = 0.0005, at 4 weeks: P = 0.0038, at 8 weeks: P = 0.0043. b Number of GFP( + )/αSMA(+) cells per area of the dissected aorta (mm2). The Muse group vs the MSC-750K group at 2 weeks: P = 0.024, at 4 weeks: P = 0.0010, at 8 weeks: P = 0.0002. c Arrowheads indicate GFP( + )/αSMA(+) cells in the media of the dissected aorta wall of the Muse group at 4 weeks after cell administration. *: false lumen. Scale bar: 200 μm (low magnification), 50 μm (high magnification), 10 μm (super high magnification, insets). d Ratio of GFP( + )/CD31(+) cells to total GFP(+) cells in the intima and neointima. The Muse group vs the MSC-750K group at 2 weeks: P = 0.032, at 4 weeks: P = 0.038, at 8 weeks: P = 0.0017. e Number of GFP( + )/CD31(+) cells per area of the dissected aorta. The Muse group vs the MSC-750K group at 2 weeks: P = 0.049, at 4 weeks: P = 0.017, at 8 weeks: P = 0.018. f Arrowheads indicate GFP( + )/CD31(+) cells in the dissected aorta of the Muse group at 4 weeks after cell administration. Scale bar: 200 μm (low magnification), 50 μm (high magnification), 10 μm (super high magnification, insets). Muse group (n = 3); MSC-750K group (n = 3). *P < 0.05; **P < 0.01; ***P < 0.001 by t-test (a, b, d, e). The error bars are expressed as standard deviation (SD).
The ratio of cells positive for the endothelial cell marker CD31 among GFP(+) cells in the intima and neointima of the aortic wall was also calculated. At 2 weeks, the ratio of CD31(+) among GFP(+) cells in the Muse group was 3.1 times higher than that in the MSC-750K group (P < 0.05). The difference between the 2 groups was 1.9 times (P < 0.05) and 3.46 times (P < 0.01) higher in the Muse group rather than the MSC-750K group at 4 and 8 weeks, respectively (Fig. 3d). The number of GFP( + )/CD31(+) cells in the intima and neointima per area (mm2) of the aorta in the Muse group was 7.00 times higher than that in the MSC-750K group at 2 weeks (P < 0.05), and similarly 5.00 times (P < 0.05) and 7.41 times (P < 0.05) higher in the Muse group rather than the MSC-750K group at 4 and 8 weeks, respectively (Fig. 3e). An example of GFP + /CD31+ cells in the neointima of the Muse group at 4 weeks is shown in Fig. 3f.
The aorta of the Muse group was subjected to light sheet analysis at 8 weeks for 3D histologic analysis. The difference in the diameter between the outer surface of the aorta (light red in Fig. 4) and the inner surface of the aorta (the lumen, red in Fig. 4) indicates the dissected area (white arrowhead and arrow) (Fig. 4). The aortic diameter was enlarged at the dissected part and comprised the larger false lumen and smaller true lumen with blood flow entrance and exit channels (Fig. 4, Supplementary Video 1). The distribution of GFP(+)-Muse cells was mostly confined to the dissected area and not to the intact area, suggesting the specific engraftment of intravenously injected Muse cells to the damaged site in the 3D analysis (Fig. 4). The movie of the light sheet data is available in Supplementary Video 1.
3D image of the aorta (arch〜descending) with Stanford B acute aortic dissection (AAD) in the Muse group (AAD mice administered with GFP-labeled 50,000 Muse cells) at 2 weeks after cell administration. The whole aortic tissue is shown in pink, the aortic lumen is shown in red, and GFP-Muse cells are shown in green. The aorta was dissected between the distal arch to the descending aorta. The dissected portion had 2 lumens; true and false lumens. Arrowheads indicate the entry site; channels of the entrance of the bloodstream (true lumen to false lumen). Arrows indicate re-entry site; channels of the exit of the bloodstream (false lumen to true lumen). The distribution of GFP-Muse cells was shown to be concentrated on the dissected aorta and not on the intact aorta.
The amount of elastic fibers in the media and neointima was evaluated by Elastica-Masson staining at 8 weeks, according to previous reports (Fig. 5a)23,36. The percent elastin area was measured in the media and neointima (Fig. S4). The elastin area comprised 45.9 ± 1.2% of the media in the sham group, 15.6 ± 2.0% of the media and neointima in the vehicle group, 15.5 ± 3.7% in the MSC-750K group, and 16.1 ± 0.7% in the Muse group at 1 day after cell injection, with no significant difference among them (P < 0.05) (Fig. 5b). At 1 week, the elastin area was 15.7 ± 1.8%, 17.2 ± 1.3% and 19.1 ± 0.4% in the vehicle, MSC-750K and Muse groups, respectively, without significance among the three groups (Fig. 5b). At 4 weeks, the Muse group (30.4 ± 2.1%) differed significantly from the vehicle (20.3 ± 2.1%) and MSC-750K (22.7 ± 2.0%) groups (both P < 0.05), while the elastin area did not differ statistically between the vehicle and MSC-750K groups (P = 0.25). At 8 weeks, the same tendency was observed in the Muse (33.6 ± 1.9%), MSC-750K (27.8 ± 1.7%) and vehicle (21.5 ± 2.0%) groups with the Muse group having a significantly greater area than the other groups (P < 0.05), but a smaller area than the sham group (P < 0.05) (Fig. 5b). Different from 4 weeks, the MSC-750K group was superior to the vehicle group (p < 0.05). Overall, the Muse group exhibited the highest percent elastin area in the media and neointima among the 3 groups at both 4 and 8 weeks.
a Elastica-Masson staining of the descending aorta with or without Stanford B acute aortic dissection (AAD) in the sham group (mice without AAD), vehicle group (AAD mice administered with no cells), MSC-750K group (AAD mice administered with 750,000 mesenchymal stem cells) and Muse group (AAD mice administered with 50,000 Muse cells) at 8 weeks after cell administration. Scale bar: 200 μm. b Elastin area in the neointima and media of the dissected aorta by Elastica-Masson staining in each group (n = 3 for 1 day and 1 week, n = 6 for 4 and 8 weeks). Elastin area at 4 weeks; the Sham group vs the Vehicle group: P = 0.026, the Sham group vs the MSC-750K group: P = 0.026, the Sham group vs the Muse group: P = 0.026, the Vehicle group vs the MSC-750K group: P = 0.25, the Vehicle group vs the Muse group: P = 0.026, the MSC-750K group vs the Muse group: P = 0.026. Elastin area at 8 weeks; the Sham group vs the Vehicle group: P = 0.026, the Sham group vs the MSC-750K group: P = 0.026, the Sham group vs the Muse group: P = 0.026, the Vehicle group vs the MSC-750K group: P = 0.026, the Vehicle group vs the Muse group: P = 0.026, the MSC-750K group vs the Muse group: P = 0.026. c Elastin gene expression level in naive Muse cells (Muse), control vector-introduced Muse cells (shRNA-control Muse), and elastin shRNA-introduced Muse cells (elastin KD-Muse) examined by digital droplet PCR. The Muse group vs the shRNA-control Muse group: P = 0.42, the Muse group vs the Elastin KD-Muse group: P = 0.032, the shRNA-control Muse group vs the Elastin KD-Muse group: P = 0.033. d Diameter of the dissected aorta measured by contrast-enhanced CT. White bars indicate the maximum minor-axis diameter of the dissected aorta. The Elastin KD-Muse group: AAD mice administered with Elastin gene knockdown-50,000 Muse cells. e The dissected aorta diameter at each time-point in each group (n = 10). The dilation ratio of the dissected aorta at 4 and 8 weeks after cell administration was calculated as the ratio to that on the first day of dissection. The dilation ratio at 4 weeks; the MSC-750K group vs the Muse group: P = 0.0076, the MSC-750K group vs the Elastin KD-Muse group: P = 0.61, the Muse group vs the Elastin KD-Muse group: P = 0.0005. The dilation ratio at 8 weeks; the MSC-750K group vs the Muse group: P = 0.0011, the MSC-750K group vs the Elastin KD-Muse group: P = 0.98, the Muse group vs the Elastin KD-Muse group: P = 0.0005. f The ratio of the elastin area to the intima and media of the AAD-aorta at 8 weeks after cell administration measured by Elastica-Masson staining. All groups were n = 6. Elastin area at 8 weeks; the MSC-750K group vs the Muse group: P = 0.014, the MSC-750K group vs the Elastin KD-Muse group: P = 0.28, the Muse group vs the Elastin KD-Muse group: P = 0.014. g Transmission electron microscopy of the aorta from the intact mouse (mice without AAD), as well as from the Muse and vehicle groups. *: elastic fibers. #: area of collagen fibers. *P < 0.05; **P < 0.01; ***P < 0.001 by Steel–Dwass test (b, c, e, f). The boxplot indicates the interquartile range (top: the third quartile; bottom: the first quartile) with the whiskers extending to the most extreme points within 1.5 times the interquartile range (outliers beyond 1.5 times the interquartile range are also shown) and with a horizontal line and cross mark respectively indicating the median and mean (b, e). The error bars are expressed as standard deviation (SD) (c, f).
We examined how elastin production affected on the dilation of aorta in the Muse group. Muse cells introduced with elastin-shRNA lentivirus (Elastin KD-Muse cells) decreased the expression of elastin gene by ~51% and ~48% of that in naïve and shRNA-control Muse cells (both P < 0.05) (Fig. 5c). No significant difference seen between naïve and shRNA-control Muse cells (P = 0.42) (Fig. 5c). The aortic diameter expansion rate was measured at 4 and 8 weeks compared with day 0 by contrast-enhanced CT imaging (Fig. 5d). Compared to the Muse group (dilation ratio 1.05 ± 0.02 times), the Elastin KD-Muse (1.16 ± 0.05) (P < 0.001) and the MSC-750K (1.15 ± 0.10) (P < 0.01) groups showed significant greater dilation, while the latter two groups did not show significant difference between them (P = 0.61) at 4 weeks. The similar trend was seen in 8 weeks. Compared to the Muse group (dilation ratio 1.09 ± 0.02 times), the Elastin KD-Muse (1.22 ± 0.04) (P < 0.001) and the MSC-750K (1.23 ± 0.11) (P < 0.01) groups showed significant greater dilation, while the latter two groups did not show significant difference between them (P = 0.98) (Fig. 5e).
Percent neointimal and medial elastin area measured by Elastica-Masson staining at 8 weeks was lower in the Elastin KD-Muse group (29.4 ± 1.8%) than in the Muse group (33.6 ± 1.9%; P < 0.05) and was rather similar to that in the MSC-750K group (27.8 ± 1.7%; P = 0.28) (Fig. 5f). There was significant difference between the Muse and MSC-750K groups (P < 0.05) (Fig. 5f).
Transmission electron microscopy at 8 weeks revealed that the organization of elastic fibers in the neointima of the aorta in the Muse group was similar to that in the media of the intact aorta in their thickness, alignment, and morphology, whereas it was disorganized and irregular in the vehicle group (Fig. 5g).
S1P concentration and CD45+ cell infiltration in the Stanford B-AAD aorta
Selective homing of Muse cells to damaged tissue is reported to be mainly controlled by the axis of S1P, produced by damaged cells, and S1P receptor 2, expressed on Muse cells19. If so, a critical question remains: because the MSC-750K group contains the same number of Muse cells as the Muse group, why did the Muse cells in the MSC-750K group not efficiently home to the AAD aorta (Fig. 2a, c, e) or inhibit the expansion of the AAD aorta (Fig. 1f). The difference between the Muse and MSC-750K groups is the presence of a large amount of non-Muse MSCs negative for SSEA-3, which comprise a majority ( ~ 98%) of the cells in the MSC-750K group.
To address this question, we created 3 groups (sham, vehicle, and non-Muse [receiving 712,000 SSEA-3(−) non-Muse MSCs]) and examined how non-Muse MSCs affected the plasma S1P level after intravenous injection. One day after cell injection, there were no statistically significant differences in the plasma S1P levels and S1P concentrations (ng/mg protein) of the AAD-aorta homogenate among the 3 groups (Fig. 6a, b).
a Plasma sphingosine-1-phosphate (S1P) level in mice blood with or without Stanford B acute aortic dissection (AAD) in the sham group (mice without AAD), vehicle group (AAD mice administered with no cells) and non-Muse group (AAD mice administered with 712,000 non-Muse mesenchymal stem cells which are negative for stage-specific embryonic antigen-3) at 1 day after cell administration. All groups were n = 3. The Sham group vs the Vehicle group: P = 0.19, the Sham group vs the non-Muse group: P = 0.39, the Vehicle group vs the non-Muse group: P = 0.19. b S1P level of the dissected aorta homogenate supernatant in each group (n = 3) at 1 day after cell administration. The Sham group vs the Vehicle group: P = 0.19, the Sham group vs the non-Muse group: P = 1.00, the Vehicle group vs the non-Muse group: P = 0.19. c Schematic diagram of co-culture using the Boyden chamber. S1P level of the upper chamber, which contains the dissected aorta fragment, was measured at 24 hr after co-culture in the AAD-aorta only group (aorta at 1 day after AAD onset was co-cultured with no cells) and non-Muse/AAD-aorta group (aorta at 1 day after AAD onset was co-cultured with 712,000 non-Muse mesenchymal stem cells which are negative for stage-specific embryonic antigen-3). Both groups were n = 3. The AAD-aorta only group vs the non-Muse/AAD-aorta group: P = 0.027. d Arrowheads indicate CD45+ cells in the AAD-aorta in each group (n = 3) 1 day after cell administration. The MSC-750K group: AAD mice administered with 750,000 mesenchymal stem cells. The Muse group: AAD mice administered with 50,000 Muse cells. Cells outside of the dashed line were not counted. The dashed line was ~40 μm away from the outermost elastic fiber. *: false lumen. Scale bar: 200 μm (upper), 20 μm (lower). e Number of CD45+ cells per dissected aortic area. All groups were n = 3. The Vehicle group vs the MSC-750K group: P = 0.19, the Vehicle group vs the Muse group: P = 0.19, the MSC-750K group vs the Muse group: P = 0.90. *P < 0.05 by Steel–Dwass test (a, b, e), t-test (c). The error bars are expressed as standard deviation (SD).
The effect of non-Muse MSCs on S1P production in damaged tissue was then examined in a Boyden chamber co-culturing 712,000 non-Muse MSCs in the lower chamber and AAD-aortic tissue at 1 day after onset in the upper chamber, measuring the S1P concentration of the AAD tissue supernatant at 24 h (non-Muse/AAD-aorta). For a control, no cells were supplied to the lower chamber and AAD-aortic tissue was placed at the upper chamber and cultured for 24 h (AAD-aorta only) (Fig. 6c). The S1P concentration in the non-Muse/AAD-aorta was lower than that in the AAD-aorta only with statistical significance (P < 0.05). This suggested that S1P production in the AAD-aortic tissue was substantially reduced by the presence of non-Muse MSCs (Fig. 6c).
Because S1P induces inflammatory cell infiltration38, we evaluated the extent of CD45(+) white blood cell infiltration at 1 day after cell injection in the vehicle, MSC-750K, and Muse groups (Fig. 6d). The CD45(+) cell infiltration was similar between the Muse and MSC-750K groups (P = 0.90) and lower in both groups than in the vehicle group (both at P = 0.19; Fig. 6e).
Discussion
This study demonstrated for the first time to the best of our knowledge the therapeutic effects of intravenously administered human Muse cells in mouse Stanford B-AAD without immunosuppressant treatment. The new findings are as follows:
The rate of death caused by aortic rupture in the vehicle group, 33.3% at 8 weeks, was significantly improved to 8.8% in the Muse group (p < 0.05).
In-vivo dynamics and 3D-histologic analysis exhibited selective homing of Muse cells to the AAD region and not to other regions in the aorta or to other organs. Muse cells differentiated in vivo into α-SMA(+) cells in the media and CD31(+) cells in the intima in the AAD-tissue, and remained in the tissue until 8 weeks without immune rejection.
Muse cells contributed to reinforcement of the aortic wall by producing and organizing elastic fibers, as demonstrated by Elastica-Masson staining, electron microscopy, and elastin-KD Muse cell experiments. When elastic fiber synthesis was knocked down in Muse cells, improvement of the aortic diameter expansion dropped to almost the same level as that in the MSC-750 group. Since elastic fibers structurally reinforce the aorta, the lower mortality rate in the acute phase and suppression of the aortic diameter expansion in the Muse group might be due in part to the successful production and organization of elastic fibers.
HLA-G is associated with immune tolerance in the placenta19. When HLA-G was knocked down, the effect on the specific homing of Muse cells to the AAD-tissue and survival of the cells in the body was insignificant at one week (Fig. 2a, b). Since the HLA-G gene expression was decreased by 44.3% in HLA-G KD-Muse cells compared to naïve Muse cells in ddPCR, as mentioned in the Method section, whether HLA-G is involved in protecting Muse cells from immunologic attack at the acute phase and whether HLA-G is enabling Muse cells to safely home to the damaged tissue after intravenous injection is still open to question. How Muse cells maintain their immune privilege after differentiation in the host tissue for an extended period of time without immunosuppressant remains to be clarified.
A possible explanation for the consistently lower therapeutic effect in the MSC-750K group than the Muse group, despite both groups contained the same number of Muse cells, might be the presence of non-Muse MSCs that occupy ~98% of the total MSC-750K cells. Since S1P receptor 2 was reported to be expressed in non-Muse cells with lower level than that in Muse cells12,19, the presence of a large number of non-Muse cells may compete with Muse cells for receiving S1P in the MSC group. In addition, the presence of non-Muse MSCs substantially reduced S1P production in the AAD-aortic tissue as shown in Fig. 6c. Therefore, the presence of non-Muse MSCs in the MSC-750K group might lead to the inefficient engraftment of Muse cells, thereby preventing adequate replenishment of vascular cells and production of elastic fibers in the AAD tissue. As seen in the lower infiltration of CD45+ cells into the AAD-tissue in MSC-750K group, non-Muse cells were suggested to exert anti-inflammatory effect (Fig. 6d, e), which might also decrease the S1P level. Indeed, non-Muse MSCs have trophic and anti-inflammatory effects14,17,18,19, but they do not selectively home to damaged sites, nor do they directly contribute to structural repair/reconstruction by differentiation into tissue comprising cells to replace damaged/dying cells, unlike Muse cells14,17,18,19. The accumulation of MSCs in the lung at 1 week after intravenous injection might be due to capillary trap rather than selective migration to the lung19,39,40. As reported, the disappearance of MSCs from the lung at 4 weeks might be due to rejection, partly due to the low HLA-G expression19. In summary, small doses of purified Muse cells were suggested to be therapeutically more effective than large doses of MSCs for treating AAD.
Muse cells produce factors relevant to anti-inflammation and immunomodulation, such as prostaglandin E2, interleukin-10, matrix metalloproteinase-2, hepatocyte growth factor, and indoleamine-2,3-dioxygenase17,40. These factors are considered effective for Stanford B-AAD. On the other hand, searching for new cytokines and factors is a challenge for the future. Consistently, infiltration of CD45(+) cells was lower in the Muse group than in the vehicle group. White blood cell infiltration induces the degradation of elastic and collagen fibers30,41. Thus, the reduced CD45(+) cell infiltration might have also contributed to suppress the aortic diameter expansion.
The therapeutic effect of intravenously administered Muse cells was previously demonstrated in mouse aortic aneurysm23. AAD and aortic aneurysm are both representative aortic diseases, but the pathology decisively differs between them; AAD is triggered by the emergence of an intimal tear followed by extraordinary blood flow into the media, creating acute dissection of the downstream media of the aortic wall accompanied by severe tissue destruction, intensive inflammation, and strong pain1,42. Aortic aneurysm, on the other hand, is generally slowly formed as a result of focal atherosclerotic degeneration of the aortic wall with a chronic time course and is not accompanied by drastic histologic destruction43,44. AAD often progresses dramatically and generates 2 channels for blood flow, leading to direct exposure of an enormous area of the media to the shear stress of blood flow. Therefore, unlike aortic aneurysm, a dissected false lumen creates a totally different harsh microenvironment for homed Muse cells. Whether or not Muse cells engraft and function in such a harsh environment, however, has not been confirmed. In fact, very few previous studies have examined the effects of stem cell therapy for AAD, although several studies have examined the effects of MSCs on degenerative aortic aneurysm45,46,47. Our present study demonstrated for the first time that intravenously administered Muse cells have therapeutic effects in AAD model.
The fact that intravenous injection is the main route for Muse cell treatment is another advantage for clinical application. This is particularly important for AAD where the tissue is severely damaged and difficult to approach directly. Notably, intravenously injected allograft-Muse cells were shown to survive in the host tissue for 6 months without immunosuppression in a rabbit acute myocardial infarction model19. Clinical trials of the application of intravenously injected donor Muse cells for 7 different diseases are currently being conducted all without HLA matching or long-term immunosuppression. No adverse effects have yet been reported26,27. Therapeutic effects have been reported in clinical trials of Muse cell for acute myocardial infarction26. Thus, intravenous injection of donor-derived Muse cells is expected to be applicable to AAD, particularly Stanford B-AAD, in which extension of the dissected aorta gradually progresses and places patients at high risk for surgery involving prosthetic vascular graft replacement.
Data availability
The source data for Figs. 1c, f, 2b, d, f, 3a, b, d, e, 5b, c, e, f, 6a, b, c, e and Supplementary Figs. 2d, 5 and 6 are in the Supplementary Data file. The CT images obtained during this study are deposited in the Science Data Bank32 URL: https://www.scidb.cn/en/detail?dataSetId=f1b7da634c334aaca05609c88740d65b. Further datasets obtained whilst undertaking this study are available from the corresponding author on reasonable request.
References
Nienaber, C. A. & Eagle, K. A. Aortic dissection: new frontiers in diagnosis and management: Part I: from etiology to diagnostic strategies. Circulation 108, 628–635 (2003).
Erbel, R. et al. Diagnosis and management of aortic dissection. Eur. Heart J. 22, 1642–1681 (2001).
Nakashima, Y., Kurozumi, T., Sueishi, K. & Tanaka, K. Dissecting aneurysm: a clinicopathologic and histopathologic study of 111 autopsied cases. Hum. Pathol. 21, 291–296 (1990).
Nakashima, Y., Shiokawa, Y. & Sueishi, K. Alterations of elastic architecture in human aortic dissecting aneurysm. Lab Invest 62, 751–760 (1990).
Bossone, E., LaBounty, T. M. & Eagle, K. A. Acute aortic syndromes: diagnosis and management, an update. Eur. Heart J. 39, 739–749d (2018).
Kaji, S. Acute medical management of aortic dissection. Gen. Thorac. Cardiovasc Surg. 67, 203–207 (2019).
Estrera, A. L. et al. Outcomes of medical management of acute type B aortic dissection. Circulation 114, I384–I389 (2006).
Schwartz, S. I. et al. Predictors of late aortic intervention in patients with medically treated type B aortic dissection. J. Vasc. Surg. 67, 78–84 (2018).
Bicknell, C. D., Riga, C. V. & Wolfe, J. H. Prevention of paraplegia during thoracoabdominal aortic aneurysm repair. Eur. J. Vasc. Endovasc. Surg. 37, 654–660 (2009).
Nienaber, C. A. et al. Endovascular repair of type B aortic dissection: long-term results of the randomized investigation of stent grafts in aortic dissection trial. Circ. Cardiovasc Inter. 6, 407–416 (2013).
Kuroda, Y. et al. Unique multipotent cells in adult human mesenchymal cell populations. Proc. Natl Acad. Sci. USA 107, 8639–8643 (2010).
Sato, T. et al. A novel type of stem cells double-positive for SSEA-3 and CD45 in human peripheral blood. Cell Transpl. 29, 963689720923574 (2020).
Leng, Z. et al. Quantitative analysis of SSEA3+ cells from human umbilical cord after magnetic sorting. Cell Transpl. 28, 907–923 (2019).
Wakao, S., Kushida, Y. & Dezawa, M. Basic characteristics of Muse cells. Adv. Exp. Med Biol. 1103, 13–41 (2018).
Alessio, N. et al. Stress and stem cells: adult Muse cells tolerate extensive genotoxic stimuli better than mesenchymal stromal cells. Oncotarget 9, 19328–19341 (2018).
Squillaro, T. et al. Stem cells and DNA repair capacity: muse stem cells are among the best performers. Adv. Exp. Med Biol. 1103, 103–113 (2018).
Uchida, N. et al. Beneficial effects of systemically administered human muse cells in adriamycin nephropathy. J. Am. Soc. Nephrol. 28, 2946–2960 (2017).
Iseki, M. et al. Muse cells, nontumorigenic pluripotent-like stem cells, have liver regeneration capacity through specific homing and cell replacement in a mouse model of liver fibrosis. Cell Transpl. 26, 821–840 (2017).
Yamada, Y. et al. S1P-S1PR2 axis mediates homing of muse cells into damaged heart for long-lasting tissue repair and functional recovery after acute myocardial infarction. Circ. Res. 122, 1069–1083 (2018).
Wakao, S. et al. Multilineage-differentiating stress-enduring (Muse) cells are a primary source of induced pluripotent stem cells in human fibroblasts. Proc. Natl Acad. Sci. USA 108, 9875–9880 (2011).
Uchida, H. et al. Human muse cells reconstruct neuronal circuitry in subacute lacunar stroke model. Stroke 48, 428–435 (2017).
Fujita, Y. et al. Intravenous injection of muse cells as a potential therapeutic approach for epidermolysis bullosa. J. Invest. Dermatol. 141, 198–202 (2021).
Hosoyama, K. et al. Intravenously injected human multilineage-differentiating stress-enduring cells selectively engraft into mouse aortic aneurysms and attenuate dilatation by differentiating into multiple cell types. J. Thorac. Cardiovasc Surg. 155, 2301–2313 e2304 (2018).
Tanaka, T. et al. Mobilized muse cells after acute myocardial infarction predict cardiac function and remodeling in the chronic phase. Circ. J. 82, 561–571 (2018).
Wakao, S. et al. Phagocytosing differentiated cell-fragments is a novel mechanism for controlling somatic stem cell differentiation within a short time frame. Cell Mol. Life Sci. 79, 542 (2022).
Noda, T., Nishigaki, K. & Minatoguchi, S. Safety and efficacy of human muse cell-based product for acute myocardial infarction in a first-in-human trial. Circ. J. 84, 1189–1192 (2020).
Fujita, Y. et al. Intravenous allogeneic multilineage-differentiating stress-enduring cells in adults with dystrophic epidermolysis bullosa: a phase 1/2 open-label study. J. Eur. Acad. Dermatol Venereol. 35, e528–e531 (2021).
Niizuma, K. et al. Randomized placebo-controlled trial of CL2020, an allogenic muse cell-based product, in subacute ischemic stroke. J. Cereb Blood Flow Metab. 43, 2029-2039 (2023).
Kuroda, Y. et al. Isolation, culture and evaluation of multilineage-differentiating stress-enduring (Muse) cells. Nat. Protoc. 8, 1391–1415 (2013).
Kurihara, T. et al. Neutrophil-derived matrix metalloproteinase 9 triggers acute aortic dissection. Circulation 126, 3070–3080 (2012).
Anzai, A. et al. Adventitial CXCL1/G-CSF expression in response to acute aortic dissection triggers local neutrophil recruitment and activation leading to aortic rupture. Circ. Res. 116, 612–623 (2015).
Repository of CT images in this study. https://www.scidb.cn/en/detail?dataSetId=f1b7da634c334aaca05609c88740d65b.
Iwano, S. et al. Single-cell bioluminescence imaging of deep tissue in freely moving animals. Science 359, 935–939 (2018).
Messal, H. A. et al. Antigen retrieval and clearing for whole-organ immunofluorescence by FLASH. Nat. Protoc. 16, 239–262 (2021).
Susaki, E. A. et al. Versatile whole-organ/body staining and imaging based on electrolyte-gel properties of biological tissues. Nat. Commun. 11, 1982 (2020).
Jones, J. A. et al. Alterations in aortic cellular constituents during thoracic aortic aneurysm development. Am. J. Pathol. 175, 1746–1756 (2009).
Dezawa, M. & Nagano, T. Contacts between regenerating axons and the Schwann cells of sciatic nerve segments grafted to the optic nerve of adult rats. J. Neurocytol. 22, 1103–1112 (1993).
Cartier, A. & Hla, T. Sphingosine 1-phosphate: lipid signaling in pathology and therapy. Science 366, eaar5551 (2019).
Shono, Y. et al. Protection of liver sinusoids by intravenous administration of human Muse cells in a rat extra-small partial liver transplantation model. Am. J. Transpl. 21, 2025–2039 (2021).
Yabuki, H., Wakao, S., Kushida, Y., Dezawa, M. & Okada, Y. Human multilineage-differentiating stress-enduring cells exert pleiotropic effects to ameliorate acute lung ischemia-reperfusion injury in a rat model. Cell Transpl. 27, 979–993 (2018).
Watanabe, R. et al. MMP (Matrix Metalloprotease)-9-producing monocytes enable T cells to invade the vessel wall and cause vasculitis. Circ. Res. 123, 700–715 (2018).
Mussa, F. F. et al. Acute aortic dissection and intramural hematoma: a systematic review. JAMA 316, 754–763 (2016).
Ali, M. U. et al. Screening for abdominal aortic aneurysm in asymptomatic adults. J. Vasc. Surg. 64, 1855–1868 (2016).
Quintana, R. A. & Taylor, W. R. Cellular mechanisms of aortic aneurysm formation. Circ. Res. 124, 607–618 (2019).
Zou, S. et al. Activation of bone marrow-derived cells and resident aortic cells during aortic injury. J. Surg. Res. 245, 1–12 (2020).
Xie, J. et al. Human adipose-derived stem cells suppress elastase-induced murine abdominal aortic inflammation and aneurysm expansion through paracrine factors. Cell Transpl. 26, 173–189 (2017).
Yamawaki-Ogata, A., Hashizume, R., Fu, X. M., Usui, A. & Narita, Y. Mesenchymal stem cells for treatment of aortic aneurysms. World J. Stem Cells 6, 278–287 (2014).
Acknowledgements
This study was supported by a Grant-in-Aid for Scientific Research (C) (K18K087230), a Grant-in-Aid for Scientific Research B (20H04510), and a Grant-in-Aid for Exploratory Research (19H22648), Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Contributions
M.T., Yo.K., Ya.K., S.W., Y.H., and H.S. collected the data. M.T., Yo.K., Ya.K., S.W., and Y.S. analyzed the data. M.D., M.T., and Y.S. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing interest
The authors declare the following competing interests: Yoshihiro Kushida, Shohei Wakao, Yasumasa Kuroda, and Mari Dezawa have a patent for Muse cells (WO2011007900). All other authors have no competing interests to declare.
Peer review
Peer review information
Communications Medicine thanks the anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Takahashi, M., Kushida, Y., Kuroda, Y. et al. Structural reconstruction of mouse acute aortic dissection by intravenously administered human Muse cells without immunosuppression. Commun Med 4, 174 (2024). https://doi.org/10.1038/s43856-024-00597-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s43856-024-00597-6