Abstract
The outcome of this study was to identify 9-year survivors of intertrochanteric fracture at each stage of chronic kidney disease (CKD) and to investigate the risk factors associated with mortality following surgery with proximal femoral nail anti-rotation (PFNA). 443 elderly intertrochanteric fractures underwent PFNA fixation were recruited. Mortality rate was identified until 9 years. We compared the survival time of hip fracture in each stage of CKD. A regression analysis was used to determine the association between risk factors and one-year mortality. The overall median survival time was 7.1 years. The Kaplan–Meier curve was significantly different in each CKD stage especially in CKD5. In addition, the incidence rate of mortality was highest in CKD 5 (17.4%) and the median survival time in CKD 5 was 3.3 years. The multivariate analysis demonstrated that heart disease, operative time > 60 min, presence of pulmonary embolism, and poor to fair Harris hip score were significantly increased mortality. CKD stage 5 is associated with the highest mortality rate and the shortest median time of survival during the 9-year follow up. Patients who have high risk should focus on long-term care planning, including the counseling for their healthcare providers and families.
Similar content being viewed by others
Osteoporotic hip fracture is becoming a major public health concern as the world’s population ages1,2. It has been demonstrated that fragility hip fracture affects ambulatory status, quality of life, functional outcomes, mortality, and resource and financial costs spent in the health care system3,4,5,6. The mortality rate of osteoporotic hip fracture has risen for at least ten years afterward, with 1-year cumulative mortality ranging from 20 to 40%7,8,9.
Previous studies found that older age, male gender, co-morbidities (such as liver disease, chronic kidney disease, and heart pathology), and a Charlson index greater than 2 were all associated with an increased risk of mortality10,11,12,13,14. However, they were primarily concerned with the mortality rate (within 1 and 2 years after hip fracture). It is well known that glomerular filtration rate decreases with age, and chronic kidney disease (CKD) is more severe in the elderly15. Mataliotakis and associates found that patients with end-stage renal disease (ESRD) had a 4.4-fold increased risk of hip fracture when compared to the general population16. Furthermore, patients with a hip fracture and renal problem had a significantly higher mortality rate17,18,19. Moreover, Intertrochanteric fractures in patients with advanced CKD was associated with increased one-year mortality13. Acute kidney injury and advanced CKD in the intertrochanteric fracture were significantly associated with increased one-year mortality, according to Kim and colleagues13. However, there is a scarcity of data on long-term survivors of elderly hip fractures combined with CKD. As a result, the primary objective of this study was to determine 9-year survivors of hip fractures at each stage of CKD. The secondary objective was to investigate the risk factors associated with mortality following hip fracture surgery with proximal femoral nail anti-rotation.
Material and methods
Setting and subjects
A retrospective study was conducted on elderly patients with intertrochanteric fractures sustained from low energy trauma and treated surgically with proximal femoral nail anti-rotation (PFNA) between December 2011 and December 2019, using the database of department of orthopaedics at Phramongkutklao hospital. Patients with high-energy trauma, multiple fractures, pathological fractures, who were referred to other hospitals after surgery, or who had incomplete medical records, including no functional outcome assessment by Harris Hip Score (HHS), were excluded from the study. The Institutional Research Board of Royal Thai Army Hospital reviewed and approved the study as per the Helsinski Declaration and the Good Clinical Practice Guidelines (S032h/64 and 353/2022). All eligible patients signed informed consent before enrollment.
Measurements
Demographic data and comorbidities including age, gender, body weight, height, body mass index (BMI), underlying diseases (hypertension, diabetes mellitus, dyslipidemia, cardiovascular disease, gout, chronic kidney disease), Charlson comorbidity index (CCI), surgical parameters (operative time and operative blood loss), functional outcomes, and complications (hematoma, pulmonary embolism) were collected and obtained from the electronic medical record. In all patients, the estimated glomerular Infiltration rate (eGFR) was calculated using the chronic kidney disease-epidemiology collaboration (CKD-EPI) Eq. 20, and the classification of CKD was defined as the international guideline group Kidney Disease Improving Global Outcomes (KDIGO) in 201221 and 201722. In this study, patients were classified as having chronic kidney disease (CKD) if their eGFR was less than 90 ml/min/1.73 m2 and non-CKD if eGFR was greater than 90 ml/min/1.73 m2. Furthermore, mortality was assessed 1 year, 3 years, 5 years, and 9 years after surgical fixation with proximal femoral nail anti-rotation (PFNA).
Surgical technique
All patients with intertrochanteric fractures who received proximal femoral nail anti-rotation (PFNA) fixation had surgery by three highly qualified orthopedic traumatologists: T.J., O.P., and Y.P. All orthopedic surgeons used the same standard procedure for fracture reduction. We all used the fracture table to help us reduce fractures percutaneously (closed reduction). However, in some cases when achieving precise reduction by closed approach proved challenging, we all considered performing a mini-open skin incision about 7 cm from the vastus ridge to the subtrochanteric region. The Homann retractor or bone hook was used on the lesser trochanter. Fluoroscopy was used to examine the fracture gap, step, and alignment in both anteroposterior and lateral views. Kirchner wires were subsequently applied to the fracture site to maintain the perfect reduction. A long guidewire was inserted into the intramedullary canal. The position of the wire was then verified using fluoroscopy in both anteroposterior (AP) and lateral views. The PFNA was subsequently inserted along the guidewire. The blade was passed from the lateral wall to the femoral head, and the appropriate tip and apex distances23 were confirmed before tightening the blade system. Finally, the distal screw was inserted.
Operational definition and outcomes
The survival time is the time from the admission to death, the incidence of mortality (failure) is any deaths during the study period, and the living patients who loss contact or had an unknown status during the study period were defined as censor observation. All patients were seen in clinic at 2 weeks, 6 weeks, 3 months, 6 months, 9 months, 1 year, and every year until 9 years. At one year after surgical fixation, all patients’ functional outcomes were assessed using Harris Hip Score (HHS). Pain (44 points), limp (11 points), support (11 points), distance walked (11 points), sitting (5 points), entering public transportation (1 point), stairs (4 points), putting on socks and shoes (4 points), absence of deformity (4 points), and range of motion (5 points) are all components of HHS. The lowest HHS is represented by zero points, while the highest HHS is represented by one hundred points24. The mortality rate in each stage of CKD was assessed. We also compared the median survival time of hip fracture patients over 60 years in each stage of CKD over a 9-year period.
Statistical analysis
All statistical analyses were calculated using STATA version 14.0 (Stata Corp., College Station, TX, USA). Descriptive statistics are used to categorize and summarize demographic data. Continuous data were presented as means with standard deviation (SD) or medians with minimum and maximum value, as appropriate. Categorical data were presented as frequency and percentage. Comparison of categorical variables, the Chi-square test or Fisher’s exact test or Fisher’s exact test were used, as appropriate. All continuous variables were tested for the normality using a Shapiro–Wilk test and were compared using the Student’s t test or Mann–Whitney U test, as appropriate. Kaplan–Meier curve was used to estimate the overall and each stage survival probability in CKD.
Result
In this study, 443 elderly patients with intertrochanteric fractures were recruited. The mean age and BMI, as shown in Table 1, were 80.6 ± 8.5 years and 22.4 ± 3.8 kg/m2, respectively. There were 319 (72.0%) female patients and 404 (91.2%) patients with CKD (eGFR 90 ml/min/1.73 m2). In the comparison of CKD and non-CKD groups, as shown in Table 2, CKD patients were significantly older, had lower BMI, and had a higher rate of ASA class III than non-CKD patients. Gender, diabetes mellitus, hypertension, CCI, operative time, hip BMD, time to walk, length of hospital stays, surgical and medical complications, and one-year HHS did not differ between groups.
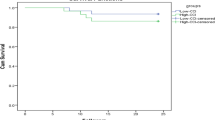
The overall mortality rate in this cohort was 42.4% (188 patients), a total follow-up time of 1717.96 person-year. The incidence of mortality was 10.94 per 100 person-year (95%CI 9.49–12.62), with a median survival time of 7.07 years (95% CI 5.89–8.59). Figure 1 shows that the survival rate after surgical fixation for intertrochanteric fracture decreased with time (89.6%, 74.1%, 59.9%, and 37.8% at 1, 3, 5, and 9 years, respectively). We found that the mortality rates differed depending on the stage of CKD (Fig. 2). Furthermore, as shown in Table 3, the incidence rate of one-year mortality was highest in CKD stage 5 (17.4% with 95% CI 11.76–25.75) and the median survival time was 3.34 years (95% CI 2.17–7.50).
A logistic regression analysis was used to determine the association between risk factors and one-year mortality, as demonstrated in Table 4. In univariate analysis, patients with CKD stage 5, operative time longer than 60 min, and the presence of a pulmonary embolism were associated with one-year mortality. Despite CKD stage 5 was not significantly increased mortality following surgical fixation of a hip fracture according to the multivariate analysis (p = 0.072), but other factors including heart disease, an operative time > 60 min, the presence of a pulmonary embolism, and poor to fair functional outcomes using HHS were significantly increased mortality (Table 4).
Discussion
ESRD was strongly associated with an increase in mortality rate17,18,19, and intertrochanteric fracture with advanced CKD was significantly associated with an increase in one-year mortality13. However, there is a lack of data on long-term survivors after hip fracture combined with CKD in elderly patients. In this study, we found that the mortality rate in elderly with intertrochanteric fracture was 10.4%, 25.9%, 40.1% and 62.2% at 1, 3, 5 and 9 years after surgical fixation. The current study’s one-year mortality rate for osteoporotic hip fracture in current study was lower than previous studies, which reported ranging from 20 to 40%7,8,9. One possible explanation is that elderly hip fractures in our facility were treated by a multidisciplinary team and received early rehabilitation.
The rate of survival after surgical fixation for an intertrochanteric fracture decreased over time, according to our findings. Non-CKD, CKD stage 2, and CKD stage 3a had median survival times of 5.75, 5.98, and 7.10 years, respectively. Furthermore, the median survival time was 3.34 years, and one-year mortality was highest in CKD stage 5 (17.4%), as previously reported17,18,19,29. Ramamurti and colleagues discovered that CKD stages 4 and 5 were significantly associated with increased mortality and all complications after surgical fixation for hip fracture compared to non-CKD25. Furthermore, LJ Hickson and associates demonstrated that CKD stage 5 patients on dialysis had a significantly higher in-hospital mortality (OR 2.65) and 30-day mortality (OR 2.03) compared to non-dialysis patients26.
We found that CKD stage 5, operative time greater than 60 min, and the presence of pulmonary embolism during admission are associated with mortality in univariate analysis, while heart diseases, operative time greater than 60 min, the presence of pulmonary embolism during admission, and a lower HHS at 1 year follow up are associated with mortality in multivariate analysis. This finding was consistent with the previous researches, which found that a number of factors, including liver diseases, chronic kidney disease, heart pathology, and the Charlson index were associated with increased mortality10,11,12,13,14. Previous studies, on the other hand, mainly identified several medical factors that were significantly associated with increased mortality after surgical fixation for hip fracture, whereas our study included surgical factor (operative time), pulmonary embolism, and functional outcome assessed by HHS.
The primary goal of risk factors is to identify patients with intertrochanteric fracture who are at high risk of death. Previous research has found that advanced stage CKD, time to surgery, rehabilitation status, post-operative complications, and previous ambulatory status all have an impact on functional status after hip fractures13,16,17,18,19,27,28,29,30. Furthermore, this study discovered that elderly patients with intertrochanteric fracture demonstrating a heart disease, a longer operative time, a pulmonary embolism, and a poor to fair functional outcome were associated with increased mortality. As a result, improving these modifiable risk factors, such as special assessment by a highly experienced cardiologist, surgery with a shorter operative time, venous thromboembolism prevention, and improved functional outcome through good surgical technique and rehabilitation program, may increase the survival rate.
This study should be interpreted in the context of a number of potential strengths and weaknesses. The strength of this study derives from its 9 years survival analysis of long-term data, which increases the ability to determine the risk factor over a longer period of time. In addition, the database collected information from a single center with an adequate sample size and also included accurate mortality information from civil registration. However, this study cannot confirm the mortality rate for each stage of CKD, with the exception of CKD stage 5 and the non-CKD group. Because our sample size was insufficient to provide sufficient data on earlier stages of CKD, the effect of CKD on other stages (stage 2, 3a, 3b, and 4) was comparable to that of the non-CKD group. This study did not identify the association between mortality and patients with CKD stage 5 on dialysis, despite the fact that a previous study26 demonstrated that this parameter significantly increased in-hospital and 30-day mortality. The study may have unintentionally recruited patients with greater survival rates or outcomes because healthier patients were more likely to participate in the study; therefore, bias may skew the results and limit generalizability. The missing data may occur because the follow-up study period was long (9 years), leading in an underestimation or overestimation of the survival rate. In this study, the CKD stage was classified based on the initial serum creatinine test and eGFR calculation performed prior to surgical operations. There could have been issues concerning classifying patients into different CKD stages, particularly when renal function differed over time. In addition, this study was limited by the lack of information regarding socioeconomic status, individual healthcare practices, and specific drugs, all of which are possible variables that could influence the relationship between chronic kidney disease (CKD) and survival.
In conclusion, during a 9-year follow-up, CKD stage 5 was associated with the highest mortality rate and shortest median survival time. In addition, heart disease, a longer operative time, pulmonary embolism, and poor to fair HHS were associated with increased risk of mortality. Recognizing these risk factors for mortality following fragility hip fracture could increase surgeons’ awareness of this vulnerable population. Patients who are at a greater risk should prioritize long-term care planning, including counseling for their healthcare providers and families.
Data availability
The datasets used during the current study available from the corresponding author on reasonable request.
Abbreviations
- CKD:
-
Chronic kidney disease
- non-CKD:
-
Non chronic kidney disease
- PFNA:
-
Proximal femoral nail anti-rotation
- ESRD:
-
End-stage renal disease
- BMI:
-
Body mass index
- CCI:
-
Charlson comorbidity index
- CKD-EPI:
-
Chronic kidney disease-epidemiology collaboration
- KDIGO:
-
Kidney disease improving global outcomes
- HHS:
-
Harris hip score
- ASA class:
-
American society of anesthesiologists classification
- SD:
-
Standard deviation
- 95% CI:
-
95% Confidential interval
- OR:
-
Odd ratio
References
Cooper, C., Campion, G. & Melton, L. J. 3rd. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 2(6), 285–289 (1992).
Gullberg, B., Johnell, O. & Kanis, J. A. World-wide projections for hip fracture. Osteoporos. Int. 7(5), 407–413 (1997).
Johnell, O. & Kanis, J. A. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos. Int. 15(11), 897–902 (2004).
Johnell, O. & Kanis, J. A. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos. Int. 17(12), 1726–1733 (2006).
Burge, R. et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J. Bone Miner. Res. 22(3), 465–475 (2007).
O’Neill, T. W. & Roy, D. K. How many people develop fractures with what outcome?. Best Pract. Res. Clin. Rheumatol. 19(6), 879–895 (2005).
Cummings, S. R. & Melton, L. J. Epidemiology and outcomes of osteoporotic fractures. Lancet. 359(9319), 1761–1767 (2002).
Kanis, J. A. et al. The components of excess mortality after hip fracture. Bone. 32(5), 468–473 (2003).
Katsoulis, M. et al. Excess mortality after hip fracture in elderly persons from Europe and the USA: The CHANCES project. J. Intern. Med. 281(3), 300–310 (2017).
Haentjens, P. et al. Meta-analysis: Excess mortality after hip fracture among older women and men. Ann. Intern. Med. 152(6), 380–390 (2010).
Guzon-Illescas, O. et al. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J. Orthop. Surg. Res. 14(1), 203 (2019).
Yaacobi, E. et al. Mortality following surgery for geriatric hip fractures: Is it the timing or the co-morbidities?. Hip Int. 32(2), 271–275 (2022).
Kim, T. W. et al. Chronic kidney disease patients with intertrochanteric fracture have a high mortality rate. Injury 52(8), 2350–2355 (2021).
Xu, B. Y. et al. Predictors of poor functional outcomes and mortality in patients with hip fracture: A systematic review. BMC Musculoskelet. Disord. 20(1), 568 (2019).
Avin, K. G. & Moorthi, R. N. Bone is not alone: The effects of skeletal muscle dysfunction in chronic kidney disease. Curr. Osteoporos. Rep. 13(3), 173–179 (2015).
Mataliotakis, G. et al. Femoral neck fractures secondary to renal osteodystrophy. Literature review and treatment algorithm. J. Musculoskelet. Neuronal Interact. 9(3), 130–7 (2009).
Lan, J. et al. The impact of chronic kidney disease and dialysis therapy on outcomes of elderly patients with hip fractures: A systematic review and meta-analysis. Scott. Med. J. 67(4), 144–156 (2022).
Lo, L. W. T. et al. End stage renal disease patients undergoing hip fracture surgery have increased length of stay, acute hospital bill size, and reduced survivorship-implications on a bundled care program. Arch. Osteoporos. 17(1), 59 (2022).
Belmont, P. J. Jr. et al. Risk factors for complications and in-hospital mortality following hip fractures: A study using the National Trauma Data Bank. Arch. Orthop. Trauma Surg. 134(5), 597–604 (2014).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate [published correction appears in Ann Intern Med. 2011 Sep 20;155(6):408]. Ann. Intern. Med. 150(9), 604–12 (2009).
Andrassy, K. M. Comments on “KDIGO 2012 Clinical practice guideline for the evaluation and management of chronic kidney disease”. Kidney Int. 84(3), 622–623 (2013).
Erratum: Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO. Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int. Suppl. 2017(7), 1–59 (2017).
Baumgaertner, M. R., Curtin, S. L., Lindskog, D. M. & Keggi, J. M. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J. Bone Joint Surg. Am. 77(7), 1058–1064 (1995).
Harris, W. H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Joint Surg. Am. 51(4), 737–55 (1969).
Ramamurti, P. et al. Impaired renal function is an independent risk factor for complications after surgery for femoral neck fracture. Hip Int. 33(2), 345–353 (2023).
Hickson, L. J. et al. Death and postoperative complications after hip fracture repair: dialysis effect. Kidney Int. Rep. 3(6), 1294–1303 (2018).
Roshanravan, B. et al. Association between physical performance and all-cause mortality in CKD. J. Am. Soc. Nephrol. 24(5), 822–830 (2013).
Abellan van Kan, G. et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J. Nutr. Health Aging 13(10), 881–9 (2009).
Phruetthiphat, O. A. et al. The effect of CKD on intertrochanteric fracture treated with proximal femoral nail anti-rotation: A 7-year study. J. Orthop. 32, 151–155 (2022).
Phruetthiphat, O. A. et al. An innovative scoring system for predicting an excellent Harris hip score after proximal femoral nail anti-rotation in elderly patients with intertrochanteric fracture. Sci. Rep. 12(1), 19939 (2022).
Acknowledgements
The authors thank the patients for their participation. We also thank Pawinee Saybungkla for statistical analyses.
Author information
Authors and Affiliations
Contributions
All authors designed the protocol, read, and approved the final manuscript. O.P. Generating the idea, collecting data, analyzing the data, and writing the manuscript. A.L., Y.S., and P.P. collecting data, sorted out the material and assisting in the discussion part. T.S. supervised the study and assisting in the discussion part. C.P. supervised the study, checked and revising the manuscript. All authors have read and approved the final submitted manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the Institutional Review Board Royal Thai Army Medical Department (IRBRTA). All procedures were performed in accordance with relevant guidelines. This study was registered to IRBRTA and it has been approved with a code of S032h/64 and 353/2022. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Phruetthiphat, Oa., Lawanprasert, A., Satravaha, Y. et al. Nine-year survival after intertrochanteric fracture in elderly with chronic kidney disease. Sci Rep 14, 20912 (2024). https://doi.org/10.1038/s41598-024-72140-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-72140-5
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.