Abstract
Post-transplantation diabetes mellitus (PTDM) negatively affects graft and patient survival after kidney transplantation (KT). This prospective study used continuous glucose monitoring (CGM) to evaluate perioperative blood glucose dynamics, identify PTDM risk factors, and compare predictive accuracy with capillary blood glucose monitoring (CBGM) in 60 non-diabetic living-donor KT recipients. Patients underwent 2-week pre- and postoperative CGM, including routine CBGM during their in-hospital stays. PTDM-related risk factors and glucose profiles were analyzed with postoperative CGM and CBG. PTDM developed in 14 (23.3%) patients and was associated with older age, male sex, higher baseline HbA1c, high-density lipoprotein cholesterol, and 3-month cumulative tacrolimus exposure levels. Male sex and postoperative time above the range (TAR) of 180 mg/dL by CGM were PTDM-related risk factors in the multivariate analysis. For predictive power, the CGM model with postoperative glucose profiles exhibited higher accuracy compared with the CBGM model (areas under the curves of 0.916, and 0.865, respectively). Therefore, we found that male patients with a higher postoperative TAR of 180 mg/dL have an increased risk of PTDM. Postoperative CGM provides detailed glucose dynamics and demonstrates superior predictive potential for PTDM than CBGM.
Similar content being viewed by others
Introduction
Post-transplantation diabetes mellitus (PTDM) refers to the development of diabetes mellitus (DM) in individuals without DM before organ transplantation. The reported occurrence rate of PTDM ranges from 2 to 52%, and the highest prevalence occurs in cases of kidney transplantation (KT)1,2. PTDM amplifies the risk of cardiovascular disease and infections, diminishes quality of life, and ultimately leads to lower overall patient and graft survival. Risk factors for PTDM overlap with conventional risk factors for type 2 DM, encompassing age, ethnicity, obesity, family history, genetic predisposition, and metabolic syndromes. Additionally, transplant-related factors, such as hepatitis C, immunosuppressive medications, and cytomegalovirus infection contribute to the onset of PTDM3,4. Physicians strive to manage these risk factors through various strategies, including adjustments to immunosuppressive medication and the implementation of rigorous glucose monitoring and regulation5.
However, reducing the use of calcineurin inhibitors and glucocorticoids, which serve as essential immunosuppressive agents for preventing rejection but are also diabetogenic, remains challenging6,7. Therefore, the best effective modifiable strategy is an early prediction of PTDM, which facilitates the reduction of complications through stringent blood glucose management and ensures long-term patient and graft survival after KT. The commonly used method, skin-prick capillary blood glucose monitoring (CBGM) is invasive and makes frequent monitoring difficult. Consequently, it is not sensitive enough to adequately monitor for dysglycemia. However, continuous glucose monitoring (CGM) in the form of a wearable device is non-invasive and provides complete 24-h data along with detailed glucose profiles, offering insights into changes in patients’ glucose levels8. Recent study have reported that incorporating CGM into standard diagnostic methods allows for earlier identification of individuals with diabetes or pre-diabetes from healthy individuals9. This study aimed to identify changes in glucose levels pre- and post-KT using CGM and investigate the risk factors associated with the incidence of PTDM. Furthermore, we compared the predictive efficacy of CBGM and postoperative CGM in relation to PTDM occurrence.
Methods
Study population
This was a single-center, prospective, observational study (ClinicalTrials.gov NCT) conducted from June 2021 to September 2022. All patients scheduled for living-donor KT were identified as potentially eligible participants. The exclusion criteria included: patients younger than 18 years, prior renal transplant recipients, those undergoing deceased-donor or multi-organ transplantation, and those diagnosed with DM prior to transplantation. All potential candidates provided informed consent prior to enrollment. Enrolled patients who completed glucose monitoring and assessment up to 6 months post-transplantation were included in the final analysis. This study was supported by a SNUH research grant (#0420210760).
Study design
Once consent was obtained, preoperative glucose data were collected 14 days before the scheduled surgery using a CGM sensor (Freestyle Libre 1; Abbott Diabetes Care Ltd., Maidenhead, UK). The device was placed on the patient’s upper arm according to the manufacturer’s instructions. The patients installed the corresponding application on their smartphones and were instructed to scan the sensors using their smartphones at least once every 8 h. The sensor collected glucose data every min and automatically stored a reading every 15 min. In addition to the daily glucose levels, the CGM system provided calculated parameters based on these daily levels, including glucose management index (GMI) (%), coefficient of variation (%), time within the range of 70–180 mg/dL (%), time above the range (TAR) of 180 mg/dL (%), time below the range of 70 mg/dL (%), and nadir and peak glucose levels.
To collect postoperative glucose data, a new sensor was applied and used for an additional 14 days following surgery. Throughout the hospitalization period for transplantation, patients adhered to the established protocol for CBGM, which was performed daily before each meal and bedtime. Interventions for abnormal glucose levels were based on the CBGM rather than CGM readings.
Preoperative waist-to-hip circumference ratio and fat-to-muscle ratio measurements using bioimpedance analysis (InBody970; InBody Co., Ltd., Seoul, Korea) were also collected in the enrolled patients. Further laboratory examinations were conducted for fasting plasma glucose (FPG), insulin, hemoglobin A1c (HbA1c), C-peptide, and lipid profiles (including total cholesterol, high-density lipoprotein [HDL], low-density lipoprotein [LDL], and triglycerides) at baseline and 1, 2, 3, and 6 months postoperatively. The homeostasis model assessment of insulin resistance (HOMA-IR) and beta-cell function (HOMA-B) were used to estimate insulin resistance and secretion by analyzing insulin levels10.
Definition of PTDM
PTDM was defined based on the American Diabetes Association (ADA) diagnostic criteria at 6 months post-transplantation in patients without a preoperative diagnosis of DM11. Fasting plasma glucose and HbA1c were both assessed, whereas the measurement of 2-h plasma glucose during a 75-g oral glucose tolerance test (OGTT) was not conducted. Consequently, the diagnosis of PTDM was established employing the former two criteria; 1. Fasting plasma glucose level ≥ 126 mg/dL (fasting is defined as no caloric intake for at least 8 h) or 2. An HbA1c level ≥ 6.5% following the duration of 6 months post-transplantation among patients who were not diagnosed with preoperative DM. Study patients who developed PTDM were categorized as the PTDM group. Those who did not develop PTDM during the study period were defined as the non-PTDM group.
Immunosuppressive regimen and postoperative glucose control protocol
The immunosuppressive regimen consisted of induction therapy and triple maintenance agents. Induction therapy included basiliximab or rabbit anti-human thymocyte immunoglobulin. The maintenance regimen consisted of tacrolimus, antimetabolites (mycophenolate mofetil and mycophenolic acid), and corticosteroids. Tacrolimus was administered twice a day. During the first 3 months post-transplantation, trough concentration levels were maintained within the range of 8–12 ng/mL, followed by a target range of 6–10 ng/mL from 3 to 6 months. Cumulative exposure to tacrolimus (CET) for 3 months was calculated as the area under the concentration–time curve (AUC) based on trough concentrations. All measured tacrolimus concentration values for a specific patient were plotted on a time-dependent graph, and the AUC of the tacrolimus level was calculated using the Wagner–Nelson equation12. Steroid therapy commenced with an intravenous injection of 500 mg on the day of surgery and was subsequently gradually tapered to 5 mg of oral prednisolone over 4 weeks. Steroids were administered after breakfast to alleviate gastrointestinal discomfort, and this was continued for 6 months. Mycophenolate mofetil (500 mg) or an equivalent dose of mycophenolic acid was administered twice daily. In cases where adverse effects such as leukopenia or elevated liver enzyme levels were observed, the medication was either discontinued or adjusted based on the clinical severity and progression of side effects.
For postoperative glycemic control, the regular insulin (RI) sliding scale protocol was initiated if the CBGM exceeded 250 mg/dL immediately after surgery. Humulin R (100 IU) was mixed with 100 mL of normal saline and started at 1 cc/h, with the dose adjusted according to the established protocol. Once the RI was tapered, intermittent subcutaneous injections of Humulin R were administered according to a consistent protocol (Supplementary Table 1).
Statistical analyses
Categorical variables are expressed as percentages within the respective derived groups and were assessed using Pearson’s chi-square and Fisher’s exact tests. Continuous variables are presented as means ± standard deviations and were evaluated using a Student’s t-test following a normality test. To compare the pre- and postoperative glucose variations between the PTDM and non-PTDM groups, the differences in glucose variation before and after surgery were calculated for each patient. The variation was calculated as standard deviations, and a Wilcoxon test was performed between groups for the differences.
Univariate and multivariate logistic regression analyses were conducted to identify factors that were independently and significantly associated with the onset of PTDM. Before conducting multivariate logistic regression, a multicollinearity test was performed using the variance inflation factor (VIF) among independent variables. If the VIF value exceeded 10, it was used as the criterion for variable removal from the model, and variables were removed in consideration of clinical relevance to the study. Variables with a P-value of less than 0.05 in the univariate analyses were subsequently included in the multivariate logistic regression using a backward elimination method.
We established two models, the CBGM and CGM model, with postoperative blood glucose data (postoperative CGM). Additionally, receiver operating characteristic (ROC) curves were generated to compare the AUC of different glucose monitoring models (postoperative CBGM vs. postoperative CGM) for PTDM prediction. DeLong’s test was conducted to compare the AUCs of both models. All analyses were performed using IBM SPSS version 26.0 (IBM Corp., Armonk, NY, USA) and R version 4.3.1 (R Foundation for Statistical Computing, Vienna, Austria). A P-value of less than 0.05 was considered significant.
Results
Patient characteristics
During the enrollment period, 264 patients underwent KT at our center, of which, 100 consented to participate in the study. In the cohort of 100 patients, 15 were diagnosed with preoperative DM, four had undergone deceased-donor transplantation without preoperative CGM data, 18 had insufficient glucose monitoring data, and three had insufficient diabetes-related data and were thus excluded from the study. Finally, 60 patients were included in the final analysis. Among them, 14 (23.3%) developed PTDM during the study period. Patient and donor demographics and transplant characteristics are summarized in Table 1. The PTDM group was significantly older (56.4 ± 9.8 years) than the non-PTDM group (46.2 ± 13.0 years, P = 0.009). In addition, male patients were more prevalent in the PTDM group (85.7%) than in the non-PTDM group (45.7%, P = 0.008). No differences were observed among donors with respect to human leukocyte antigen incompatibility, age, sex, body mass index (BMI), or their relationship with the recipient between the two groups. All study patients exhibited a normal preoperative glucose profile, with a mean C-peptide level of 5.9 ± 3.5 ng/mL. Indices of insulin secretion and resistance, represented by HOMA-B (226.8 ± 251.8) and HOMA-IR (2.3 ± 1.1), respectively, were within the normal range. Although enrolled patients showed a normal range of HbA1c levels (5.2 ± 0.5%), patients in the PTDM group exhibited significantly higher preoperative HbA1c levels (5.5 ± 0.4% vs. 5.2 ± 0.5%, respectively; P = 0.023). Those in the PTDM group also had lower HDL levels than those in the non-PTDM group (37.7 ± 11.8 mg/dL vs. 51.3 ± 16.3 mg/dL, respectively; P = 0.006).
Transplant outcomes
All transplantations were performed successfully without immediate postoperative complications or rejections. Regarding immunosuppressive agents, there were no significant differences in terms of induction agents, steroid pulse treatment during follow-up, or mean steroid dose during hospitalization. However, the PTDM group exhibited significantly higher tacrolimus trough concentrations on the day of discharge than the non-PTDM group (11.4 ± 2.2 ng/mL vs. 9.8 ± 1.9 ng/mL, respectively; P = 0.014), along with higher mean tacrolimus concentrations during the index admission (11.3 ± 2.2 ng/mL vs. 9.6 ± 1.7 ng/mL, respectively; P = 0.003). Furthermore, the 3-month CET was significantly greater in the PTDM group than in the non-PTDM group (898.3 ± 54.4 ng/mL vs. 804.7 ± 90.0 ng/mL, respectively; P = 0.001) (Table 1).
No significant difference was seen in the occurrence of transplant rejection demonstrated by indication biopsy and postoperative 10-days protocol biopsy between the non-PTDM (37.0%) and PTDM (21.4%) groups (P = 0.281). No graft failure occurred during follow-up in either group. The estimated glomerular filtration rate levels at discharge and 1, 2, 3, and 6 months postoperatively showed no significant differences between the two groups (Table 2).
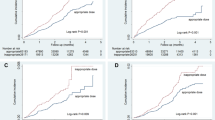
Changes in perioperative glucose profile
Figure 1 illustrates the preoperative and postoperative changes in glucose variation relative to PTDM development. More increase in daily glucose levels and variation were observed in the postoperative period compared with values in the preoperative period in the PTDM group. The mean standard deviation was 15.8 in the PTDM group and 10.6 in the non-PTDM group. A Wilcoxon rank test revealed a statistically significant difference (P = 0.02). Figure 2 presents a visualized graph of changes in glucose levels before and after KT for the entire cohort, and Fig. 3 further shows significant increases in average, peak, and nadir glucose levels that occurred postoperatively in both groups.
Daily glucose variation in the preoperative and postoperative non-PTDM and PTDM groups was assessed using CGM. (A) Preoperative daily glucose variation in the non-PTDM group. (B) Postoperative daily glucose variation in the non-PTDM group. (C) Preoperative daily glucose variation in the PTDM group. (D) Postoperative daily glucose variation in the PTDM group. CGM continuous glucose monitoring, PTDM post-transplantation diabetes mellitus.
Comparison of preoperative and postoperative glucose levels in the PTDM and non-PTDM groups as assessed using continuous glucose monitoring. (A) Preoperative and postoperative mean daily peak glucose levels in the non-PTDM and PTDM groups. (B) Preoperative and postoperative mean daily glucose levels in the non-PTDM and PTDM groups. (C) Preoperative and postoperative mean daily nadir glucose levels in the non-PTDM and PTDM groups. Pre-op preoperative, post-op postoperative, PTDM post-transplantation diabetes mellitus.
In the preoperative period, CGM showed that the PTDM group had significantly higher preoperative mean glucose levels (107.4 ± 13.2 mg/dL vs. 95.5 ± 13.4 mg/dL, respectively; P = 0.006), GMI (5.8 ± 0.3% vs. 5.6 ± 0.3%, respectively; P = 0.016), and mean peak glucose levels (175.5 ± 19.6 mg/dL vs. 150.0 ± 31.5 mg/dL, respectively; P = 0.006) than the non-PTDM group. In the postoperative period, the CGM values of the mean glucose levels (141.6 ± 21.4 mg/dL vs. 120.2 ± 18.0 mg/dL, respectively; P < 0.001), TAR of 180 mg/dL during the day (21.1 ± 12.3% vs. 9.0 ± 8.8%, respectively; P < 0.001), and mean daily peak glucose levels (221.5 ± 22.3 vs. 189.1 ± 31.2 mg/dL, respectively; P = 0.002) were significantly higher in the PTDM group than those in the non-PTDM group (Table 3).
Similarly, CBGM also showed that the PTDM group exhibited higher average glucose levels postoperatively (164.6 ± 25.3 mg/dL vs. 151.9 ± 18.9 mg/dL, respectively; P = 0.027) and daily peak glucose values (208.7 ± 31.7 mg/dL vs. 189.6 ± 26.2 mg/dL, respectively; P = 0.048) than the non-PTDM group.
Postoperative changes in metabolic indices during the follow-up period
There were no significant differences in body weight and BMI changes between the two groups at 1, 2, 3, and 6 months postoperatively. However, the PTDM group consistently demonstrated significantly higher of HbA1c levels than the non-PTDM group at all follow-up periods. There were no significant differences in total cholesterol and LDL levels between the two groups during the 6-month follow-up period. However, the PTDM group showed significantly lower HDL levels at 2 and 3 months postoperatively. The HOMA-IR values at 1, 2, and 3 months after KT did not show any significant differences between the two groups. However, the PTDM group showed an increasing trend of HOMA-IR after transplantation and exhibited a significantly higher value of HOMA-IR (7.0 ± 9.5) at 6 months, whereas patients in the non-PTDM group had a lower value (3.1 ± 1.5, P = 0.001). Regarding the triglycerides to HDL ratio, a surrogate marker for insulin resistance, the PTDM group consistently showed higher values than non-PTDM group from baseline to 6 months post-operation, although this difference did not reach statistical significance. There were no significant differences between the two groups in terms of HOMA-B during the follow-up period (Fig. 4).
Postoperative changes in the metabolic indices HbA1c, HDL, HOMA-IR, HOMA-B, Triglyceride/HDL ratio, and body weight during the follow-up period. *P < 0.05, **P < 0.01. CGM continuous glucose monitoring, HOMA-B homeostasis model assessment of beta-cell function, HOMA-IR homeostasis model assessment of insulin resistance, HbA1c hemoglobin A1c, HDL high-density lipoprotein, PTDM post-transplantation diabetes mellitus.
Risk factors and prediction models for PTDM
In the univariate analysis, baseline characteristics such as age, male sex, and preoperative HbA1c and HDL levels were associated with the development of PTDM. The 3-month CET was identified as an immunosuppression-related factor for PTDM development. Among postoperative glucose profiles, mean daily peak glucose by CBGM, mean glucose level, TAR of 180 mg/dL, and mean daily peak glucose levels by CGM were statistically significant. A multicollinearity assessment was conducted on factors exhibiting statistical significance in the univariate analysis (Table 4). Confirming no evidence of multicollinearity, we performed the multivariate logistic regression analysis using baseline characteristics and postoperative indices. Male sex (odds ratio [OR] 17.45; 95% confidence interval [CI] 1.79–70.01; P = 0.014) and a CGM-detected postoperative TAR of 180 mg/dL (OR 1.17; 95% CI 1.06–1.29; P = 0.002) were found to be independent risk factors associated with the occurrence of PTDM (Table 5).
To compare the predictive abilities of the CBGM and CGM models for PTDM, we plotted the ROC curves for the CBGM model and the postoperative CGM model. Each model was constructed by combining variables with a P-value of less than 0.05, identified through univariate regression analysis. The AUCs of CBGM and postoperative CGM were 0.865 and 0.916, respectively (Fig. 5). In DeLong’s test, the difference in AUCs between the CBGM model and the postoperative CGM model resulted in a P-value of 0.12.
Discussion
Previous studies have demonstrated the accuracy, reliability, and feasibility of CGM in patients with type 1 DM, simultaneous pancreas-KT, and critical care settings13,14,15,16. Furthermore, some transplant centers have adopted CGM as part of their standard protocol. However, only a limited number of studies have analyzed postoperative glucose dynamics through CGM in KT recipients, specifically examining its association with the onset of PTDM. Additionally, monitoring in previous studies was limited to the short stress period within 5 days immediately postoperatively, making it difficult to secure accurate predictive power17,18.
We conducted a comprehensive analysis to investigate factors influencing the incidence of PTDM using CGM. Blood glucose levels were monitored using CGM for 14 days, before and after surgery, in addition to CBGM during hospitalization. KT recipients showed elevated mean glucose levels, GMI, TAR of 180 mg/dL, and mean daily peak glucose levels post-KT compared with pre-KT values. Among the patients included in the study, 23.3% developed PTDM. Our findings identified major risk factors associated with PTDM, including male sex and elevated postoperative TAR of 180 mg/dL, detected using CGM.
Preoperative impaired glucose tolerance (IGT) and impaired fasting glucose (IFG) represent significant risk factors for developing PTDM19. Previous studies have indicated a 15% prevalence of pre-transplantation IGT or IFG, with a subsequent 35% progression to PTDM20,21. Although all values remained within the normal range, preoperative CGM indicated that patients in the PTDM group had significantly higher mean glucose levels, GMI, and mean daily peak glucose levels prior to transplantation than those in the non-PTDM group. Similar to DM, IGT or IFG is characterized by significant glucose variability, which can be assessed through CGM.19 Without overt DM before transplantation, the preemptive use of antihyperglycemic agents or insulin may not be warranted. However, lifestyle modifications and dietary adjustments alone have been reported to prevent the progression to DM in patients with impaired glucose metabolism22,23. Furthermore, unlike invasive CBGM, CGM can be implemented in an outpatient setting before surgery and provide comprehensive 24-h data, offering more sensitive glucose readings. It also allows patients to independently access their glucose data and initiate management strategies prior to surgery. Therefore, CGM not only improves the accuracy of predicting PTDM, but also has the potential to reduce its incidence through early detection and correction.
Regarding postoperative glycemic control, the multivariate logistic regression analysis identified a postoperative TAR of 180 mg/dL using CGM as a significant risk factor for PTDM. However, values obtained through CBGM were not statistically significant. The CBGM follows a standard protocol that involves measuring glucose levels upon waking up, before lunch and dinner, and before bedtime. Patients with KT experience various physiological changes along with stress hormone secretion due to surgery immediately after transplantation, administration of high-dose immunosuppressants, and the dawn phenomenon. Administration of prednisolone after breakfast contributes to prolonged elevation of glucose levels or an extended period of prolonged elevation before levels return to baseline. However, intermittent monitoring with CBGM leads to imprecision in average values and precludes the capture of glucose dynamics24,25, including peak values or TAR of 180 mg/dL. Consequently, CGM showed higher predictive power for PTDM occurrence compared with CBGM.
Among other factors related to blood glucose, male sex was identified as a significant predictive factor for the occurrence of PTDM, consistent with previous findings26,27,28. The development of type 2 DM, attributed to visceral adipose tissue, was due to the higher androgen receptors and lower estrogen receptors (ER) in this tissue. Estrogen and ER signaling, which are protective against DM, also apply to the PTDM29. Although not considered significant risk factors, differences between the two groups in CET for 3 months exhibited a trend aligning with PTDM occurrence and are recognized as conventional risk factors. High cumulative dose tacrolimus has been observed to decrease insulin mRNA transcription and insulin production in rat models30. According to Elias et al., in patients undergoing Tacrolimus-based treatment, the evaluation of insulin secretion using the HOMA-b progressively declined with the occurrence of PTDM, whereas insulin resistance, assessed through HOMA-IR showed no significant changes. This suggests Tacrolimus may impact PTDM development by inhibiting insulin secretion31. Conversely, Qing-Jie et al. suggest that the primary mechanism associated with Tacrolimus-induced PTDM is the induction of insulin resistance. Although the mechanisms may vary, patients who exhibited high CET may have a higher likelihood of PTDM occurrence32.
This study had limitations. First, it was based on a single-center sample with a relatively small number of patients. Therefore, our results may not be readily generalizable, and further validation is warranted through extensive multicenter investigations. Second, an oral glucose tolerance test (OGTT) was not conducted in our center. However, ADA guidelines emphasize the equivalency of FPG, 2-h plasma glucose OGTT, and HbA1c for diagnostic screening. Furthermore, it is underscored that utilizing FPG and HbA1c tests in screening can effectively reduce the overall requirement for OGTTs4. Third, the carbohydrate intake and physical activity of the cohort were not controlled. Therefore, we cannot exclude the possibility that our findings could be explained by variations in the patients’ diet or physical activity levels. Finally, in the ROC curve analysis comparing the predictive abilities of the CBGM model and the postoperative CGM model for PTDM occurrence, the postoperative CGM model showed a higher AUC, indicating better predictive power; however, this difference was not statistically significant. CBGM is a recognized protocol for managing patients with diabetes; thus, it should not be regarded as significantly inferior to CGM, even when compared to clinical studies.
Conclusion
We found that male patients with a higher postoperative TAR of 180 mg/dL have an increased risk of PTDM. Moreover, CGM provides a reliable method for glucose monitoring and offers superior predictive performance for detecting the occurrence of PTDM compared with CBGM. The utilization of CGM facilitates the identification of individuals at risk of developing PTDM and could support the implementation of more rigorous glycemic control in at-risk patients. Further investigation is warranted to substantiate these results, including cost-effectiveness considerations.
Data availability
The source data for all figures included in the manuscript are stored in Mendeley Data (https://doi.org/10.17632/r5n5zt4xs9.1). If permissible, the dataset generated and/or analyzed during the current research will be made available upon request from the corresponding author. Limited access to certain clinical data generated in the current study is restricted due to the absence of prior authorization for external sharing of data from research subjects without explicit consent.
References
Song, J. L. et al. Higher tacrolimus blood concentration is related to increased risk of post-transplantation diabetes mellitus after living donor liver transplantation. Int. J. Surg. 51, 17–23 (2018).
Wang, L. et al. Postoperative fasting plasma glucose and family history diabetes mellitus can predict post-transplantation diabetes mellitus in kidney transplant recipients. Endocrine 81, 58–66 (2023).
Zielińska, K. et al. Prevalence and risk factors of new-onset diabetes after transplantation (NODAT). Ann. Transplant. 25, e926556 (2020).
Smyrli, M., Smyrlis, A., Tsouka, G., Apostolou, T. & Vougas, V. Risk factors of the development of diabetes mellitus after kidney transplantation. Transplant. Proc. 53, 2782–2785 (2021).
Hecking, M., Sharif, A., Eller, K. & Jenssen, T. Management of post-transplant diabetes: Immunosuppression, early prevention, and novel antidiabetics. Transplant. Int. 34, 27–48 (2021).
Dziedziejko, V. et al. Leptin receptor gene polymorphisms in kidney transplant patients with post-transplant diabetes mellitus treated with tacrolimus. Int. Immunopharmacol. 124, 110989 (2023).
Liu, Y. et al. Impact of varied immunosuppressive agents and posttransplant diabetes mellitus on prognosis among diverse transplant recipients (experimental studies). Int. J. Surg. 110, 2007–2024 (2024).
Martens, T. et al. Effect of continuous glucose monitoring on glycemic control in patients with type 2 diabetes treated with basal insulin: A randomized clinical trial. Jama 325, 2262–2272 (2021).
Gottfried, S., Pontiggia, L., Newberg, A., Laynor, G. & Monti, D. Continuous glucose monitoring metrics for earlier identification of pre-diabetes: Protocol for a systematic review and meta-analysis. BMJ Open 12, e061756 (2022).
Matthews, D. R. et al. Homeostasis model assessment: Insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985).
American Diabetes Association Professional Practice Committee. 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes—2022. Diabetes Care 45, S17–S38 (2022).
Rodríguez-Perálvarez, M. et al. Cumulative exposure to tacrolimus and incidence of cancer after liver transplantation. Am. J. Transplant. 22, 1671–1682 (2022).
Al Hayek, A. A., Robert, A. A. & Al Dawish, M. A. Evaluation of FreeStyle libre flash glucose monitoring system on glycemic control, health-related quality of life, and fear of hypoglycemia in patients with type 1 diabetes. Clin. Med. Insights Endocrinol. Diabetes 10, 1179551417746957 (2017).
Dmitriev, I. V. et al. Continuous glucose monitoring in patients following simultaneous pancreas-kidney transplantation: Time in range and glucose variability. Diagnostics 13, 1606 (2023).
Dadlani, V. et al. Continuous glucose monitoring to assess glycemic control in the first 6 weeks after pancreas transplantation. Clin. Transplant. 33, e13719 (2019).
Perez-Guzman, M. C., Shang, T., Zhang, J. Y., Jornsay, D. & Klonoff, D. C. Continuous glucose monitoring in the hospital. Endocrinol. Metab. 36, 240–255 (2021).
Jandovitz, N. et al. A randomized trial of continuous glucose monitoring to improve post-transplant glycemic control. Clin. Transplant. 37, e15139 (2023).
Wojtusciszyn, A., Mourad, G., Bringer, J. & Renard, E. Continuous glucose monitoring after kidney transplantation in non-diabetic patients: Early hyperglycaemia is frequent and may herald post-transplantation diabetes mellitus and graft failure. Diabetes Metab. 39, 404–410 (2013).
Mittal, S. et al. Early postoperative continuous glucose monitoring in pancreas transplant recipients. Transplant. Int. 28, 604–609 (2015).
Caillard, S. et al. Incidence and risk factors of glucose metabolism disorders in kidney transplant recipients: Role of systematic screening by oral glucose tolerance test. Transplantation 91, 757–764 (2011).
Guthoff, M. et al. Diabetes mellitus and prediabetes on kidney transplant waiting list-prevalence, metabolic phenotyping and risk stratification approach. PLoS ONE 10, e0134971 (2015).
Tuomilehto, J. et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N. Engl. J. Med. 344, 1343–1350 (2001).
Li, G. et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: A 20-year follow-up study. Lancet 371, 1783–1789 (2008).
Rodríguez, L. M., Knight, R. J. & Heptulla, R. A. Continuous glucose monitoring in subjects after simultaneous pancreas-kidney and kidney-alone transplantation. Diabetes Technol. Ther. 12, 347–351 (2010).
Clemens, K. K. et al. Reducing hyperglycaemia post-kidney and liver transplant: A quality improvement initiative. BMJ Open Qual. 11, e001796 (2022).
Ye, Y. et al. Association between preoperative lipid profiles and new-onset diabetes after transplantation in Chinese kidney transplant recipients: A retrospective cohort study. J. Clin. Lab. Anal. 35(8), e23867 (2021).
Cheng, C. Y., Feng, Y. T. & Wang, H. Y. Incidence and relative risk factors in posttransplant diabetes mellitus patients: A retrospective cohort study. Korean J. Transplant. 34(4), 213–237 (2020).
Rosettenstein, K. et al. Diagnostic accuracies of glycated hemoglobin, fructosamine, and homeostasis model assessment of insulin resistance in predicting impaired fasting glucose, impaired glucose tolerance, or new onset diabetes after transplantation. Transplantation 100(7), 1571–1579 (2016).
Shepard, B. D. Sex differences in diabetes and kidney disease: Mechanisms and consequences. Am. J. Physiol. Renal Physiol. 317(2), F456–F462 (2019).
van Hooff, J. P., Christiaans, M. H. & van Duijnhoven, E. M. Tacrolimus and posttransplant diabetes mellitus in renal transplantation. Transplantation 79(11), 1465–1469 (2005).
David-Neto, E. et al. The dynamics of glucose metabolism under calcineurin inhibitors in the first year after renal transplantation in nonobese patients. Transplantation 84(1), 50–55 (2007).
Chen, Q. J. et al. Tacrolimus decreases insulin sensitivity without reducing fasting insulin concentration: A 2-year follow-up study in kidney transplant recipients. Ren Fail. 37(4), 601–606 (2015).
Author information
Authors and Affiliations
Contributions
JY: Data curation, Formal analysis, Investigation, Writing—original draft, Writing—review & editing. EA: Conceptualization, Data curation, Methodology, Project administration. HY, AR, and MH: Investigation, Methodology, Project administration. SW: Software, Validation, Visualization, Formal analysis. AhR and JW: Investigation, Resources, Supervision. SI: Conceptualization, Funding acquisition, Investigation, Project administration, Supervision, Writing—review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted in accordance with the principles of the Declaration of Helsinki. All study procedures were approved by the independent Institutional Review Board (IRB) of Seoul National University Hospital (IRB number: 2102-083-1197). All participants provided written informed consent.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shin, J., Jo, EA., Woo, H.Y. et al. Perioperative glucose monitoring with continuous glucose monitors identifies risk factors for post-transplant diabetes mellitus in kidney transplant recipients. Sci Rep 14, 21240 (2024). https://doi.org/10.1038/s41598-024-72025-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-72025-7
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.