Abstract
Despite evidence suggesting the benefit of prophylactic regional antibiotic delivery (RAD) to sternal edges during cardiac surgery, it is seldom performed in clinical practice. The value of topical vancomycin and gentamicin for sternal wound infections (SWI) prophylaxis was further questioned by recent studies including randomized controlled trials (RCTs). The aim of this systematic review and meta-analysis was to comprehensively assess the safety and effectiveness of RAD to reduce the risk of SWI.We screened multiple databases for RCTs assessing the effectiveness of RAD (vancomycin, gentamicin) in SWI prophylaxis. Random effects meta-analysis was performed. The primary endpoint was any SWI; other wound complications were also analysed. Odds Ratios served as the primary statistical analyses. Trial sequential analysis (TSA) was performed.Thirteen RCTs (N = 7,719 patients) were included. The odds of any SWI were significantly reduced by over 50% with any RAD: OR (95%CIs): 0.49 (0.35–0.68); p < 0.001 and consistently reduced in vancomycin (0.34 [0.18–0.64]; p < 0.001) and gentamicin (0.58 [0.39–0.86]; p = 0.007) groups (psubgroup = 0.15). Similarly, RAD reduced the odds of SWI in diabetic and non-diabetic patients (0.46 [0.32–0.65]; p < 0.001 and 0.60 [0.44–0.83]; p = 0.002 respectively). Cumulative Z-curve passed the TSA-adjusted boundary for SWIs suggesting adequate power has been met and no further trials are needed. RAD significantly reduced deep (0.60 [0.43–0.83]; p = 0.003) and superficial SWIs (0.54 [0.32–0.91]; p = 0.02). No differences were seen in mediastinitis and mortality, however, limited number of studies assessed these endpoints. There was no evidence of systemic toxicity, sternal dehiscence and resistant strains emergence. Both vancomycin and gentamicin reduced the odds of cultures outside their respective serum concentrations’ activity: vancomycin against gram-negative strains: 0.20 (0.01–4.18) and gentamicin against gram-positive strains: 0.42 (0.28–0.62); P < 0.001. Regional antibiotic delivery is safe and effectively reduces the risk of SWI in cardiac surgery patients.
Similar content being viewed by others
Introduction
Sternal wound infections (SWIs) are among the most devastating complications following cardiac surgery and significantly increase postoperative morbidity and mortality1. Direct regional antibiotic delivery (RAD) to the sternal edges upon entering and just prior to closing the sternum, along with intravenous (iv) prophylactic antibiotics, has gained attention due to the potential in reducing surgical site infections (SSIs) following cardiac surgery2. Topical antibiotics, such as vancomycin or gentamicin, have been considered as a measure of antibiotic prophylaxis in cardiac surgery by the 2006 Society of Thoracic Surgeons (STS) Practice Guidelines (Class II, Level of Evidence B), which noted concerns about iv antibiotic penetration in the sternal area and the potential for infection with S. aureus3. As a result of additional studies showing the benefits of RAD in preventing SSIs, a class I recommendation (Level of Evidence B) was given in the 2016 prevention and management of sternal wound infections guidelines of the American Association for Thoracic Surgery (AATS) for the application of RAD to the cut edges of the sternum on opening and before closing in all cardiac surgical procedures involving a median sternotomy1. However, there were some concerns regarding potential elevated serum levels of RAD and the possibility of selecting antibiotic-resistant strains. In view of these concerns, the 2017 European Association for Cardio-Thoracic Surgery (EACTS) expert consensus highlighted the importance of careful monitoring and prudent use of this essential antibiotic4.
Controversies arose regarding RAD after recent randomized clinical trials (RCT) found that patients who were assigned to receive either vancomycin-soaked sponges or saline-soaked sponges had a similar occurrence of SWI (2.7% vs. 4.1%; P = 0.23)5. Therefore, the aim of this systematic review and meta-analysis of RCTs was to comprehensively assess the safety and effectiveness of RAD to reduce the risk of SWI in cardiac surgery procedures requiring a sternotomy.
Methods
Data sources and search strategy
Established methods were used in compliance with the updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) in the health care interventions statement6. A PRISMA checklist is available in Supplementary Table 1. We conducted a database screening for relevant studies up to May 16th 2023 through PubMed, EMBASE (Supplementary Table 2), the Cumulative Index of Nursing and Allied Health Literature (CINAHL), the Web of Science, the Cochrane Register of Controlled Clinical Trials, Clinical Key and Google Scholar registries, as well as published proceedings from major cardiac, thoracic, cardiothoracic, and cardiology society meetings. Abstracts were eligible for detailed assessment if available online and reporting outcomes of interest. Search terms included “vancom*cin; -paste, -gel, -ointment, -slurry”; “topical*-, local*-, regional*- vancom*cin”, gentam*cin, antiobiotic*; “vancom*cin/ gentam*cin/ antiobiotic AND stern*”; “vancom*cin/ gentam*cin/ antiobiotic AND mediastin*.” No language, publication date, or publication status restriction was imposed. Both blinded and open-label trials were considered eligible. The most updated or inclusive data for each study were used for abstraction. The references of original and review articles were cross-checked.
Selection criteria and quality assessment
Studies were considered eligible when comparing prophylactic topically administered vancomycin- or gentamicin-based therapy versus no antibiotic or placebo in the setting of cardiac surgery performed via a median sternotomy. We restricted the search to these agents since these are endorsed in the guidelines1. Citations were screened at the title/abstract level and retrieved as full reports if they fulfilled the inclusion criteria: (1) human studies; (2) RCTs and (3) the reporting of a pre-specified outcome of SWI. We excluded studies which (1) were not of a randomized design; (2) reported no control group; (3) evaluated different regimens of RADs; (4) reported no clinical data. Studies in which a combination of different RADs were used and compared with no antibiotic or placebo were also considered for inclusion.
We extracted data for the included studies using a pre-specified datasheet. Variables in the pre-specified datasheet included study characteristics, demographic data, clinical characteristics, interventions, and outcomes.
Two independent reviewers (M.M.K. and M.P.) selected the studies for inclusion and extracted studies and patient characteristics of interest and relevant outcomes. Conflicts were resolved by consensus after discussion with a third reviewer (M.K.). Two authors (M.M.K. and M.P.) independently assessed the trials’ eligibility and risk of bias. The risk of bias for randomized studies was assessed using the components recommended by the Cochrane Collaboration7 including random sequence generation and random allocation; allocation concealment; blinding of participants, personnel, and outcome assessors; incomplete outcome data; selective outcome reporting; and other sources of bias8. Certainty of evidence was assessed by four main factors (risk of bias, inconsistency, indirectness, and imprecision) using the Grading of Recommendations Assessment, Development and Evaluations (GRADE) approach9. The certainty of the evidence was rated from high (ie, we are very confident that the true effect lies close to that of the effect estimate) to very low (ie, we have very little confidence in the effect estimate: the true effect is likely to be substantially different)10. Any discrepancies in bias assessment between the assessors were recorded.
Outcome measures
The primary end point was the occurrence of any SWI in overall, diabetic and no-diabetic population. Secondary end points were the occurrence of deep SWI (DSWI), superficial SWI (SSWI), mediastinitis, and in-hospital mortality. Definitions for the type, degree, and depth of the infection were applied as per the study protocol. The review protocol was registered at PROSPERO database (nr CRD42022385529) and the current meta-analysis represents the portion of the protocol11.
Statistical analysis
The analysis followed the intention-to-treat principle. Continuous variables were presented as mean and standard deviation (SD) for normally distributed data, while non-normally distributed variables were summarized as median and interquartile range (IQR). Group comparisons were conducted using the Mann–Whitney U test or appropriate standard t test. Odds ratios (ORs) with corresponding 95% confidence intervals (CIs) were calculated as summary statistics. Heterogeneity was evaluated using the Cochran Q test12 and the I2 statistic, with thresholds of 25%, 50%, and 75% representing low, moderate, and considerable degrees of heterogeneity, respectively13. Pooled ORs were computed using a random-effects model via the DerSimonian-Laird method, with the Mantel–Haenszel fixed-effects model utilized in case of moderate or low heterogeneity. Publication bias was explored for the primary endpoint using a funnel plot, assessed visually and through linear regression analysis14. To address studies reporting ‘0 events’, calculations were repeated using risk difference (RD) as the primary statistic. Bias risk was evaluated according to the Revised Cochrane risk-of-bias tool (RoB 2) (Supplementary Table 4). Sensitivity analyses were conducted by sequentially removing each study to assess its impact on the pooled results. Additionally, trial sequential analysis (TSA [Version 0.9.5.10 Beta, Copenhagen Trial Unit, Center for Clinical Intervention Research, Rigshospitalet, Copenhagen, Denmark]) was performed to validate the meta-analysis findings for SWI, maintaining a 5% type I error and 80% power. Review Manager 5.4 (The Nordic Cochrane Center, Copenhagen, Denmark) was employed for all analyses..
Results
Studies selection and patients baseline characteristics
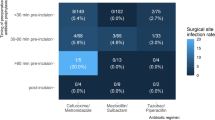
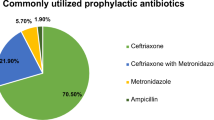
The current systematic review follows the GRADE criteria (Supplementary Table 3). Figure 1 depicts the process of study selection. Thirteen RCTs (7,719 patients) were included in the analysis5,15,16,17,18,19,20,21,22,23,24,25,26. Characteristics of the included studies are summarized in Table 1. Studies were predominantly at a low-to-moderate risk of bias. The median follow-up was three months and ranged from one month19,20,22,25 to one year5,18. Studies analyzed topical vancomycin vs control (2,187 patients)5,15,16,17,18,19,20 and topical gentamicin vs control (5,532 patients)21,22,23,24,25,26 as SWI prophylaxis. Patients’ baseline characteristics are reported in Table 2. Seventy two percent of patients in the vancomycin-based RAD studies were male versus 75% patients in gentamicin-based RAD studies. Median age was 58.77 in vancomycin studies vs 65.25 in gentamicin studies. Diabetes was present in 22.1% of patients in vancomycin studies and 30.4% patients in gentamicin studies. Bilateral internal mammary artery (BIMA) use was not consistently reported.
Among vancomycin-based RAD four studies used paste15,16,19,20, one, vancomycin powder17, one, vancomycin solution18, and one used a sponge soaked in vancomycin5. All gentamicin studies evaluated gentamicin-collagen implants23 or sponges21,22,24,25,26 (Supplementary Table 5). Intra-venous antibiotic prophylaxis consistent mostly of second-or third -generation cephalosporins; one study reported routine iv. cefepime prophylaxis. Six studies reported on the protocol mandated blood glucose levels control17,18,19,21,22,26 (Supplementary Table 5).
Sternal wound infections
SWI definitions are available in Supplementary Table 6. All thirteen studies (7,719) contributed to the analysis of any SWI. The funnel plot for the visual assessment of publication bias is available as Fig. 2A. In the random effects model, topical antibiotic use was associated with an over 50% reduction of the odds of any SWI: OR (95% CIs): 0.49 (0.35–0.68); p < 0.001; I2 = 52%; that was significant regardless of the type of antibiotic (vancomycin vs. no-RAD; 0.34 (0.18–0.64); p < 0.001; I2 = 38% and gentamicin vs no-RAD; 0.58 (0.39–0.86); p = 0.007; I2 = 58%; Pheterogeneity for between subgroups comparison = 0.15. The corresponding rates in the overall cohort were 2.7% (30/1,113) versus 7.1% (76/1,074) for the topical vancomycin and no-vancomycin groups, and 5% (143/2,764) versus 8.2% (226/2,768) for the topical gentamicin and no-gentamicin groups (Fig. 2B).
Analysis of sternal wound infections. A funnel plot for the assessment of publication bias; B individual (blue squares) and summary (black diamonds) odds ratios (ORs) along with 95% confidence intervals (CIs) and the forest plot for the comparison between RAD and no RAD; C Trial sequential analysis. IV, Inverse variance; CI, confidence interval; RAD, regional antibiotic delivery.
Cumulative Z-curve passed the TSA-adjusted boundary for SWIs suggesting adequate power has been met and no further trials are needed; TSA adjusted OR was 0.49 (0.35–0.68) P < 0.001 (Fig. 2C).
Nine studies contributed to the analysis of DSWIs. The effect of topical RAD remained significant with a 40% DSWI odds reduction: OR (95%CIs): 0.60 (0.43–0.83); p = 0.003; I2 = 15%; The effect was similar in vancomycin trials (0.40 [0.17–0.98]; p = 0.05; I2 = 0%) and gentamicin studies (0.64 [0.45–0.92]; p = 0.02; I2 = 15%; Pheterogeneity for between subgroups comparison = 0.35). The corresponding rates in the overall cohort were 1.7% (56/3,270) versus 2.8% (93/3,265) for RAD and no-RAD groups respectively Fig. 3A. Superficial SWIs data were available from 8 studies: RAD was associated with a significant, over 45% reduction of the odds of SSWI: OR (95%CIs): 0.54 (0.32–0.90); p = 0.01; I2 = 63%; that reached borderline significance in gentamicin studies (0.55 (0.30–1.01); p = 0.05; I2 = 70%; Pheterogeneity for between subgroups comparison = 0.71. The corresponding rates in the overall cohort were 3.1 (98/3,132) versus 5.1% (160/3,127) for the RAD and no-RAD groups respectively Fig. 3B.
Analysis of deep sternal wound infections (A) and superficial sternal wound infections (B). Abbreviations as in Fig. 2.
The incidence of mediastinitis was reported in 8 studies respectively; while numerical reduction in mediastinitis odds was seen (OR: 0.74 [0.40–1.37]) I2 = 0%; statistical significance was not reached (P = 0.81). Supplementary Fig. 1. No differences in mortality (OR: 0.99 [0.48–2.06]; p = 0.98; I2 = 5%) between RAD and no-RAD were observed. Supplementary Fig. 2.
Systemic toxicity and microbiology
Studies did not report definition nor specific outcomes on systemic toxicity; three studies reported acute kidney injury (AKI) data; no differences between RAD and no-RAD were found: OR: 1.17 (0.57–2.40); P = 0.67; I2 = 75%). Four studies only reported microbiology data; the occurrence of gram-positive cultures was significantly reduced with both vancomycin and gentamicin based RAD: OR: 0.42 (0.17–1.01); P = 0.05; I2 = 53% and OR: 0.42 (0.27–0.64); P < 0.001; I2 = 40% respectively. One study only reported on the cultures of drug resistant bacteria: there were 4 and 2 cases of methicillin resistant S. Aureus in the gentamicin based RAD and no-RAD respectively; together with 1 case of gentamicin resistant P. Stuarti and 2 cases of S. Epidermidis in the gentamicin based RAD arm constituting total of 0.04% resistance emergence. Meta-analysis was not attempted since one study only reported the data of interest. Details on microbiology findings and systemic toxicity are available as Table 3. No differences in terms of sternal dehiscence or non-union were seen as far as RAD was concerned: Basha et al.15 reported 0 cases of sternal non-union in both vancomycin and control groups; SWIPE trial reports alone on patients’ feeling of chest wall instability (0 vs. 9 for gentamycin sponge and control respectively); remaining studies do not report on these data.
Diabetes versus no-diabetes
We observed no difference in RAD efficacy between diabetic (OR: 0.4 [0.32–0.65]; P < 0.001; I2 = 34%) and non-diabetic (OR: 0.60 [0.45–0.83]; P = 0.002; I2 = 55%) patients (p for subgroup difference p = 0.32). Figure 4.)
Analysis of sternal wound infections in diabetic and no-diabetic population. Abbreviations as in Fig. 2.
Sensitivity analyses
The sensitivity analyses were consistent with the main results. Similarly, we excluded single studies, one at a time and repeated the calculations (Supplementary Table 7) and observed no significant study effect.
Discussion
The current study is the first meta-analysis, focused on randomized controlled trials (RCTs) to address the effectiveness of two most commonly regionally administered antibiotics (RAD) in sternal wound infection (SWI) prophylaxis among patients undergoing cardiac surgeries. The main findings of this study are: (1) the odds of any SWI were significantly reduced by over 50% with any RAD; (2) RAD reduced the odds of SWI in diabetic and non-diabetic patients; (3) both antibiotics reduced the odds of cultures outside their respective serum concentrations’ activity; (4) no evidence of systemic toxicity, sternal dehiscence and resistant strains emergence was found. It is the first meta-analysis to assess jointly vancomycin and gentamicin- based protocols for RAD. Data from previous studies showed a reduction of the incidence of SWI regardless of the RAD protocol. As a result, guideline recommendations were developed, which endorsed the use of local prophylaxis together with systemic iv. antibiotics, tight glycemic control and adequate surgical techniques to control the infection rates (1). However, routine use of RAD has been avoided due to concerns of potential systemic toxicity augmented by local administration. Furthermore, there are claims of the possible emergence of bacterial strains that may develop resistance to vancomycin and gentamicin. Two recent studies5,27 on RAD found no benefit of local vancomycin prophylaxis in SWI reduction, which have fueled the ongoing debate.
Rationale for local antibiotics and SSI reduction
The rationale for using local antibiotics in reducing surgical site infections (SSIs) is based on several key factors. Local antibiotics provide a targeted approach by delivering high concentrations of antimicrobial agents directly to the surgical site, effectively controlling bacteria in the vicinity of the incision. This localized application allows for higher concentrations of antimicrobial agents compared to systemic administration, enhancing their bactericidal effect and reducing bacterial growth. By minimizing systemic exposure, local antibiotics help reduce potential adverse effects and the development of antibiotic resistance. They also serve as an additional layer of prophylaxis against SSIs, inhibiting bacterial colonization at the incision site. Local antibiotics are particularly beneficial in high-risk cases and complement standard infection control practices11. Incorporating local antibiotics into surgical protocols can contribute to the reduction of SSIs and improve patient outcomes.
Local antibiotic prophylaxis in cardiac surgery
The choice between gentamicin and vancomycin for RAD depends on the local antibiotic resistance patterns, specific bacteria targeted and the risk factors for infection. If the risk of gram-negative bacteria is high, such as in certain types of surgeries or patient populations, gentamicin may be preferred. If there is a higher risk of gram-positive bacteria, including MRSA, vancomycin may be more appropriate. Limited reports are available on the synergistic effects of locally applied gentamicin and vancomycin28,29.
Effectiveness
Our meta-analysis found that RAD was effective prophylaxis against SWI; the odds were significantly reduced by over 50%, regardless whether vancomycin or gentamicin local prophylaxis was used.
These findings are in line with those of recent meta-analyses, which also demonstrated the benefit for single antibiotics protocols11,30,31.
The largest to date meta-analysis addressing vancomycin based RAD in addition to SWI incidence benefit, found that the magnitude of benefit varied across patient populations in the risk-regression analysis11. Patients at the highest risk of developing SWI, such as those with diabetes, reached the highest reductions of SWI as compared to controls; the magnitude of benefit from RAD in lowering SWI rates may be even greater if strict glycaemic control protocols are in place; Lazar et al. showed “0 incidence” of SSIs regardless of the baseline HbA1c levels in the previous study in which continuous insulin infusion was used to achieve tight perioperative glycemic control2; Furnary et al. demonstrated in a study of 5,510 patients that glycemic control rather than baseline HbA1c levels correlated with SWI incidence32. This was also noted in gentamicin-based RAD; where in those patients at higher risk of developing SWI such as those in whom BIMA was harvested, the magnitude of benefit was proportionally higher30.
The effectiveness of RAD is, beyond doubt, dependant on the local concentration of antibiotic in the wound. All the actions taken that may reduce this concentration, in turn, may result in the loss of prophylaxis against SSIs. A striking example of this phenomenon was the first large-scale RCT to address the effectiveness of gentamicin in SWI prophylaxis where the authors, in order to facilitate handling, did not follow the manufacturer’s instructions to implant the sponge; in this study, the sponge was soaked in saline prior to placing it between the sternal halves21, which washed away the gentamicin and resulted in no reduction in SSIs. This was later confirmed in an in-vitro study33. Servito et al. soaked the gauze in vancomycin solution placed it on the sternal edges at the time of surgery and then removed the gauze before rewiring the sternum at conclusion of the surgery5. This approach significantly reduced the concentration of the antibiotic when it was dissolved in the saline. It is, in addition, essential for the antibiotic to remain in the wound for as long as possible to act as a prophylactic agent. Similarly, single “sprinkling” of antibiotic solution over the wound as done in another study18 also proved to be ineffective. These flaws were explained in detail in previous reports34,35,36.
Studies to measure the effective concentrations in the wound are available from experimental studies37. When antibiotic wound concentrations are high and serum concentrations remain stable, it was found that the antibiotics were effective against bacteria for which systemic administration is generally not recommended5,38. This finding was partially confirmed in the previous meta-analysis11 which showed that patients who received vancomycin-based RAD and developed infections did not show an increase in vancomycin-resistant strain cultures in infected wounds. Contrarily, vancomycin non-susceptible organisms like Gram-negative strains38 were isolated nearly three times less frequently in the vancomycin group compared to the no-vancomycin group. This finding confirms the results of previous experimental studies. Mączyńska et al. demonstrated the in-vitro efficacy of gentamicin released from a collagen sponge carrier against Pseudomonas aeruginosa and Klebsiella pneumoniae biofilms that displayed a resistance pattern in routine diagnostics39. Additionally, gentamicin was shown in the in-vitro model of infected meshes used for hernia repair to prevent growth of all bacteria, including even gentamicin-resistant S. aureus strains40.
Safety
The current study found no evidence of drug-resistant bacteria growth from the wounds in patients receiving RAD. Indeed, only one single study41 reported 6 cases of MRSA [4 in the gentamicin and 2 in the placebo arm) which together with gentamicin resistant strains (3 vs. 3 in gentamicin and no-gentamicin arms) constituted 0.04% emergence of resistant bacteria when compared to roughly 8% infection rate in the RAD control arm. In addition, an often-raised concern regarding the widespread use antibiotics in general, is its presumed association with an increase in drug resistant strains. It is, however, persistent systemic exposure to sub-inhibitory levels of vancomycin or gentamicin that may cause resistant strains. The development of vancomycin intermediate-resistant Staphylococcus was demonstrated in an in vitro model with persistent vancomycin exposure above 10 mg/L while the emergence of vancomycin resistance has not been reported in studies on the use of topical vancomycin42. Furthermore, extended intravenous prophylaxis or long-term intravenous antibiotic administration may be associated with systemic toxicity. Although none of the studies included in our analysis specifically investigated systemic toxicity, we conducted an analysis of acute kidney injury (AKI) as a potential surrogate endpoint. Similar to our previous findings, we observed no significant differences between patients who received RAD and those who did not in terms of AKI incidence. Application of vancomycin paste or gentamicin sponges did not impair the wound healing process. One histopathological study revealed that gentamicin was highly effective in reducing infection and promoting callus repair, resulting in early bone healing43. Vancomycin paste, in contrast to wax that will hardly be absorbed and produces a foreign body giant cell reaction, is perfectly water-soluble. Limited data was available for the analysis of sternal dehiscence or non-union.
This systematic review and meta-analysis included only 13 studies, number which may have resulted in type I errors due to an increased risk of random errors resulting from sparse studies and data. To gauge the risk of type I errors, we utilized TSA, a method integrating estimated information size (accumulated sample size of incorporated trials) with an adjusted threshold for statistical significance in cumulative meta-analyses. If the cumulative Z-curve intersects the trial sequential monitoring boundary or enters the futility area, it suggests that there might be adequate evidence for the expected intervention effect, and additional trials may not be necessary. Conversely, when the evidence is considered insufficient to draw a conclusion, additional trials are needed to confirm the results. In conducting this TSA, we estimated the required information size using α = 0.05 (two sided) and β = 0.20 (power = 80%) and a relative risk reduction of 20% in outcomes. The cumulative Z-curve surpassed the TSA-adjusted boundary for SWIs indicating that sufficient power has already been reached and robust benefit of RAD in reducing SWIs is well-established, and there is no need for further trials.
Limitations
We must acknowledge several limitations to the current meta-analysis. First, the absence of a standardized prophylaxis protocol across the included studies resulted in varying rates of surgical wound infections (SWIs) in the control groups, contributing to substantial observed heterogeneity. The assessment using ROB analysis indicated a high risk of bias in several studies, although our sensitivity analysis, which excluded those studies, confirmed the consistency of the overall results. Furthermore, there was limited reporting on information regarding off-pump techniques, BIMA use and harvesting techniques, which are known factors that can also influence the occurrence of SWIs. Data on patients with higher risk of opportunistic infections, such as on chronic glucocorticoids or with concomitant hematological diseases was also limited. Data on systemic antibiotic levels were unavailable for other studies in our analysis, limiting our ability to evaluate redosing strategies and the impact of intravenous antibiotics on outcomes.
Conclusions
The results of this systematic review and updated meta-analysis confirm the high effectiveness of the topical antibiotics vancomycin and gentamicin, in preventing sternal wound infections after cardiac surgery without compromising safety and with no signs of side effects including systemic toxicity and emergence of resistant bacteria.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
References
Lazar, H. L. et al. Prevention and management of sternal wound infections. J. Thorac. Cardiovasc. Surg. 152(4), 962–972 (2016).
Lazar, H. L. et al. Topical vancomycin in combination with perioperative antibiotics and tight glycemic control helps to eliminate sternal wound infections. J. Thorac. Cardiovasc. Surg. 148(3), 1035–1038 (2014).
Engelman, R. et al. Workforce on evidence-based medicine, society of thoracic surgeons. The society of thoracic surgeons practice guideline series: Antibiotic prophylaxis in cardiac surgery, part II: Antibiotic choice. Ann. Thorac. Surg. 83(4), 1569–1576 (2007).
Abu-Omar, Y. et al. European Association for Cardio-Thoracic Surgery expert consensus statement on the prevention and management of mediastinitis. Eur. J. Cardiothorac. Surg. 51(1), 10–29 (2017).
Servito, M. et al. Topical vancomycin and risk of sternal wound infections: A double-blind randomized controlled trial. Ann. Thorac. Surg. 114(5), 1555–1561 (2022).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 29(372), n71 (2021).
Higgins, J. P. et al. Bias methods group; cochrane statistical methods group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343, d5928 (2011).
Boutron I, Page M & Higgins JPT et al. Considering bias and conflicts of interest among the included studies. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page M, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions. 2 ed: Wiley-Blackwell; (2019). p. 177–204.
Iorio, A. et al. Use of GRADE for assessment of evidence about prognosis: Rating confidence in estimates of event rates in broad categories of patients. BMJ 16(350), h870 (2015).
Santesso, N. et al. GRADE working group. GRADE guidelines 26: Informative statements to communicate the findings of systematic reviews of interventions. J. Clin. Epidemiol. 119, 126–135 (2020).
Kowalewski M, Pasierski M, Makhoul M et al. Topical vancomycin for sternal wound infection prophylaxis. a systematic review and updated meta-analysis of over 40,000 cardiac surgery patients. Surgery (2023). Accepted in press
Cohen, J. F. et al. Q test was useful to assess heterogeneity in likelihood ratios in studies of diagnostic accuracy. J. Clin. Epidemiol. 68(3), 299–306 (2015).
Ioannidis, J. P., Patsopoulos, N. A. & Evangelou, E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ 335(7626), 914–916 (2007).
Egger, M. et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109), 629–634 (1997).
Basha, M. A. A. et al. Computed tomography imaging assessment of the effect of vancomycin paste on poststernotomy healing. Int. J. Gen. Med. 14, 9287–9296 (2021).
Maldonado, L. A. M. et al. Effect of topical vancomycin on consolidation of sternum surgical fracture in open-heart surgery. J. Cardiothorac. Med. 7, 523–529 (2019).
Mahmood, M. M. et al. Use of tropical vancomycin in decreasing the incidence of surgical site infection in open heart surgery. Pak. J. Med. Health Sci. 15, 968–970 (2021).
Pervaiz, F. et al. Topical vancomycin in cardiac surgery to reduce sternal wound infections: A randomized controlled trial at a tertiary cardiac care facility. J. Surg. Surg. Res. 5, 15–18 (2019).
Shah, S. J. & Jadhav, U. E. Efficacy of topical vancomycin application in cardiac surgery to reduce deep sternal wound infection: A randomised control trial at tertiary cardiac care hospital. Int. Surg. J. 9, 601–605 (2022).
Vander Salm, T. J. et al. Reduction of sternal infection by application of topical vancomycin. J. Thorac. Cardiovasc. Surg. 98, 618–622 (1989).
Bennett-Guerrero, E. et al. SWIPE-1 trial group. Effect of an implantable gentamicin-collagen sponge on sternal wound infections following cardiac surgery: A randomized trial. JAMA. 304(7), 755–762 (2010).
Balkanay, O. O. Does locally administered gentamicin affect the incidence of sternal wound infections after coronary artery bypass graft surgery?. Turk. J. Thorac. Cardiovasc. Surg. 23(1), 32–38 (2015).
Eklund, A. M., Valtonen, M. & Werkkala, K. A. Prophylaxis of sternal wound infections with gentamicin-collagen implant: Randomized controlled study in cardiac surgery. J. Hosp. Infection 59(2), 108–112 (2005).
Friberg, O. et al. Local gentamicin reduces sternal wound infections after cardiac surgery: A randomized controlled trial. Ann. Thorac. Surg. 79(1), 153–161 (2005).
Schimmer, C. et al. Gentamicin-collagen sponge reduces sternal wound complications after heart surgery: A controlled, prospectively randomized, double-blind study. J. Thorac. Cardiovasc. Surg. 143(1), 194–200 (2012).
Schimmer, C. et al. Prevention of surgical site sternal infections in cardiac surgery: A two-centre prospective randomized controlled study. Eur. J. Cardiothorac. Surg. 51(1), 67–72 (2017).
Lander, H. L. et al. Vancomycin paste still does not reduce the incidence of deep sternal wound infection after cardiac surgery. J. Thorac. Cardiovasc. Surg. 156(3), 1125–1126 (2018).
Bertazzoni Minelli, E. et al. Antimicrobial activity of gentamicin and vancomycin combination in joint fluids after antibiotic-loaded cement spacer implantation in two-stage revision surgery. J. Chemother. 27(1), 17–24 (2015).
Andreas, M. et al. Direct sternal administration of Vancomycin and Gentamicin during closure prevents wound infection. Interact Cardiovasc. Thorac. Surg. 25(1), 6–11 (2017).
Kowalewski, M. et al. Gentamicin-collagen sponge reduces the risk of sternal wound infections after heart surgery: Meta-analysis. J. Thorac. Cardiovasc. Surg. 149(6), 1631–1640 (2015).
Kowalewski, M. et al. Meta-analysis to assess the effectiveness of topically used vancomycin in reducing sternal wound infections after cardiac surgery. J. Thorac. Cardiovasc. Surg. 154(4), 1320–1323 (2017).
Furnary, A. P. & Wu, Y. Clinical effects of hyperglycemia in the cardiac surgery population: The Portland diabetic project. Endocr. Pract. : Off. J. Am. Coll. Endocrinol. Am. Assoc. Clin. Endocrinol. 12(Suppl 3), 22–26 (2006).
Li, Y. & Zhou, J. A preliminary exploration of the efficacy of gentamicin sponges in the prevention and treatment of wound infections. Infect. Drug Resist. 14, 2633–2644 (2021).
Pasierski, M. et al. Devil is in the detail-how to critically analyze studies designed to assess effectiveness of topical antibiotics in preventing sternal wound infections?. J. Thorac. Dis. 11(Suppl 15), S1861–S1864 (2019).
Lazar, H., Suwalski, P., Lorusso, R., Meani, P. & Kowalewski, M. Topical vancomycin for sternal wound infection prophylaxis. Reinventing the wheel all over again. Ann. Thorac. Surg. 116(2), 440–441 (2022).
Lazar, H. L. Vancomycin paste should be used in all sternotomies. Ann. Thorac. Surg. 115(6), 1561–1562 (2023).
Thomassen, M. B. et al. Local concentrations of gentamicin obtained by microdialysis after a controlled application of a GentaColl sponge in a porcine model. J. Orthop. Res : Off. Publ. Orthop. Res Soc. 38(8), 1793–1799 (2020).
Holmes, N. E. et al. Treatment of methicillin-resistant Staphylococcus aureus: Vancomycin and beyond. Semin. Respir. Crit. Care Med. 36(1), 17–30 (2015).
Maczynska, B. et al. In vitro efficacy of gentamicin released from collagen sponge in eradication of bacterial biofilm preformed on hydroxyapatite surface. PloS one 14(6), e0217769 (2019).
Wiegering, A. et al. Gentamicin for prevention of intraoperative mesh contamination: Demonstration of high bactericide effect (in vitro) and low systemic bioavailability (in vivo). Hernia 18(5), 691–700 (2014).
Tsuji, B. T., Rybak, M. J., Lau, K. L. & Sakoulas, G. Evaluation of accessory gene regulator (agr) group and function in the proclivity towards vancomycin intermediate resistance in Staphylococcus aureus. Antimicrob. Agents Chemother. 51(3), 1089–1091 (2007).
Ghobrial, G. M. et al. Complications from the use of intrawound vancomycin in lumbar spinal surgery: A systematic review. Neurosurg. Focus. 39(4), E11 (2015).
Ramot, Y. et al. Treatment of contaminated radial fracture in Sprague-Dawley rats by application of a degradable polymer releasing gentamicin. J. Toxicol. Pathol. 34(1), 11–22. https://doi.org/10.1293/tox.2020-0041 (2021).
Acknowledgements
Work by Thoracic Research Centre (www.trc.org.pl)
Funding
This research did not receive any specific funding from any agencies in the public, commercial, or not-for-profit areas.
Author information
Authors and Affiliations
Consortia
Contributions
Study design, conceptualization, writing and revision were performed by all of the authors. The literature search, data screening, data extraction and statistical analysis were performed by MK, MK, TU, MEDP. Supervision and project administration were performed by MK and HL. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kowalewski, M., Kołodziejczak, M.M., Urbanowicz, T. et al. Regional antibiotic delivery for sternal wound infection prophylaxis a systematic review and meta-analysis of randomized controlled trials. Sci Rep 14, 9690 (2024). https://doi.org/10.1038/s41598-024-60242-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-60242-z
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.