Abstract
Pancreatic cancer is a commonly occurring malignant tumor, with pancreatic ductal carcinoma (PDAC) accounting for approximately 95% of cases. According of its poor prognosis, identifying prognostic factors of pancreatic ductal carcinoma can provide physicians with a reliable theoretical foundation when predicting patient survival. This study aimed to analyze the impact of marital status on survival outcomes of PDAC patients using propensity score matching and machine learning. The goal was to develop a prognosis prediction model specific to married patients with PDAC. We extracted a total of 206,968 patient records of pancreatic cancer from the SEER database. To ensure the baseline characteristics of married and unmarried individuals were balanced, we used a 1:1 propensity matching score. We then conducted Kaplan–Meier analysis and Cox proportional-hazards regression to examine the impact of marital status on PDAC survival before and after matching. Additionally, we developed machine learning models to predict 5-year CSS and OS for married patients with PDAC specifically. In total, 24,044 PDAC patients were included in this study. After 1:1 propensity matching, 8043 married patients and 8,043 unmarried patients were successfully enrolled. Multivariate analysis and the Kaplan–Meier curves demonstrated that unmarried individuals had a poorer survival rate than their married counterparts. Among the algorithms tested, the random forest performed the best, with 0.734 5-year CSS and 0.795 5-year OS AUC. This study found a significant association between marital status and survival in PDAC patients. Married patients had the best prognosis, while widowed patients had the worst. The random forest is a reliable model for predicting survival in married patients with PDAC.
Similar content being viewed by others
Introduction
Pancreatic cancer is among the group of malignant tumors of the digestive tract that mainly originate from the ductal epithelium and alveolar cells of the pancreas. Approximately 95% of these tumors are pancreatic ductal carcinoma (PDAC), which has the fourth-highest mortality rate among cancers1. According to a global report in the year 2020, there were 495,773 newly diagnosed cases of pancreatic cancer and 466,003 fatalities. Notably, the incidence of pancreatic cancer was almost equivalent to the observed mortality rate2. Pancreatic cancer is projected to become the second most common cause of cancer-related deaths worldwide by 20303,4. Despite significant advances in diagnosis and treatment, the prognosis of PDAC remains poor, with a 5-year survival rate of only 8–9%5,6. Surgical resection remains the only curative approach, but is often associated with poor outcomes and many postoperative complications7. Several factors, including age8, tumor stage, tumor size, lymph node metastasis, and treatment modalities, have been identified to impact the survival of PDAC patients. Notably, marital status has been shown to be an independent prognostic factor for perioperative and long-term survival among pancreatic cancer patients9. However, previous studies failed to consider the influence of confounding factors. Therefore, it is essential to account for confounding factors and thoroughly examine the association between marital status and the prognosis of PDAC in clinical practice.
Marriage, as a social phenomenon, represents a form of social support that bears great significance in the lives of human beings. Previous studies indicates that one's marital status can considerably influence their physical and mental well-being, including but not limited to cancer incidence and prognosis10. Marital support, emotional, financial stability and access to healthcare resources have been proposed to significantly influence cancer outcomes for married patients. In contrast, unmarried individuals are more likely to experience high levels of stress, social isolation, and lack of support, which may lead to poorer survival rates among cancer patients. Previous research has demonstrated that unmarried individuals have a higher risk of mortality in several types of cancers, including non-small cell lung cancer11, breast cancer12, laryngeal squamous cell carcinoma13, duodenal adenocarcinoma14, and esophageal cancer15, among others.
In this study, we utilized the SEER database to analyze the marital status of PDAC patients at the time of diagnosis and employed propensity score matching (PSM) to investigate the potential association between marital status and prognosis of PDAC. Additionally, we leveraged machine learning techniques to predict the survival time of married patients with PDAC.
Materials and methods
Ethics approval and consent to participate
The SEER database provides publicly available data for this study, which means that obtaining informed consent from participants or ethical approval from an institutional review board is not necessary. We obtained access to the 1979–2019 SEER Research Data File by signing a Data-Use Agreement that outlines the terms and conditions for access.
Data source and patient selection
We utilized the SEER*Stat software (Version 8.4.0.1) to gather comprehensive data submitted to SEER until November 2021. In order to obtain patients with primary pancreatic site, we implemented the International Classification of Diseases for Oncology (ICD-O-3) topographical codes (C25.0-C25.3, C25.7-C25.9). We included patients diagnosed with ICD-O-3 histology/behavior codes of 8140/3 (adenocarcinoma) or 8500/3 (infiltrating duct adenocarcinoma) as part of our inclusion criteria. On the other hand, patients with pancreatic Islets of Langerhans (C25.4) tumor origin were excluded. Also, patients with missing/unknown/undifferentiated data on marital status, 6th AJCC stage and T/N/M stage, race, tumor differentiation, treatment information and the cause of death, as well as those with unknown or less than 1 month survival time were eliminated.
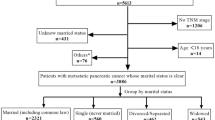
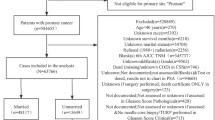
Following the application of our selection criteria, we identified a sum of 24,044 pancreatic ductal adenocarcinoma (PDAC) patients to serve as pertinent subjects for this investigation. Two patient clusters were then defined according to the marital status, namely, the married or unmarried group. A detailed flow-process diagram representation of our rigorous screening procedure is provided by Fig. 1.
Variable classification
Our analysis incorporated a range of factors from the database such as sex, age at diagnosis, marital status, race, grade, TNM stage (6th), and primary site surgery. Age was dichotomized into two groups: those aged < 50 years and those aged ≥ 50 years. With regard to marital status, we distinguished participants as either married or unmarried groups based on their recorded statuses at the time of diagnosis. The unmarried group was composed of those who were divorced/separated, single, or widowed.
Outcome measurement
In our study, we operationalized overall survival (OS) as the interval from the date of diagnosis to either the date of patient's decease or the last recorded follow-up instance if still alive. Similarly, cancer-specific survival (CSS) was gauged by determining the duration from the date of diagnosis to the date of death attributable solely to PDAC.
Statistical analysis
To minimize potential confounding variables between married and unmarried patients, we gathered data on potential covariates such as sex, age, race, grade, TNM stage (6th), and primary site surgery for 1-to-1 propensity score matching (the nearest-neighbor method with a stringent caliper of 0.001), utilizing the R package of MatchIt. We utilized the chi-square test to assess differences in categorical variables and estimated OS and CSS by generating survival curves using the Kaplan–Meier method. Through the implementation of log-rank tests, we evaluated survival comparisons between distinct groups. To investigate possible prognostic factors and examine the hazard ratios, we employed both univariate and multivariable Cox proportional-hazards regression models.
With the aim of establishing a machine learning model, patients within the married group were partitioned into a training set and a test set at random, at an 8:2 ratio. Within the training set, we developed the K-nearest neighbor, artificial neural network, Naïve Bayes, and random forest models aimed at predicting the 5-year CSS and OS of married patients with PDAC. K-nearest neighbor (KNN) is a non-parametric algorithm that classifies or predicts outcomes based on the majority class or average of ‘k’ closest data points in the feature space. Artificial Neural Network (ANN) is composed of interconnected nodes (neurons) organized in layers, designed to learn and make predictions by adjusting the weights of connections during the training process. Naïve Bayes is a probabilistic algorithm that leverages Bayes' theorem, assuming independence between features, to calculate the likelihood of a particular class based on the observed data. Random Forest (RF) in machine learning prediction models is an ensemble learning method that constructs multiple decision trees during training and outputs the mode of the classes (classification) or the mean prediction (regression) of the individual trees for robust and accurate predictions.
All statistical analyses were carried out using R software (version 4.1.3) and SPSS software (version 25) with statistical significance set at two-sided P < 0.05.
Results
Pathological features and baseline characteristics
The SEER database provided data on a total of 206,968 PDAC patients for potential inclusion in our study. Ultimately, 24,044 individuals were deemed suitable after a series of screening procedures, as delineated in Fig. 1. Notably, of the eligible patients, 15,024 (62.49%) were classified as married and 9,020 (37.51%) as unmarried. Additional details regarding pathological features are elaborated in Table 1. Moreover, after executing the primary comparisons, significant differences were noted between the married and unmarried cohorts with regard to sex, race, TNM stage, and surgery status, with all values recorded as P ≤ 0.001 (Table 1).
The primary comparison assessed the impact of marital status on OS and CSS
In univariate Cox regression analysis, mortality rates associated with PDAC were demonstrated to be significantly linked with seven variables, including sex, age, race, grade, TNM stage, primary site surgery, and marital status for both OS and CSS (P < 0.05; Table 2). Upon conducting multivariate Cox regression analysis to further investigate survival factors, we found that marital status, as well as sex, race, grade, TNM stage, and surgery status, emerged as independent prognostic factors that significantly influenced OS and CSS outcomes in patients with PDAC (P < 0.001; Table 3).
The secondary comparison assessed the impact of marital status on both OS and CSS
To eliminate for potential confounding variables such as age, sex, and race between the married and unmarried groups, we employed the 1:1 propensity score matching method. After matching, 8043 married patients and an equal number of unmarried patients (for a total of 8043 individuals) were successfully enrolled. Notably, the baseline characteristics were found to be well-balanced between the two groups (Table 4; Fig. 2), and no significant differences were observed (P > 0.05).
The findings indicate that, with the exception of race, all baseline characteristics were significant predictors of both OS and CSS (Table 5). In the univariate analysis after propensity-score matching, being unmarried (with reference to married) remained a statistically significant predictive risk factor of death (OS: HR = 0.870, 95% CI = 0.842–0.898, P < 0.001; CSS: HR = 0.882, 95% CI = 0.853–0.912, P < 0.001). Upon subjecting relevant variables to further multivariate analysis, all components maintained independent significance in predicting OS/CSS with the exception of sex. Moreover, unmarried status (with reference to married) exhibited a noteworthy negative influence on survival outcomes (OS: HR = 0.834, 95% CI 0.808–0.861, P < 0.001; CSS: HR = 0.845, 95% CI 0.817–0.873, P < 0.001; Table 5). It is worth noting that patients diagnosed prior to age 50, those with stage I cancer, well-differentiated tumors, and those who had undergone surgery were observed to be more likely to experience an improvement in both OS and CSS compared to their respective reference groups (Table 5).
The Kaplan–Meier curves presented in Fig. 3 indicate that unmarried individuals have a significantly lower survival rate than married individuals (P < 0.001). To further investigate the prognosis of different unmarried statuses, we grouped unmarried patients into separated/divorced, single, and widowed subgroups. As shown in Fig. 4, we found that there was a significant difference between their OS/CSS and different marital statuses (P < 0.001).
In the secondary comparison, we utilized a forest plot to evaluate the impact of different kinds of unmarried statuses versus married status. As illustrated in Fig. 5, separated/divorced patients (OS: aHR = 1.134, 95% CI 1.082–1.189, P < 0.001; CSS: aHR = 1.119, 95% CI 1.066–1.175, P < 0.001), single patients (OS: aHR = 1.142, 95% CI 1.091–1.196, P < 0.001; CSS: aHR = 1.140, 95% CI 1.087–1.195, P < 0.001), and widowed patients (OS: aHR = 1.319, 95% CI = 1.261–1.377, P < 0.001; CSS: aHR = 1.291, 95% CI 1.233–1.352, P < 0.001) exhibit poorer survival outcomes relative to married patients. Additionally, we observed that widowed patients have the highest risk of death among the three unmarried statuses (Figs. 4 and 5).
Machine-learning based outcome prediction in patients who married
To explore the factors that influence the survival of married patients with PDAC, we utilized age, sex, race, tumor differentiation, TNM stage, and surgery status as input parameters for developing machine learning prediction models of the 5-year CSS and 5-year OS. The performance metrics of the algorithms for the four models are presented in Table 6. Among the machine learning models, the random forest model exhibits superior discrimination performance. For predicting the 5-year CSS, the random forest model achieves an AUROC of 0.734, accuracy of 0.592, recall of 0.552, specificity of 0.806, precision of 0.939, and F1 score of 0.695. The 5-year OS results are 0.795, 0.572, 0.536, 0.940, 0.989, and 0.695 for AUROC, accuracy, recall, specificity, precision, and F1 score, respectively. Artificial neural network, naïve bayes, and k-nearest neighbor follow with AUROCs of 0.788, 0.771, and 0.708, respectively. Receiver operating characteristics (ROC) curves and AUROCs of the four models are displayed in Fig. 6. By using GridSearch, the hyperparameters of the optimal random forest model were: N_estimators = 100, Max_depth = 10, Min_samples_leaf = 2, Min_samples_split = 4, Max_features = auto (Table S1).
The calibration curves demonstrated an excellent agreement between predictions and observations (Fig. 7). For predicting the 5-year CSS, the k-nearest neighbor, artificial neural network, naïve bayes and random forest models gave brier scores of 0.125, 0.118, 0.134, and 0.118, respectively. Similarly, while the 5-year OS, brier scores of 0.080, 0.073, 0.106, and 0.072 were obtained using the same models, as outlined in Table 7.
In this study, the clinical effectiveness of four predictive models was assessed using decision curves and clinical impact curves. The DCA curve (Fig. 8) indicated that the random forest model had a greater net benefit compared to the "treat none" or "treat all" schemes across a threshold probability range of 0.6 to 1.0. Further, the random forest model exhibited superior clinical impact when compared to the other models. Notably, when the threshold probability was set above 75% (Fig. 9), the number of positive cases predicted by the models (i.e., those at high risk) was closely matched the number of true-positive cases (i.e., those who actually had high-risk outcomes). Considering all four evaluation metrics, it can be concluded that the random forest algorithm performed the best for prediction purposes and could offer more precise and systematic treatment guidance and support to married patients with PDAC.
Discussion
Marital status has been shown to be associated with survival in chronic diseases such as cancer, with married individuals having a longer life expectancy and better quality of life in various diseases. For instance, Cheng Xu et al. used a matching method to discover that married patients had better 5-year CSS/OS than unmarried patients with NPC from 1973 to 201216. Gino Inverso et al. also observed a significant protective impact of marital status on metastatic oral cancer and laryngeal cancer17. However, while studies have confirmed that marital status is a prognostic factor for pancreatic cancer using SEER database, the available studies have failed to exclude confounding factors9,18,19. Previous studies have found that sex, age, stage, race20 and surgery21 were associated with the survival of PDAC patients. Therefore, to improve comparability between married and unmarried patients, we conducted a 1:1 propensity matching using the SEER database to screen eligible patients with PDAC, resulting in relatively reliable results based on well-matched datasets. As well as a larger sample size, our study could provide more robust results compared with previous studies. Male sex, age over 50 years, higher TNM stage, worse tumor differentiation, and no surgical treatment were determined to be risk factors for prognosis, and married patients had better survival outcomes; however, their unmarried counterparts had significantly poor OS/CSS.
The current study found that marital status plays a significant role in PDAC patients, and we suspect that several possible reasons exist. First, marriage provides positive social support. It has been found that widowed, divorced, and separated individuals lack legal relationships, partner support and help during diagnosis and treatment, and are hence at a higher risk of psychological distress22. Similarly, relative to married patients, unmarried patients are more likely to experience negative emotional states for a prolonged period due to the absence of social support and partner companionship, which could lead to physiological dysfunctions resulting from long-term exposure to glucocorticoids and catecholamines, negatively affecting the tumor microenvironment and tumor growth, migration and stimulating angiogenesis, thus affecting the prognosis23. Healthy marital status plays an essential role in establishing a good psychological state, reducing negative emotions, such as anxiety and depression, and improving survival rate10,24. Secondly, stable marital relationships are typically associated with higher economic status, and family members such as spouses and children may provide financial and spiritual support for long-term treatment25. In other words, stable marital status can improve patient compliance with the treatment regimen comparatively26. In addition, married people with a good economic base are more likely to purchase health insurance and can receive some Medicaid at the time of diagnosis27. Furthermore, studies have found that patients with private health insurance are found in a greater proportion of early stages of cancer, have longer survival time and better prognosis. Patients without private health insurance, on the other hand, are usually detected at an advanced stage of cancer and have a poor prognosis28. Thirdly, married individuals typically adopt healthier lifestyles, with better diets, more exercise, and less substance abuse, contributing to better healthy outcomes. It has been shown that bad habits such as smoking and alcoholism are risk factors for the development of pancreatic ductal carcinoma, while unmarried people are more likely to be infected26. Lastly, in daily life, family members of married patients are more likely to detect early symptoms of PDAC, resulting in early detection and diagnosis and positive impacts on disease treatment.
Recently, machine learning has been widely used in the medical field29. Some researchers have developed prognostic prediction models for pancreatic cancer using machine learning methods, because machine learning algorithms are more accurate than traditional statistical methods in predicting survival outcome in the fifth year30. Specifically, in this study, the k-nearest neighbor, artificial neural network, naïve bayes, and random forest algorithms were used to predict the 5-year CSS and OS for married patients with PDAC. The results indicate that the random forest algorithm outperformed the other models in predicting 5-year CSS/OS, especially in its good discriminative performance and its AUROC value was high, indicating that the model could better distinguish between lives and deaths. Furthermore, since random forest has good generalization capability, it can avoid the overfitting issue. Moreover, the random forest model stands out in prognostic prediction tasks due to its superior predictive accuracy, robustness to noisy data, interpretability through feature importance analysis, capacity to handle non-linearity, generalization to unseen data, stability, and ease of implementation. Our study presents the first predictive model based on machine learning algorithms that predicts the survival impact of married patients with PDAC, which demonstrates excellent performance and provides doctors with an easily accessible and more accurate survival prediction tool for married patients with PDAC, which may guide clinical practice better. It must be admitted that with the rapid evolution of machine learning, particularly in deep learning, ensemble methods, and reinforcement learning, have led to models with increased predictive power. Therefore, we believe that our prediction model would be improved with the development of machine learning and provide more accurate prediction.
Although marriage has positive impacts on cancer outcomes, it is vital to note that not all marriages are beneficial for health. Marital conflict and stress may lead to negative effects on health, including increased risk of depression, anxiety, and heart disease. Thus, future studies should investigate the quality of marital relationships and the impact of marital therapy on cancer patient health outcomes.
Limitations
Although the results of this study indicates that marital status is a significant prognostic factor for PDAC, it is not without limitations.
Firstly, the SEER database contains limited clinical characteristics of patients and lacks critical risk factors such as tobacco smoking, alcohol consumption, type 2 diabetes, chronic pancreatitis, and family history of pancreatic cancer31. The lack of accurate screening before data matching may result in biased conclusions. Particularly, diabetes confers a 3.05-fold increased risk of PDAC onset in diabetic individuals compared to non-diabetic individuals32. Secondly, the absence of data on the quality of life of patients in the SEER database, such as socioeconomic level and living environment, the quality of life of patients were not available for inclusion in our analysis. Thirdly, the marital status extracted in this study was recorded only at diagnosis, and dynamic follow-up surveys assessing changes in marital status during PDAC treatment were not taken. This may pose information bias on clinical outcomes. We cannot understand marital status during the later treatment of patients, which may have some information bias. Fourthly, our classification of PDAC patients living together with partners but not legally married as single patients may underestimate survivorship outcomes among this group, which may be better than that of unmarried or single patients. Despite the limited proportion of such patients, they may impact the conclusions of this study. Finally, this study's generalizability may be limited to the population under investigation, as cultural variations, disparities in living standards, and economic differences between countries may influence the applicability of these findings to patients in other regions.
Conclusion
Our study provides evidence that marital status is an independent prognostic factor for PDAC. Future studies should investigate the mechanisms behind this association and the impact of marital quality and therapy on cancer outcomes. We established machine learning predictions about the survival of married patients with PDAC, with the RF model performing best.
Data availability
The data used in this study are available free of charge online at http://www.seer.cancer.gov on request.
Change history
22 March 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41598-024-57179-8
Abbreviations
- aHR:
-
Adjusted hazard ratio
- ANN:
-
Artificial neural network
- CI:
-
Confidence interval
- CSS:
-
Cause-specific survival
- K-nn:
-
K-nearest neighbor
- NB:
-
Naïve Bayes
- RF:
-
Random forest
- ROC:
-
Receiver operating characteristics
- OS:
-
Overall survival
- PDAC:
-
Pancreatic ductal carcinoma
References
Siegel, R. et al. Cancer statistics. CA Cancer J. Clin. 64(1), 9–29 (2014).
Jian-xiong, Hu. et al. Pancreatic cancer: A review of epidemiology, trend, and risk factors. World J. Gastroenterol. 27(27), 4298–4321 (2021).
Collisson, E. A. et al. Molecular subtypes of pancreatic cancer. Nat. Rev. Gastroenterol. Hepatol. 16(4), 207–220 (2019).
Neoptolemos, J. P. et al. Therapeutic developments in pancreatic cancer: Current and future perspectives. Nat. Rev. Gastroenterol. Hepatol. 15(6), 333–348 (2018).
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2019. CA Cancer J. Clin. 69(1), 7–34 (2019).
Gupta, R., Amanam, I. & Chung, V. Current and future therapies for advanced pancreatic cancer. J. Surg. Oncol. 116(1), 25–34 (2017).
Mizrahi, J. D., Surana, R., Valle, J. W. & Shroff, R. T. Pancreatic cancer. Lancet (London, England) 395(10242), 2008–2020. https://doi.org/10.1016/S0140-6736(20)30974-0 (2020).
Xu, Y. et al. Prognostic effect of age in resected pancreatic cancer patients: A propensity score matching analysis. Front. Oncol. 12, 789351. https://doi.org/10.3389/fonc.2022.789351 (2022).
Baine, M. et al. Marital status and survival in pancreatic cancer patients: A SEER based analysis. PloS One 6(6), e21052. https://doi.org/10.1371/journal.pone.0021052IF:3.752Q2 (2011).
Irani, E., Park, S. & Hickman, R. L. Negative marital interaction, purpose in life, and depressive symptoms among middle-aged and older couples: Evidence from the Health and Retirement Study. Aging Mental Health 26(4), 860–869. https://doi.org/10.1080/13607863.2021.1904831 (2022).
Chen, Z. et al. Marital status independently predicts non-small cell lung cancer survival: A propensity-adjusted SEER database analysis. J. Cancer Res. Clin. Oncol. 146(1), 67–74. https://doi.org/10.1007/s00432-019-03084-x (2020).
Hefei, L. et al. Real-world study of the effect of marital status on survival in early breast cancer patients. Oncol. Res. Clin. 34(3), 198–203. https://doi.org/10.3760/cma.j.cn115355-20211205-00560 (2022).
Wang G., Zhu S., Yang M., Ming X., Yang X., Chen X., et al. Effect of marital status on patients with laryngeal squamous cell carcinoma: based on SEER database. New Med. Vol. 32, No.6, (2022).
Wang, N. et al. Effect of marital status on duodenal adenocarcinoma survival: A surveillance epidemiology and end results population analysis. Oncol. Lett. 18(2), 1904–1914 (2019).
Liu H., Meng X., Xin D., Liu D., Fan Q., Wang F., et al. Effect of marital status on survival of patients with distant metastatic esophageal cancer. Journal Esophageal Dis. Vol. 1 No. 1 (2019).
Xu, C. et al. Impact of marital status at diagnosis on survival and its change over time between 1973 and 2012 in patients with nasopharyngeal carcinoma: A propensity score-matched analysis. Cancer Med. 6(12), 3040–3051. https://doi.org/10.1002/cam4.1232 (2017).
Inverso, G. et al. Marital status and head and neck cancer outcomes. Cancer 121(8), 1273–1278. https://doi.org/10.1002/cncr.29171 (2015).
Wang, X. et al. Marital status independently predicts pancreatic cancer survival in patients treated with surgical resection: An analysis of the SEER database. Oncotarget 7, 24880–24887 (2016).
Ma, X. et al. Development of a prognostic nomogram for metastatic pancreatic ductal adenocarcinoma integrating marital status. Sci. Rep. 12, 7124 (2022).
Rawla, P., Sunkara, T. & Gaduputi, V. Epidemiology of pancreatic cancer: Global trends, etiology and risk factors. World J. Oncol. 10(1), 10–27. https://doi.org/10.14740/wjon1166 (2019).
Benassai, G. et al. Long-term survival after curative resection for pancreatic ductal adenocarcinoma–Surgical treatment. Int. J. Surg. 21(Suppl 1), S1–S3. https://doi.org/10.1016/j.ijsu.2015.06.050 (2015).
Holmes, T. H. & Rahe, R. H. The social readjustment rating scale. J. Psychosom. Res. 11(2), 213–218. https://doi.org/10.1016/0022-3999(67)90010-4 (1967).
Antoni, M. H. et al. The influence of bio-behavioural factors on tumour biology: Pathways and mechanisms. Nat. Rev. Cancer 6(3), 240–248. https://doi.org/10.1038/nrc1820 (2006).
Zhu, P., Chen, C., Liu, X., Gu, W. & Shang, X. Factors associated with benefit finding and mental health of patients with cancer: A systematic review. Support. Care Cancer 30(8), 6483–6496. https://doi.org/10.1007/s00520-022-07032-3 (2022).
Xu, C. et al. Socioeconomic factors and survival in patients with non-metastatic head and neck squamous cell carcinoma. Cancer Sci. 108(6), 1253–1262. https://doi.org/10.1111/cas.13250 (2017).
Ding, Z., Yu, D., Li, H. & Ding, Y. Effects of marital status on overall and cancer-specific survival in laryngeal cancer patients: A population-based study. Sci. Rep. 11(1), 723. https://doi.org/10.1038/s41598-020-80698-z (2021).
Yang, K. B. et al. Contribution of insurance status to the association between marital status and cancer-specific survival: A mediation analysis. BMJ Open 12(9), e060149. https://doi.org/10.1136/bmjopen-2021-060149 (2022).
Zhao, J. et al. Health insurance status and cancer stage at diagnosis and survival in the United States. CA Cancer J. Clin. 72(6), 542–560. https://doi.org/10.3322/caac.21732 (2022).
Choi, R. Y., Coyner, A. S., Kalpathy-Cramer, J., Chiang, M. F. & Campbell, J. P. Introduction to machine learning, neural networks, and deep learning. Transl. Vis. Sci. Technol. 9(2), 14. https://doi.org/10.1167/tvst.9.2.14 (2020).
Yokoyama, S. et al. Predicted prognosis of patients with pancreatic cancer by machine learning. Clin. Cancer Res. 26(10), 2411–2421. https://doi.org/10.1158/1078-0432.CCR-19-1247 (2020).
Maisonneuve, P. & Lowenfels, A. B. Risk factors for pancreatic cancer: A summary review of meta-analytical studies. Int. J. Epidemiol. 44(1), 186–198. https://doi.org/10.1093/ije/dyu240 (2015).
Sharma, S., Tapper, W. J., Collins, A. & Hamady, Z. Z. R. Predicting pancreatic cancer in the UK biobank cohort using polygenic risk scores and diabetes mellitus. Gastroenterology 162(6), 1665-1674.e2. https://doi.org/10.1053/j.gastro.2022.01.016 (2022).
Funding
This study was supported by the Fujian Province young and middle-aged teachers education and scientific research project (No: JAT210115).
Author information
Authors and Affiliations
Contributions
Conceptualization and methodology, L.Y.; writing—original draft preparation, Y.H.; writing—review and editing, Q.C. and W.L.; validation, Z.H., H.L. and R.D.; formal analysis, Q.C. and J.L.; data curation, Y.H. All authors have read and agreed to the published version of the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: In the original version of this Article, Affiliations were not listed in the correct order. Full information regarding the corrections made can be found in the correction for this Article.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, Q., Hu, Y., Lin, W. et al. Studying the impact of marital status on diagnosis and survival prediction in pancreatic ductal carcinoma using machine learning methods. Sci Rep 14, 5273 (2024). https://doi.org/10.1038/s41598-024-53145-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-53145-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.