Abstract
The COVID-19 pandemic has substantially affected people and healthcare systems. One of the main challenges was the reduction and change in the pattern of non-COVID-19 diseases and conditions. Moreover, due to the mental burden of the pandemic, the trend of poisonings and abuses changed. In this study, we aimed to assess the trends of poisonings from different agents before and during the COVID-19 pandemic using the interrupted time series method. This study was conducted at one of the main Tehran referral centers for poisoning, Baharloo Hospital. Pre-COVID-19 period was defined as April 2018 to January 2020 while the COVID-19 time was from February 2020 to March 2022. The total number of monthly poisoning cases in addition to eight categories of drugs/substances/agents were identified, including drugs (such as psychiatric drugs, cardiovascular drugs, and analgesics), opioids, stimulants, methanol, ethanol, cannabis, pesticides, and carbon monoxide. Interrupted time series analysis was performed to compare the pre-pandemic trend of total monthly cases from each category in addition to the proportion (%) of each one. In total, 13,020 cases were poisoned during the study period, among which 6088 belonged to the pre-pandemic period and 6932 were admitted during the COVID-19 era. There was no significant difference in terms of demographic characteristics of patients before and during the pandemic (p-value > 0.05). At the beginning of the pandemic, there was a sudden fall in the number of poisoning patients (− 77.2 cases/month, p-value = 0.003), however, there was a significant increasing trend during the COVID time (3.9 cases/month, p-value = 0.006). Most of the categories had a sharp decrease at the beginning of the pandemic except for methanol and ethanol which had increases, although not significant. Cannabis also had a significant change in slope (− 0.6 cases/month, p-value = 0.016), in addition to the sudden decrease at the beginning of the pandemic (− 10 cases/month, p-value = 0.007). Regarding the proportion of each category from total monthly poisoning cases, methanol, and ethanol had immediate rises of 4.2% per month and 10.1% per month, respectively (both significant). The pandemic had significant effects on the pattern of poisonings from different agents in Iran, the most important of which were alcohol (ethanol and methanol). These differences had policy implications that can be helpful for policymakers and healthcare systems in combating similar situations in the future.
Similar content being viewed by others
Introduction
The pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2) changed the patterns of hospitalizations in several medical conditions1. Although the coronavirus disease of 2019 (COVID-19) led to the hospitalization of a large number of patients worldwide2, a decrease was observed in hospitalizations due to other medical conditions requiring acute care1; which was reported to be up to 32% in a study3. They found the most significant decreases in asthma, chronic obstructive pulmonary disease (COPD), and heart failure admissions. However, respiratory-related admissions (e.g., respiratory failure) and hospitalization following traumatic brain injury increased. Moreover, the pandemic affected hospital admissions and readmissions related to the mental health4 which could lead to higher drug and substance overdose.
The COVID-19 pandemic has also changed the trend of hospitalizations related to poisoning as well as deaths related to poisonings5,6. For instance, Hadeiy et al. found a higher rate of alcohol intoxication and intoxication-related mortality during the COVID-19 pandemic compared to before7. Moreover, opioid overdose was reported to be higher than pre-COVID-19 than during the pandemic in the United States8. Another retrospective study found a lower rate of patients with carbon monoxide (CO) intoxication needing treatment in Germany9. Using interrupted time series analysis, a nationwide study among young children in the United States showed that there was an immediate increase in the ingestion of cannabis, opioids, and ethanol10.
Several studies compared hospitalizations due to alcohol intoxications before and during the COVID-19 pandemic7,11,12, while some also investigated cannabis use in some limited populations13. However, there is not much evidence regarding hospitalization trends of these two types of poisoning in large-scale studies and also there is no literature regarding the poisoning with other substances such as opioids, CO gas, stimulants, and pesticides before and during the pandemic. Therefore, comparing the trends and slope of hospitalizations before and during COVID-19, as well as the sudden change at the start of the pandemic, can help policymakers update guidelines for informing, preventing, and treating poisonings, and also may be useful in preparation for following pandemics. In this study, we used interrupted time series analysis to compare hospitalizations due to poisonings in Tehran, Iran before and during COVID-19. We investigated the number of each poisoning and the ratio of them before and after the COVID-19 pandemic with a monthly interrupted time series method. This method has been used in several similar instances and for COVID-197,14,15.
Methods
Study population and design
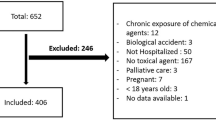
This retrospective cross-sectional study was performed in Baharloo Hospital, a referral hospital for poisoning and COVID-19 patients in Tehran, Iran. Hospitalized patients from April 2018 to March 2022 who were confirmed poisoning cases entered the study. The Iranian Ministry of Health announced the official initiation of the COVID-19 pandemic in Iran in February 2020. Therefore, the pre-COVID-19 and post-COVID pandemics were defined as April 2018–January 2020 and February 2020 to March 2022, respectively. The following baseline characteristics were collected from electronic health records (EHR) and clinical documents: sex, age, marital status, job status, residency, physiological disorders, addiction history, suicide history, and cause of poisoning were compared between pre- and post-COVID-19 periods.
Types of drugs/poisonings
The following nine groups of substances causing poisoning were detected from the manifestation of patients and toxicological analysis (screen tests and confirmation tests).
(1) Ethanol intoxication (ICD-10 code: T51.0, F10.12); (2) Methanol intoxication, (ICD-10 codes: T51.1); (3) Opioid intoxication, which includes natural or synthetic opioids and opioid drugs such as tramadol, methadone drugs, detected (ICD-10 codes: T40.0, T40.1, T40.2, T40.3, T40.4, and T40.6); (4) Stimulant intoxication include drugs such as cocaine and amphetamines, (ICD-10 codes: T43.6, and T40.5); (5) Drug intoxication, defined as anti-psychotics, anti-depressants, anti-convulsants, cardiovascular drugs, and analgesics (ICD-10 codes: T43.0, T43.1, T43.2, T43.4, T43.4, T43.5, and T46); (6) CO poisoning (ICD-10: T58), (7) Cannabis intoxication (ICD-10: T40.7, F12.12), and (8) Pesticide intoxication (ICD-10: T60).
Statistical analysis
In descriptive and analytical analysis, data were presented as mean ± standard deviation (SD) for continuous variables and number (percentage) for categorical variables. Chi-squared test and independent t-test were utilized for evaluating differences between pre- and post-COVID-19 periods, for categorical and continuous variables, respectively. The Kolmogorov–Smirnov test was used to evaluate the normal distribution of data.
Interrupted time series analysis (ITS) is a quasi-experimental time series analysis that involves statistical analysis of tracking a long-term period before and after a point of intervention such as the COVID-19 epidemic. In this method, outcomes are measured constantly at different time points before and after special events and the change in trend and levels of those particular outcomes are determined. The Newey–West method was used to conduct ITS incorporating autocorrelation assumption by defining a lag and based on the Breusch–Godfrey (BG) approach16,17,18. ITS was used for totally poisoned patients and each group of substances that caused poisoning. Also, the proportion of each type of substance was separately analyzed. Finally, the test of Dickey and Fuller was used to assess the non-stationary assumption19.
STATA 17 (Stata Corp LLC, Texas, USA) was used to perform ITS and measurement of trends during the pre- and post-COVID-19 period. A p-value of ≤ 0.05 was considered statistically significant.
Ethics approval and consent to participate
All participants provided written informed consent. This study was approved by the ethics committee of the Tehran University of Medical Sciences (IR.TUMS.MEDICINE.REC.1400.1330) and was conducted in accordance with the Declaration of Helsinki.
Results
Baseline characteristics of patients
A total of 13,020 patients were poisoned from April 2018 to March 2022, of which 6088 were during the pre-COVID time and 6932 during the COVID-19 pandemic. The mean age of patients was 32.42 ± 9.11 years (mean ± SD) and 8007 (61.5%) were male. Most of the patients were single (68.7%) and 90% lived in urban areas. The rate of unemployment increased from 18% in the pre-pandemic era to 20.2% during the pandemic, which was not statistically significant (p-value = 0.06). Table 1 shows all baseline characteristics of all patients and also before and after COVID-19. There was no statistical difference between sex, age, marital status, job status, residence area, psychological disorder, addiction history, and suicide history before and after COVID-19.
Total poisoning trend
The poisoning trend was ascending before COVID-19 initiation with a significant increase of 1.6 monthly cases (95% CI 0.023 to 3.171, p-value = 0.047). At the start of the COVID-19 pandemic, there was a sudden significant decrease in poisonings (− 77.211 cases/month, 95% CI − 126.662 to − 27.759, p-value = 0.003). However, the change in the slope of the trend was not significant (p-value = 0.148). Also, the trend slope was significant in an increasing manner during the COVID-19 pandemic (p-value = 0.006). All of these are described in Table 2 and Fig. 1.
Interrupted time series analysis of poisoning numbers by each substance/drug
Drugs
Figure 2A represents the trend for drug poisonings and the ratio of drug poisonings before and after COVID-19. In total, 4013 drug poisonings were recorded from April 2018 to March 2022, among which 1805 were before February 2020 and 2208 were reported during the pandemic. As Table 3 shows, before the pandemic drug poisoning was at a significantly increasing trend of 0.4 cases per month while at the initiation of the COVID-19 pandemic in Iran, a significant drop of − 22.08 monthly cases was observed (p-value = 0.021).
Interrupted time series analysis of the absolute number of poisonings from each category before and after the COVID-19 pandemic; (A) Drugs, (B) Opioids, (C) Stimulants, (D) Cannabis, (E) Methanol, (F) Ethanol, (G) Pesticides and (H) Carbon Monoxide; Dashed line represents COVID-19 outbreak; m month.
Opioids
There were 2524 opioid poisoning before the pandemic and 2225 cases during the pandemic, the trend of which is illustrated in Fig. 2B. Before the pandemic, there was a slight insignificant increasing trend in opioid poisonings that changed significantly after the pandemic (1.47 cases per month, p-value = 0.006, Table 3) and led to an increasing trend of 1.53 monthly cases during the pandemic (p-value < 0.001). Moreover, at the beginning of the pandemic, a sudden decrease of − 49.04 monthly cases of opioid poisoning was observed (p-value = 0.006).
Stimulants
Before the pandemic, there were 332 patients with stimulant poisoning, and 336 cases during the COVID-19 pandemic course. As shown in Fig. 2C and Table 3, before the pandemic, stimulants had an increasing trend of 0.371 monthly cases (95% CI 0.131 to 0.612, p-value = 0.003). At the time of the COVID-19 pandemic initiation in Iran, a decrease of 8 cases per month was observed (95% CI − 13.98 to − 1.94, p-value = 0.011). However, the changes in slope and slope after COVID-19 were not significant.
Cannabis
A total of 491 patients were admitted due to poisoning, among which 268 were before the pandemic. There was an increasing trend in cannabis poisoning before February 2020 (0.579 cases/month, 95% CI 0.240 to 0.918, p-value = 0.001, Table 3, Fig. 2D). While there was a sudden decrease in February 2020 (p-value = 0.007), the slope decreased significantly (− 0.597, 95% CI − 1.079 to − 0.116, p-value = 0.016).
Methanol
Regarding methanol poisoning, there were 101 methanol poisoning patients before February 2020 and 108 during the pandemic. As shown in Fig. 2E and Table 4, there was an insignificant increasing trend of 0.18 cases per month which had a sudden increase of 5.3 monthly cases at the time of COVID-19 initiation, although insignificant. The trend slope changed in a decreasing manner (− 0.798, 95% CI − 1.233 to − 0.363, p-value = 0.001), resulting in a decreasing trend of − 0.622 cases (p-value = 0.003).
Ethanol
A total of 639 and 1286 patients had ethanol poisoning before and after the COVID-19 era, respectively. As shown in Fig. 2F, the slope of the ethanol poisoning trend changed from diminishing to rising after the COVID-19 pandemic in Iran. This change was significant (1.1, 95% CI 0.113 to 2.087, p-value = 0.030, Table 4). A monthly increase of 0.904 cases was observed since February 2020 (p-value = 0.008).
Pesticides
Totally 775 patients were admitted due to pesticide poisoning and 328 (42.3%) were before the pandemic. There was no significant trend before COVID-19 in terms of pesticide poisoning (p-value = 0.292, Table 4). Also, the change in slope was increasing despite being insignificant which resulted in a significant trend of 0.335 cases/month during the COVID-19 period (p-value = 0.029) (Fig. 2G).
CO
Before the pandemic, 91 patients presented with CO poisoning while 70 patients were after COVID-19 initiation in the country. CO poisoning had no significant trend before and after COVID-19 (p-value = 0.472 and 0.122, respectively) (Fig. 2H). As described in Table 4, the level change and slope change were not significant as well.
Interrupted time series analysis of poisoning ratio by each substance/drug
The trends of the proportion of each type of poisoning from the overall poisoning cases are shown in Fig. 3A–H. The statistics and ITS analysis results are described in Tables 5 and 6.
Drugs
The trend for drug poisoning ratio was not significant either before or after the COVID-19 era. The level change and slope change were not significant as well (p-value = 0.737 and 0.103, respectively).
Opioids
While there was a mild insignificant decreasing trend in opioids proportion before the pandemic, which changed insignificantly to a mild increasing trend (slope change 0.365%, 95% CI − 0.021% to 0.752%, p-value = 0.063). However, the level change at the time of the COVID-19 pandemic initiation was significant showing a sudden decrease of − 8.8% (p-value = 0.001).
Stimulants
Stimulants had an increasing trend which was changed to decreasing after COVID-19 initiation, however, the slope before, after, and slope change was not significant.
Cannabis
The cannabis poisoning percentage from the total poisonings was rising before February 2020 (0.195%, 95% CI 0.077% to 0.314%, p-value = 0.002). There was a significant decrease in trend slope after the pandemic (− 0.253%, 95% CI − 0.431% to − 0.073%, p-value = 0.007).
Methanol
The methanol poisoning ratio had an increasing trend before the pandemic which was not significant. At the time of COVID-19 initiation, a sudden increase of 4.2% was observed in methanol poisoning percentage (p-value = 0.045). Moreover, the slope decreased by − 0.41% (p-value = 0.001), resulting in a − 0.35% post-COVID trend.
Ethanol
The slopes before and after the pandemic in addition to slope change were not significant. Only the level change in February 2020 was significant with an increase of 10.1% (p-value = 0.008).
Pesticides
No significant trend was observed for pesticide poisoning percentage trend before and after the pandemic. Also, the level change and slope change were not significant (p-value = 0.434 and 0.881, respectively).
CO
The proportion of CO poisoning was not changed in terms of trends before and after the COVID-19 pandemic. There was a mild increasing trend both before and after the pandemic.
Discussion
To the best of our knowledge, this study was the first to investigate the poisoning patterns related to different drugs/substances before and after the COVID-19 pandemic. With the assessment of more than 13,000 patients, we found no difference between the demographic characteristics of the patients before and during the pandemic. In overall poisoning cases, while there was an increasing trend before the pandemic, there was a sudden drop in the first month of COVID-19. However, the trend slope was rising during the COVID-19 pandemic as well. Other main findings of the current study were: (1) there was a sudden decrease in the rates of all poisonings except ethanol and methanol, (2) the overall trend was rising for all poisonings other than methanol and cannabis, and (3) although all there was a sudden decrease in all poisoning admissions at the beginning of the pandemic, the proportion of ethanol and methanol poisonings had significant increases.
The COVID-19 pandemic had a profound impact on healthcare systems all around the world. These effects included decreased hospitalization from non-COVID-19 diseases and conditions and increased in-hospital mortality20,21. For instance, in Spain, a decrease of 22% in non-COVID medical and 33% in surgical hospitalizations was observed during the first wave of the pandemic22. In another study conducted in the United States as well, a steep decline was observed in admissions other than COVID-19 during the first months of the pandemic20. This was observed in several other studies as well23,24,25,26. Similarly, we found a significant decrease in poisoning admissions at our center, mostly due to the allocation of available beds to patients with COVID-19.
The global use of alcohol has increased from 1990 to 2017 and the trend is still upward27. The COVID-19 pandemic increased the rate of consumption and changed the patterns of using alcohol28. Several surveys found higher alcohol consumption in the United States during the COVID-19 pandemic compared to 201929,30,31,32. In the report National Center for Health Statistics (NCHC) published in November 2022, they found a sharp increase in alcohol-related mortality with the emergence of COVID-1933. Although the increase rate between 2000 and 2018 was about 7% in alcohol-related deaths, this was changed to 26% from 2019 to 2020 which can be the effect of the COVID-19 pandemic. Another study in Iran found a 13.8% increase in hospital admissions due to alcohol intoxication in the first six months of the pandemic7. In addition to the global trend of increasing alcohol intake and the effect of the COVID-19 pandemic on this trend, Iranians believed that drinking ethanol can prevent or treat COVID-1934. Similar to the mentioned studies, we found a significant increase in the slope of ethanol intoxication in our center which changed the downward trend of ethanol intoxication before the pandemic to an upward trend.
Consuming and marketing ethanol in every form (e.g., beer, wine, etc.) is illegal in Iran. However, a meta-analysis found a 12% prevalence of last 1-year alcohol consumption in the general population in Iran which was 15% higher in young people35. This prevalence is not consistent in different regions of Iran due to cultural differences. Due to the illegal use of handmade alcoholic beverages in Iran, methanol intoxication is a public health issue. In a report, 768 intoxications were reported in 23 days, of which 69 died. Our study showed that the trend was upward for methanol intoxication before the pandemic. The COVID-19 emergence increased methanol intoxication in our center which can be explained by several reasons including the shortage of ethanol at the beginning of the pandemic as ethanol was mainly used for hand sanitizers in addition to the myth that ethanol can prevent and treat COVID-19 which increased the use of handmade beverages in Iran resulting in more methanol intoxication.
The Centers for Disease Control and Prevention (CDC) reported that about 50% of deaths due to drug overdose in the United States involved synthetic opioids36. This study found that the trend is upward with an increase of 1040% in opioid-related mortality from 2013 to 2019. Another study conducted by Olfson et al. found an increase in the rate of opioid overdose deaths from 2000 to 2017 in the United States; however, the proportion of opioid-related suicide reduced from 9 to 4%37. Although there are several challenges in collecting accurate data for opioid overdose in Iran38, a study estimated that about 65% of drug-related deaths in Iran are due to opioid overdose39. Similar to the global trend, we found an upward trend for opioid overdose in our center. Interestingly, the pandemic dramatically increased the slope of opioid overdose. This finding is in line with a study conducted in the United States which showed that COVID-19 significantly increased the rate of opioid-related deaths8.
Regarding total drug poisonings, rising trends were observed both before and during the pandemic. Drugs investigated comprised benzodiazepines, anti-depressants, anti-psychotics, and analgesics. The change in poisoning trends from these drugs might reflect the effect of the pandemic on the mental status of populations, attributable to social distancing and isolation, economic problems, and uncertainty about the future of the pandemic40,41,42. Several early studies reported conflicting results for benzodiazepine use after the initiation of the COVID-19 pandemic, with some reporting an increase in their use43,44, and some reporting a decrease45,46. A more recent study conducted in Spain which compared the patterns of benzodiazepine use and misuse in the first two years of the pandemic and compared it with the previous 2 years found that benzodiazepines used were significantly higher during the COVID-19 time, in particular clonazepam, the most frequent benzodiazepine consumed47. In anti-depressant use, an ITS study conducted in Israel, the use of anti-depressants changed from a decreasing trend to an increasing trend during the pandemic48. This was observed in nationwide data from Europe and the United States as well49,50. This further emphasizes the substantial risk that the pandemic posed to people’s mental health to the extent that it is described as a “mass social trauma”51. All these increased uses of drugs increase the chance of abuse and poisoning from them.
Stimulant poisoning had an increasing trend before the pandemic, however, there was a sudden decrease at the beginning of the pandemic. Stimulants consisted of amphetamines and cocaine. In a study conducted on young children, no immediate change was observed in cocaine and amphetamine ingestion rates at the pandemic initiation time10. However, a decreasing trend was observed for amphetamine ingestion after the pandemic. Similar to our study’s findings, in an interesting study that assessed the use, price, and availability of several drugs and substances worldwide, a decrease in amphetamine and cocaine use was observed during the pandemic52.
As the most widely used illicit substance worldwide, cannabis was estimated to have 192 million users in 201853. Although opium has long been the main illicit drug used in Iran, in recent years, cannabis has also increased use mostly among high school and university students53,54. This increasing trend was also reflected in poisoning patterns found in our study. However, the pandemic led to a sudden decrease in the poisoning related to cannabis and also the trend. This is in line with findings from a community survey in the United States55. Conversely, in the global estimates, 42% of countries reported increased use of cannabis52. It should be noted that there might be increased use of marijuana during the pandemic due to the mental effects of the pandemic, however, the poisoning which stems from the dangerous use of cannabis might have decreased.
Finally, there is not much reported data regarding poisoning from pesticides in the literature. However, an increasing trend after the pandemic has several implications for policymaking. Intentional and unintentional uses should be addressed as the pesticide’s use has increased in recent years56.
Our study has several policy implications which should be highlighted. First, is the fact that there was a sudden decrease in the rate of poisoning while the trend was increasing for most of the substances. Policymakers should take this into consideration in similar situations such as pandemics or even endemics. The increase in methanol and ethanol intoxication is of high importance since it can be a potentially lethal condition with similar events in the past in the country. Educating the normal population and preparing for this rise among healthcare systems in these conditions could be doable actions for future crises. Future studies should focus on the impact of other aspects of the COVID-19 pandemic such as vaccination and each wave of the COVID-19 pandemic.
Despite investigating a large number of patients for assessment of trends in a referral center of poisoning in Iran, this study has some limitations. First, due to the single-center nature of our study, the generalizability of our findings might be threatened. Second, there are some inherent biases for ITS analysis, including history bias, cofounders, and the impact of other interventions and policies during the assessed period57,58. Third, although one of our findings might be a sudden reduction in poisoning-related hospitalizations, the fear of referring to hospitals and social distancing might have been effective. Finally, several factors such as the introduction of vaccines, different waves of COVID-19, and lockdown policies might be other determinants of drug/substance abuse that might not be interpretable with a single stratification into pre-COVID and COVID time. All of these suggest further research on these trends considering these factors and comparing the effect of each on overall poisonings.
Conclusion
Although the COVID-19 pandemic has been announced to be not a major challenge anymore, there are several lessons that can help policymakers in the future. The impact of a pandemic on the trends of poisoning is one of the most affected ones. Our findings suggest that although there was a sudden fall in all poisonings at the beginning of the COVID-19 pandemic, the trend slope increased. Among poisoning agents, ethanol and methanol had immediate increases at the initiation of the pandemic which was accompanied by a decreasing trend during the pandemic for methanol. Opioids, drugs, stimulants, and ethanol had rising trends during the COVID-19 pandemic. Public health policies should benefit from these results for designing and making preventive plans for future situations59.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- EHR:
-
Electronic health records
- ICD:
-
International classification of diseases
- ITS:
-
Interrupted time series
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- SD:
-
Standard deviation
References
Birkmeyer, J. D., Barnato, A., Birkmeyer, N., Bessler, R. & Skinner, J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff. 39(11), 2010–2017 (2020).
Steele, M. K. et al. Estimated number of COVID-19 infections, hospitalizations, and deaths prevented among vaccinated persons in the US, December 2020 to September 2021. JAMA Netw. Open 5(7), e2220385 (2022).
Nourazari, S. et al. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am. J. Emerg. Med. 42, 203–210 (2021).
Raffagnato, A. et al. The impact of the two-year COVID-19 pandemic on hospital admission and readmissions of children and adolescents because of mental health problems. Front. Public Health 11, 1152876 (2023).
Behnoush, A. H. et al. Impact of COVID-19 on poisoning-related mortality in Iran: An interrupted time series study. Int. J. Drug Policy 117, 104051 (2023).
Alhussein, N. et al. The effect of the COVID-19 lockdown on the frequency of acute poisoning presentation to adult and pediatric emergency departments. Cureus 15(1), e33581 (2023).
Hadeiy, S. K. et al. An interrupted time series analysis of hospital admissions due to alcohol intoxication during the COVID-19 pandemic in Tehran, Iran. Sci. Rep. 12(1), 10574 (2022).
Ghose, R., Forati, A. M. & Mantsch, J. R. Impact of the COVID-19 pandemic on opioid overdose deaths: A spatiotemporal analysis. J. Urban Health 99(2), 316–327 (2022).
Prost, M. et al. Influence of the COVID-19 pandemic on causes for the development of carbon monoxide intoxications. Undersea Hyperbaric Med. 49(4), 479–483 (2022).
Raffa, B. J. et al. Ingestion of illicit substances by young children before and during the COVID-19 pandemic. JAMA Netw. Open 6(4), e239549 (2023).
Estedlal, A. R. et al. Temperament and character of patients with alcohol toxicity during COVID-19 pandemic. BMC Psychiatry 21(1), 49 (2021).
Pigeaud, L., de Veld, L., van Hoof, J. & van der Lely, N. Acute alcohol intoxication in Dutch adolescents before, during, and after the first COVID-19 lockdown. J. Adoles. Health 69(6), 905–909 (2021).
Myran, D. T. et al. Unintentional pediatric poisonings before and during the COVID-19 pandemic: A population-based study. Am. J. Emerg. Med. 76, 185–192 (2023).
Maleki, M., Mahmoudi, M. R., Wraith, D. & Pho, K.-H. Time series modelling to forecast the confirmed and recovered cases of COVID-19. Travel Med. Infect. Dis. 37, 101742 (2020).
Mahmoudi, M. R., Baleanu, D., Mansor, Z., Tuan, B. A. & Pho, K.-H. Fuzzy clustering method to compare the spread rate of Covid-19 in the high risks countries. Chaos Solitons Fractals 140, 110230 (2020).
Newey, W. K. & West, K. D. A Simple, Positive Semi-definite, Heteroskedasticity and Autocorrelation Consistent Covariance Matrix (1986).
Breusch, T. S. Testing for autocorrelation in dynamic linear models. Austral. Econ. Pap. 17(31), 334–355 (1978).
Godfrey, L. G. Testing against general autoregressive and moving average error models when the regressors include lagged dependent variables. Econometrica 46, 1293–1301 (1978).
Dickey, D. A. & Fuller, W. A. Distribution of the estimators for autoregressive time series with a unit root. J. Am. Stat. Assoc. 74(366a), 427–431 (1979).
Dang, A. et al. Hospitalizations and mortality from non-SARS-CoV-2 causes among medicare beneficiaries at US hospitals during the SARS-CoV-2 pandemic. JAMA Netw. Open 5(3), e221754 (2022).
Bartolomeo, N., Giotta, M. & Trerotoli, P. In-hospital mortality in non-COVID-19-related diseases before and during the pandemic: A regional retrospective study. Int. J. Environ. Res. Public Health 18(20), 10886 (2021).
Gasch-Illescas, A. et al. Impact of the first wave of the COVID-19 pandemic on non-COVID inpatient care in southern Spain. Sci. Rep. 13(1), 1634 (2023).
Caminiti, C. et al. Effects of the COVID-19 epidemic on hospital admissions for non-communicable diseases in a Large Italian University-Hospital: A descriptive case-series study. J. Clin. Med. 10(4), 880 (2021).
Moynihan, R. et al. Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open 11(3), e045343 (2021).
Rennert-May, E. et al. The impact of COVID-19 on hospital admissions and emergency department visits: A population-based study. PLoS ONE 16(6), e0252441 (2021).
Abebe, W. et al. Trends of follow-up clinic visits and admissions three-months before and during COVID-19 pandemic at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia: An interrupted time series analysis. BMC Health Serv. Res. 21, 1–10 (2021).
Manthey, J. et al. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: A modelling study. Lancet 393(10190), 2493–2502 (2019).
Murthy, P. & Narasimha, V. L. Effects of the COVID-19 pandemic and lockdown on alcohol use disorders and complications. Curr. Opin. Psychiatry 34(4), 376–385 (2021).
Dempsey, S. K., Glicksberg, L., Rausch, A. J., Christensen, H. & Casey, B. K. Alcohol use trends in Dallas County during the COVID-19 pandemic. Forensic Sci. Int. Rep. 7, 100318 (2023).
White, A. M., Castle, I. P., Powell, P. A., Hingson, R. W. & Koob, G. F. Alcohol-related deaths during the COVID-19 pandemic. JAMA 327(17), 1704–1706 (2022).
Pollard, M. S., Tucker, J. S. & Green, H. D. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw. Open 3(9), e2022942 (2020).
Barbosa, C., Cowell, A. J. & Dowd, W. N. Alcohol consumption in response to the COVID-19 pandemic in the United States. J. Addict. Med. 15(4), 341–344 (2021).
Spencer, M. R., Curtin, S. C. & Garnett, M. F. Alcohol-induced death rates in the United States, 2019–2020. NCHS Data Brief. 448, 1–8 (2022).
Aghababaeian, H., Hamdanieh, L. & Ostadtaghizadeh, A. Alcohol intake in an attempt to fight COVID-19: A medical myth in Iran. Alcohol 88, 29–32 (2020).
Chegeni, M. et al. Alcohol consumption in Iran: A systematic review and meta-analysis of the literature. Drug Alcohol Rev. 39(5), 525–538 (2020).
Mattson, C. L. et al. Trends and geographic patterns in drug and synthetic opioid overdose deaths—United States, 2013–2019. Morb. Mortal. Wkly. Rep. 70(6), 202–207 (2021).
Olfson, M., Rossen, L. M., Wall, M. M., Houry, D. & Blanco, C. Trends in intentional and unintentional opioid overdose deaths in the United States, 2000–2017. JAMA 322(23), 2340–2342 (2019).
Rostami, M. & Rezaeian, S. Challenges of estimates in drug-related overdose deaths in Iran: Evidence from the literature. Iran J. Public Health 49(8), 1592–1593 (2020).
Akhgari, M., Jokar, F. & Etemadi, A. A. Drug related deaths in Tehran, Iran: Toxicological, death and crime scene investigations. IJT 5(12), 402–409 (2011).
Jacques-Aviñó, C. et al. Gender-based approach on the social impact and mental health in Spain during COVID-19 lockdown: A cross-sectional study. BMJ Open 10(11), e044617 (2020).
Marí-Dell’Olmo, M. et al. Socioeconomic inequalities in COVID-19 in a European urban area: Two waves, two patterns. Int. J. Environ. Res. Public Health 18, 1256 (2021).
González-Rodríguez, A. & Labad, J. Mental health in times of COVID: Thoughts after the state of alarm. Med. Clin. 155(9), 392–394 (2020).
Gili, A. et al. Changes in drug use patterns during the COVID-19 pandemic in Italy: Monitoring a vulnerable group by hair analysis. Int. J. Environ. Res. Public Health 18, 4 (2021).
McCarthy, C. P. et al. Early clinical and sociodemographic experience with patients hospitalized with COVID-19 at a large American healthcare system. EClinicalMedicine 26, 100504 (2020).
Niles, J. K., Gudin, J., Radcliff, J. & Kaufman, H. W. The opioid epidemic within the COVID-19 pandemic: Drug testing in 2020. Popul. Health Manag. 24(S1), S43–S51 (2021).
Downs, C. G., Varisco, T. J., Bapat, S. S., Shen, C. & Thornton, J. D. Impact of COVID-19 related policy changes on filling of opioid and benzodiazepine medications. Res. Soc. Adm. Pharm. 17(1), 2005–2008 (2021).
Perelló, M. et al. Changes in prescription drug abuse during the COVID-19 pandemic evidenced in the Catalan pharmacies. Front. Public Health 11, 1116337 (2023).
Frangou, S. et al. Increased incident rates of antidepressant use during the COVID-19 pandemic: Interrupted time-series analysis of a nationally representative sample. Psychol. Med. 53, 1–9 (2022).
Estrela, M. et al. Prescription of anxiolytics, sedatives, hypnotics and antidepressants in outpatient, universal care during the COVID-19 pandemic in Portugal: A nationwide, interrupted time-series approach. J. Epidemiol. Community Health 76(4), 335–340 (2022).
Rabeea, S. A., Merchant, H. A., Khan, M. U., Kow, C. S. & Hasan, S. S. Surging trends in prescriptions and costs of antidepressants in England amid COVID-19. Daru 29(1), 217–221 (2021).
Reger, M. A., Stanley, I. H. & Joiner, T. E. Suicide mortality and coronavirus disease 2019—A perfect storm? JAMA Psychiatry 77(11), 1093–1094 (2020).
Farhoudian, A. et al. A global survey on changes in the supply, price, and use of illicit drugs and alcohol, and related complications during the 2020 COVID-19 pandemic. Front. Psychiatry 12, 646206 (2021).
Rostam-Abadi, Y. et al. Evidence for an increase in cannabis use in Iran—A systematic review and trend analysis. PLoS ONE 16(8), e0256563 (2021).
Nazarzadeh, M. et al. Prevalence of Cannabis lifetime use in iranian high school and college students: A systematic review, meta-analyses, and meta-regression. Am. J. Mens Health 9(5), 397–409 (2015).
Goodyear, K., Moyo, P., Avila, J. C., Ahluwalia, J. S. & Monnig, M. A. Associations between alcohol and cannabis use before and during the COVID-19 pandemic: Results of a community survey. Addict. Behav. Rep. 16, 100455 (2022).
Boedeker, W., Watts, M., Clausing, P. & Marquez, E. The global distribution of acute unintentional pesticide poisoning: Estimations based on a systematic review. BMC Public Health 20(1), 1875 (2020).
Ewusie, J. E. et al. Methods, applications, interpretations and challenges of interrupted time series (ITS) data: Protocol for a scoping review. BMJ Open 7(6), e016018 (2017).
Lopez Bernal, J., Cummins, S. & Gasparrini, A. The use of controls in interrupted time series studies of public health interventions. Int. J. Epidemiol. 47(6), 2082–2093 (2018).
Wittchen, H. U. et al. What are the high risk periods for incident substance use and transitions to abuse and dependence? Implications for early intervention and prevention. Int. J. Methods Psychiatr. Res. 17(Suppl 1), S16–S29 (2008).
Author information
Authors and Affiliations
Contributions
A.H.B., E.B.: Writing—original draft/Conceptualization/Formal analysis/Visualization, A.K.: Writing—original draft/Data curation, A.J.M., N.B., A.R.D.: Writing—review & editing, B.B.: Supervision/Writing—review & editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Behnoush, A.H., Bazmi, E., Khalaji, A. et al. The trend of poisonings before and after the COVID-19 pandemic. Sci Rep 14, 2098 (2024). https://doi.org/10.1038/s41598-024-52537-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-52537-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.