Abstract
Low skeletal muscle index (SMI) and low skeletal muscle radiodensity (SMD) are associated with reduced survival time in pancreatic ductal adenocarcinoma (PDAC). The negative prognostic impact of low SMI and low SMD is often reported as independent of cancer stage when using traditional clinical staging tools. Therefore, this study sought to explore the relationship between a novel marker of tumour burden (circulating tumour DNA) and skeletal muscle abnormalities at diagnosis of PDAC. A retrospective cross-sectional study was conducted in patients who had plasma and tumour tissue samples stored in the Victorian Pancreatic Cancer Biobank (VPCB) at diagnosis of PDAC, between 2015 and 2020. Circulating tumour DNA (ctDNA) of patients with G12 and G13 KRAS mutations was detected and quantified. Pre-treatment SMI and SMD derived from analysis of diagnostic computed tomography imaging was tested for its association to presence and concentration of ctDNA, as well as conventional staging, and demographic variables. The study included 66 patients at PDAC diagnosis; 53% female, mean age 68.7 years (SD ± 10.9). Low SMI and low SMD were present in 69.7% and 62.1% of patients, respectively. Female gender was an independent risk factor for low SMI (OR 4.38, 95% CI 1.23–15.55, p = 0.022), and older age an independent risk factor for low SMD (OR 1.066, 95% CI 1.002–1.135, p = 0.044). No association between skeletal muscle stores and concentration of ctDNA (SMI r = − 0.163, p = 0.192; SMD r = 0.097, p = 0.438) or stage of disease according to conventional clinical staging [SMI F(3, 62) = 0.886, p = 0.453; SMD F(3, 62) = 0.717, p = 0.545] was observed. These results demonstrate that low SMI and low SMD are highly prevalent at diagnosis of PDAC, and suggest they are comorbidities of cancer rather than related to the clinical stage of disease. Future studies are needed to identify the mechanisms and risk factors for low SMI and low SMD at diagnosis of PDAC to aid screening and intervention development.
Similar content being viewed by others
Introduction
Pancreatic ductal adenocarcinoma (PDAC) is associated with a persistently poor survival rate with only 6.7% of Australian patients surviving longer than five years from diagnosis1. Most patients present with advanced disease, with less than 20% of patients deemed to have resectable disease at diagnosis of PDAC2. Prognostication and treatment planning for PDAC hinges on thorough radiological and/or histological investigation to determine the stage and therefore resectability of disease3,4; this process can be complex and is recommended to be undertaken in a multidisciplinary setting4,5. In the majority of cases of resectable PDAC there is recurrence of disease even after surgery6, contributed to by the presence of subclinical metastatic disease not detectable at diagnosis using conventional staging techniques5,7. The degree of cancer proliferation described using clinical staging frameworks (e.g. the National Comprehensive Cancer Network (NCCN) guidelines8) has traditionally provided the basis for prediction of survival and planning of treatment in the context of expected outcomes9, due to the strong association between cancer stage and survival10. However, there is a need for additional biomarkers to guide clinicians in prognostication and treatment planning, and for intervention targets to improve survival outcomes in PDAC.
The measurement of cell-free DNA containing genetic mutations of a malignancy, known as circulating tumour DNA (ctDNA), is a novel biomarker of cancer burden with promising implications for improving prognostication and monitoring of disease11. Plasma concentration of ctDNA correlates with tumour stage and volume, and fluctuations in ctDNA levels provide a rapid and precise indication of response to systemic therapy and presence of minimal residual disease after treatment12. After curative therapy, detection of ctDNA is predictive of cancer recurrence13,14, and identifies this recurrence earlier than conventional monitoring using radiological imaging15. As such, ctDNA has promising utility as a biomarker in prognostication and treatment planning for PDAC.
In the setting of cancer, skeletal muscle stores are susceptible to depletion through several molecular pathways affecting metabolic, inflammatory and immune function16,17,18,19,20, although little is known about factors that initiate and regulate severity of skeletal muscle deterioration in cancer patients18,21. Reduction in measures of height-adjusted skeletal muscle mass (skeletal muscle index, SMI), and fatty infiltration of muscle which reduces computed tomography (CT)-assessed radiodensity (skeletal muscle radiodensity, SMD22) occur in addition to potential premorbid reductions precipitated by ageing, illness or injury, malnutrition, obesity, or muscle deconditioning through inactivity or degenerative disease22,23,24,25,26,27. Suboptimal skeletal muscle stores below sex-specific thresholds are22 highly prevalent in PDAC, with low SMI and low SMD reported to be present in up to 73%28 and 55%29,30 of patients, respectively.
Low SMI and low SMD are distinct phenotypical conditions which do not always coincide, conferring additive detriments to cancer outcomes31: low SMI is an independent prognostic indicator in PDAC32 and many other cancer types, associated with decreased overall survival33,34,35,36, reduced disease-free survival and increased risk of cancer recurrence after curative treatment37,38,39,40,41. Low SMD confers risk of reduced survival and post-operative complications in PDAC and other cancers30,42,43. In light of their association to important outcomes, there is interest in the potential for skeletal muscle measures (particularly SMI) to function as an additional biomarker for risk stratification and prognostication in clinical practice, and as a target for interventions in anticipation of improved outcomes44,45,46. However, the mechanism for skeletal muscle depletion influencing cancer survival is not yet clear37,47,48, limiting understanding of the potential impact of skeletal muscle-optimising interventions.
While significant muscle wasting has been previously associated with progression through the stages of cancer cachexia as a result of advancing disease49, the advent of CT-derived skeletal muscle measurement has revealed that low SMI can occur independently of weight loss or features of the cachexia syndrome21,28,50,51,52,53,54, and is also present in patients with early stages of cancer40,55,56,57. Moreover, the poor survival outcomes associated with low SMI36 are often independent of cancer stage, affecting patients with early, potentially curable cancers, indicating that the relationship between low SMI and reduced survival may not be a simple function of advancing or terminal disease37,55. The association between presence of sub-optimal skeletal muscle stores with worse survival outcomes, while having no apparent association to cancer stage in both PDAC33,58,59,60 and other cancer types56,61,62,63,64,65,66,67 has not yet been explained. For SMI, the reporting of contradictory findings in some studies68,69,70 where reduction in SMI is in fact associated with higher clinical stage of disease, complicates the interpretation of any association between these measures. There is a need to elucidate the nature of the relationship between skeletal muscle and cancer stage, to further our understanding of whether sub-optimal skeletal muscle stores are a consequence or a comorbidity of the biological process of cancer progression. This distinction has implications for the utility of skeletal muscle measurements in cancer management and treatment, through either incorporation of these measures into prognostications along with other clinical considerations, or development of interventions to optimise skeletal muscle status with the intent to improve outcomes.
Tumour interaction with the host environment contributes to skeletal muscle depletion18, but the effect of overall tumour burden on this wasting process, including the occult presence of micrometastases has not yet been explored. Detection and quantification of ctDNA allows for a novel method of evaluating the relationship between skeletal muscle and tumour burden, to enhance understanding about the association between skeletal muscle and disease stage, and whether overt or subclinical progression of disease contributes to the occurrence or rate of skeletal muscle deterioration. Exploration of the association between ctDNA and CT-derived measures of body composition has been previously recommended, with suggestion it may be useful in guiding prognostication and expectations around response to cancer treatment71, however an analysis of this kind has not yet been reported. As high recurrence rates, poor survival, and skeletal muscle depletion are characteristic of PDAC, the aim of this study was to identify risk factors for low SMI and low SMD at diagnosis, and explore the interplay between tumour burden and skeletal muscle stores. This novel investigation will enhance understanding about the association between skeletal muscle and cancer stage, and whether burden of disease contributes to deterioration in skeletal muscle stores.
Methods
Study design and participant selection
This study was reported according to the Strengthening of the Reporting of Observational studies in Epidemiology (STROBE) guidelines72. This was an exploratory retrospective cross-sectional study approved by the Monash Health Human Research Ethics Committee (Ref: RES-17-0000387L), for analysis of available data from participants of the Victorian Pancreatic Cancer Biobank (VPCB). All participants of the VPCB had provided informed consent to collection and storage of biospecimens for the purpose of future research between January 2015 and May 2020, approved by the Monash Health Human Research Ethics Committee (HREC). Criteria for inclusion in the VPCB was a diagnosis of either PDAC (all histological types), in adults over the age of 18 years. A retrospective Waiver of Consent application was approved by the Monash Health HREC, to allow for collection of additional clinical information about VPCB participants, necessary to undertake the present study. This included height and weight data, and allowed for contact with radiological imaging providers external to Monash Health in order to obtain relevant CT imaging of participants enrolled in the VPCB for whom there was an adequate plasma sample available for detection and quantification of ctDNA (> 3 mL).
Demographic and clinical information was obtained through retrospective review of medical records to determine participant gender, age, prior surgical resection, tumour location, pathological inflammatory markers (high neutrophil to lymphocyte (NLR) ratio > 3, or low albumin < 35 g/L) and clinical stage of disease according to the 2017 National Comprehensive Cancer Network (NCCN) guidelines8.
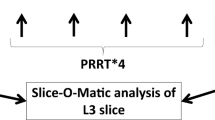
Skeletal muscle analysis
Contrast-enhanced diagnostic CT imaging undertaken as part of participants’ routine clinical care, as close as possible to the date of collection of the biobank sample, was used for skeletal muscle analysis. Single-slice axial CT images at the level of the third lumbar vertebra (L3) were imported in Digital Imaging and Communications in Medicine (DICOM) format into sliceOmatic 5.0 Rev-7 software (Tomovision, Canada) for analysis using the validated technique which has been widely reported35,73. The range of − 29 to 150 Hounsfield Units (HU) was used to segment skeletal muscle tissue, according to the Alberta Protocol74. The cross-sectional skeletal muscle area was normalised for participant height to obtain the skeletal muscle index (SMI, cm2/m2). The mean radiodensity of the cross-sectional skeletal muscle area was also recorded (skeletal muscle radiodensity, SMD). Presence of skeletal muscle abnormality was determined using thresholds published by Martin et al., which was derived from a cohort of cancer patients across all categories of body mass index (BMI) and therefore congruent with the present study35; low SMI was defined as SMI < 41cm2/m2 in females, < 43cm2/m2 in males with a BMI ≤ 24.9 kg/m2, and < 53 cm2/m2 in males with a BMI > 25 kg/m2; in both genders, low SMD was defined as < 41HU if BMI ≤ 24.9 kg/m2, and < 33HU if BMI > 25 kg/m2.
Circulating tumour DNA analysis
Samples of frozen plasma and tumour tissue taken from diagnostic biopsy or surgical resection were retrieved from the Victorian Pancreatic Cancer Biobank. Mutational status of tumour tissue samples was detected using a KRAS StripAssay (ViennaLab Diagnostics, Vienna, Austria). Samples with KRAS mutations on codons 12 and 13 were included in the analysis. ctDNA analysis was conducted using the KRAS G12/G13 Screening Kit (Bio-Rad, Hercules, CA, USA) according to the manufacturer’s recommended protocols. G12/G13 KRAS mutations were detected via droplet digital PCR (ddPCR), with inclusion of positive and negative controls, and all samples were analysed in duplicate. Detection and quantification of ctDNA was conducted using QuantaSoft software (Bio-Rad, Hercules, CA, USA), with the lower limit of detection for a positive ctDNA result set at three or more droplets75. The mutant allele fraction (MAF) represents the proportion of mutant to total allele detected.
Statistical analysis
Data were tested for normality using the Shapiro–Wilk test. Differences between groups stratified by SMI or SMD status were evaluated using independent samples t-tests or Mann–Whitney U tests for continuous variables. The chi-squared test for independence or Fishers-Exact test were used to investigate difference between groups for categorical variables. Pearson’s correlation test was used for analysis of relationships between most continuous variables; Spearman’s rank correlation was used for non-parametric data (concentration of ctDNA).
Differences in SMI, SMD, and concentration of ctDNA between clinical stages of PDAC were examined using the Kruskal–Wallis test or one-way analysis of variance. The Jonckheere–Terpstra test for ordered alternatives was used to investigate the trend of median ctDNA concentration across advancing clinical stages of PDAC. Concentration of ctDNA was median dichotomised for comparison between participants with low or undetected ctDNA vs those with higher levels of ctDNA.
Univariate logistic regression was used to determine odds ratios and 95% CIs to test for variables associated with low SMI and low SMD at diagnosis of PDAC. For this exploratory study, variables with a significance of p < 0.25 on univariate analysis were included in a multiple logistic regression model76. Analyses of differences in SMI and SMD between genders and between clinical stages was additionally conducted in a larger sample comprising participants with available data who had been initially excluded due to type of mutation or lack of plasma for ctDNA analysis, for comparison with the primary study cohort. Statistical analyses were conducted using SPSS software (Version 27). All statistical tests were two-sided, with a p value of < 0.05 indicating statistical significance.
Ethics approval and consent to participate
This research was conducted in accordance with the principles of the 1964 Declaration of Helsinki and its later amendments. All participants of the VPCB provided informed consent to collection and storage of biospecimens for the purpose of future research between January 2015 and May 2020, approved by the Monash Health HREC (Ref: 15450A). A retrospective Waiver of Consent application was approved by the Monash Health HREC (HREC/15/MonH/117), to allow for collection of additional clinical information about VPCB participants, necessary to undertake the present study.
Results
Participant selection
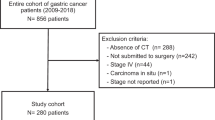
The flowchart for selection of participants is presented in Fig. 1. One-hundred-and-one participants were identified as having both pancreatic tumour tissue and plasma samples stored within the VPCB (‘the biobank’). Tissue samples for these participants were retrieved from the biobank and tested for KRAS oncogene mutations. Eighty-six samples were positive for G12/13 KRAS mutations, and 15 were either wild type or harboured Q61H mutations and were therefore excluded from the analysis. ctDNA could not be quantified for 16 participants due to insufficient plasma in the biobank sample. Participants who had commenced chemotherapy prior to CT imaging or biobank sampling (n = 3) were excluded, to remove the confounding effect of chemotherapy on both measures of skeletal muscle and concentration of ctDNA12,77. Participants who had undergone CT imaging > 60 days prior to biobank sampling (n = 1) were also excluded from the analysis. The median time difference between CT imaging and ctDNA sampling was 6 days pre-biopsy (IQR 15 days pre, to 2 days post).
Participant characteristics
Demographics and clinical characteristics of all study participants (n = 66) are presented in Table 1. The mean participant age was 68.7 (± 10.9) years, and 53% of participants were female. Most participants were diagnosed with pancreatic head and/or neck tumours, and systemic inflammation (NLR ≥ 3 or albumin < 35 g/L) was present in around half of participants at diagnosis.
Fifty-two percent of participants had unresectable tumours at diagnosis; almost a third of participants had metastatic disease. ctDNA was detected in 74% of participants (Table 1). Concentration of ctDNA was significantly different between stages of disease [H(3) = 15.307, p = 0.002], with a significant trend of increasing ctDNA concentration associated with more advanced disease at diagnosis defined by NCCN clinical stage (J = 1103.5, z = 3.737, p < 0.001, r = 0.46) (Fig. 2). There was no correlation between concentration of ctDNA and age (r = 0.090, p = 0.470) or BMI (r = − 0.107, p = 0.393).
Factors associated with skeletal muscle stores at diagnosis of pancreatic ductal adenocarcinoma.
Skeletal muscle index
The prevalence of low SMI was 69.7% for the whole group. Females had a lower mean SMI than males (p < 0.001), and a significantly higher prevalence of low SMI than males (85.7% vs. 53.3%, p = 0.006) (Table 1). There was a weak, negative correlation between SMI and age (r = − 0.245, p = 0.047), but no significant correlation with BMI (r = − 0.191, p = 0.125). There was no statistical difference in SMI between clinical stages of PDAC at diagnosis (F(3, 62) = 0.886, p = 0.453) (Fig. 3a), and no significant linear correlation between concentration of ctDNA and SMI (r = − 0.163, p = 0.192). In a multiple regression analysis, female gender was independently associated with higher odds of having low SMI, after controlling for increasing age and high NLR (Table 2).
Boxplots of participants’ skeletal muscle stores grouped by clinical stage at diagnosis of pancreatic ductal adenocarcinoma (PDAC), n = 66. Reference lines show thresholds for low SMI/SMD according to Martin et al.35. (a) Skeletal muscle index (SMI), no difference between clinical stages; (1) males with BMI ≥ 25 kg/m2; (2) males with BMI < 25 kg/m2; (3) females (all). (b) Skeletal muscle radiodensity (SMD), no difference between clinical stages; (1) BMI < 25 kg/m2; (2) BMI ≥ 25 kg/m2; HU Hounsfield Units.
A comparative analysis was conducted in a larger sample of participants (n = 89) which included 23 additional participants who were previously excluded due to type of mutation or lack of plasma for ctDNA analysis [48% female, mean age 69.0 (± 10.8) years]. As observed in the smaller primary cohort (n = 66), low SMI was more highly prevalent in females (84% vs 54%, p = 0.006) and there was no difference in SMI between clinical stages of PDAC at diagnosis (F(3, 85) = 0.580, p = 0.630, n = 89).
Skeletal muscle radiodensity
Low SMD was present in 62.1% of participants, with no gender differences in prevalence (Table 1). There was a moderate, negative correlation between SMD and age (r = − 0.415, p < 0.001) and BMI (r = − 0.491, p < 0.001). There was no statistical difference in SMD between clinical stages of PDAC at diagnosis (F(3, 62) = 0.717, p = 0.545), and no significant linear correlation between concentration of ctDNA and SMD (r = 0.097, p = 0.438). In a multivariable analysis, increasing age remained independently associated with increased odds of having low SMD after controlling for unresectable disease, BMI, high NLR, and concentration of ctDNA (Table 3). In the comparative analysis using a larger cohort (n = 89), similar results were observed: there was no difference in prevalence of low SMD between genders (male 50%, female 65%, p = 0.220), and no difference in SMD between clinical stages of PDAC at diagnosis (F(3, 85) = 1.314, p = 0.275).
Discussion
This study aimed to explore the association between skeletal muscle stores and tumour burden (using ctDNA as a novel biomarker as well as traditional clinical staging) at diagnosis of PDAC. Skeletal muscle abnormalities were found to be highly prevalent at diagnosis of PDAC in this cohort (low SMI 69.7%, low SMD 62.1%). Presence of low SMI or low SMD was not associated with clinical stages of PDAC, and neither presence nor concentration of ctDNA was associated with increased likelihood of having low SMI or SMD at diagnosis of PDAC. Instead, female gender was the strongest predictor of low SMI, and increasing age was associated with low SMD. These findings suggest that the deterioration of skeletal muscles stores in people diagnosed with PDAC may occur early in the disease process, and are not simply a direct result of advancing clinical stage or increasing tumour burden.
To better understand the association between tumour burden and skeletal muscle status we studied circulating tumour DNA, which is a more sensitive marker of cancer progression than standard clinical staging measures15. The analysis of this relationship is novel, and has not been conducted in any cancer type. In this exploratory study, concentration of ctDNA increased with progressively higher clinical stage of disease as expected78,79, but there was no association between detection or concentration of ctDNA, with SMI or SMD measures in this cohort of patients with PDAC. The significant increase in ctDNA concentration with higher cancer stage, while having no association to skeletal muscle measures, supports the findings from other studies that there is no clear association between sub-optimal skeletal muscle stores and clinical stage of disease57,59.
As low skeletal muscle stores are prevalent comorbidities of PDAC, it is important to understand the factors that are associated with their presence to enable identification and intervention. Nearly three in four participants had low SMI at diagnosis, which is consistent with other reports28,53. The lack of difference in BMI between participants with low or normal SMI reinforces the notion that basic anthropometric methods cannot be relied upon to distinguish those at risk of skeletal muscle depletion, which can occur independent of change in body weight53,80,81. Presence of low SMI was strongly associated with female gender in this study, but this remains contentious in the PDAC literature where most analyses are univariate; some studies report a similar finding82,83, however in other studies no gender differences are seen42,84. Classification of gender as a risk factor for low SMI has potential importance in screening of PDAC patients to identify those most vulnerable to skeletal muscle depletion, but there is a dearth of multivariate investigations of factors influencing SMI in PDAC patients. In the single study where factors influencing SMI prior to resection of PDAC have been investigated using multivariate regression analysis (n = 273), the association with female gender aligned with our findings53. Future multivariate analyses in larger cohorts are needed to confirm our finding that female gender is a risk factor for low SMI in PDAC.
Low SMD is more prevalent in PDAC than most other cancers, though the reason for this is not known85. In our study, low SMD was identified in 62% of participants which is a higher prevalence than has been previously reported29,30,85,86. Increasing age was associated with higher likelihood of having low SMD in our cohort, which aligns with results of studies in other cancer types21,51; to our knowledge, this is the first study to explore risk factors for low SMD in PDAC patients. Ageing is both a risk factor for development of cancer87 and associated with the characteristics of obesity, diabetes and inactivity which are also linked to reduction in SMD22,23, which may explain this association. Low SMD has also been associated with the presence of inflammatory markers such as high NLR or low albumin level21, however the evidence-base is limited. This association was not demonstrated in the present study but this may be attributed to the small sample size. Similar to SMI, there are several studies reporting a lack of association between low SMD and clinical stage of disease42,56,67, indicating that low SMD is a comorbidity of cancer with a potentially complex aetiology involving demographic, phenotypic, and lifestyle characteristics22. While the aetiology of intramuscular lipid accumulation resulting in reduced skeletal muscle radiodensity in the cancer population is poorly understood, it has been identified that both history of cigarette smoking and presence of comorbidities such as diabetes are associated with low SMD21,88. These characteristics are also risk factors for developing PDAC89, which may explain why prevalence of low SMD in PDAC is high.
The focus on a single cancer type, with participants studied prior to commencement of treatment, is a strength of this study. Additionally, a single, trained investigator conducted all CT-derived skeletal muscle analyses and as a result, the main between-participant differences in variables included in the analysis were natural variations in stage or location of disease, and phenotypical characteristics such as age and BMI. Limitations of this exploratory study are its small sample size and convenience sampling approach which is acknowledged to affect the generalisability of results. Moreover, the retrospective design precluded statistical adjustment for factors known to have an association with SMI or SMD such as nutrition status and/or weight loss history46, presence of comorbidities88, smoking history21, strength or physical activity level90,91, or impairment of digestion due to pancreatic enzyme insufficiency92. These factors should be incorporated into future prospective study designs with larger sample sizes to enhance external validity.
The findings of the present study suggest that low SMI and low SMD are comorbidities of PDAC. Our data suggest that women with PDAC are more likely to have low SMI, and those with older age more likely to have low SMD at diagnosis of PDAC. Screening is needed to identify sub-optimal skeletal muscle status in people with PDAC who are at greatest risk of poor outcomes, because it is not easily identified by indices such as BMI. Future research is required to further elucidate potential mechanisms and risk factors for low SMI and low SMD at diagnosis of PDAC; the lack of association between ctDNA, a novel, sensitive marker of disease burden, and SMI or SMD, suggests that sub-optimal skeletal muscle conditions are not simply a function of advancing cancer stage. Assessment of skeletal muscle stores in clinical practice therefore has utility beyond prognostication, and therapy for people with PDAC should also consider interventions aimed at improving muscle status alongside treatment for the underlying disease.
Data availability
The ethical approval obtained to conduct this study does not extend to sharing of data, therefore the data supporting the findings of this study are not openly available. De-identified data may be shared upon reasonable request to the corresponding author if proposed research has undergone ethical review.
References
Australian Institute of Health and Welfare. Cancer Data in Australia. (Australian Institute of Health and Welfare, 2022). https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia. Accessed 21 Aug 2021.
Kamisawa, T., Wood, L. D., Itoi, T. & Takaori, K. Pancreatic cancer. Lancet 388(10039), 73–85 (2016).
Cooper, A. B., Tzeng, C.-W.D. & Katz, M. H. G. Treatment of borderline resectable pancreatic cancer. Curr. Treat. Options Oncol. 14(3), 293–310 (2013).
Rhee, H. & Park, M. S. The Role of Imaging in Current Treatment Strategies for Pancreatic Adenocarcinoma. Korean J. Radiol. 22(1), 23–40 (2021).
Chawla, A. & Aguirre, A. J. Staging classification and stratification of pancreatic cancer for clinical practice. Clin. Pancreatol. Pract. Gastroenterol. Surg. 2, 433–442. https://doi.org/10.1002/9781119570097.ch54 (2021).
Oettle, H. et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: The CONKO-001 randomized trial. JAMA 310(14), 1473–1481 (2013).
Hidalgo, M. et al. Addressing the challenges of pancreatic cancer: Future directions for improving outcomes. Pancreatology 15(1), 8–18 (2015).
Tempero, M. A. et al. Pancreatic adenocarcinoma, version 2.2017, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Canc. Netw. 15(8), 1028–1061 (2017).
Ludwig, J. A. & Weinstein, J. N. Biomarkers in cancer staging, prognosis and treatment selection. Nat Rev Cancer. 5(11), 845–856 (2005).
Sirri, E. et al. Recent trends in survival of patients with pancreatic cancer in Germany and the United States. Pancreas 45(6), 908–914 (2016).
De Rubis, G., Krishnan, S. R. & Bebawy, M. Circulating tumor DNA: Current state of play and future perspectives. Pharmacol. Res. 136, 35–44 (2018).
Reece, M. et al. The use of circulating tumor DNA to monitor and predict response to treatment in colorectal cancer. Front. Genet. 10, 1118 (2019).
Tie, J. et al. Circulating tumor DNA analysis detects minimal residual disease and predicts recurrence in patients with stage II colon cancer. Sci. Transl. Med. 8(346), 346–392 (2016).
Osumi, H., Shinozaki, E., Yamaguchi, K. & Zembutsu, H. Clinical utility of circulating tumor DNA for colorectal cancer. Cancer Sci. 110(4), 1148–1155 (2019).
Dawson, S.-J. et al. Analysis of circulating tumor DNA to monitor metastatic breast cancer. N. Engl. J. Med. 368(13), 1199–1209 (2013).
Argilés, J. M., Busquets, S., Stemmler, B. & López-Soriano, F. J. Cancer cachexia: understanding the molecular basis. Nat. Rev. Cancer. 14(11), 754–762 (2014).
Jones, K., Gordon-Weeks, A., Coleman, C. & Silva, M. Radiologically determined sarcopenia predicts morbidity and mortality following abdominal surgery: A systematic review and meta-analysis. World J. Surg. 41(9), 2266–2279 (2017).
Biswas, A. K. & Acharyya, S. Cancer-associated cachexia: A systemic consequence of cancer progression. Annu. Rev. Cancer Biol. 4(1), 391–411 (2020).
Argilés, J. M., Stemmler, B., López-Soriano, F. J. & Busquets, S. Inter-tissue communication in cancer cachexia. Nat. Rev. Endocrinol. 15(1), 9–20 (2018).
Porporato, P. E. Understanding cachexia as a cancer metabolism syndrome. Oncogenesis. 5, e200 (2016).
Xiao, J. et al. The association of medical and demographic characteristics with sarcopenia and low muscle radiodensity in patients with nonmetastatic colorectal cancer. Am. J. Clin. Nutr. 109(3), 615–625 (2019).
Aubrey, J. et al. Measurement of skeletal muscle radiation attenuation and basis of its biological variation. Acta Physiol. 210(3), 489–497 (2014).
Marcus, R. L., Addison, O., Kidde, J. P., Dibble, L. E. & Lastayo, P. C. Skeletal muscle fat infiltration: impact of age, inactivity, and exercise. J. Nutr. Health Aging. 14(5), 362–366 (2010).
Bhullar, A. S. et al. Lipid is heterogeneously distributed in muscle and associates with low radiodensity in cancer patients. J. Cachexia Sarcopenia Muscle. 11(3), 735–747 (2020).
Grimby, G. & Saltin, B. The ageing muscle. Clin. Physiol. 3(3), 209–218 (1983).
Argilés, J. M., Campos, N., Lopez-Pedrosa, J. M., Rueda, R. & Rodriguez-Mañas, L. Skeletal muscle regulates metabolism via interorgan crosstalk: Roles in health and disease. J. Am. Med. Dir. Assoc. 17(9), 789–796 (2016).
Demling, R. H. Nutrition, anabolism, and the wound healing process: An overview. Eplasty 9, e9 (2009).
Basile, D. et al. The IMPACT study: Early loss of skeletal muscle mass in advanced pancreatic cancer patients. J. Cachexia Sarcopenia Muscle. 10(2), 368–377 (2019).
Rollins, K. E. et al. The impact of sarcopenia and myosteatosis on outcomes of unresectable pancreatic cancer or distal cholangiocarcinoma. Clin. Nutr. 35(5), 1103–1109 (2016).
van Dijk, D. P. J. et al. Low skeletal muscle radiation attenuation and visceral adiposity are associated with overall survival and surgical site infections in patients with pancreatic cancer. J. Cachexia Sarcopenia Muscle. 8(2), 317–326 (2017).
Stretch, C. et al. Sarcopenia and myosteatosis are accompanied by distinct biological profiles in patients with pancreatic and periampullary adenocarcinomas. PLoS ONE 13(5), e0196235 (2018).
Mintziras, I. et al. Sarcopenia and sarcopenic obesity are significantly associated with poorer overall survival in patients with pancreatic cancer: Systematic review and meta-analysis. Int. J. Surg. 59, 19–26 (2018).
Choi, M. H. et al. Preoperative sarcopenia and post-operative accelerated muscle loss negatively impact survival after resection of pancreatic cancer. J. Cachexia Sarcopenia Muscle. 9(2), 326–334 (2018).
Deng, H.-Y. et al. Preoperative sarcopenia is a predictor of poor prognosis of esophageal cancer after esophagectomy: A comprehensive systematic review and meta-analysis. Dis. Esophagus. 32(3), 115 (2018).
Martin, L. et al. Cancer cachexia in the age of obesity: Skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J. Clin. Oncol. 31(12), 1539–1547 (2013).
Shachar, S. S., Williams, G. R., Muss, H. B. & Nishijima, T. F. Prognostic value of sarcopenia in adults with solid tumours: A meta-analysis and systematic review. Eur. J. Cancer. 57, 58–67 (2016).
Chang, K. V. et al. Association between loss of skeletal muscle mass and mortality and tumor recurrence in hepatocellular carcinoma: A systematic review and meta-analysis. Liver Cancer. 7(1), 90–103 (2018).
Zhang, G., Meng, S., Li, R., Ye, J. & Zhao, L. Clinical significance of sarcopenia in the treatment of patients with primary hepatic malignancies, a systematic review and meta-analysis. Oncotarget 8(60), 102474–102485 (2017).
Tsukioka, T. et al. Loss of muscle mass is a novel predictor of postoperative early recurrence in N2-positive non-small-cell lung cancer. Ann. Thorac. Cardiovasc. Surg. 24(3), 121 (2018).
Hopkins, J. J. et al. The impact of muscle and adipose tissue on long-term survival in patients with stage I to III colorectal cancer. Dis. Colon Rectum. 62(5), 549–560 (2019).
Hua, X. et al. When the loss costs too much: A systematic review and meta-analysis of sarcopenia in head and neck cancer. Front. Oncol. 9, 1561 (2020).
Okumura, S. et al. Impact of preoperative quality as well as quantity of skeletal muscle on survival after resection of pancreatic cancer. Surgery. 157(6), 1088–1098 (2015).
Carvalho, A. L. M. et al. Low skeletal muscle radiodensity is the best predictor for short-term major surgical complications in gastrointestinal surgical cancer: A cohort study. PLoS ONE 16(2), e0247322 (2021).
Abbass, T., Dolan, R. D. & McMillan, D. C. Computed tomography-derived body composition analysis in patients with advanced cancer: Clinical utility and future research. Curr. Opin. Support Palliat Care. 14(4), 309–315 (2020).
Hilmi, M. et al. Body composition and sarcopenia: The next-generation of personalized oncology and pharmacology?. Pharmacol. Ther. 196, 135–159 (2019).
Prado, C. M., Purcell, S. A. & Laviano, A. Nutrition interventions to treat low muscle mass in cancer. J. Cachexia Sarcopenia Muscle. 11(2), 366–380 (2020).
Zhu, Y., Guo, X., Zhang, Q. & Yang, Y. Prognostic value of sarcopenia in patients with rectal cancer: A meta-analysis. PLoS ONE 17(6), e0270332 (2022).
Ahn, H. et al. Updated systematic review and meta-analysis on diagnostic issues and the prognostic impact of myosteatosis: A new paradigm beyond sarcopenia. Ageing Res. Rev. 70, 101398 (2021).
Fearon, K. et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 12(5), 489–495 (2011).
Zhang, F.-M. et al. Development and validation of nomograms for the prediction of low muscle mass and radiodensity in gastric cancer patients. Am. J. Clin. Nutr. 113(2), 348–358 (2020).
Malietzis, G. et al. Low muscularity and myosteatosis is related to the host systemic inflammatory response in patients undergoing surgery for colorectal cancer. Ann. Surg. 263(2), 320–325 (2016).
Weinberg, M. S. et al. Beyond sarcopenia: Characterization and integration of skeletal muscle quantity and radiodensity in a curable breast cancer population. Breast J. 24(3), 278–284 (2018).
Carrara, G. et al. Preoperative sarcopenia determinants in pancreatic cancer patients. Clin. Nutr. 36(6), 1649–1653 (2017).
Okugawa, Y. et al. Close relationship between immunological/inflammatory markers and myopenia and myosteatosis in patients with colorectal cancer: A propensity score matching analysis. JPEN J. Parenter. Enteral. Nutr. 43(4), 508–515 (2019).
Caan, B. J. et al. Association of muscle and adiposity measured by computed tomography with survival in patients with nonmetastatic breast cancer. JAMA Oncol. 4(6), 798–804 (2018).
McSorley, S. T., Black, D. H., Horgan, P. G. & McMillan, D. C. The relationship between tumour stage, systemic inflammation, body composition and survival in patients with colorectal cancer. Clin. Nutr. 37(4), 1279–1285 (2018).
Shirdel, M. et al. Body composition measured by computed tomography is associated with colorectal cancer survival, also in early-stage disease. Acta Oncol. 59(7), 799–808 (2020).
Di Sebastiano, K. M. et al. Accelerated muscle and adipose tissue loss may predict survival in pancreatic cancer patients: The relationship with diabetes and anaemia. Br. J. Nutr. 109(2), 302–312 (2013).
Ninomiya, G. et al. Clinical impact of sarcopenia on prognosis in pancreatic ductal adenocarcinoma: A retrospective cohort study. Int. J. Surg. 39, 45–51 (2017).
Okumura, S. et al. Visceral adiposity and sarcopenic visceral obesity are associated with poor prognosis after resection of pancreatic cancer. Ann. Surg. Oncol. 24(12), 3732–3740 (2017).
Fujiwara, N. et al. Sarcopenia, intramuscular fat deposition, and visceral adiposity independently predict the outcomes of hepatocellular carcinoma. J. Hepatol. 63(1), 131–140 (2015).
Richards, C. H. et al. The relationships between body composition and the systemic inflammatory response in patients with primary operable colorectal cancer (body composition in colorectal cancer). PLoS ONE 7(8), e41883 (2012).
Harimoto, N. et al. Sarcopenia as a predictor of prognosis in patients following hepatectomy for hepatocellular carcinoma. Br. J. Surg. 100(11), 1523–1530 (2013).
Miyamoto, Y. et al. Sarcopenia is a negative prognostic factor after curative resection of colorectal cancer. Ann. Surg. Oncol. 22(8), 2663–2668 (2015).
Harada, K. et al. Prognostic and clinical impact of sarcopenia in esophageal squamous cell carcinoma. Dis. Esophagus. 29(6), 627–633 (2016).
Nakanishi, R. et al. Sarcopenia is an independent predictor of complications after colorectal cancer surgery. Surg. Today. 48(2), 151–157 (2018).
Dolan, R. D. et al. The relationship between computed tomography-derived body composition, systemic inflammatory response, and survival in patients undergoing surgery for colorectal cancer. J. Cachexia Sarcopenia Muscle. 10(1), 111–122 (2019).
Sakurai, K. et al. Adverse effects of low preoperative skeletal muscle mass in patients undergoing gastrectomy for gastric cancer. Ann. Surg. Oncol. 24(9), 2712–2719 (2017).
Caan, B. J. et al. Explaining the obesity paradox: The association between body composition and colorectal cancer survival (C-scans study). Cancer Epidemiol. Biomark. Prev. 26(7), 1008 (2017).
Takagi, K. et al. Sarcopenia and American society of anesthesiologists physical status in the assessment of outcomes of hepatocellular carcinoma patients undergoing hepatectomy. Acta Med. Okayama. 70(5), 363–370 (2016).
van Seventer, E. E., Fintelmann, F. J., Roeland, E. J. & Nipp, R. D. Leveraging the potential synergy between patient-reported outcomes and body composition analysis in patients with cancer. Oncologist. 25(4), 271–273 (2020).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 61(4), 344–349 (2008).
Mourtzakis, M. et al. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl. Physiol. Nutr. Metab. 33(5), 997–1006 (2008).
TomoVision. Alberta Protocol: User's Manual. (2017). https://tomovision.com/Sarcopenia_Help/index.htm.
Basu, A. S. Digital assays part I: Partitioning statistics and digital PCR. SLAS Technol. 22(4), 369–386 (2017).
Hosmer, D. W. & Lemeshow, S. Applied Logistic Regression 2nd edn. (Wiley, 2000).
Daly, L. E. et al. Loss of skeletal muscle during systemic chemotherapy is prognostic of poor survival in patients with foregut cancer. J. Cachexia Sarcopenia Muscle. 9(2), 315–325 (2018).
Bettegowda, C. et al. Detection of circulating tumor DNA in early-and late-stage human malignancies. Sci. Transl. Med. 6(224), 224 (2014).
Sellahewa, R., Lundy, J., Croagh, D. & Jenkins, B. High circulating tumour DNA is a strong negative prognostic factor in operable pancreatic cancer. HPB 23, S263 (2021).
Martin, L., Gioulbasanis, I., Senesse, P. & Baracos, V. E. Cancer-associated malnutrition and CT-defined sarcopenia and myosteatosis are endemic in overweight and obese patients. J. Parenter. Enter. Nutr. 44(2), 227–238 (2020).
Brown, J. C. et al. Weight stability masks changes in body composition in colorectal cancer: A retrospective cohort study. Am. J. Clin. Nutr. 113(6), 1482–1489 (2021).
Jalal, M., Campbell, J. A., Wadsley, J. & Hopper, A. D. Computed tomographic sarcopenia in pancreatic cancer: Further utilization to plan patient management. J. Gastrointest. Cancer. 2021, 1–5 (2021).
Uemura, S. et al. The impact of sarcopenia and decrease in skeletal muscle mass in patients with advanced pancreatic cancer during FOLFIRINOX therapy. Br. J. Nutr. 125(10), 1140–1147 (2021).
Sui, K. et al. Correlation between the skeletal muscle index and surgical outcomes of pancreaticoduodenectomy. Surg. Today. 48(5), 545–551 (2018).
Armstrong, V. et al. Characterizing cancer-associated myosteatosis: Anatomic distribution and cancer-specific variability of low radiodensity muscle. JCSM Rapid Commun. 4(2), 197–206 (2021).
Griffin, O. M. et al. Characterising the impact of body composition change during neoadjuvant chemotherapy for pancreatic cancer. Pancreatology 19(6), 850–857 (2019).
US Cancer Statistics Working Group. United States Cancer Statistics: 1999–2009 Incidence and Mortality Web-Based Report. (US Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute, 2013).
Xiao, J. et al. Associations of pre-existing co-morbidities with skeletal muscle mass and radiodensity in patients with non-metastatic colorectal cancer. J. Cachexia Sarcopenia Muscle. 9(4), 654–663 (2018).
Rawla, P., Sunkara, T. & Gaduputi, V. Epidemiology of pancreatic cancer: Global trends, etiology and risk factors. World J. Oncol. 10(1), 10–27 (2019).
Goodpaster, B. H. et al. The loss of skeletal muscle strength, mass, and quality in older adults: The health, aging and body composition study. J. Gerontol. A. 61(10), 1059–1064 (2006).
Hughes, V. A. et al. Longitudinal muscle strength changes in older adults: Influence of muscle mass, physical activity, and health. J. Gerontol. A. 56(5), B209–B217 (2001).
Shintakuya, R. et al. Sarcopenia is closely associated with pancreatic exocrine insufficiency in patients with pancreatic disease. Pancreatology 17(1), 70–75 (2017).
Funding
This research was supported by an Australian Government Research Training Program scholarship, and a Monash University Postgraduate Publications Award, to LH. This work was also supported by a Monash Partners Comprehensive Cancer Consortium (MPCCC) Research Grant, a Victorian Cancer Agency Research Grant [Grant Number HSR15007 to CEH] and a National Health and Medical Research Council (NHMRC) Translating Research Into Practice (TRIP) Fellowship [Grant Number GNT1168483 to CEH].
Author information
Authors and Affiliations
Contributions
L.H. was responsible for collection and assembly of skeletal muscle assessment data, data analysis and interpretation, and drafting of the manuscript. R.S. was responsible for collection and assembly of participant sample, and conducted the circulating tumour DNA analysis; C.E.H. contributed significantly to study conception/design, data analysis and interpretation, and manuscript writing; J.L. assisted with provision of study materials and collection and assembly of data; D.C. was responsible for study conception/design, assisted with data analysis and interpretation, and provision of study materials and patients. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hanna, L., Sellahewa, R., Huggins, C.E. et al. Relationship between circulating tumour DNA and skeletal muscle stores at diagnosis of pancreatic ductal adenocarcinoma: a cross-sectional study. Sci Rep 13, 9663 (2023). https://doi.org/10.1038/s41598-023-36643-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-36643-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.