Abstract
Supraglottic airway (SGA) may have advantages over endotracheal tube (ETT) regarding laryngospasm, coughing, sore throat, and hemodynamic changes; however, studies on the use of SGA in laparoscopic donor nephrectomy (LDN) are lacking. Here, we aimed to confirm the safety and feasibility of second-generation SGA in LDN and compare them with those of ETT. Enrolled adult donors (aged > 18 years) who underwent LDN between August 2018 and November 2021 were divided into two groups—ETT vs. SGA. Airway pressure, lung compliance, desaturation, and hypercapnia were recorded during surgery. After propensity score matching for baseline characteristics and surgical duration, 82 and 152 donors were included in the ETT and SGA groups, respectively, and their outcomes were compared. The peak airway pressure was lower in the SGA group than in the ETT group 5 min after pneumoperitoneum. Dynamic lung compliance was higher in the SGA group than in the ETT group during surgery. There were no cases of intraoperative desaturation, hypercapnia, or postoperative aspiration pneumonitis. The use of second-generation SGA, a safe alternative to ETT for LDN, resulted in reduced airway resistance and increased lung compliance, which suggests its benefits for airway management in kidney donors.
Similar content being viewed by others
Introduction
Although endotracheal intubation is the gold standard for maintaining the airway under general anesthesia, it can induce physiological stress responses. The use of supraglottic airway (SGA) is known to reduce the incidence of laryngospasm, coughing, sore throat, and hemodynamic changes compared to that of endotracheal tube (ETT)1,2. Because of these advantages, the use of SGA has gradually increased. However, the risk of inadequate ventilation and pulmonary aspiration remains a major concern associated with the use of SGA2.
As living kidney donors have no physical benefit from donation, living-donor nephrectomy aims to enhance donor recovery with safe organ acquisition3. As one of the enhanced recovery protocols for donors, the laparoscopic approach is favored over the open approach because it involves reduced postoperative pain and shorter hospital stay and helps the donors resume normal activities quickly4,5. SGA has advantages in terms of enhanced donor recovery because it can reduce stress responses compared to ETT. However, the use of SGA has been limited in laparoscopic donor nephrectomy (LDN) because of concerns regarding inadequate ventilation and gastric regurgitation in the lateral position and pneumoperitoneum. Although many studies have demonstrated that SGA is safe to use in laparoscopic surgeries6,7,8,9,10, they were mostly conducted under supine position, and the safety of SGA in lateral position under laparoscopy, a potentially unfavorable condition for SGA, still remains in question.
The design of SGA has been modified to achieve tight airway sealing and reduce gastric distension. The second-generation SGA provides higher sealing pressure than classical SGA and reduces the risk of aspiration by occluding the esophagus through SGA tip and providing gastric drainage channel10. In addition, some second-generation SGAs are known to reduce accidental rotation and displacement using buccal cavity stabilizer11. However, there is a lack of studies on the use of SGA in LDN. In our institute, second-generation SGA has been used in LDN since 2018. The aim of this study was to confirm the safety and feasibility of second-generation SGA in LDN and compare them with those of ETT.
Methods
Study design and population
This single-center retrospective study was approved by the Institutional Review Board of the Samsung Medical Center (2021-04-142). The Institutional Review Board of Samsung Medical Center waived the requirement for informed consent due to retrospective design of the study, and the study was conducted in accordance with the Declaration of Helsinki. Adult donors (> 18 years old) who underwent LDN between August 2018 and November 2021 were enrolled. Exclusion criteria were conversion to open surgery, violation of the anesthetic protocol, and failure of SGA insertion. Donors were divided into the ETT and SGA groups. Donor information was retrieved from electronic medical records.
Study protocol
Anesthesia was induced with thiopental sodium (5 mg/kg) or propofol (2 mg/kg), vecuronium (0.1 mg/kg), and sevoflurane and maintained with desflurane. Neuromuscular blockade was monitored by Train-of-Four measurement with EZstim II (Life-Tech, Texas, the United States), and continuous vecuronium or rocuronium infusion was administered according to the attending anesthesiologist. The protocol for inducing anesthesia remained the same throughout the study period. Routine monitoring devices such as pulse oximetry, electrocardiography, and noninvasive blood pressure monitoring were used. Endotracheal intubation was performed with an internal diameter of 8.0 mm for male donors and 7.0 mm for female donors. The second-generation SGA, LMA Protector™ (Teleflex Medical Europe, Westmeath, Ireland) was chosen according to the manufacturer’s recommendations. The LMA Protector™ has two ports that serve for insertion of the gastric tube and suction of the laryngeal region. After SGA insertion, a 14 Fr gastric tube was inserted through the female port of the SGA. Mechanical ventilation using a 0.5 fraction of inspired oxygen at a fresh gas flow rate of 2 L/min was set with 5 to 6 cmH2O positive end-expiratory pressure (PEEP) and a tidal volume (TV) of 8 mL/kg of ideal body weight12. Respiratory rate was adjusted to maintain normocapnia. During pneumoperitoneum, the intra-abdominal carbon dioxide (CO2) pressure was adjusted to 12 mmHg.
Data collection
Information about donor characteristics including age, sex, height, body weight, body mass index, American Society of Anesthesiologist physical status classification, and durations of anesthesia, surgery, and pneumoperitoneum was collected. The peak airway pressure (Ppeak), plateau airway pressure (Pplat), PEEP, set TV (TVset), actual TV (TVact), pulse oximetry saturation (SpO2), end-tidal CO2 (EtCO2), and respiratory rate were recorded at five time points: after induction, after lateral position, 5 min after pneumoperitoneum, 5 min after pneumoperitoneum removal, and at the end of surgery. Dynamic compliance (Cdyn) and static compliance (Cstat) were calculated using Eqs. (1) and (2), respectively:
In the SGA group, the leakage fraction was calculated using Eq. (3):
If TVact was greater than TVset, the leakage fraction was regarded as zero. Data on the duration of postoperative care unit (PACU) stay, hospital stay, and postoperative pulmonary complications during hospital stay were collected.
Statistical analysis
The primary outcomes were respiratory mechanics, including airway pressure and lung compliance. The secondary outcomes were the incidence of desaturation (SpO2 < 97%) and suboptimal ventilation (EtCO2 > 45 mmHg), leakage fraction in the SGA group, and incidence of postoperative pulmonary complications. To reduce the influence of potential confounding factors of baseline characteristics and surgical duration, propensity score matching was performed with nearest-neighbor matching without replacement. Each donor in the ETT group was matched to two donors in the SGA group (1:2 matching). The matching factors were age, sex, height, body weight, body mass index, anesthesia time, surgical time, and pneumoperitoneum time. Caliper size was defined as the 0.25 standard deviation of the logit of the propensity score13. Successful matching was determined using an absolute standardized difference < 0.2.
Continuous variables were expressed as mean ± standard deviation, and categorical variables as numbers and percentages. Continuous variables were compared using Student’s t-test, and categorical variables were compared using Fisher’s exact test or the chi-square test. Repeatedly measured variables were analyzed using the two-way mixed ANOVA test. When intergroup differences were statistically significant, post-hoc analyses were performed using the independent t-test for two samples, and the P-value was adjusted with Bonferroni correction for multiple comparisons. All statistical analyses were performed using IBM SPSS Statistics for Windows, version 25.0, (IBM Corporation, Armonk, NY, USA) or R software version 4.0.5. P < 0.05 was considered statistically significant.
Results
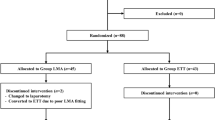
Between August 2018 and November 2021, 365 donors underwent LDN. Of these, 67 donors in the ETT group were excluded because of inadequate PEEP (0–4 mmHg). Failure of SGA insertion occurred in six donors who were excluded from the analysis. Finally, 292 donors were included in the analysis. After propensity score matching, 82 and 152 donors were included in the ETT and SGA groups, respectively (Fig. 1). The change in SGA size occurred in three donors in the SGA group. Failure of gastric tube insertion occurred in one donor in the SGA group.
Comparisons of preoperative and intraoperative variables before and after matching between the two groups are shown in Table 1. Before matching, anesthesia time and surgery time were unbalanced between the two groups, as demonstrated by the absolute standardized difference of > 0.2. After matching, heterogeneity was reduced, and all variables were within an absolute standardized difference of < 0.2.
Airway pressure and lung compliance after matching are shown in Fig. 2. Ppeak and Pplat showed significant intergroup differences over time (Pgroup*time = 0.027 and < 0.001, respectively). Ppeak was consistently higher in the ETT group than in the SGA group over time and statistically significant 5 min after pneumoperitoneum (P = 0.030). Pplat did not show consistent trends between the two groups over time but was significantly higher in the SGA group than in the ETT group after lateral positioning (P = 0.030). Cdyn showed intergroup differences over time (Pgroup×time = 0.014) and was significantly higher in the SGA group than in the ETT group at all time points (all P-values < 0.05). Cstat did not show any significant intergroup differences (Pgroup×time = 0.171).
None of the donors showed desaturation during the surgery (SpO2 ≥ 97%). The EtCO2 was within the optimal ventilation range (≤ 45 mmHg) during surgery, except in one donor in the ETT group (EtCO2 47 mmHg at 5 min after pneumoperitoneum).
The leakage fraction was investigated in all donors in the SGA group before matching (n = 205). The mean leakage fraction showed a range of 6–8% during surgery and the lateral position and pneumoperitoneum did not significantly influence the leakage fraction (after induction vs. after lateral position: P = 0.094; after induction vs. 5 min after pneumoperitoneum: P = 0.094; after lateral position vs. 5 min after pneumoperitoneum: P > 0.999). The duration of PACU stay was comparable between ETT (59 ± 11 min) and SGA (58 ± 12 min, P = 0.839) groups; hospital stays were also comparable between two groups after matching (9.0 ± 3.1 days vs. 9.0 ± 1.7 days, P = 0.868, respectively). None of the donors showed clinically significant postoperative pulmonary complications.
Discussion
This study showed that the use of SGA during LDN was favorable in terms of respiratory mechanics based on the reduction in Ppeak and increase in Cdyn compared to those achieved with the use of ETT. No cases of intraoperative desaturation (SpO2 < 97%) or hypercapnia (EtCO2 > 45 mmHg) were observed in the SGA group, suggesting adequate oxygenation and ventilation. Lateral position and pneumoperitoneum did not significantly influence the leakage fraction in the SGA group. There were no cases of postoperative pulmonary complications, particularly aspiration pneumonitis.
LDN requires simultaneous lateral positioning and pneumoperitoneum; hence, the procedure is often considered suboptimal for SGA use. Although several studies have reported the safe use of SGA in the lateral position14 and pneumoperitoneum6,7, there are only few studies on the combined effect of the lateral position and pneumoperitoneum. Rustagi et al. investigated the feasibility of LMA Proseal™, another second-generation SGA, in laparoscopic urological procedures in 25 patients15. They found that the mean oropharyngeal sealing pressure was always above the mean Ppeak even in the lateral position with pneumoperitoneum. Lan et al. compared oropharyngeal sealing pressure in two different second-generation SGA (LMA Proseal™ and LMA Supreme™) in the lateral position with pneumoperitoneum and concluded that ventilation was adequate in both SGA types16. Our study adds to the investigation of feasibility of second-generation SGA use in the lateral position with pneumoperitoneum through analyses of respiratory mechanics and leakage fraction in a large pool of donors.
The current study suggests that mechanical ventilation using the LMA Protector™ offers more favorable respiratory mechanics than that using ETT in LDN. Ppeak was lower during pneumoperitoneum and Cdyn was higher throughout surgery in the SGA group than in the ETT group. Because Cdyn involves combination of lung compliance and airway resistance, the results may be explained by the fact that the airway resistance under SGA was significantly lower owing to its wider inner diameter and shorter shaft compared to those of ETT17,18. Dynamic parameters, including Ppeak and Cdyn, are components of the power delivered to the respiratory system during mechanical ventilation19. Mechanical power is a comprehensive concept that comprises all risk factors for ventilator-induced lung injury20,21. Therefore, ventilation with SGA may be one of the ways to reduce ventilator-induced lung injury.
This study has several limitations. First, because of its retrospective nature, we could not determine important factors related to the safety of SGA use and airway-related complications such as oropharyngeal sealing pressure, glottis view using fiber bronchoscopy, sore throat, dysphagia, and hoarseness. Second, PaO2 and PaCO2 were replaced by measures of SpO2 and EtCO2 because intra-arterial catheters are not routinely placed in kidney donors at our institute due to their invasiveness. Third, because we used only the LMA Protector™ in the SGA group, the results may not be reproducible with other SGA devices.
In conclusion, second-generation SGA can be safe alternative to ETT for LDN. There was no change in the leakage fraction during mechanical ventilation with SGA in the lateral position or pneumoperitoneum. SGA use resulted in reduced airway resistance and increased compliance, which suggests that its use can be beneficial in the airway management of kidney donors. Our study suggests the need for a large sample size randomized study to demonstrate the safety of SGA in lateral position under laparoscopy.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
El-Boghdadly, K., Bailey, C. R. & Wiles, M. D. Postoperative sore throat: A systematic review. Anaesthesia 71, 706–717 (2016).
Gordon, J., Cooper, R. M. & Parotto, M. Supraglottic airway devices: Indications, contraindications and management. Minerva Anestesiol. 84, 389–397 (2018).
Brown, T. et al. Introduction of an enhanced recovery protocol into a laparoscopic living donor nephrectomy programme. Ann. R. Coll. Surg. Engl. 102, 204–208 (2020).
Byrne, M. H. V., Mehmood, A., Summers, D. M., Hosgood, S. A. & Nicholson, M. L. A systematic review of living kidney donor enhanced recovery after surgery. Clin. Transplant. 35, e14384 (2021).
Chung, E., Grant, A. B. F., Hibberd, A. D. & Sprott, P. Why potential live renal donors prefer laparoscopic nephrectomy: A survey of live donor attitudes. BJU Int. 100, 1344–1346 (2007).
Liu, Y. et al. LMA® protector™ in patients undergoing laparoscopic surgeries: A multicenter prospective observational study. BMC Anesthesiol. 21, 318 (2021).
Yoon, S. W. et al. Comparison of supraglottic airway devices in laparoscopic surgeries: A network meta-analysis. J. Clin. Anesth. 55, 52–66 (2019).
de Montblanc, J., Ruscio, L., Mazoit, J. X. & Benhamou, D. A systematic review and meta-analysis of the i-gel(®) vs laryngeal mask airway in adults. Anaesthesia 69, 1151–1162 (2014).
Wu, L. et al. Effect of neuromuscular block on surgical conditions during short-duration paediatric laparoscopic surgery involving a supraglottic airway. Br. J. Anaesth. 127, 281–288 (2021).
Kim, D., Park, S., Kim, J. M., Choi, G. S. & Kim, G. S. Second generation laryngeal mask airway during laparoscopic living liver donor hepatectomy: A randomized controlled trial. Sci. Rep. 11, 3532 (2021).
Hernandez, M. R., Klock, P. A. J. & Ovassapian, A. Evolution of the extraglottic airway: A review of its history, applications, and practical tips for success. Anesth. Analg. 114, 349–368 (2012).
Futier, E. et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N. Engl. J. Med. 369, 428–437 (2013).
Austin, P. C. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm. Stat. 10, 150–161 (2011).
McCaul, C. L. et al. Airway management in the lateral position: A randomized controlled trial. Anesth. Anal. 101, 1221–1225 (2005).
Rustagi, P., Patkar, G. A., Ourasang, A. K. & Tendolkar, B. A. Effect of pneumoperitoneum and lateral position on oropharyngeal seal pressures of proseal LMA in laparoscopic urological procedures. J. Clin. Diagn. Res. 11, UC05–UC09 (2017).
Lan, S., Zhou, Y., Li, J. T., Zhao, Z. Z. & Liu, Y. Influence of lateral position and pneumoperitoneum on oropharyngeal leak pressure with two types of laryngeal mask airways. Acta Anaesthesiol. Scand. 61, 1114–1121 (2017).
Bhatt, S. B., Kendall, A. P., Lin, E. S. & Oh, T. E. Resistance and additional inspiratory work imposed by the laryngeal mask airway. A comparison with tracheal tubes. Anaesthesia 47, 343–347 (1992).
Reissmann, H., Pothmann, W., Füllekrug, B., Dietz, R. & Schulte am Esch, J. Resistance of laryngeal mask airway and tracheal tube in mechanically ventilated patients. Br. J. Anaesth. 85, 410–416 (2000).
Marini, J. J., Rocco, P. R. M. & Gattinoni, L. Static and dynamic contributors to ventilator-induced lung injury in clinical practice. Pressure, energy, and power. Am. J. Respir. Crit. Care Med. 201, 767–774 (2020).
Cressoni, M. et al. Mechanical power and development of ventilator-induced lung injury. Anesthesiology 124, 1100–1108 (2016).
Tonetti, T. et al. Driving pressure and mechanical power: New targets for VILI prevention. Ann. Transl. Med. 5, 286–286 (2017).
Author information
Authors and Affiliations
Contributions
Conception and design: G.S.K.; provision of study materials or donors: K.W.L.; collection and assembly of data: J.E.L.; data analysis and interpretation: H.Y.K.; manuscript writing: J.E.L. and H.Y.K.; final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, J.E., Kim, H.Y., Lee, K.W. et al. Second-generation supraglottic airway in laparoscopic donor nephrectomy. Sci Rep 13, 8406 (2023). https://doi.org/10.1038/s41598-023-34691-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-34691-x
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.