Abstract
The aim of this study was to develop a robust algorithm to quantify pulse sharpness that can complement the limitations of radial augmentation index (rAIx) and explore the role of this quantitative sharpness index in reflecting vascular aging or arterial stiffness. The pulse sharpness index (PSI) was developed by combining the end point angle and virtual height, and 528 radial pulses were analyzed. The PSI could be uniformly applied to various waveform morphologies, even those with no or vague tidal waves, unlike the rAIx. Significant sex differences were identified in the rAIx and PSI (P < 0.01 for both), and significant age-dependent decreases in the PSI were observed (P < 0.01). In addition, the PSI and age were correlated (r = − 0.550) at least as strong as the rAIx and age (r = 0.532), and the PSI had a significant negative correlation with arterial stiffness (r = − 0.700). Furthermore, the multiple linear regression model for arterial stiffness using the PSI, age, sex and heart rate showed the excellent performance (cross-validated R2 = 0.701), and the PSI was found to have the greatest influence on arterial stiffness. This study confirmed that the PSI could be a quantitative index of vascular aging and has potential for use in inferring arterial stiffness with an advantage over the rAIx.
Similar content being viewed by others
Introduction
As age increases, the elasticity of arterial vessels decreases, and the inner diameter widens due to changes in the mechanical properties of blood vessels and the cardiovascular system1,2. A decrease in elasticity leads to the stiffness of arterial vessels increasing and the reflected wave returning quickly3,4, and abnormalities in proximal aortic diameter are responsible for the abnormal aortic pressure-flow relationship1,5. This phenomenon increases arterial pressure, which elevates the risk of cardiovascular disease (CVD), including hypertension6,7. Therefore, examining these age-related changes in arterial stiffness and appropriate indicators reflecting the stiffness caused by cardiovascular aging are important to prevent risk factors for CVD8.
The pulse wave velocity (PWV), one of the representative indicators of arterial stiffness, is the speed at which a blood pressure pulse wave propagates through the arterial system. There is a distance measurement error caused by assuming a straight arterial segment, and in the most frequently used carotid-femoral PWV, the carotid and femoral pulse waves traveling in opposite directions cause overestimation of the PWV6.
Another measure of arterial stiffness is the augmentation index (AIx), which is the ratio of the height of the peak above the shoulder of the wave to the pulse pressure9. The AIx is easier to measure and less time consuming than the PWV; additionally, the AIx enables observation of the reflective properties of the arteries10. The AIx increases with age and blood pressure, which has been explained by the fact that wave reflection increases with age3,11. In addition, AIx is known as an independent risk factor for CVD, including coronary artery disease12,13, heart failure14, hypertension15, diabetic retinopathy16 and atherosclerosis17.
An important step in calculating the AIx is exact identification of the shoulder point on the waveform18. At this time, because a close correlation between the aortic AIx and radial AIx (rAIx) has been demonstrated, similar information on the reflection of the central pressure wave can be obtained directly from the radial pulse waveform19. In the case of the radial or type C waveform, the algorithm based on the second negative-to-positive zero-crossing of the fourth derivative pulse waveform has been established to determine the AIx and has been widely used. Recently, because numerical differentiation could amplify noise, especially at high frequencies, a robust algorithm based on a B-spline wavelet or only first- and second-order derivatives of the waveforms have been proposed for improved accuracy and reduced noise18,20. However, there are other inherent limitations in the calculation of AIx aside from algorithm dependency. If the tidal wave in the radial pulse becomes vague, the inflected shoulder point becomes difficult to extract accurately; additionally, in the case of the pulse waveform with only two peaks and without a tidal wave, the AIx cannot be calculated or set to zero21. The most appropriate mathematical expression of the AIx is unclear; in other words, the AIx is an incomplete index because the method for calculating the AIx does not consider various pulse morphologies8,22. Furthermore, an average pulse morphology variability of 7.2% near the rAIx was observed, as determined according to the intra-class distance within a single-period pulse in a previous study, and the variabilities of several pulses were greater than 15%23. These values are now low, and another index that is robust to the morphology variability is needed.
The sharpness of the pulse wave is a representative characteristic in pulse waveform analysis. Because it is well known that blunter waveforms are generally found in older people, whereas sharper pulse waveforms are found in younger people, pulse sharpness could reflect age-related characteristics, such as vascular aging or arterial stiffness, as well as the AIx. In addition, as the average pulse morphology variability near the peak point of the percussive wave was less than only 2% in a previous study, pulse sharpness could be an index with low variability23. However, despite these intuitive considerations of pulse sharpness, few studies have been explored the availability of sharpness as an indicator of vascular aging or arterial stiffness, unlike the AIx. In addition, a formally accepted algorithm for detecting sharpness has not been reported. Although a method for finding both end points of the width of a percussive wave based on determining 2/3 the pulse height and calculating the distance, defined as w, between the two end points has been proposed for calculating the pulse apex angle, it is difficult to derive an accurate result if a tidal wave is generated at a higher position than 2/3 the pulse height24,25,26,27. In addition, in previous studies, the apex angle was calculated based on coordinates using four points before and after the pulse peak28 and on the law of cosines using two neighboring fiducial points29, but these methods were applicable only to the specific shape of the pulse waveform.
Therefore, an objective and easily computable index reflecting pulse sharpness that can be uniformly applied to various waveform morphologies is needed. Furthermore, if the possibility for the clinical usefulness of pulse sharpness is demonstrated, the limitations of the AIx could be overcome. The aim of this study was to develop a robust algorithm to quantify pulse sharpness that can complement the limitations of rAIx and explore the role of this quantitative sharpness index in reflecting vascular aging or arterial stiffness.
Results
A comparison of the PSI, the first proposed index in this study, according to pulse waveform samples with differences in pulse sharpness was performed, and details of the results are provided in Supplementary Fig. S1. The PSI could be uniformly applied to various pulse morphologies, including waveforms that are difficult or too obscure to use in calculating the rAIx or pulse apex angle using w accurately.
Mean difference analysis by sex and age
Table 1 shows the baseline characteristics, including the distribution of sex, age, heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse pressure, height and weight and the sex differences in the rAIx and PSI in each age group with the mean and standard deviation (SD). The rAIx in men was significantly lower than that in women in the entire group and in the groups of subjects in their 20 s, 40 s (P < 0.01), and 30 s (P < 0.05). The PSI in men was significantly higher than that in women in the entire group and in those from their 20 s to 40 s (P < 0.01). Both indices showed no significant sex difference in those over 50 years old.
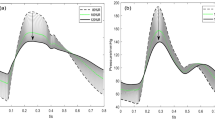
The results of one-way ANOVA for observing the age-related changes in each age group according to sex are presented in Fig. 1 with the morphologies of the ensemble average pulse waveforms in each age group. Both the rAIx and PSI showed a significant difference according to age (P < 0.01). The rAIx was significantly lower in those in their 20 s than in those in the other age groups regardless of sex (P < 0.05); in men, the rAIx was significantly higher in those over 50 years old than in those in the other age groups (P < 0.05). The PSI showed significant results opposite those of the rAIx (P < 0.05 for those in their 20 s and over 50 years old), and the PSI of women in their 30 s was significantly different from that in women over 50 years old (P < 0.05). In addition, typical patterns of waveforms and age-related changes with respect to the rAIx and PSI were observed through the ensemble average pulse waveforms in each age group.
Age-related changes in the radial augmentation index (rAIx) and pulse sharpness index (PSI) according to (a) men and (b) women. The first row indicates the results of the one-way ANOVA in each age group, and the second row indicates the morphologies of ensemble average pulse waveforms in each age group. *P < 0.05.
Correlation and regression analysis according to age
Figure 2a shows scatterplots of the relationship between age and various indices. Positive associations between age and the rAIx and between age and w were observed (correlation coefficient (r) = 0.532 and 0.529, respectively, P < 0.001 for all). On the other hand, a highly negative association between age and the PSI was observed (r = − 0.550, P < 0.001). Figure 2b shows a scatterplot of the relationship and the regression line between the PSI and arterial stiffness inferred by the rAIx. The PSI showed a strong and significant negative correlation with arterial stiffness (r = − 0.700, P < 0.001), and the stiffness could be approximated from the PSI using the appropriate regression equations (R-squared (R2) = 0.484, P < 0.001). Subsequently, scatterplots of the relationship and the regression line between rAIx, PSI and age were shown in Supplementary Fig. S2 for all available data classified by index examination SBP group 1 through 3. The rAIx showed an increasing pattern with aging and the PSI showed a decreasing pattern with aging in all three groups. In addition, the group with lower SBP generally showed higher PSI values.
(a) Scatterplots of relationship between age and the radial augmentation index (rAIx), w and pulse sharpness index (PSI). (b) Scatterplots of relationship and the regression line between the PSI and arterial stiffness inferred by the rAIx. Narrow dotted lines represent the 95% confidence interval of the mean, and wide solid lines represent the 95% prediction interval for individual observations.
Table 2 presents the multiple linear regression (MLR) results for the rAIx and PSI according to age and sex and for arterial stiffness inferred by the rAIx according to the PSI, age, sex and HR. Because the rAIx and PSI showed significant differences by sex, a term for sex was considered in creating the regression model as well as a term for age. MLR analysis revealed that the rAIx and PSI were significantly associated with age and sex (adjusted R2 = 0.320 and 0.357, respectively, P < 0.001 for all). In addition, a higher β value for age than sex was shown for both indices. Arterial stiffness was significantly associated with all four variables (adjusted R2 = 0.699, P < 0.001), and the model including age, sex and HR showed an increased correlation (r = 0.838) compared with that of the model considering the PSI alone (r = − 0.700). In addition, the absolute β value of the PSI for stiffness (β = − 0.601) was found to be greater than that of age (β = 0.167); on the other hand, sex did not appear to have a relatively strong effect.
Table 3 presents the cross-validated R2, root mean square error (RMSE) and mean absolute error (MAE) for the training and test datasets calculated by tenfold cross-validation to evaluate the performance of the three simple linear regression models and an MLR model.
Model 1 for the rAIx according to age showed a relatively lower cross-validated R2 value and lower RMSE and MAE values than model 2 for the PSI according to age. In addition, the performance of model 3 for predicting arterial stiffness inferred by the rAIx based on the PSI was better than that of model 1. Furthermore, MLR model 4 for arterial stiffness according to the PSI, age, sex and HR showed the greatest cross-validated R2 of 0.701 in the test dataset, and it showed excellent performance when evaluated using the RMSE and MAE. Because the performance was not improved with the quadratic model, the results are not described.
Discussion
In this study, the PSI was proposed by combining the end point angle (EPA) calculated based on the intersecting tangent method (ITM) focusing near the peak point regions and virtual height (VH) considering the overall shape of the pulse waveform. It was confirmed that this quantifiable index could be uniformly applied to various waveform morphologies even with no or vague tidal waves, from which it is difficult to calculate the rAIx accurately. In addition, even if a tidal wave was generated at a position higher than 2/3 the pulse height, leading to an incorrect pulse apex angle derived from w, the PSI could also be applied to these waveforms for determining the pulse sharpness accurately. In other words, the PSI could objectively represent the pulse sharpness of any type of waveform, unlike the rAIx or w. Nevertheless, obscure waveforms that could not be used to calculate the rAIx clearly were excluded from this study for comparison with the PSI, and analysis with recognition of the limitation of the rAIx was performed.
A comparison of the rAIx and PSI between men and women showed a significant difference in the entire group and in those from their 20 s to 40 s. The rAIx in women was significantly higher than that in men, which is consistent with the findings of previous studies10,11,30. It has been shown that reflected waves return faster in women than in men because women are generally shorter than men, which leads to a higher rAIx in women than men. In this study, the height in men was significantly higher than that in women as expected, which was considered to be one of the factors that rAIx and PSI are significantly different according to sex.
In addition, the smaller diameter of the radial artery and higher PWV in women could also affect the higher AIx in women31. The PSI was significantly higher in men than in women, which indicates that men have a sharper pulse wave than women. This seems to be explained by the similar phenomenon by which reflected waves affect the rAIx, even though the PSI derived from percussive waves is affected by reflected waves slightly later in time than the rAIx.
A significant age-dependent increase in the rAIx and a significant age-dependent decrease in the PSI were observed in those from their 20 s to 40 s regardless of sex. For example, the rAIx of those in their 20 s was significantly lower than that of subjects in other age groups; on the other hand, the PSI of those in their 20 s was significantly higher than that of subjects in other age groups. These findings indicate that the rAIx and PSI are subject to age-dependent alterations, with sharper pulse waves appearing in younger individuals. In general, blood vessels become stiffer with age, so reflected waves in older people return more quickly and create more overlap with forward waves, causing blunter pulse waveforms3. These hemodynamics affect both the rAIx and PSI, which could be observed in the systolic phase. In addition, these findings are consistent with those of a prior study showing that components of systole could be principal components contributing to age-related factors of the radial pulse8. These sex and age differences could be observed more clearly through the morphology of the ensemble average pulse waveforms according to sex and age. The relationship between the change in the rAIx and PSI was investigated, and the predictive role of both indices could be explored though the waveform morphology.
There were significant associations between age and various indices. The rAIx and distance w used in previous studies showed similar positive correlations with age. In addition, the correlation between the EPA and age (r = 0.497) was slightly weaker than that between the rAIx and age, and VH showed no strong correlation with age (r = 0.284). However, the PSI calculated by combining the EPA and the VH showed the best correlation with age (r = − 0.550). Thus, the EPA, which is focused only near the peak point region, and the VH, which plays an additional role in considering the overall shape of the percussive wave, seem to complement each other. Because the PSI calculated by the robust algorithm showed a usefulness that could be applied to various waveform morphologies and showed a correlation with age at least as strong as that of the rAIx, the possibility of its becoming another indicator reflecting vascular aging, in addition to the rAIx, could be explored. To do this, simple regression analysis was performed, and the PSI showed a strong and significant negative correlation with arterial stiffness inferred by the rAIx (r = − 0.700), and an appropriate regression line could be estimated. Although the correlation between the rAIx and pulse apex angle derived by w has been observed in a previous study (r = 0.428)24, the correlation between the rAIx and PSI in this study showed a much higher value. Based on these relationships between the PSI and age and between the PSI and arterial stiffness, the PSI might be a candidate index to reflect vascular aging and to infer stiffness. In addition, because vascular stiffness is also linked to blood pressure, the relationship between PSI and age at identical levels of blood pressure was also examined32,33. PSI showed a decreasing pattern with aging in all three identical levels of blood pressure groups, and the group with lower SBP generally showed higher PSI values. Even though, there is relatively little data for people over 50 years old, nevertheless it was possible to roughly confirmed that PSI as a quantitative index of vascular aging was related to blood pressure.
The MLR models for the rAIx and PSI considering age and sex together showed a stronger correlation than the simple models considering only age. In addition, the MLR model for the PSI could be suggested to be slightly more accurate than the model for the rAIx. Furthermore, by analogy with β, it was found that age rather than sex had more influence on both rAIx and PSI. The results of rAIx are consistent with the findings of prior studies that age is the most powerful predictor of the rAIx compared to sex, height, HR and so on10,30.
The MLR analysis of arterial stiffness using the PSI, age, sex and HR showed that the four independent variables were significantly associated with stiffness, and the influence of the PSI on stiffness was found to be greater than that of any other variable, including age, which is known as one of the most important factors of stiffness. This means that the PSI contains more information regarding stiffness than age; of course, the age characteristic is also included in the PSI itself. Increasing HR causes a shift in the reflected wave from systole into diastole due to shortening of the ejection duration, which leads to a lower rAIx34. For this reason, HR was also associated with stiffness.
To evaluate the performances of the three simple regression models and an MLR model in this study, tenfold cross-validation was performed. When using the same age group as an independent variable, model 2 showed slightly better performance than model 1, as shown in Table 3. These results indicate that the model for the PSI can reflect vascular aging at least as much as the model for the rAIx. To investigate optimal fitting of the model for arterial stiffness inferred by the rAIx, the PSI alone was first considered in model 3, and four variables were all considered in model 4. Model 3, using the PSI, showed quite better performance than model 1, using age, which means that the PSI could be a more suitable index for reflecting stiffness than age. In addition, model 4 showed the highest performance among the tested models. Approximately 70% of the variance for stiffness could be accounted for by this model, and arterial stiffness could be approximated well from the PSI, age, sex and HR.
In general, the rAIx increases progressively with age up to 60 years and then plateaus, which might be attributable to impaired contractility10,35. In this study, quadratic relations were additionally considered in each regression model, but the performance of these models was not noticeably better than that of the linear models. This is thought to be because there were few data for subjects in their 60 s or older in this study. Therefore, more pulse data from elderly people are required to closely examine changes in the PSI in advanced age. In addition, this study did not consider the PWV, which has been widely used for reflecting arterial stiffness. Although the comparison between AIx and PWV has shown a significant association in prior studies36,37, detailed comparative analysis of the PSI, rAIx and normal PWV is required for a wider and more convincing generalization. And characteristics of the PSI by age based on hemodynamics or heart function should be also investigated38. According to our results, the larger the rAIx, the smaller the PSI tended to be, but it couldn’t always be asserted. The reasons of slightly different tendencies are thought to be that there are various factors affecting the shape of the waveform such as the amplitude or speed of reflected wave and cardiac ejection capacity. Furthermore, this study focused only on the sharpness of radial pulses. The sharpness quantification of aortic, carotid or brachial pulse waveforms and its clinical importance remain to be explored. Nevertheless, it is considered that there is a sufficient possibility that PSI can be used in arteries other than the radial artery. The PSI algorithm may need to be slightly modified due to differences in hemodynamic characteristics for each region, but the basic concept is not expected to be significantly different.
In this study, to complement the limitations of the rAIx, the PSI using a robust algorithm was proposed. The PSI could be uniformly applied to various pulse morphologies without having to consider the shape of the waveform in clinical practice, unlike the rAIx. In addition, this study confirmed that the PSI could be a quantitative index of vascular aging and has potential for use in inferring arterial stiffness with an advantage over the rAIx.
Methods
Experimental data
In this study, left radial artery pulse data recorded in a comfortable upright position from 528 subjects aged 20–84 years were analyzed. These data were collected as part of the Korea Institute of Oriental Medicine (KIOM) project: Development of pulse analysis system for personalized medicine by converging hemodynamics and pulse diagnostics. All 6 clinical trials over the 5 years were approved by the Institutional Review Board of the Kyung Hee University Korean Medicine Hospital: KOMCIRB-2014-70(KCT0002302); KOMCIRB-150622-HR-021(KCT0001604); KOMCIRB-150818-HR-030(KCT0001663); KOMCIRB-160620-HR-031(KCT0002070); and the Institutional Review Board of Gwangju Medical Center, Wonkwang University: 2015/8(KCT0001676); 2016/8-1(KCT0002147). The registration numbers of Korean Clinical Research Information Service are given in parentheses. All studies were conducted in accordance with the principles of the Declaration of Helsinki, and subjects signed written informed consent forms and agreed to the use of their pulse data for the study. Only normal control group subjects without any other medical history were used in this study.
Measurements and signal processing
Pulse signals were measured using a pulse tonometric device (KIOM-PAS ver. 2.0, Republic of Korea) developed by KIOM. The device has been widely used in many clinical studies and several reliable variables calculated using this device have been found to have clinical significances23,39,40,41. The reliability and safety of the device were confirmed based on clinical good manufacturing practices by the Ministry of Food and Drug Safety of Korea, and the electromechanical stability of the device was certified based on the IEC 60601-1 2nd edition. The six-channel piezo-resistive sensor arrayed in a row was used to obtain the pulse signal and the signal from the channel with the largest amplitude was fi-nally selected to analysis. The sensing element has dimensions of 1 × 1 square millimeters (C33, EPCOS, Germany). The continuously evolving tonometric mechanism with a sampling rate of 1000 Hz was applied to the device, and a 60-s pulse series under the same applied pressure was used for the ensemble average pulse analysis39.
The pulse signal was smoothed using the weighted Handerson’s moving average algorithm, and noise from 0.005 to 30 Hz was minimized by applying a Butterworth filter. Baseline correction was performed by third-order spline fitting and spline interpolation, and ITM was applied to extract the starting point of each pulse wave42. Each separated pulse was truncated to the minimum size among the intervals from each starting point to the next starting point. After amplitude normalization, an ensemble average pulse was obtained from a well-refined pulse series. Since individual average pulse signals always have unequal lengths, the pulse length was set at the same interval of 0.8 s by applying resampling method3,34,43. The above signal processing and variable calculations mentioned later were performed on all pulse waveforms using LabVIEW 2016 (National Instruments, USA).
rAIx
The algorithm based on the numerical fourth derivative pulse waveform was applied to calculate the rAIx with the following equation: (late systolic blood pressure/early systolic blood pressure) × 100 (%)9. Because the rAIx decreases linearly with increasing heart rate due to an alteration in the relative timing of the reflected pressure wave caused by a reduction in the ejection duration34,44, the rAIx was corrected for a HR of 75 beats per minute (bpm)45. The PSI proposed in this study can be calculated from any shape of the waveform. However, because a comparative analysis with the previously used rAIx is required in this study, waveforms where the amplitude of the tidal wave did not appear clearly or was obscure were excluded. About 4.5% (24 out of 528 waveforms) of waveforms were found to be difficult to calculate rAIx accurately, and 504 waveforms that could be used to calculate the rAIx clearly were used for analysis10.
Feature extraction and calculation of the pulse sharpness index (PSI)
The ITM mentioned above is the most well-known algorithm with the best performance in extracting the starting point of the pulse waveform46. In this study, the idea of the ITM was converted and applied to the peak point of the percussive wave rather than the starting point of the ensemble average pulse, and feature points for pulse sharpness were detected by this switching of the ITM concept.
First, the correlation coefficient between the average pulse signal and the fitted line consisting of three points on either side of the intersecting tangent (IT) starting point 1 and 2 was calculated. If the correlation was greater than 0.99, points were then added on both sides for regenerating fitted line of five points. This process was repeated adding a point on both sides continuously until the correlation was less than 0.99. Then, if the correlation was less than 0.99, the fitting line generation process was stopped and the final regenerated fitting line becomes IT line 1 or 2. After that, the point on the pulse signal corresponding to the time of an intersection between the tangent at the peak and the IT line 1 or 2 was extracted as end point 1 or 2. A flowchart of the feature extraction and calculation of the EPA, VH and PSI is presented with graphical descriptions in Fig. 3. The EPA could generally reflect the pulse sharpness well based on the solid standard method with feature points, but it might be a local variable that focuses only near the peak point regions. Another variable of VH could consider the overall shape of the percussive wave. Finally, the PSI was determined by using a combination of the EPA and the VH, and it was converted to a natural number by simply multiplying by 1000 as follows:
A sharp pulse waveform yields a high PSI, whereas a blunt pulse waveform yields a low PSI. Differences in the pulse sharpness inferred by the EPA, VH and PSI were compared with the limitations of the two single indicators. The PSI could reflect the pulse sharpness intuitively, unlike the EPA and VH, and details are provided in Supplementary Fig. S3. The PSI could be calculated for all waveforms regardless of the shape of the pulse waveforms. Additionally, the distance w between the points on both sides of the waveform at 2/3 the pulse height was determined to infer the pulse apex angle, as previously described24,25,26,27.
Statistical method
The demographic and baseline characteristics including vital signs of the 504 subjects by sex were summarized. All subjects were separated into four groups based on age, i.e., those in their 20 s, 30 s, 40 s and 50 s or older (N = 147, 111, 180, and 66, respectively), and all statistical methods were applied for the rAIx and PSI.
First, to compare the mean differences between the men and women in each age group, independent t-tests were applied. In addition, the mean differences by age group for each sex were analyzed by one-way ANOVA with Duncan’s post hoc test. If Levene’s test for equal variance was violated, Welch’s robust ANOVA with Dunnett’s T3 post hoc test was applied. The level of significance was set to P < 0.05. Representative ensemble average pulse waveforms by sex and age group were generated to observe the typical patterns of waveforms and age-related changes.
Next, correlation analyses of age with the rAIx, w and the PSI were performed with the r, and linear regression analyses to explore the effect of the PSI on arterial stiffness were performed. At this time, in order to further examine the relationship between blood pressure and other variables, pulse data were divided into three groups according to recorded SBP at the index examination: group 1, < 120 mmHg; group 2, 120 to 139 mmHg; group 3, 140 to 159 mmHg32. In addition, MLR analyses of age and sex with respect to the rAIx following previous studies and with respect to the PSI to explore age-related characteristics were performed. Furthermore, combinations of the PSI, age, sex and HR were applied to determine the best regression model. Because the age distribution of our data was exponential with relatively little data for the elderly, linear regression using logarithm of the age was performed47,48. The results were described by the standardized regression coefficient (β), and a P value of < 0.05 was considered statistically significant. The cross-validated R2, RMSE and MAE after standardizing variables during tenfold cross-validation were used to measure the constructed regression model performance. For reference, in simple linear regression model 1, rAIx is expressed as an index name in order to examine the relation between age and the rAIx variable itself. On the other hand, in multiple linear regression models 3 and 4, arterial stiffness inferred by rAIx is expressed as an index name to examine whether the newly proposed PSI has relevance to arterial stiffness, and for direct interpretation. Mean difference analyses were performed using IBM SPSS statistics 20, and pulse waveform analyses and regression analyses with validation were performed using MATLAB R2018b.
References
O’Rourke, M. F. & Nichols, W. W. Aortic diameter, aortic stiffness, and wave reflection increase with age and isolated systolic hypertension. Hypertension 45, 652–658. https://doi.org/10.1161/01.HYP.0000153793.84859.b8 (2005).
Lazović, B., Mazić, S., Zikich, D. & Žikić, D. The mathematical model of the radial artery blood pressure waveform through monitoring of the age-related changes. Wave Motion 56, 14–21. https://doi.org/10.1016/j.wavemoti.2015.02.001 (2015).
Vlachopoulos, C., O’Rourke, M. & Nichols, W. W. McDonald’s blood flow in arteries: theoretical, experimental and clinical principles 195–223 (CRC Press, 2011).
Hashimoto, J. & Ito, S. Some mechanical aspects of arterial aging: physiological overview based on pulse wave analysis. Ther. Adv. Cardiovasc Dis. 3, 367–378. https://doi.org/10.1177/1753944709338942 (2009).
Mitchell, G. F. et al. Determinants of elevated pulse pressure in middle-aged and older subjects with uncomplicated systolic hypertension: The role of proximal aortic diameter and the aortic pressure-flow relationship. Circulation 108, 1592–1598. https://doi.org/10.1161/01.CIR.0000093435.04334.1F (2003).
Reesink, K. D., Hoeks, A. P. G., Reneman, R. S. & Hermeling, E. Advances in arterial stiffness assessment. Artery Res. https://doi.org/10.1016/j.artres.2011.10.003 (2011).
Rizzoni, D. et al. Prognostic significance of small-artery structure in hypertension. Circulation 108, 2230–2235. https://doi.org/10.1161/01.CIR.0000095031.51492.C5 (2003).
Bae, J.-H., Jeon, Y. J., Lee, S. & Kim, J. U. in 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). 6202–6205 (IEEE).
Kelly, R., Hayward, C., Avolio, A. & O’rourke, M. J. C. Noninvasive determination of age-related changes in the human arterial pulse. Circulation 80, 1652–1659 (1989).
Janner, J. H., Godtfredsen, N. S., Ladelund, S., Vestbo, J. & Prescott, E. Aortic augmentation index: Reference values in a large unselected population by means of the SphygmoCor device. Am. J. Hypertens. 23, 180–185. https://doi.org/10.1038/ajh.2009.234 (2010).
Mitchell, G. F. et al. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: The Framingham Heart Study. Hypertension 43, 1239–1245. https://doi.org/10.1161/01.HYP.0000128420.01881.aa (2004).
Weber, T. et al. Arterial stiffness, wave reflections, and the risk of coronary artery disease. Circulation 109, 184–189. https://doi.org/10.1161/01.CIR.0000105767.94169.E3 (2004).
Hametner, B. et al. Wave reflection quantification based on pressure waveforms alone: Methods, comparison, and clinical covariates. Comput. Methods Programs Biomed. 109, 250–259 (2013).
Tartiere, J. M., Logeart, D., Safar, M. E. & Cohen-Solal, A. Interaction between pulse wave velocity, augmentation index, pulse pressure and left ventricular function in chronic heart failure. J. Hum. Hypertens. 20, 213–219. https://doi.org/10.1038/sj.jhh.1001965 (2006).
Shimizu, M. & Kario, K. Role of the augmentation index in hypertension. Ther. Adv. Cardiovasc. Dis. 2, 25–35. https://doi.org/10.1177/1753944707086935 (2008).
Rema, M., Mohan, V., Deepa, R. & Ravikumar, R. Association of carotid intima-media thickness and arterial stiffness with diabetic retinopathy: The Chennai Urban Rural Epidemiology Study (CURES-2). Diabetes Care 27, 1962–1967 (2004).
Eldrup, N., Sillesen, H., Prescott, E. & Nordestgaard, B. G. Ankle brachial index, C-reactive protein, and central augmentation index to identify individuals with severe atherosclerosis. Eur. Heart J. 27, 316–322. https://doi.org/10.1093/eurheartj/ehi644 (2006).
He, Z. et al. A low-pass differentiation filter based on the 2nd-order B-spline wavelet for calculating augmentation index. Med. Eng. 36, 786–792 (2014).
Millasseau, S. C., Patel, S. J., Redwood, S. R., Ritter, J. M. & Chowienczyk, P. J. Pressure wave reflection assessed from the peripheral pulse: Is a transfer function necessary?. Hypertension 41, 1016–1020 (2003).
Krivoshei, A., Min, M., Lamp, J. & Annus, P. in 2014 IEEE International Symposium on Medical Measurements and Applications (MeMeA). 1–4 (IEEE).
Xu, L., Meng, M. Q.-H. & Wang, K. in 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society. 3148–3151 (IEEE).
Stoner, L. et al. Should the augmentation index be normalized to heart rate?. J. Atherosclerosis 21, 11–16 (2014).
Bae, J.-H., Kim, J. U. & Kim, J. Harmonic analysis of pulse morphology variability for pulse smoothness assessment. Biomed. Signal Process. Control 44, 1–11. https://doi.org/10.1016/j.bspc.2018.03.015 (2018).
Yim, Y. K., Lee, C., Lee, H. J. & Park, K. S. Gender and measuring-position differences in the radial pulse of healthy individuals. J. Acupunct. Meridian Stud. 7, 324–330. https://doi.org/10.1016/j.jams.2014.06.014 (2014).
Wang, K.-Q., Xu, L.-S., Zhang, D. & Shi, C. in Proceedings International Conference on Machine Learning and Cybernetics. 1366–1370 (IEEE).
Ha, Y.-J. et al. Characteristics of Pulse waves in various age categories and applicability of pulse wave to metabolic syndrome using pen-type piezoresistive sensor. J. Internal Korean Med. 33, 257–271 (2012).
Lee, H. Y. et al. Study on the correlation between Sasang constitution and the data of pulse diagnosis device-a systematic review in Korean articles. J. Physiol. Pathol. Korean Med. 26, 621–629 (2012).
Zhang, P.-Y. & Wang, H.-Y. A framework for automatic time-domain characteristic parameters extraction of human pulse signals. EURASIP J. Adv. Signal Process. https://doi.org/10.1155/2008/468390 (2007).
Choi, C. et al. in 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). 4090–4093 (IEEE).
Kohara, K. et al. Radial augmentation index: A useful and easily obtainable parameter for vascular aging. Am. J. Hypertens. 18, 11S-14S. https://doi.org/10.1016/j.amjhyper.2004.10.010 (2005).
Gatzka, C. Australian comparative outcome trial of angiotensin-converting enzyme inhibitor-and diuretic-based treatment of hypertension in the elderly: Gender differences in the timing of arterial wave reflection beyond differences in body height. J. Hypertens. 19, 2197–2203 (2001).
Franklin, S. S. et al. Hemodynamic patterns of age-related changes in blood pressure: The Framingham Heart Study. Circulation 96, 308–315 (1997).
Pogue, V. A., Ellis, C., Michel, J. & Francis, C. K. J. H. New staging system of the fifth Joint National Committee report on the detection, evaluation, and treatment of high blood pressure (JNC-V) alters assessment of the severity and treatment of hypertension. Hypertension 28, 713–718 (1996).
Wilkinson, I. B. et al. Heart rate dependency of pulse pressure amplification and arterial stiffness. Am. J. Hypertens. 15, 24–30 (2002).
O’Rourke, M. F. & Hashimoto, J. Mechanical factors in arterial aging: A clinical perspective. J. Am. Coll. Cardiol. 50, 1–13. https://doi.org/10.1016/j.jacc.2006.12.050 (2007).
Brown, M. Similarities and differences between augmentation index and pulse wave velocity in the assessment of arterial stiffness. Q. J. Med. 92, 595–600 (1999).
Durmus, I., Kazaz, Z., Altun, G. & Cansu, A. Augmentation index and aortic pulse wave velocity in patients with abdominal aortic aneurysms. Int. J. Clin. Exp. Med. 7, 421 (2014).
Reference Values for Arterial Stiffness. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: “Establishing normal and reference values”. Eur. Heart J. 31, 2338–2350. https://doi.org/10.1093/eurheartj/ehq165 (2010).
Bae, J. H., Jeon, Y. J., Kim, J. Y. & Kim, J. U. New assessment model of pulse depth based on sensor displacement in pulse diagnostic devices. Evid. Based Complement. Alternat. Med. 2013, 938641. https://doi.org/10.1155/2013/938641 (2013).
Bae, J. H. et al. Radial pulse and electrocardiography modulation by mild thermal stresses applied to feet: An exploratory study with randomized, crossover design. Chin. J. Integr. Med. 26, 299–306. https://doi.org/10.1007/s11655-017-2972-0 (2017).
Kim, J. et al. A comparative study of the radial pulse between primary dysmenorrhea patients and healthy subjects during the menstrual phase. Sci. Rep. 9, 9716. https://doi.org/10.1038/s41598-019-46066-2 (2019).
Chiu, Y. C., Arand, P. W., Shroff, S. G., Feldman, T. & Carroll, J. D. Determination of pulse wave velocities with computerized algorithms. Am. Heart J. 121, 1460–1470 (1991).
Wang, D., Zhang, D. & Lu, G. A robust signal preprocessing framework for wrist pulse analysis. Biomed. Signal Process. Control 23, 62–75. https://doi.org/10.1016/j.bspc.2015.08.002 (2016).
Wilkinson, I. B. et al. The influence of heart rate on augmentation index and central arterial pressure in humans. J. Physiol. 525, 263 (2000).
Nakae, I., Matsuo, S., Matsumoto, T., Mitsunami, K. & Horie, M. Augmentation index and pulse wave velocity as indicators of cardiovascular stiffness. Angiology 59, 421–426 (2008).
Hemon, M. C. & Phillips, J. P. Comparison of foot finding methods for deriving instantaneous pulse rates from photoplethysmographic signals. J. Clin. Monit. Comput. 30, 157–168. https://doi.org/10.1007/s10877-015-9695-6 (2016).
Rodriguez-Barranco, M., Tobias, A., Redondo, D., Molina-Portillo, E. & Sanchez, M. J. Standardizing effect size from linear regression models with log-transformed variables for meta-analysis. BMC Med. Res. Methodol. 17, 44. https://doi.org/10.1186/s12874-017-0322-8 (2017).
Newman, M. C. Regression analysis of log-transformed data: Statistical bias and its correction. Environ. Toxicol. Chem. 12, 1129–1133 (1993).
Acknowledgements
This study was supported by a grant from the Korea Institute of Oriental Medicine, Republic of Korea (KSN2013110).
Author information
Authors and Affiliations
Contributions
J-H.B. developed the pulse waveform analysis algorithm and contributed to the formal analysis with data curation and interpretation of the results. J-H.B. drafted and wrote the manuscript and Y.J.J. reviewed and edited the manuscripts. All authors approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bae, JH., Jeon, Y.J. Pulse sharpness as a quantitative index of vascular aging. Sci Rep 11, 19895 (2021). https://doi.org/10.1038/s41598-021-99315-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-99315-8
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.