Abstract
Previous studies on the adverse events of acute pulmonary embolism (APE) were mostly limited to single marker, and short follow-up duration, from hospitalization to up to 30 days. We aimed to predict the long-term prognosis of patients with APE by joint assessment of D-dimer, N-Terminal Pro-Brain Natriuretic Peptide (NT-ProBNP), and troponin I (cTnI). Newly diagnosed patients of APE from January 2011 to December 2015 were recruited from three hospitals. Medical information of the patients was collected retrospectively by reviewing medical records. Adverse events (APE recurrence and all-cause mortality) of all enrolled patients were followed up via telephone. D-dimer > 0.50 mg/L, NT-ProBNP > 500 pg/mL, and cTnI > 0.40 ng/mL were defined as the abnormal. Kaplan–Meier curve was used to compare the cumulative survival rate between patients with different numbers of abnormal markers. Cox proportional hazard regression model was used to further test the association between numbers of abnormal markers and long-term prognosis of patients with APE after adjusting for potential confounding. During follow-up, APE recurrence and all-cause mortality happened in 78 (30.1%) patients. The proportion of APE recurrence and death in one abnormal marker, two abnormal markers, and three abnormal markers groups were 7.69%, 28.21%, and 64.10% respectively. Patients with three abnormal markers had the lowest survival rate than those with one or two abnormal markers (Log-rank test, P < 0.001). After adjustment, patients with two or three abnormal markers had a significantly higher risk of the total adverse event compared to those with one abnormal marker. The hazard ratios (95% confidence interval) were 6.27 (3.24, 12.12) and 10.7 (4.1, 28.0), respectively. Separate analyses for APE recurrence and all-cause death found similar results. A joint test of abnormal D-dimer, NT-ProBNP, and cTnI in APE patients could better predict the long-term risk of APE recurrence and all-cause mortality.
Similar content being viewed by others
Introduction
Acute pulmonary embolism (APE) is one of the most frequent cardiovascular diseases which characterizes the blockage of pulmonary arterial bed by thromboemboli, usually a consequence of deep vein thrombosis (DVT)1. It is the most serious clinical outcome of venous thromboembolism (VTE), with a high mortality rate following myocardial infarction and cancer. Untreated APE could have a mortality rate as high as 30%, whereas diagnosis and treatment could lower the disease-attributed mortality rate to 2–8%, with the recurrence rate at 4–17%2. Comprehensive examinations and treatment are therefore essential for APE patients.
D-dimer, N-terminal pro b-type natriuretic peptide (NT-proBNP), and Cardiac troponin I (cTnI) are important biomarkers of the occurrence, development, and prognosis of APE. D-dimer is a biomarker for activation of coagulation and fibrinolysis. NT-proBNP is released due to increasing myocardial stretch and is positively associated with the severity of right ventricular dysfunction. cTnI specifically reflects myocardial injury. These biomarkers have also been reported for predicting clinical adverse events in APE patients3,4,5.
Current literature on the adverse events of APE was mostly limited to mortality in the short duration of hospitalization6,7, or up to 30 days8,9. A few studies suggested that these clinical tests may potentially be associated with long-term prognosis10,11. Because of the specificity limitation of any single biomarker1, combinations of these tests have been created and applied to improve risk stratification12,13,14,15,16. This study aimed to analyze the joint effect of D-dimer, NT-proBNP, and cTnI on predicting long-term adverse event risk on APE patients.
Methods
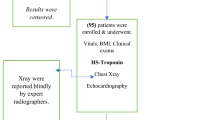
Study population
Physician retrospectively reviewed medical records of hospitalized APE patients in the North China University of Science and Technology Affiliated Hospital, Tangshan Workers’ Hospital, and Kailuan General Hospital during January 1st, 2011 and December 31st, 2015. This study was approved by the Review Board of the Kailuan General Hospital. All methods were performed in accordance with the relevant guidelines and regulations and were in accord with the Declaration of Helsinki. All participants provided written informed consent. Inclusion criteria were: (1) incident APE patient, (2) no history of chronic PE, and (3) aged over 18 years. Exclusion criteria were: patients who (1) received thrombolytic or anticoagulant therapy prior to hospitalization, (2) accompanied by thrombotic diseases, myocardial infarction, cerebrovascular diseases, hematologic diseases, infectious diseases, sepsis, liver diseases, or kidney diseases, or (3) had no D-dimer, NT-proBNP, and cTnI tests.
Due to the lack of the risk ratio of the combination of indicators in the literature, we used the sample size calculation for cohort studies:
According to the literature, the APE mortality rate for the individual mortalities are around 11.2% for D-dimer > 0.50 mg/L17, 20.0% for cTnI > 0.05 ng/ml18, and 16.8% for NT-Pro BNP > 600 pg/Ml1, respectively. Based on these values, when a single marker is abnormal, the maximum mortality of cTnI abnormality is estimated as 20.00%, therefore p0 = 20.0%. We estimated that when all three indicators are abnormal, the mortality rate of APE should be higher than 50%, therefore p1 = 50.0%. Using the formula with α = 0.05 (bilateral) and β = 0.10, the sample size calculation resulted in a single group of 51 cases, and a total of 102 cases. Considering a 20% potential risk of loss to follow follow-up, at least 128 cases were required.
APE was diagnosed according to the 2015 Chinese Expert Consensus on Diagnosis and Management of Acute Pulmonary Embolism17. Patients received and were diagnosed on at least one of the following examinations: computed tomographic pulmonary angiography, ventilation-perfusion scintigraphy, and pulmonary artery angiography.
The following data were retrieved from medical records. Personal characteristics included hospital, age, sex, smoking status (never, past, or current smoker), and alcohol consumption status (never, past, or current drinker). Clinical and physical characteristics included change in psychological status (presence of anxiety, tiring, sleepiness, fatigue, frustration, unconsciousness, fear, and agony, etc.), heart rate, systolic blood pressure (SBP), D-dimer, NT-proBNP, and cTnI levels, and blood oxygen saturation (SaO2; prior to oxygen supply). Treatment details included thrombolytic therapy, anticoagulant treatment, and interventional therapy. Accompanied diseases included cancer and chronic cardiovascular diseases. Data were de-identified during analyses.
Classification
All three hospitals used the same methods for assessments. D-dimers were quantitatively determined by enzyme-linked immunosorbent assay (ELISA), and NT-Pro BNP and cTnI were quantitatively determined by electrochemiluminescence immunoassay (ECLIA). Detailed analytical methods were summarized in Supplemental Table 1. According to the Chinese expert consensus on the diagnosis and treatment of acute pulmonary embolism in 2015, D-dimer > 0.50 mg/L was classified as abnormal19. According to the 2011 scientific statement of the American Heart Association on the treatment of large and sub-large pulmonary embolism, deep vein thrombosis, and chronic thromboembolic pulmonary hypertension, NT-ProBNP > 500 pg/ml and cTnI > 0.40 ng/ml were considered as abnormal and these values were used as cut-off values in our study20. Patients were further categorized by the number of abnormalities met: 0, 1, 2, or 3.
Follow-up
Included APE patients were followed up via telephone call in May 2016 for adverse events and prescription adherence after discharge. Adverse events included all-cause mortality and APE recurrence. Prescription adherence was considered satisfactory if patients: (1) followed prescriptions without altering the drugs or dosage, (2) had regular revisits with their doctors, and (3) refrained from smoke, alcohol, and warfarin inhibitors. Deaths reported during telephone interviews were confirmed through linkage to the vital office for exact time and cause. Rehospitalization cases reported were confirmed through medical records. Patients who survived without APE recurrence were censored for an adverse event.
Statistical analysis
Data were recorded and managed in EpiData version 3.1, and analyzed in SAS version 9.3 9SAS Institute, Cary, USA) after de-identification. Chi-square test and Fisher’s exact test were used to compared baseline characteristics across baseline markers abnormalities. Kaplan–Meier survival curves categorized by the number of abnormalities were plotted and compared by log-rank test for total adverse event, and APE recurrence or all-cause mortality separately.
Cox proportional hazard model was used to analyze the association between baseline abnormality number and adverse events. Time to event or censor was calculated from the date of hospitalization to the date of follow-up. Covariates included age, sex, heart rate, SBP, smoking, alcohol consumption, change in psychological status, SaO2, disease history, treatment, and prescription adherence. Prescription adherence was collected from patients who were alive at the time of follow-up and adjusted only in the analysis for APE recurrence. The significance level was set as α = 0.04. All tests were two-sided.
Results
A review of medical records identified 432 APE patients. Of them, 13 were excluded for receiving thrombolytic or anticoagulant therapy prior to hospitalization; 20 were lost to follow-up; 43 did not receive D-dimer test, 96 did not receive NT-proBNP test, and 1 did not receive cTnI test. A total of 259 APE patients were included in the analysis.
At baseline, the mean age was 61.4 + 13.8 years, and 132 (51.0%) were men. Baseline characteristics of the included participants are presented in Table 1. Seven did not have abnormal values for either D-dimer, NT-proBNP, or cTnI tests; 67 had single abnormality; 117 had 2 abnormalities (Group 2); 68 had 3 abnormalities (Group 3). Due to the small number of patients without abnormal values, they were categorized together with the single abnormality group (Group 1).
The median survival time to the total adverse event was 45.6 months. Group 3 had the shortest median survival time of 17.3 months, and a significantly lower survival rate than the other two groups (p < 0.001, Fig. 1).
Compared to Group 1, Group 3 had a significantly higher hazard ratio (HR) of 10.7 (95% confidence interval [CI]: 4.08 to 28.06) and 6.27 (95% CI: 3.24, 12.12, Table 2), compared to Groups 1 and 2, respectively, for adverse events. A significantly higher risk persisted in Group 3 after separating the outcomes. For APE recurrence, the HRs (95% CIs) compared to Groups 1 and 2 were 8.78 (2.49, 30.91) and 5.06 (2.18, 11.83); for all-cause mortality, HRs (95% CIs) compared to Groups 1 and 2 were 7.88 (1.70, 36.54) and 4.98 (1.72, 14.48), respectively (Table 2). No significant difference was found between Groups 1 and 2 (p > 0.05 for all outcomes, Table 2). Comparison between individual markers was presented in Supplemental Table 2.
Discussion
This study found that joint test of D-dimer, NT-proBNP, and cTnI during hospitalization was able to predict long-term adverse events after discharge. Patients with abnormal values in all 3 markers had 11.3 and 6.4 times of risk of patients with one or two abnormalities.
Compared to patients with a single abnormality, a higher risk of adverse events in patients with two markers of abnormalities was not found in this study. This finding did not support previous studies on the joint effect of two tests. One study reported that APE patients with abnormal NT-proBNP and cTnI levels had a 30% mortality rate, while those with a single abnormal NT-proBNP only had a 3.7% mortality rate18. Similarly, another study found that APE patients with NT-proBNP ≥ 600 ng/L and cTnT ≥ 0.07 mg/L had a 33% mortality rate at 40 days after discharge12. Several reasons may explain the difference. First, due to the rapid progress of APE, there may be variability in three biomarkers2. Second, these studies were limited in small sample size which limited the ability to test the difference between groups12,18. Third, these biomarkers might have different prognostic values in predicting short-term versus long-term adverse event risk. Large prospective cohort studies are warranted for elucidating the association.
Studies have shown that biomarkers such as D-dimer, NT-proBNP, and cTnI are related to pulmonary artery obstruction. Pulmonary circulatory disturbances caused by APE can increase pulmonary artery pressure, leading to myocardial damage or right ventricular dysfunction21. D-dimer is a soluble degradation product of cross-linked fibrin under the action of the fibrinolytic system. Its level reflects the generation of thrombin and the activity of plasmin and has high clinical sensitivity for the diagnosis of APE22. NT-proBNP is mainly synthesized and secreted by the ventricular myocytes of the heart. When acute pulmonary embolism occurs, it will reduce the effective blood flow of the pulmonary vascular bed, increase the pressure of the pulmonary artery, increase the tension of the right ventricle, and cause right heart dysfunction23. As a specific marker of myocardial injury, a high cTnI level indicates impaired right ventricular function, which is more likely to cause right heart failure or cardiogenic shock in patients24. Together, these three markers suggest strong potential in predicting the long-term prognosis of individuals with APE. The survival plot in our study indicated that during the follow-up of around 4 years, the all-cause mortality rate kept at a high level (Fig. 1). Moreover, the current consensus on APE also focused on short-term adverse events, therefore the recommendations might not be able to effectively predict long-term outcomes. The joint analysis of 3 frequently used biomarkers might be of clinical significance for identifying high-risk patients. For patients with abnormal values of D-dimer, NT-proBNP, and cTnI together, special treatment and frequent revisit might be warranted to lower the risk for long-term recurrence and mortality.
Limitations of this study should be noted. First, due to the limited sample size, cause-specific deaths were not analyzed separately. The association between joint tests of D-dimer, NT-proBNP, and cTnI and APE-attributed mortality remained unclear. Second, 173 patients were excluded due to missing information or lost to follow-up. However, we compared the baseline characteristics of included versus the total identified participant and found no significant difference. Despite these limitations, the quality of our study was well controlled. Medical records of patients were reviewed by two physicians, where uncertain cases were decided by a third physician. Recurrence and mortality information reported during telephone interviews were confirmed by review of records or certificates. Various confounding factors were adjusted in our model.
To conclude, the presence of D-dimer, NT-proBNP, and cTnI abnormalities together in APE patients was associated with a higher risk of long-term recurrence and mortality compared to less or no abnormalities. Special care and follow-up might be important for these patients.
Data availability
Data would be made available from the corresponding authors upon reasonable request and approval.
References
Konstantinides, S. V. et al. Corrigendum to: 2014 ESC Guidelines on the diagnosis and management of acute pulmonary embolism. Eur. Heart J. 36, 2642 (2015).
Carson, J. L. et al. The clinical course of pulmonary embolism. N. Engl. J. Med. 326, 1240–1245 (1992).
Palareti, G. et al. D-dimer to guide the duration of anticoagulation in patients with venous thromboembolism: a management study. Blood 124, 196–203 (2014).
Alonso-Martínez, J. L., Annicchérico-Sánchez, F. J., Urbieta-Echezarreta, M. A. & Pérez-Ricarte, S. N-terminal pro-B type natriuretic peptide as long-term predictor of death after an acute pulmonary embolism. Med. Clin. 144, 241–246 (2015).
Weekes, A. J. et al. Prognostic value of right ventricular dysfunction markers for serious adverse events in acute normotensive pulmonary embolism. J. Emerg. Med. 52, 137–150 (2017).
Kucher, N. et al. Low pro-brain natriuretic peptide levels predict benign clinical outcome in acute pulmonary embolism. Circulation 107, 1576–1578 (2003).
Kucher, N., Printzen, G. & Goldhaber, S. Z. Prognostic role of brain natriuretic peptide in acute pulmonary embolism. Circulation 107, 2545–2547 (2003).
Tanabe, Y., Obayashi, T., Yamamoto, T., Takayama, M. & Nagao, K. Predictive value of biomarkers for the prognosis of acute pulmonary embolism in Japanese patients: Results of the Tokyo CCU Network registry. J. Cardiol. 66, 460–465 (2015).
Bajaj, A. et al. Prognostic value of biomarkers in acute non-massive pulmonary embolism: A systematic review and meta-analysis. Lung 193, 639–651 (2015).
van der Meer, R. W. et al. Right ventricular dysfunction and pulmonary obstruction index at helical CT: Prediction of clinical outcome during 3-month follow-up in patients with acute pulmonary embolism. Radiology 235, 798–803 (2005).
Tong, C. & Zhang, Z. Evaluation factors of pulmonary embolism severity and prognosis. Clin. Appl. Thromb. Hemost. 21, 273–284 (2015).
Kostrubiec, M. et al. Biomarker-based risk assessment model in acute pulmonary embolism. Eur. Heart J. 26, 2166–2172 (2005).
Lankeit, M. et al. A simple score for rapid risk assessment of non-high-risk pulmonary embolism. Clin. Res. Cardiol. 102, 73–80 (2013).
Dellas, C. et al. Elevated heart-type fatty acid-binding protein levels on admission predict an adverse outcome in normotensive patients with acute pulmonary embolism. J. Am. Coll. Cardiol. 55, 2150–2157 (2010).
Hunt, B. J. et al. The DiPEP (Diagnosis of PE in Pregnancy) biomarker study: An observational cohort study augmented with additional cases to determine the diagnostic utility of biomarkers for suspected venous thromboembolism during pregnancy and puerperium. Br. J. Haematol. 180, 694–704 (2018).
Stewart, L. K. et al. Comparison of acute and convalescent biomarkers of inflammation in patients with acute pulmonary embolism treated with systemic fibrinolysis vs. placebo. Blood Coagul. Fibrinol. 28, 675–680 (2017).
Grau, E. et al. D-dimer levels correlate with mortality in patients with acute pulmonary embolism : Findings from the RIETE registry. Crit. Care Med. 35(8), 1937–1941 (2007).
Torbicki, A. et al. Guidelines on the diagnosis and management of acute pulmonary embolism: The Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). Eur. Heart J. 29(18), 2276–2315 (2008).
[Chinese expert consensus on the diagnosis and management of acute pulmonary embolism (2015)]. Zhonghua Xin Xue Guan Bing Za Zhi. 2016;44:197–211.
Michael, R. J., Sean McMurtry, M., Stephen, L. A., Mary, C., Neil, G., Samuel, Z. G., et al. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation. 123(16):1788–1830 (2011).
Kline, J. A. et al. Comparison of 8 biomarkers for prediction of right ventricular hypokinesis 6 months after submassive pulmonary embolism. Am. Heart J. 156(2), 308–314 (2008).
Sendama, W. & Musgrave, K. M. Decision-making with D-dimer in the diagnosis of pulmonary embolism. Am. J. Med. 131(12), 1438–1443 (2018).
Verschuren, F. et al. The prognostic value of pro-B-Type natriuretic peptide in acute pulmonary embolism. Thromb. Res. 131(6), e235–e239 (2013).
Hakemi, E. U., Alyousef, T., Dang, G., Hakmei, J. & Doukky, R. The prognostic value of undetectable highly sensitive cardiac troponin I in patients with acute pulmonary embolism. Chest 147(3), 685–694 (2015).
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
H.G. and Y.L. designed this study. X.L., L.Z., J.H., and L.S. collected the data. X.L. and L.Z. conducted the statistical analyses and drafted the manuscript. All authors revised the manuscript and gave final approval. X.L. and L.Z. contributed equally and served as co-first authors. H.G. and Y.L. contributed equally and served as co-corresponding authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, X., Zheng, L., Han, J. et al. Joint analysis of D-dimer, N-terminal pro b-type natriuretic peptide, and cardiac troponin I on predicting acute pulmonary embolism relapse and mortality. Sci Rep 11, 14909 (2021). https://doi.org/10.1038/s41598-021-94346-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-94346-7
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.