Abstract
Hepatectomy and transplantation are the main surgical therapies for HCC patients, and radiotherapy or chemotherapy is often used as adjuvant treatment. Researches have evaluated the independent predictors of HCC, but evidence for factors predicting the efficacy of chemotherapy is rare. Patients diagnosed with HCC between 2010 and 2015 from the SEER database were included and randomly divided into non-chemotherapy and chemotherapy groups. The predictors of CSS and OS were analyzed with the Cox proportional-hazards regression model and Fine and Gray’s competing risk model. Although there was no significant difference in survival analysis between the chemotherapy and non-chemotherapy groups, the cumulative cancer-specific mortality of most HCC patients was decreased in the chemotherapy group. AJCC stage, tumor size, grade, surgery and radiotherapy were predictors of OS and CSS in the non-chemotherapy group, while AJCC stage, tumor size, AFP, grade and surgery in the chemotherapy group. Surgery combined with chemotherapy was applicable to all AJCC stage patients. Surgery was the major treatment option for patients in AJCC I and AJCC II stage, and chemotherapy in AJCC III and AJCC IV stage. In conclusion, the study provided population-based estimates of the prognostic factors in HCC patients with or without chemotherapy.
Similar content being viewed by others
Introduction
According to Global Cancer Statistics 20181, liver cancer is the sixth most commonly diagnosed cancer and the fourth leading cause of cancer death worldwide (8% of total cancer deaths). Primary liver cancer includes hepatocellular carcinoma (HCC), intrahepatic cholangiocarcinoma (ICC) and other types. HCC comprises approximately 75–85% of all liver cancers, while ICC approximately 10–15%. The incidence of liver cancer increased in many eras of the world between 1978–1982 and 2008–2012, particularly in Oceania, North and South America and in much of Europe. While the incidence rates declined in many Asian countries2. Kaplan–Meier methods and the Cox proportional-hazards regression model are the most widely used method of survival analysis3. However, cancer-specific death and death of other causes are common in the outcomes of patients with liver cancer. These two kinds of death are competing events, one of which will prevent the occurrence of the other. Traditional survival analysis can only consider one endpoint, which may overestimate the risk of interesting events, so we used the Fine and Gray model based on the sub-distribution hazard to solve this problem at the same time4,5,6.
Currently, hepatectomy and liver transplantation are the main surgical therapies for patients with HCC. And radiotherapy or chemotherapy is often used as adjuvant or palliative treatment. The American Association for the Study of Liver Diseases (AASLD) suggested that adjuvant therapy should not be routinely used in patients with liver cancer following successful resection or ablation7. And several studies have analyzed the independent predictive factors of HCC by utilizing traditional survival analysis or competing risk analysis8,9,10,11. However, evidence for factors that could predict the efficacy of chemotherapy is still lacking.
Thus, our objective of this study is to evaluate the predictors associated with the survival of patients with HCC, who were registered within the SEER database grouped by chemotherapy through the competing risk model and the Cox proportional-hazards regression model.
Materials and methods
Data source
Specific clinicopathological data and prognostic outcomes of HCC patients from 2010 to 2015 were retrieved from the SEER database. This study did not require a local ethics approval or a statement. Because all the data used in this study were retrieved from the SEER database with a publicly available approach.
Patients
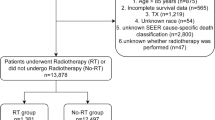
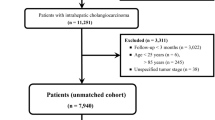
The identification of HCC was based on the International Classification of Disease for Oncology. The inclusion criteria included: (1) the patients were diagnosed between 2010 and 2015; (2) age < 75 years old; (3) primary site code C22.0; (4) histologic type code 8170-8175; (5) complete survival data. The exclusion criteria included: (1) incomplete AJCC7th tumor-node-metastasis (TNM) stage; (2) unknown SEER cause-specific death classification; (3) unknown grade and tumor size; (4) unknown AFP and fibrosis score; (5) unknown race; (6) unknown treatment. (Fig. 1).
All included patients (n = 1988) were divided into two groups according to whether they receive chemotherapy. Chi-square test was used for the comparison of these categorical variables in two groups. Race, AJCC TNM stage, grade, tumor size, AFP, fibrosis score, radiation and surgery were statistically different. So we matched the two groups of data with propensity score matching (PSM) method to eliminate these differences.
Clinical variables of patients
Information on demographic factors (race, age and sex), tumor-related factors (tumor diameter, grade and AJCC staging system), therapeutic factors (surgery, chemotherapy, and radiotherapy) and follow-up were collected from the SEER database. Based on the Surgery Codes of the SEER program, we divided the surgical procedures into four categories: no surgery, hepatectomy, transplantation and other surgical procedures (e.g., Heat-Radio-Frequency ablation (RFA), and Percutaneous Ethanol Injection (PEI)).
OS and CSS were the interesting endpoints. The specific cause of death was based on the code of “SEER cause-specific death classification” in the SEER database. OS was calculated from the date of diagnosis to the date of death caused by any cause or the most recent follow-up. CSS was defined as the interval between the date of diagnosis and date of death due only to HCC or the most recent follow-up.
Statistical analysis
Age and tumor size were categorically divided based on the optimal cut-off value generated by X-tile software version 3.6.1 (Yale University School of Medicine, US) (Fig. 2). Categorical variables were expressed as a number (percent, %) and compared by the chi-square test. The propensity score matching analysis was completed by using the “Matchlt” package on R software. After obtaining PSM matched data, we analyzed the statistical differences in variables between the two groups by using the “CBCgrps” package on R software. Cancer-specific death and death of other causes were regarded as the two competing endpoint events, and the associations between variables and the risk of cancer-specific death were evaluated by Fine and Gray’s competing risk analysis. The Kaplan–Meier method and log-rank test were used for survival analysis. The independent predictive factors in the Fine and Gray competing risk model were incorporated to predict the 1-, 3-, and 5-year CSS probability. The independent risk factors were identified by univariate and multivariate Cox proportional-hazards regression analyses for OS and CSS. SPSS version 24 (SPSS, Inc., Chicago, IL, USA) and R software version 4.1.1 (R Project, Vienna, Austria) was used for all analysis. A statistically significant cutoff value was set up as P < 0.05, two-sided. P < 0.2 was selected as filter value for univariate to multivariate analysis.
Results
Patients' demographics and clinicopathological characteristics
A total of 1988 patients were selected in the process and randomly divided into non-chemotherapy group and chemotherapy group before propensity score matching, of which 758 received chemotherapy while the others did not. Of all the risk factors, race, AJCC stage, grade, tumor size, AFP, fibrosis score, radiotherapy, surgery and survival time were statistically different between the two groups. In the chemotherapy group, the patients who were males, Whites, age between 66 and 74 years old were more than that in the non-chemotherapy group. Besides, more patients had AJCC II or III stage, well-differentiated tumors, positive AFP, severe fibrosis and cirrhosis and tumor size between 3.5 and 7.2 cm in the chemotherapy group. And more patients with chemotherapy received radiotherapy, hepatectomy and transplantation, and didn’t undergo the surgery (S1).
Patients' demographics and clinicopathological characteristics after propensity score matching
1092 patients were selected in the process and randomly divided into non-chemotherapy group and chemotherapy group at a ratio of 1:1, of which 546 received chemotherapy while the others did not. Of all the patients, most of them were males (79%), Whites (68%), age less than 59 years old (46%) and had tumors with AJCC I stage (39%), moderate differentiation (50%) and tumor size less than 3.5 cm (46%). In addition, the majority of patients had positive AFP (70%) and severe fibrosis and cirrhosis (77%). As for treatment, 993 (91%) didn’t receive radiotherapy and 444 (41%) were not available for any surgical procedures. The median survival time was 23 months in all 1092 patients, and 22 months, 23 months in non-chemotherapy and chemotherapy groups, respectively (Table 1).
Univariate and multivariate analysis of OS in the patients with chemotherapy and without chemotherapy
Univariate analysis demonstrated that AJCC stage, tumor size, grade, surgery and radiotherapy were associated with OS in the non-chemotherapy group, and AJCC stage, tumor size, AFP, fibrosis score, grade, surgery and radiotherapy in the chemotherapy group.
Multivariate Cox analysis of OS showed that patients with radiation had a longer OS (hazard ratio (HR), 0.603; 95% confidence interval (CI) 0.410–0.885; p = 0.010) in the non-chemotherapy group, as for those with chemotherapy, radiation made no difference to the OS (p = 0.195). AFP positive was associated with a shorter OS in the chemotherapy group (HR, 1.434; 95% CI 1.081–1.901; p = 0.012). While for patients without chemotherapy, whether AFP positive or not had no effect on the OS. Using well-differentiated grade as a reference, poorly differentiated tumors (HR, 1.947; 95% CI 1.349–2.809; p = < 0.001) and undifferentiated tumors (HR, 3.892; 95% CI 1.496–10.128; p = 0.005) were associated with poor OS in the non-chemotherapy group, while only poorly differentiated tumors (HR, 1.578; 95% CI 1.097–2.269; p = 0.014) in the chemotherapy group.
In both groups, AJCC TNM stage (II, III, IV), tumor size (3.5–7.2 cm, > 7.2 cm) and surgical options (hepatectomy, hepatectomy and transplant, others) were identified as significantly associated with OS in multivariate analysis (Table 2).
Univariate and multivariate analysis of CSS in the patients with chemotherapy and without chemotherapy
Univariate analysis demonstrated that AJCC stage, tumor size, grade, surgery and radiotherapy were associated with CSS in the non-chemotherapy group, and AJCC stage, tumor size, AFP, fibrosis score, grade, surgery and radiotherapy in the chemotherapy group.
Multivariate Cox analysis of CSS showed that patients with radiation had a longer CSS (hazard ratio (HR),0.519; 95% CI 0.341–0.789; p = 0.002) in the non-chemotherapy group, while for those with chemotherapy, radiation made no difference to the CSS (p = 0.429). AFP positive was associated with a shorter OS in the chemotherapy group (HR, 1.487; 95% CI 1.095–2.020; p = 0.011). While for patients without chemotherapy, whether AFP positive or not did not affect CSS. All surgical options were associated with a longer CSS in the non-chemotherapy group, but in the chemotherapy group, other surgical therapies were not associated with CSS (p = 0.051). Using well-differentiated grade as a reference, poorly differentiated tumors and undifferentiated tumors were associated with poor CSS in the non-chemotherapy group, while only poorly differentiated tumors in the chemotherapy group.
In both groups, AJCC TNM stage (III, IV) and tumor size (3.5–7.2 cm, > 7.2 cm) were identified as significantly associated with the CSS in multivariate analysis (Table 3). The conclusion above was consistent with the result of competing risk regression analysis (S3).
Cumulative cancer-specific mortality and other causes-specific mortality of patients with HCC stratified for chemotherapy
Table 4 showed the cumulative incidence of cancer-specific death increased with elevated AJCC TNM stage, poorly differentiated grade, increasing tumor size, positive AFP, radiotherapy and surgery in both groups. In addition, in the chemotherapy group, severe fibrosis or cirrhosis was associated with the increased cumulative incidence of cancer-specific death (p = 0.007), but not in the non-chemotherapy group (p = 0.638) (Table 4).
The cumulative incidence and causes of death between the non-chemotherapy and chemotherapy groups
The cumulative incidence of cancer-specific death was higher than that of other causes-specific death, but there was no statistically significant difference between the two groups. Compared with the non-chemotherapy group, the 1-year cumulative incidence of cancer-specific death was decreased in the chemotherapy group, but the 3-year and 5-year cumulative incidence were increased (Table 5). What’s more, the 1-year, 3-year and 5-year cumulative incidence of other causes-specific death were all decreased after receiving chemotherapy (Table 6).
In both groups, the majority of patients died of liver-related diseases. But the significant differences in causes of death between the two groups were not found (Table 5).
Patients’ demographics and clinicopathological characteristics grouped by AJCC stage
Considering the different severity of the disease, clinicians were inclined to take different treatment options, so we divided the patients into groups according to the AJCC stage. Among the total 1092 patients, 426 were in AJCC I stage, 389 in II, 185 in III, and 92 in IV. Regardless of the AJCC stage, patients with well-differentiated and moderately differentiated tumors formed a sizeable majority. Overall, the degree of tumor differentiation decreased with the increasing AJCC stage. Tumor size, fibrosis score and AFP varied greatly with different stages. And surgery alone (S) or surgery combined with chemotherapy (SC) was the major treatment for patients in AJCC I (S, 31%; SC, 31%) and AJCC II stage(S, 39%; SC, 32%). While in AJCC III and IV stage, chemotherapy alone (C) (AJCC III, 23%; AJCC IV, 21%) or surgery combined with chemotherapy (SC) (AJCC III, 20%; AJCC IV, 14%) was the main treatment for patients (S2).
Competing risk analysis of cancer-specific death in HCC patients grouped by AJCC stage
Competing risk analysis of cancer-specific death in HCC patients grouped by AJCC stage showed that surgery alone (S) was the better treatment option than surgery combined with chemotherapy (SC) in AJCC I, II and III stage, but not in AJCC IV stage. This conclusion was broadly consistent with the results obtained by grouping chemotherapy. The contrary result in the AJCC IV stage may be due to the fact that most of the patients at this stage chose the surgery combined with chemotherapy, while very few chose the surgery alone (S3).
Discussion
Cancer-specific death and other causes-specific death are mutually exclusive endpoints in oncology research. Competing events are regarded as censoring and cancer-specific mortalities, which may be overestimated when using traditional Kaplan–Meier and Cox methods23,24. Therefore, there may be a deviation in the prognosis assessment of patients, which will create a substantial psychological burden to patients and affect their lives. Currently, we conducted a real-world study based on the SEER database to identify the independent predictive factors of CSS of patients diagnosed with HCC depending on whether receiving chemotherapy or not through using the competing risk method. And we used the competing risk model to predict cumulative mortality. By comparing the Cox regression method and competing risk method, we could find the more precise predictor for the prognosis of HCC patients.
The two regression models both identified AJCC stage, tumor size, grade, surgical therapy and radiotherapy as independent predictive factors of OS and CSS in the non-chemotherapy group, and AJCC stage, tumor size, grade, surgical therapy as well as AFP in the chemotherapy group. In our research, competing factors had little impact on the mortality of these patients. Regardless of chemotherapy, higher AJCC stage and grade, larger tumor size and without surgical procedures were associated with poor prognosis. In addition, radiotherapy had been proved to be an effective treatment for patients with unresectable HCC25, in this research, radiotherapy was also an effective treatment for patients who hadn’t received chemotherapy. And negative AFP predicted a longer survival time for those who had received chemotherapy, which was consistent with many studies26,27.
Through comparing the prognosis outcomes of different surgical therapies, we found that liver transplantation was the most effective treatment regardless of chemotherapy. And the proportion of patients dead of HCC after liver transplantation was similar in both groups. Of 153 patients in the non-chemotherapy group were administered liver transplantation and 30 died during follow-up, including 16 (53%) of HCC and 14 (47%) of other causes. While in the chemotherapy group, of 145 patients, 24 died, including 16 (67%) of HCC and 8 (33%) of other causes. Thus, the survival analysis of patients receiving liver transplantation should consider the competing events. Interestingly, for patients with hepatectomy or transplantation, the cumulative incidence of cancer-specific death was increased in the chemotherapy group, but decreased for patients without any surgical therapies after being administered chemotherapy. In addition, for patients undergoing other types of surgery and chemotherapy, the 1-year mortality rate was decreased, but the 3-year and 5-year mortality rates were increased. That was to say, our research demonstrated that transplantation remained the optimal treatment choice, but for patients who had received surgery, the systematic chemotherapy was not conducive to the long-term survival. However, this conclusion remains controversial. Several studies had shown that the combination of surgical treatment and chemotherapy was of benefit for patients with HCC12,13. Whereas, neither local14,15 nor systemic16,17,18 chemotherapy studies had been able to show the advantage of adjuvant chemotherapy in the prognosis of HCC patients who had undergone surgery. Therefore, this needs to be studied further, and considers the individual differences and diversity of chemotherapies, as well as the severity of the disease, such as the presence of thrombogenesis and distant metastasis. Considering the different severity of the disease, clinicians were inclined to take different treatments, so we divided the patients into groups according to AJCC stage. The conclusion was broadly consistent with the results obtained by grouping chemotherapy except in the AJCC IV stage. But the contrary result in the AJCC IV stage may be due to the fact that most of the patients at this stage chose the surgery combined with chemotherapy, while very few chose the surgery alone.
Liver resection or transplantation is not appropriate for patients with inferior vena cava thrombosis (IVTT) or portal venous tumor thrombosis (PVTT), but radiotherapy can be a treatment option in order to shrink the vascular thrombus. Researches have shown that the combination of radiotherapy and transcatheter arterial chemoembolization (TACE) was better for patients’ survival than TACE alone19,20,21. However, according to our multivariate analysis, radiotherapy was beneficial to the survival of patients without chemotherapy, while for patients with chemotherapy, radiotherapy had no effect on the overall survival. Besides, the cumulative incidence of death of HCC and other causes were increased for patients when administered radiotherapy in both groups. This result may be due to the fact that our cumulative death probability analysis was univariate, or it may be associated with adverse reactions of radiotherapy, such as radiation-induced liver disease (RILD)22.
Although using population-based data from SEER can reduce selection or treatment biases, we can’t ignore its limitations. First, the data sources were limited to the United States. Different countries could have diverse characteristics of diseases and options of treatments. Second, the SEER database provided only macroscopic information about the treatment, which lacked individual information about it. Additionally, it was a retrospective study. Finally, the database only contained a baseline lacking the dynamic changes in each indicator during follow-up, which led to the limitations of our research.
Method statement
All methods were carried out in accordance with relevant guidelines and regulations.
Change history
31 January 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41598-022-05396-4
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- ICC:
-
Intrahepatic cholangiocarcinoma
- AASLD:
-
The American Association for the Study of Liver Diseases
- RFA:
-
Heat-Radio-Frequency ablation
- PEI:
-
Percutaneous Ethanol Injection
- SEER:
-
The Surveillance, Epidemiology, and End Results
- PSM:
-
Propensity score matching
- OS:
-
Overall survival
- CSS:
-
Cancer-specific survival
- CI:
-
Coincidence interval
- AJCC:
-
American Joint Committee on Cancer (7th)
- HR:
-
Hazard ratio
- COD:
-
Cause of death
- RILD:
-
Radiation-induced liver disease
References
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA 68, 394–424 (2018).
Petrick, J. L. & McGlynn, K. A. The changing epidemiology of primary liver cancer. Curr. Epidemiol. Rep. 6, 104–111 (2019).
Fox, J. Cox proportional-hazards regression for survival data. See Also. 3, 371–372 (2002).
Carmona, R. et al. Improved method to stratify elderly patients with cancer at risk for competing events. J. Clin. Oncol. 34, 1270–1277 (2016).
Pintilie, M. Competing risks: A practical perspective. Technometrics 50, 411 (2008).
Fine, J. P. & Gray, R. J. A proportional hazards model for the subdistribution of a competing risk. J. Am. Stat. Assoc. 94, 496–509 (1999).
Heimbach, J. K. et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 67, 358–380 (2018).
Lin, K. et al. Prognostic models for predicting overall and cancer-specific survival in hepatocellular carcinoma: A competing risk analysis. Res. Square https://doi.org/10.21203/rs.3.rs-46064/v1 (2020).
Oweira, H. et al. Prognostic value of site-specific extra-hepatic disease in hepatocellular carcinoma: A SEER database analysis. Expert. Rev. Gastroenterol. Hepatol. 11, 695–701 (2017).
Liu, H. et al. Does fibrosis have an impact on survival of patients with hepatocellular carcinoma: Evidence from the SEER database?. BMC Cancer 18, 1125 (2018).
Welzel, T. M. et al. Metabolic syndrome increases the risk of primary liver cancer in the United States: A study in the SEER-Medicare database. Hepatology 54, 463–471 (2011).
Liang, L. et al. Adjuvant intraportal venous chemotherapy for patients with hepatocellular carcinoma and portal vein tumor thrombi following hepatectomy plus portal thrombectomy. World J. Surg. 32, 627–631 (2008).
Fukuda, S. et al. Surgical resection combined with chemotherapy for advanced hepatocellular carcinoma with tumor thrombus: Report of 19 cases. Surgery 131, 300–310 (2002).
Kim do, Y. et al. Adjuvant hepatic arterial infusional chemotherapy with 5-fluorouracil and cisplatin after curative resection of hepatocellular carcinoma. Oncology 81, 184–191 (2011).
Lai, E. C., Lo, C. M., Fan, S. T., Liu, C. L. & Wong, J. Postoperative adjuvant chemotherapy after curative resection of hepatocellular carcinoma: A randomized controlled trial. Arch. Surg. 133, 183–188 (1998).
Hasegawa, K. et al. Uracil-tegafur as an adjuvant for hepatocellular carcinoma: A randomized trial. Hepatology 44, 891–895 (2006).
Xia, Y. et al. Adjuvant therapy with capecitabine postpones recurrence of hepatocellular carcinoma after curative resection: A randomized controlled trial. Ann. Surg. Oncol. 17, 3137–3144 (2010).
Yamamoto, M., Arii, S., Sugahara, K. & Tobe, T. Adjuvant oral chemotherapy to prevent recurrence after curative resection for hepatocellular carcinoma. Br. J. Surg. 83, 336–340 (1996).
Koo, J. E. et al. Combination of transarterial chemoembolization and three-dimensional conformal radiotherapy for hepatocellular carcinoma with inferior vena cava tumor thrombus. Int. J. Radiat. Oncol. Biol. Phys. 78, 180–187 (2010).
Feng, M. & Benjosef, E. Radiation therapy for hepatocellular carcinoma. Sem Radiat. Oncol. 21, 271–277 (2011).
Cupino, A. C. et al. Does external beam radiation therapy improve survival following transarterial chemoembolization for unresectable hepatocellular carcinoma?. GCR 5, 13–17 (2012).
Lawrence, T. S. et al. Hepatic toxicity resulting from cancer treatment. Int. J. Radiat. Oncol. Biol. Phys. 31, 1237–1248 (1995).
Latouche, A. et al. A competing risks analysis should report results on all cause-specific hazards and cumulative incidence functions. J. Clin. Epidemiol. 66, 648–653 (2013).
Wolkewitz, M. et al. Interpreting and comparing risks in the presence of competing events. BMJ 349, g5060 (2014).
Jason, C. et al. Local radiotherapy with or without transcatheter arterial chemoembolization for patients with unresectable hepatocellular carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 47, 435–442 (2000).
Ryoko, Y. et al. Impact of alpha-fetoprotein on hepatocellular carcinoma development during entecavir treatment of chronic hepatitis B virus infection. J. Gastroenterol. 50, 785–794 (2015).
Jordi, B. et al. Prognostic factors and predictors of sorafenib benefit in patients with hepatocellular carcinoma: Analysis of two phase III studies. J. Hepatol. 67, 999–1008 (2017).
Acknowledgements
We gratefully acknowledge the Infectious Diseases Department of the Children's Hospital affiliated to Xi'an Jiaotong University for its support. The authors also gratefully acknowledge the assistance from medical writers, proof-readers and editors.
Author information
Authors and Affiliations
Contributions
M.L. Investigation, Project administration, Data curation, Formal analysis, Writing—original draft. M.X. Project administration, Writing—review & editing, Visualization. T.T. Conceptualization, Writing—review & editing, Supervision. M.L. and M.X. contributed equally to this article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: The original version of this Article contained extensive errors in Tables 1, 2, 3 and 5, where column headings were mislabelled and data was listed in the incorrect columns.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, M., Xu, M. & Tang, T. Association between chemotherapy and prognostic factors of survival in hepatocellular carcinoma: a SEER population-based cohort study. Sci Rep 11, 23754 (2021). https://doi.org/10.1038/s41598-021-02698-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-02698-x
This article is cited by
-
Prediction of survival and analysis of prognostic factors for patients with AFP negative hepatocellular carcinoma: a population-based study
BMC Gastroenterology (2024)
-
Construction and validation of a survival prognostic model for stage III hepatocellular carcinoma: a real-world, multicenter clinical study
BMC Gastroenterology (2023)
-
Hepatocellular carcinoma immune prognosis score predicts the clinical outcomes of hepatocellular carcinoma patients receiving immune checkpoint inhibitors
BMC Cancer (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.