Abstract
Spondylodiscitis is a serious and potentially life-threatening disease. Obesity is a risk factor for many infections, and its prevalence is increasing worldwide. Thus, the aim of this study was to describe characteristics of obese patients with spondylodiscitis and identify risk factors for a severe disease course in obese patients. Between December 2012 and June 2018, clinical records were screened for patients admitted for spondylodiscitis. The final analysis included 191 adult patients (mean age 64.6 ± 14.8 years). Patient data concerning demographics, comorbidities, surgical treatment, laboratory testing, and microbiological workup were analysed using an electronic database. Patients were grouped according to body mass index (BMI) as BMI ≥ 30 kg/m2 or < 30 kg/m2. Seventy-seven patients were classified as normal weight (BMI 18.5–24.9 kg/m2), 65 as preobese (BMI 25–29.9 kg/m2), and 49 as obese (BMI ≥ 30 kg/m2). Obese patients were younger, had a higher revision surgery rate, and showed higher rates of abscesses, neurological failure, and postoperative complications. A different bacterial spectrum dominated by staphylococci species was revealed (p = 0.019). Obese patients with diabetes mellitus had a significantly higher risk for spondylodiscitis (p = 0.002). The mortality rate was similar in both cohorts, as was the spondylodiscitis localisation. Obesity, especially when combined with diabetes mellitus, is associated with a higher proportion of Staphylococcus aureus infections and is a risk factor for a severe course of spondylodiscitis, including higher revision rates and sepsis, especially in younger patients.
Similar content being viewed by others
Introduction
Spondylodiscitis is a severe and potentially life-threatening disease which continues to be a problem worldwide1,2,3. Patients present with a wide range of clinical symptoms, making diagnosis difficult. Therapy requires prompt and aggressive medical treatment, including proof of germs and surgical therapy, if necessary3.
Obesity is a major worldwide health problem that is associated with decreased life expectancy. Furthermore, obesity is known to be a risk factor for surgical site infection and poor outcomes in polytrauma patients4,5.
As the prevalence of both spondylodiscitis and obesity are increasing, it is of great interest to identify risk factors and develop treatment paths to improve treatment options and outcomes for patient in this cohort. The aim of this study was to describe characteristics of obese patients with spondylodiscitis and identify risk factors for a severe disease course in obese patients.
Epidemiology
Spondylodiscitis
Pyogenic spondylodiscitis used to be a rare disease, with an incidence of 0.4–2 cases per 100,000 patients each year; however, it has increased in recent decades to 5.8 cases per 100,000 patients in Denmark1 and 7.4 cases per 100,000 patients in Japan, which is an increase of 140%2. This has been attributed to the higher life expectancy of patients with chronic debilitating diseases3,8,9,10. It is more common in elderly patients, with a peak between 59 and 69 years of age, and there is a male preponderance of 52–69%6,7,8, which is further increased in elderly populations1,2. In the current literature, the overall mortality of spondylodiscitis lies between 4.5 and 11%2,9,10,11. The predisposing factors include diabetes mellitus, immunosuppression, intravenous drug use, HIV infection, spinal surgery and dorsal instrumentation, preceding bacteraemia, the presence of intravascular devices, rheumatoid arthritis, and malnutrition1,2,12,13,14,15. The prevalence of risk factors in large studies (n > 100) vary widely, for example, diabetes mellitus and intravenous drug abuse were found to be 10–37% and 2–79%, respectively1,2,12,13. Furthermore, the outcome is significantly worsened when patients present with neurologic compromise, delayed time to diagnosis, or suffer a hospital-acquired infection9. Compared to other diseases, spondylodiscitis in obese patients is not well described. Accordingly, although potential risk factors have been identified, their impact remains unclear.
Obesity
Obesity is classified according to body mass index (BMI), which is divided into six different categories (see Table 1). Obesity is an increasing worldwide health concern because excess weight gain is associated with an increased risk for several diseases, most notably cardiovascular disease, diabetes, and cancer16,17. Obese patients show higher mortality after blunt trauma and have a higher risk of multiple organ failure after severe trauma4,18. According to Keaver et al.19, the percentage of overweight and obese individuals in England and Ireland by 2030 is proposed to reach 89% and 85% in males and females, respectively, by 2030. By then, obesity is expected to affect 86% of adults in the US20. This rise in obesity prevalence has been estimated to lead to an increase in obesity-related coronary heart disease, cancers, and type-2 diabetes mellitus of 97%, 61%, and 21%, respectively19. Obesity is associated with decreased life expectancy of approximately 3.3–18.7 years21,22. It is known to be a risk factor for surgical site infection in joint arthroplasty and abdominal surgery5,23. Additionally, obesity represents an increasing economic burden24.
Pathogens and pathophysiology
In terms of aetiology, spinal infections can be divided into pyogenic, granulomatous (TBC, Brucella, fungal), and parasitic infections8. Pyogenic and granulomatous spinal infections each make up almost 50% of all spinal infections, whereas parasitic spinal infections are rare7. Spondylodiscitis commonly arises from the hematogenous spread of bacteria; the arterial route is more frequent than the venous route25.
Staphylococcus aureus (29–39%) and streptococci (19%)7,26 are the most common microorganisms encountered. The proportion of gram-negative bacteria (mostly Escherichia coli) varies between 15 and 39%7,27,28,29.
Materials and methods
Data source
The study was conducted at a large university medical center located in central Europe. The hospital is a 1600-bed tertiary care provider hosting in-house departments for medical microbiology and pathology. All methods were conducted in accordance with relevant guidelines and regulations. All experimental protocols were reviewed and approved by the Ethics Committee of the University Medical Center Hamburg-Eppendorf (Hamburg Medical Chamber, Aerztekammer Hamburg; WF-013/20). Informed consent was obtained from all subjects to be included in our prospective database on spondylodiscitis. The evaluation was then carried out as a retrospective analysis of all cases between 2013 and 2018 according to regulations of the Ethics Committee of the University Medical Center Hamburg-Eppendorf.
The manuscript was written following the STROBE guidelines30.
Patient data
The included patients were treated in the division of spine surgery in the department of trauma and orthopaedic surgery. In line with the retrospective study design, clinical records were screened for patients admitted for spondylodiscitis between December 2012 and June 2018.
Patient data concerning demographics, comorbidities, surgical treatment, laboratory testing, and microbiological workup were recorded and analysed using an electronic database. Patients with spondylodiscitis following previous spine surgery were excluded from the study.
Therapy strategy and approach
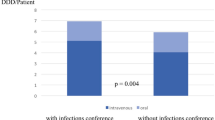
We took a multidisciplinary approach involving spine surgeons, microbiologists, and infectious disease specialists. The diagnostic approach included clinical history and physical examination, lab values including C-reactive protein (CRP) levels, white blood cell (WBC) counts, native radiographs, and full spine contrast-enhanced magnetic resonance imaging (MRI) or computer tomography (positron emission tomography [PET-CT]) when MRI was contraindicated. Serial blood cultures were collected from 185 patients (87.3%). Also, transoesophageal echography was performed in 147 patients (69.3%). All patients received intravenous antibiotics followed by an oral course. Anti-infectious treatment was conducted individually for 6 to 12 weeks (mostly intravenous for 14 days followed by an oral course) following the recommendation of our in-house multidisciplinary infections conference. Patients were stratified into a “normal and preobese” group (NWG; BMI of 20–30 kg/m2) and an “obese” group (OG; BMI of > 30 kg/m2) for risk analysis. Patients with a BMI below 18.5 kg/m2 were excluded from the risk analyses due to the low number of patients affected (n = 7). Surgery was performed by four experienced surgeons from the spine surgery team. Surgical treatment, either minimally invasive or conventional/open, depended on the decision of the team. For emergency cases that required surgery during the night shift, the surgeon in charge made the decisions. The patients included were scheduled for surgical treatment due to neurological deficits, septic disease with organ failure or the beginning of organ failure, spinal instability because of major spinal destruction, immobilising back pain, or the failure to respond to adequate conservative treatment including adapted analgesia, physiotherapy, and antibiotic therapy adapted to the spectrum of bacteria. Open surgical treatment was primarily performed, but minimally invasive percutaneous instrumentation was used as an alternative. Radiological guided biopsies were only performed in 20 cases.
Statistics
Datasets were analysed by Student’s t-test, cross tables, and chi-square tests using IBM SPSS V 25 (IBM, Armonk, NY, USA) and Microsoft Excel (Microsoft).
Odds ratios (OR) were computed for all 2 × 2 crosstabulations with chi-square tests for statistical significance in binary coded variables. Non-parametric data was analysed using Kruskall–Wallis and Mann–Whitney-U test. P-values of 0.05 or less were considered significant.
Results
Demographics
We identified a total of 212 patients with spondylodiscitis (n = 140, 66% male), aged 64.6 ± 14.8 years. Body weight and body length records were incomplete for 14 patients, so these patients were excluded. Of the remaining 198 patients, 7 were underweight (3.5%), 77 were normal weight (38.9%) and 65 were preobese (32.8%). Among the patients with obesity, 26 were classified as class I (13.1%), 13 as class II (6.6%), and 10 as class III (5.1%), according to the World Health Organization (Fig. 1). The underweight patients were excluded as this represents a disease of its own. Final analysis was performed for the remaining 191 patients.
The mean duration of hospital stay was 27.2 ± 20.7 days, and the mean stay in the intensive care unit (ICU) was 7.3 ± 15.1 days. The mean BMI was 26.9 ± 7.0 kg/m2. When comparing the groups, there was no significant difference in the duration of hospital stay (NWG 24.8 ± 15.3; OG 28.6 ± 18.4; p = 0.2). The ICU stay was longer for obese patients, but this difference was not significant (NWG 6.6 ± 13.4, OG 7.0 ± 12.1; p = 0.2; Table 2).
Localisation
Spondylodiscitis was localised in the cervical spine in 31 patients (16.2%), in the thoracic spine in 43 patients (22.5%), in the lumbar spine in 101 patients (52.9%), and in a disseminated location in 16 patients (8.4%).
Clinical findings
The groups did not show any significant differences concerning age, gender distribution, rate of revision surgery, general mortality, patient stay, or localisation (Table 2). Overall, there was a trend towards younger age in patients with diagnosed obesity °I-III compared to patients with normal or pre-obese bodyweight (median 70 vs. 65 years, U = 3084.5, Z = − 1183, p = 0.237, Mann–Whitney-U test). In a more detailed analysis of the WHO subgroups using one-way ANOVA and Kruskall-Wallis test, mean age for those groups was: Underweight: 56 years; Normal: 65 years; Preobese: 73 years; Obesity °I: 70 years; Obesity °II: 65 years; Obesity °III 53 years. Kruskall Wallis test showed an effect between patient age and obesity p = 0.044, however this was based solely on the comparison between Preobese and Obesity °III patients p = 0.05 Bonferroni with Dunn’s correction for multiple tests. All other pairwise comparisons were not statistically significant.
Pre-existing conditions were comparable, except for a significantly higher rate of diabetes mellitus in the OG (10.6% for the NWG vs. 28.6% for the OG; p = 0.002). The rates of non-insulin-dependent diabetes mellitus (NIDDM) were similar between the groups. The OR was 3.387 for obese patients with diabetes versus normal weight patients with diabetes. Hepatitis B occurred significantly more often in the NWG (9.9% for the NWG vs. 0.0% for the OG; p = 0.022; Table 3). There was no difference in mortality rate between the two groups (12% for the NWG vs. 12.2% for the OG p = 0.34). Mortality rates were higher in our tertiary care centre compared to the current literature8,12,26.
There was a slightly higher rate of epidural abscesses in the OG (53.1%) compared to the NWG group (45.1%; p = 0.334), as well as psoas abscesses (26.5% for the OG vs. 19.7% for the NWG group; p = 0.317).
Neurological deficits affected a higher number of obese patients (26.5%, n = 13), compared to NWG (18%, n = 25), but this result was not statistically significant (p = 0.439). In four cases, the loss of function was reversible (one in the OG, three in the NWG) by the time they were discharged from the hospital. Neurological deterioration was only found in two cases in the NWG (none in the OG), most likely due to an individual severe illness course with acute kidney failure followed by sepsis and pneumonia in the second case.
Laboratory findings
Preoperative CRP counts were significantly higher in the OG (142.3 mg/L) compared to the NWG group (113.3 mg/L; reference range of < 5 mg/L; p = 0.038), but there was no significant difference in leukocyte levels between obese patients (10.3 × 109 cells/L) and normal weight patients (11 × 109 cells/L; reference range of 3.8–11 × 109 cells/L; p = 0.925).
Complications
A higher rate of revision surgery was found in the OG (24.5% for the OG [n = 12] vs. 14.1% for the NWG [n = 20]; p = 0.09). Obese patients had a three times higher chance of unplanned revision surgery (OR 2.8, RR 2.2) compared to normal weight patients. Also, patients who required unplanned revision surgery had a higher BMI compared to patients who did not (29.8 and 26.5 kg/m2, respectively). Regarding in-hospital complications, a significant difference and doubled rate of sepsis (16.2% for the NWG vs. 32.7% for the OG, p = 0.01; OR 1.7, RR 1.4) and liver failure (1.4% for the NWG vs. 8.2% for the OG; p = 0.02) was found. There were no other statistically significant differences for any other complication, except for a trend towards cardiac decompensation in the OG (7.0% for the NWG vs. 16.3% for the OG; p = 0.06; Table 4).
Pathogens
Bacteria were isolated from blood cultures in 56.4% of OG patients and 47.2% of NWG patients. Intraoperative samples were positive in 65.5% of the NWG and 57.1% of the OG (p = 0.54). There was a significant difference concerning the isolated bacterial species responsible for spondylodiscitis between the groups. The NWG group presented significantly fewer staphylococcus species (57.6%) than the OG (85.7%; p = 0.019). However, both groups showed the same rates for resistant species (4.5% for the NWG vs. 4.8% for the OG; p = 0.236). All other differences were not significant (Fig. 2).
Treatment
There was no significant difference in the NWG group or the OG in terms of the chosen surgical technique (Table 5). Conservative treatment was carried out in 4.3% of patients in the NWG and 6.1% in the OG. Most patients in the two groups were treated surgically by a posterior approach (40.4% for the NWG vs. 44.9% for the OG; p = 0.511) followed by a posterior-anterior approach (27.0% for the NWG vs. 34.7% for the OG; p = 0.511).
Discussion
Infectious spondylodiscitis is not an uncommon disease, with an increasing prevalence reported in western society in recent decades1,2. The prevalence of obesity has also increased across the world19,20. Accordingly, the correlations and effects of spondylodiscitis and obesity on each other are of considerable interest.
Patient data
Our patient cohort had a mean age of 64.6 years, which is consistent with other studies that identified spondylodiscitis as the main manifestation of hematogenous osteomyelitis in patients older than 50 years of age31,32. In the NWG, the average age was 65.8 years, and the OG had an average age of 63.3 years. It is interesting to note that when only patients with obesity grades 2 and 3 were included, classified according to the World Health Organization, the average age was 59.7 years, and when grade 3 alone was considered, the average age was only 54.8 years. These patients still belong to the over 50 age group, but they are noticeably younger than normal weight patients who suffered spondylodiscitis.
Clinical and laboratory findings
Preoperative CRP counts were significantly higher in the OG compared to the NWG group. Unexpectedly, although not significant, obese patients showed lower leukocyte levels than normal weight patients, which is in contrast to common findings concerning the impact of obesity on immunity. Thus, the underlying reason remains unclear33.
In our cohort, obese patients showed a higher rate of epidural abscess (53.1%) compared to the NWG group (45.1%), as well as psoas abscess (26.5% and 19.7%, respectively). Consequently, obese patients had a higher rate of neurological dysfunction (26.5%, n = 13), whereas only 18% of the NWG showed neurological dysfunction. In four cases, the loss of function was reversible (one in the OG, three in the NWG) by the time of discharge from the hospital. The rates of the NWG were comparable to former studies9,26,34, but the rates in the OG were noticeably higher.
Additionally, we found a trend toward a higher rate of revision surgery in the OG (OG 25% vs. NWG 14.1%; p = 0.08; OR 2.8, RR 2.2). Also, patients who underwent unplanned revision surgery had a higher BMI compared to those who did not (29.8 and 26.5 kg/m2, respectively), which is similar to the results observed for arthroplasty surgery35.
In our study, most patients with pyogenic spondylodiscitis suffered from concomitant diseases. The most common and significant in our study were diabetes mellitus (28.6%) in the OG and hepatitis B (9.9%) in the NWG. In accordance with former studies, diabetes mellitus, renal insufficiency, and cardiac diseases are the most frequent concomitant diseases in patients with spondylodiscitis36. In our cohort, we found an equal occurrence of NIDDM in the NWG and OG groups, and there was no significant difference for renal insufficiency (NWG 16.2%, OG 24.5%; p = 0.196; OR 1.687). In our data, we found a trend but no significant difference in cardiac disease prevalence (NWG 13.4%, OG 24.5%; p = 0.069; OR 2.1). When compared to data from a primary care study addressing the subject of obesity and diabetes, the present collective shows comparable results. Bramlage et al. reported an OR of 1.67 (1.54–1.81) for the overweight population (BMI 25– < 30) and an OR of 3.52 (3.23–3.83) for the obese population (BMI > 30), which are similar to the results of the present study, with an OR of 3.387 (1.493–7.680, p = 0.002) for obese patients37.
Mortality rates were higher in our tertiary care centre compared to the current literature due to a higher than average number of patients living with heavy pre-existing diseases in our center (ASA score > 3)8,12,26. Another explanation might be related to the high proportion of inpatient transfers from other spine centers (99/191 = 52%) where no care was possible due to the severity of the disease or where conservative therapy had failed.
Pathogens
With regard to pathogens isolated from blood cultures, 56.4% of patients in the OG and 47.2% in the NWG showed positive samples. Perioperative samples were positive in 65.5% of the NWG and 57.1% of the OG. These results are comparable to former studies15,36.
Significantly different bacteria were isolated in both groups. Previous studies demonstrated that staphylococci species are the main pathogens responsible for spondylodiscitis, followed by streptococci and Enterobacteriaceae32,36,38. In the OG, staphylococci represented almost 86% (57.6% of the NWG) of all infections, followed by Enterobacteriaceae (9.5%). This greatly outperforms rates reported in the current literature7,26. We do not know the underlying reason for the high incidence of staphylococcus species that caused spondylodiscitis in obese patients. Coincidentally, Pseudomonas aeruginosa, an uncommon cause of pyogenic spondylodiscitis, was isolated in 48% of 61 patients who reported intravenous drug use39. Most likely, obesity together with recurring lesions in skin folds creates a favourable environment for staphylococci infection as intravenous drug use does for Pseudomonas aeruginosa.
Complications
Significant rates of in-hospital complications were found for liver failure and sepsis in obese patients with spondylodiscitis.
Localisation
No difference concerning localisation was seen between the obese and normal weight cohort, with a similar distribution for lumbar, thoracic, and cervical spondylodiscitis (Table 2) compared to current data40.
Surgical treatment
Bodyweight had no impact on the surgical approach chosen for treatment; however, it is commonly understood that surgery on obese patients is highly challenging. It is of great importance that the ideal therapy is not denied to the patient due to obesity. To our knowledge, there are no further data regarding whether obesity is a limiting factor in spinal surgery.
Limitations
The limitations of this study include its single-center retrospective study design and that a relatively high number of patients (n = 21/212; 10%) were excluded due to a lack of information in our electronic database or an underweight body mass index.
Conclusion
Obese patients have significantly higher rates of postoperative liver failure and sepsis compared to normal weight patients. There were higher rates of revision surgery and cardiac decompensation in the obese group, but they were not statistically significant.
Abscesses occurred more often in the obese group, but also not statistically significant. Obese patients are younger than normal weight patients when they suffer from spondylodiscitis. Obese patients suffering from diabetes represent a special risk profile for spondylodiscitis. Obese patients demonstrate a unique bacterial spectrum compared to normal weight patients.
Obese patients do not have a higher mortality rate than normal weight patients with spondylodiscitis. Summarised, obese patients show a more severe course of spondylodiscitis, but we were unable to completely substantiate these presumptions as the length of hospital stay and mortality rate were similar between the two groups. As both obesity and spondylodiscitis have increased over the past couple of decades, it is necessary to focus more attention on this patient cohort.
References
Kehrer, M., Pedersen, C., Jensen, T. G. & Lassen, A. T. Increasing incidence of pyogenic spondylodiscitis: a 14-year population-based study. J. Infect. 68, 313–320 (2014).
Akiyama, T. et al. Incidence and risk factors for mortality of vertebral osteomyelitis: a retrospective analysis using the japanese diagnosis procedure combination database. BMJ Open 3, 1 (2013).
Valancius, K. et al. Failure modes in conservative and surgical management of infectious spondylodiscitis. Eur. Spine J. 22, 1837–1844 (2013).
Neville, A. L., Brown, C. V. R., Weng, J., Demetriades, D. & Velmahos, G. C. Obesity is an independent risk factor of mortality in severely injured blunt trauma patients. Arch. Surg. 139, 983–987 (2004).
Winfield, R. D., Reese, S., Bochicchio, K., Mazuski, J. E. & Bochicchio, G. V. Obesity and the risk for surgical site infection in abdominal surgery. in American Surgeon vol. 82 331–336 (Southeastern Surgical Congress, 2016).
Nickerson, E. K. & Sinha, R. Vertebral osteomyelitis in adults: an update. Br. Med. Bull. 117, 121–138 (2016).
Nolla, J. M. et al. Spontaneous pyogenic vertebral osteomyelitis in nondrug users. Semin. Arthritis Rheum. 31, 271–278 (2002).
Hadjipavlou, A. G., Mader, J. T., Necessary, J. T. & Muffoletto, A. J. Hematogenous pyogenic spinal infections and their surgical management. Spine (Phila. Pa. 1976) 25, 1668–1679 (2000).
McHenry, M. C., Easley, K. A. & Locker, G. A. Vertebral osteomyelitis: long-term outcome for 253 patients from 7 Cleveland-area hospitals. Clin. Infect. Dis. An Off. Publ. Infect. Dis. Soc. Am. 34, 1342–1350 (2002).
Pigrau, C. et al. Spontaneous pyogenic vertebral osteomyelitis and endocarditis: incidence, risk factors, and outcome. Am. J. Med. 118, 1287 (2005).
Waheed, G., Soliman, M. A. R., Ali, A. M. & Aly, M. H. Spontaneous spondylodiscitis: review, incidence, management, and clinical outcome in 44 patients. Neurosurg. Focus 46, E10 (2019).
Loibl, M. et al. Outcome-related co-factors in 105 cases of vertebral osteomyelitis in a tertiary care hospital. Infection 42, 503–510 (2014).
Urrutia, J., Zamora, T. & Campos, M. Cervical pyogenic spinal infections: are they more severe diseases than infections in other vertebral locations?. Eur. Spine J. 22, 2815–2820 (2013).
Corrah, T. W., Enoch, D. A., Aliyu, S. H. & Lever, A. M. Bacteraemia and subsequent vertebral osteomyelitis: a retrospective review of 125 patients. QJM 104, 201–207 (2011).
Mylona, E., Samarkos, M., Kakalou, E., Fanourgiakis, P. & Skoutelis, A. Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin. Arthritis Rheum. 39, 10–17 (2009).
Wang, Y. C., McPherson, K., Marsh, T., Gortmaker, S. L. & Brown, M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet (London, England) 378, 815–825 (2011).
Tilg, H. & Moschen, A. R. Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat. Rev. Immunol. 6, 772–783 (2006).
Ciesla, D. J. et al. Obesity increases risk of organ failure after severe trauma. J. Am. Coll. Surg. 203, 539–545 (2006).
Keaver, L. et al. Application of the UK Foresight Obesity Model in Ireland: The Health and Economic consequences of projected obesity trends in Ireland. PLoS ONE 8, e79827 (2013).
Ginter, E. & Simko, V. Becoming overweight: is there a health risk?. Bratisl. Lek. Listy 115, 527–531 (2014).
Leung, M.-Y.M., Pollack, L. M., Colditz, G. A. & Chang, S.-H. Life years lost and lifetime health care expenditures associated with diabetes in the US, National Health Interview Survey, 1997–2000. Diabetes Care 38, 460–468 (2015).
Baier, C. et al. Incidence and risk factors of surgical site infection after total knee arthroplasty: results of a retrospective cohort study. Am. J. Infect. Control https://doi.org/10.1016/j.ajic.2019.04.010 (2019).
Kunutsor, S. K., Whitehouse, M. R., Blom, A. W. & Beswick, A. D. Patient-related risk factors for periprosthetic joint infection after total joint arthroplasty: a systematic review and meta-analysis. PLoS ONE 11, e0150866 (2016).
Rtveladze, K. et al. Obesity prevalence in Mexico: impact on health and economic burden. Public Health Nutr. 17, 233–239 (2014).
Ratcliffe, J. F. Anatomic basis for the pathogenesis and radiologic features of vertebral osteomyelitis and its differentiation from childhood discitis. A microarteriographic investigation. Acta Radiol. Diagn. (Stockh.) 26, 137–143 (2020).
Cebrián Parra, J. L. et al. Management of infectious discitis. Outcome in one hundred and eight patients in a University Hospital. Int. Orthop. 36, 239–244 (2012).
Kim, C.-J. et al. A comparative study of pyogenic and tuberculous spondylodiscitis. Spine (Phila. Pa. 1976) 35, E1096-1100 (2010).
Perronne, C. et al. Pyogenic and tuberculous spondylodiskitis (vertebral osteomyelitis) in 80 adult patients. Clin. Infect. Dis. An Off. Publ. Infect. Dis. Soc. Am. 19, 746–750 (1994).
Graham, S. M., Fishlock, A., Millner, P. & Sandoe, J. The management gram-negative bacterial haematogenous vertebral osteomyelitis: a case series of diagnosis, treatment and therapeutic outcomes. Eur. Spine J. Off. Publ. Eur. Spine Soc. Eur. Spinal Deform. Soc. Eur. Sect. Cerv. Spine Res. Soc. 22, 1845–1853 (2013).
Von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann. Intern. Med. 147, 573–577 (2007).
Jensen, A. G., Espersen, F., Skinhøj, P., Rosdahl, V. T. & Frimodt-Møller, N. Increasing frequency of vertebral osteomyelitis following Staphylococcus aureus bacteraemia in Denmark 1980–1990. J. Infect. 34, 113–118 (1997).
Espersen, F., Frimodt-Møller, N., Thamdrup Rosdahl, V., Skinhøj, P. & Bentzon, M. W. Changing pattern of bone and joint infections due to Staphylococcus aureus: study of cases of bacteremia in Denmark, 1959–1988. Rev. Infect. Dis. 13, 347–358 (2020).
Andersen, C. J., Murphy, K. E. & Fernandez, M. L. Impact of obesity and metabolic syndrome on immunity. Adv. Nutr. 7, 66–75 (2016).
Eismont, F. J., Bohlman, H. H., Soni, P. L., Goldberg, V. M. & Freehafer, A. A. Pyogenic and fungal vertebral osteomyelitis with paralysis. J. Bone Joint Surg. Am. 65, 19–29 (1983).
Sisko, Z. W. et al. Morbid obesity in revision total knee arthroplasty: a significant risk factor for re-operation. J. Arthroplasty 34, 932–938 (2019).
Pola, E. et al. Multidisciplinary management of pyogenic spondylodiscitis: epidemiological and clinical features, prognostic factors and long-term outcomes in 207 patients. Eur. Spine J. 27, 229–236 (2018).
Bramlage, P. et al. Recognition and management of overweight and obesity in primary care in Germany. Int. J. Obes. 28, 1299–1308 (2004).
Mavrogenis, A. F. et al. Spondylodiscitis revisited. EFORT Open Rev. 2, 447–461 (2017).
Patzakis, M. J., Rao, S., Wilkins, J., Moore, T. M. & Harvey, P. J. Analysis of 61 cases of vertebral osteomyelitis. Clin. Orthop. Relat. Res. https://doi.org/10.1097/00003086-199103000-00019 (1991).
Gentile, L. et al. A systematic review: characteristics, complications and treatment of spondylodiscitis. Eur. Rev. Med. Pharmacol. Sci. 23, 117–128 (2019).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
B.S. wrote the main manuscript text and prepared figures and tables. Data was collected by B.S., M.S., D.T. Statistic analysis was performed by B.S., K.M. and D.T. The manuscript was reviewed carefully by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schoof, B., Stangenberg, M., Mende, K.C. et al. Obesity in spontaneous spondylodiscitis: a relevant risk factor for severe disease courses. Sci Rep 10, 21919 (2020). https://doi.org/10.1038/s41598-020-79012-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-79012-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.