Abstract
The purpose of this study was to investigate the changes in patient subjective happiness and satisfaction with cataract surgery and evaluate the association between satisfaction and types of cataract. This study surveyed 247 participants (mean age, 67.9 years) and they completed questionnaires on their satisfaction with the surgery, the subjective happiness scale (SHS) and the Pittsburgh Sleep Quality Index (PSQI) before and after surgery. The SHS increased postoperatively from 4.6 ± 0.7 to 4.8 ± 0.7 (P = 0.007) and 83.4% of patients were satisfied with the surgical results and the average satisfaction score was 4.2 out of a possible 5.0. Multiple regression analysis showed that patient satisfaction was significantly associated with the postoperative SHS (β = 0.380; P < 0.001), the postoperative PSQI (β = −0.041; P = 0.035) and the presence of a posterior subcapsular cataract (PSC) (β = 0.277; P = 0.026). This study clarified that cataract surgery may improve both visual function and patient happiness and that patient satisfaction was affected by postoperative sleep quality and the disappearance of a PSC.
Similar content being viewed by others
Cataracts are common in elderly individuals, and surgery is indicated in most cases. Several studies have reported that cataract surgery improves not only the visual function but also the patients’ quality of life (QOL). Previous studies have reported that the risk of falls decreased after cataract surgery1,2,3 and that cataract surgery can improve postural stability and mobility4,5. Another study reported improvements in the QOL, cognition, and depression after cataract surgery6. We evaluated changes in the sleep quality and gait speed before and after cataract surgery and reported that surgery effectively improved sleep quality and slow gaid speed7. Therefore, cataract surgery can improve the patients’ lives.
Recent psychology research has indicated that happiness has become an important goal for many people8, and positive emotions are highly beneficial for physical and mental health9,10,11,12,13. In Ophthalmology, Kawashima et al. reported an association between subjective happiness and dry eye disease14. Matsuguma et al. evaluated the relationship between subjective happiness and laser-assisted in situ keratomileusis15 and visual impairment16. A recent review reported that positive affective states, including happiness, may contribute to sleep17. As mentioned previously, using the Pittsburgh Sleep Quality Index (PSQI), we found that cataract surgery effectively improved sleep quality and that the PSQI improved significantly in patients with a posterior subcapsular cataract (PSC)18. Considering these findings, we assumed that the patient subjective happiness and sleep quality also may be better postoperatively. Feeny et al. showed that in Vietnam cataract surgery provided benefits that included significant improvements in earnings, mobility, self-care, ability to undertake daily activities, self-assessed health and mental health, life satisfaction, hope, and self-efficacy19.
In the current study, we investigated the changes in the patient subjective happiness before and after cataract surgery and surgical satisfaction in Japan and the association between subjective happiness, satisfaction, and cataract-related factors by evaluating the types and severity of cataracts.
Results
Results of ocular examinations and questionnaires
During the study, 261 patients underwent cataract surgery and 14 were excluded. The 247 remaining patients (99 men, 148 women; mean age, 67.9 ± 11.4 years; range, 32–92 years) were evaluated. Seventy-four patients underwent unilateral surgery and 173 underwent bilateral surgeries. Fifty-six patients of undergoing unilateral surgery were the first-eye surgery and 18 patients were second-eye surgery. There were not any complications including posterior capsule rupture.
The preoperative and postoperative results of ocular examinations and questionnaires are summarized in Table 1. The postoperative SHS increased significantly (P = 0.007) from 4.6 ± 0.7 to 4.8 ± 0.7. The average satisfaction score was 4.2 ± 0.9; 83.4% of patients were satisfied with the surgery (very satisfied, n = 108; satisfied, n = 98). The postoperative CDVA, UDVA, and PSQI were significantly better than the preoperative values (CDVA and UDVA, P < 0.001 for both comparisons; PSQI, P = 0.009).
There are not significant differences between first-eye surgery group and second-eye surgery group in unilateral surgery patients about satisfaction score, change in SHS and PSQI (Table 2).
The numbers of patients with nuclear opalescence (≥ grade 3), cortical cataract, and PSC were 54, 71, and 54, respectively. The presence of nuclear opalescence was significantly (P = 0.035) more prevalent in women than men (P = 0.035), and their refractive error was significantly (P < 0.01) more myopic than the patients without nuclear opalescence (− 4.79 ± 6.11 diopters and − 1.37 ± 3.80 diopters, respectively).
Factors associated with subjective happiness
Table 3 shows the factors associated with the preoperative SHS results. The presence of nuclear opalescence (≥ grade 3) (β = 0.276; P = 0.017) and the preoperative CDVA (β = −0.248; P = 0.008) significantly affected the patient happiness before cataract surgery. Table 4 shows the factors associated with the postoperative SHS results, then the postoperative SHS was associated significantly (β = 0.334; P < 0.001) with the preoperative SHS. The satisfaction score was significantly (β = 0.169; P = 0.005) associated with the changes in the SHS (Table 5).
Factors affecting surgical satisfaction
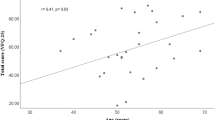
The correlations between patient satisfaction and the postoperative SHS, changes in the SHS, and postoperative PSQI are shown in Fig. 1 respectively. Patient satisfaction was correlated significantly with the postoperative SHS (r = 0.324, P < 0.001) (Fig. 1a), changes in the SHS (r = 0.157, P = 0.013) (Fig. 1b) and postoperative PSQI (r = −0.144, P = 0.024) (Fig. 1c).
The Correlation Between Patient Satisfaction and Postoperative Subjective Happiness Scale (SHS)/Changes in SHS/Pittsburgh Sleep Quality Index (PSQI). (a) The patient satisfaction is correlated significantly with the postoperative SHS score (r = 0.324, P < 0.001). (b) The patient satisfaction is correlated significantly with the changes in the SHS score (r = 0.157, P = 0.013). (c) The patient satisfaction is correlated significantly with the postoperative PSQI score (r = −0.144, P = 0.024).
Multiple regression analysis showed that the postoperative SHS (β = 0.380; P < 0.001), the postoperative PSQI (β = −0.041; P = 0.035) and the presence of a PSC (β = 0.277; P = 0.026) significantly affected the patient surgical satisfaction (Table 6). The patient satisfaction scores with or without a PSC were 4.50 ± 0.76 and 4.14 ± 0.86, respectively, and the score of patients with a PSC was higher significantly (P = 0.004) than without a PSC (Fig. 2a). The postoperative PSQI scores with and without a PSC were 4.02 ± 2.44 and 5.04 ± 2.70, respectively (P = 0.010) (Fig. 2b).
Patient Satisfaction and Postoperative Pittsburgh Sleep Quality Index (PSQI) Scores with and without a Posterior Subcapsular Cataract (PSC). (a) The patient satisfaction scores with and without a PSC are 4.50 ± 0.76 and 4.14 ± 0.86, respectively, and the mean score of patients with a PSC is significantly (P = 0.004) higher than without a PSC. (b) The postoperative PSQI scores with and without a PSC are 4.02 ± 2.44 and 5.04 ± 2.70, respectively. The score of patients with a PSC is significantly (P = 0.010) better than without a PSC.
Discussion
The current study was the first to investigate the effect of cataract surgery on patient subjective happiness and the relationship between patient surgical satisfaction and subjective happiness. We found that cataract surgery improved both the visual function and the patient subjective happiness postoperatively.
Using the SHS, Kawashima et al.14 evaluated the subjective happiness of office workers with subjective and/or objective dry eye symptoms. That study reported that the mean SHS score among patients with subjective and objective dry eye symptoms was 4.87 ± 1.00. A previous study reported that the mean SHS in a sample of healthy Japanese college students was 4.68 ± 1.0520. In the current study, the preoperative SHS score of patients with cataract was 4.64 ± 0.73; nevertheless, Shimai et al. reported that the SHS score had been increasing continuously in patients over 50 years old in Japan and the mean SHS score among 60- to 65-year-olds was 4.83 ± 0.9921. For these reasons, the results of the current study indicated that declines in visual function resulting from the presence of cataracts have a negative effect on patient happiness.
In the current study, the disappearance of a PSC and improved sleep quality were associated with the patient surgical satisfaction. We previously reported correlations between subjective sleep quality and cataract surgery, especially that patients with a PSC achieved the greatest improvement in subjective sleep quality measured using the PSQI18. Cataracts increase the intraocular light scattering and thereby reduce the retinal image contrast22,23. Previous studies have reported that PSC especially causes reduced contrast sensitivity23,24 and objective glare disability is more commonly associated with PSC than with other cataract types25. In addition, patients with a PSC had considerably impaired visual function and the self-reported visual satisfaction was significantly lower than with the other cataract types26. Therefore, it is reasonable to speculate that patients with a PSC had impaired vision with reduced contrast sensitivity and glare disability and had great surgical satisfaction because their preoperative discomfort improved after cataract surgery.
Many previous studies have evaluated sleep quality before and after cataract surgery; two meta-analyses27,28 showed that cataract surgery significantly improved the PSQI score-derived subjective sleep quality irrespective of the intraocular lens (IOL) type implanted. The current study confirmed that sleep quality improved significantly after cataract surgery and further confirmed the association between the improvement and patient satisfaction.
Interestingly, we also found that the preoperative SHS score was associated with poor VA and the presence of nuclear opalescence. The patients with poor VA had a lower SHS score, and those with nuclear opalescence had a higher SHS score. More women than men were among those with nuclear opalescence. Shimai et al. reported that the SHS scores of women were higher than those of men20,21. The current results agree with those of previous studies. In addition, refractive error of the patients with nuclear opalescence in this study was more myopic than the patients without nuclear opalescence. We speculated that better near vision in myopic patients with nuclear opalescence may account for their higher SHS score compared with patients without nuclear opalescence.
The current study had some limitations. First, we could not collect additional data that might have affected subjective happiness, such as income or marital status. We inferred that the patients with nuclear opalescence may have elements that made them happier than those without nuclear opalescence. Second, we did not evaluate the improvement of symptoms such as glare or haloes. We should have assessed these points with questionnaire, glare testing and low contrast visual acuity testing, because these factors possibly affected the patient’s daily life. Third, the study included some biases because it was conducted in one hospital and two clinics in an urban area. Fourth, the patients’ happiness may change over time, considering the set-point theory of happiness29. We should follow these patients for longer periods, such as 6 months or 1 year. Finally, this study was conducted in a mixed sample that included two types of IOLs (a clear ultraviolet light-filtering IOL and a yellow blue light-filtering IOL) and unilateral/bilateral cataracts.
Methods
Study design and study population
The study participants were patients who underwent cataract surgery at Todoroki Eye Clinic, Tokyo, Japan, Minatomirai Eye Clinic, Kanagawa, Japan, and Keio University Hospital, Tokyo, Japan, between June 2016 and June 2018. The subjects completed questionnaires that measured their subjective happiness within 1 month before and after surgery and their satisfaction 1 month with surgery.
Patients were excluded who were younger than 20 years, did not answer all questions, and Took a psychotropic drug. The Institutional Review Board of Keio University School of Medicine approved the research protocol, and the study was conducted in accordance with the tenets of the 1995 Declaration of Helsinki. All participants were provided informed consent.
Ocular examinations
All participants underwent preoperative and postoperative ocular examinations that included measurement of the uncorrected distance visual acuity (UDVA), corrected distance VA (CDVA), and spherical equivalent (SE) by an orthoptist. The SE is a commonly used to express the refractive error by algebraically adding half the cylindrical power to the spherical power. Three experienced ophthalmologists who performed the cataract surgeries evaluated the types and severity of the cataracts by slit-lamp biomicroscopy under maximal pupillary dilation. The types of cataracts were classified according to the Lens Opacities Classification System III30 as nuclear opalescence grade 3 or higher, cortical cataracts disrupting the visual axis, and PSCs. Nuclear opalescence was graded by comparing the color slit-lamp image to be graded with the standard nuclear images (standards 1–6)30. A cortical cataract is visualized in retroillumination images focused either anteriorly or posteriorly30. Only posteriorly focused retroillumination images are used in grading PSC30.
Surgical technique
All surgeons underwent phacoemulsification and aspiration. The selection of anesthesia during surgery, two of them underwent with only topical anesthesia (oxybuprocaine hydrochloride and lidocaine hydrochloride 4.0%) and another clinic underwent both topical anesthesia and intracameral anesthesia (lidocaine hydrochloride 0.5%). After the surgery, two medical institutions prescribed three ophthalmic solutions (levofloxacin hydrate 1.5%, betamethasone sodium phosphate 0.1% and bromfenac sodium hydrate 0.1% or moxifloxacin hydrochloride 0.5%, betamethasone sodium phosphate 0.1% and diclofenac sodium ophthalmic solution 0.1%) for postoperative medication. Another clinic prescribed two ophthalmic solutions (moxifloxacin hydrochloride 0.5% and bromfenac sodium hydrate 0.1%) and add a corticosteroid ophthalmic solution (betamethasone sodium phosphate fradiomycin sulfate) in case the patient has severe inflammation after the surgery.
Subjective happiness scale
Regarding the outcome measures, subjective happiness was measured using the validated Japanese version of the Subjective Happiness Scale (SHS)20 originally developed by Lyubomirsky (eTable 1)31. The scale is a four-item questionnaire of subjective global happiness; each item requires patients to rate the statements on a 7-point Likert scale. The possible scores range from 1 to 7, and higher values corresponded to higher subjective happiness. The overall SHS score was calculated by calculating the mean of the responses to the four items. Both the internal consistency (α = 0.80 for men; α = 0.84 for women) and test–retest reliability (r = 0.86) over 5 weeks were scientifically sound31.
Satisfaction score
We also evaluated the patient postoperative satisfaction using the original questionnaire. The questionnaire used a 5-point Likert scale ranging from 1 (least satisfied) to 5 (very satisfied).
Pittsburgh sleep quality index
The PSQI32, a self-administered questionnaire, is comprised of seven subscales that evaluate sleep quality, including subjective sleep quality, daytime dysfunction, sleep latency, sleep duration, habitual sleep efficacy, sleep disturbances, and use of sleep medications; the score was calculated according to separate algorithms and analyzed. Each component was scored on a scale of 0–3, with 3 indicating the worst score. The highest possible global score is 21, and the normal range on the PSQI is less than 632. We used the validated Japanese version of the PSQI33.
Statistical analysis
If the patient underwent bilateral surgeries, the data from the eye with the better VA were used for all statistical analyses. The VA was converted to the logarithm of the minimum angle of resolution (logMAR). For the statistical analysis of the CDVA and UDCA, counting fingers was categorized as logMAR 2.00 and hand motions as logMAR 3.00, according to the VA conversion chart of the Journal of Cataract & Refractive Surgery.
The differences between the preoperative and postoperative CDVA, UDVA, SE, SHS, and PSQI were analyzed using the Wilcoxon signed-rank test. The differences between first-eye surgery group and second-eye surgery group in unilateral surgery patients were also analyzed using the Wilcoxon signed-rank test.
The correlations were evaluated using the Spearman’s rank correlation test. Multiple regression analysis was performed for potential variables with statistical significance (P < 0.20) in simple correlation to identify the factors affecting the patient satisfaction and happiness with the results of cataract surgery. Multiple regression analysis then was performed to determine the predictors of the SHS score and satisfaction, and possible predictors (sex; age; number of operated eyes; presence of nuclear opalescence, cortical cataract and PSC; and preoperative or postoperative CDVA, UDVA, SHS, and PSQI). P < 0.05 was considered significant. All statistical analyses were performed using SPSS version 25 (SPSS Inc., Chicago, IL).
Conclusions
In summary, the current study showed that cataract surgery may improve not only the visual function but also the patient happiness with surgery. The study also showed that the patient postoperative subjective happiness was associated with surgical satisfaction, and the satisfaction was affected by postoperative sleep quality and the disappearance of a PSC.
References
Harwood, R. H. et al. Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br. J. Ophthalmol. 89, 53–59 (2005).
Desapriya, E., Subzwari, S., Scime-Beltrano, G., Samayawardhena, L. A. & Pike, I. Vision improvement and reduction in falls after expedited cataract surgery systematic review and metaanalysis. J. Cataract. Refract. Surg. 36, 13–19 (2010).
Meuleners, L. B., Fraser, M. L., Ng, J. & Morlet, N. The impact of first- and second-eye cataract surgery on injurious falls that require hospitalisation: a whole-population study. Age Ageing 43, 341–346 (2014).
Schwartz, S. et al. The effect of cataract surgery on postural control. Invest. Ophthalmol. Vis. Sci. 46, 920–924 (2005).
Durmus, B., Emre, S., Cankaya, C., Baysal, O. & Altay, Z. Gain in visual acuity after cataract surgery improves postural stability and mobility. Bratisl. Lek. Listy 112, 701–705 (2011).
Ishii, K., Kabata, T. & Oshika, T. The impact of cataract surgery on cognitive impairment and depressive mental status in elderly patients. Am. J. Ophthalmol. 146, 404–409 (2008).
Ayaki, M., Muramatsu, M., Negishi, K. & Tsubota, K. Improvements in sleep quality and gait speed after cataract surgery. Rejuvenation Res. 16, 35–42 (2013).
Lyubomirsky, S., King, L. & Diener, E. The benefits of frequent positive affect: does happiness lead to success?. Psychol. Bull. 131, 803–855 (2005).
Frey, B. S. Psychology. Happy people live longer. Science 331, 542–543 (2011).
Danner, D. D., Snowdon, D. A. & Friesen, W. V. Positive emotions in early life and longevity: findings from the nun study. J. Pers. Soc. Psychol. 80, 804–813 (2001).
Shirai, K. et al. Perceived level of life enjoyment and risks of cardiovascular disease incidence and mortality: the Japan public health center-based study. Circulation 120, 956–963 (2009).
Steptoe, A., Dockray, S. & Wardle, J. Positive affect and psychobiological processes relevant to health. J. Pers. 77, 1747–1776 (2009).
Matsunaga, M. et al. Association between perceived happiness levels and peripheral circulating pro-inflammatory cytokine levels in middle-aged adults in Japan. Neuro Endocrinol. Lett. 32, 458–463 (2011).
Kawashima, M. et al. Associations between subjective happiness and dry eye disease: a new perspective from the Osaka study. PLoS ONE 10, e0123299 (2015).
Matsuguma, S. et al. Patients’ satisfaction and subjective happiness after refractive surgery for myopia. Patient Prefer. Adher. 12, 1901–1906 (2018).
Matsuguma, S. et al. Strengths use as a secret of happiness: another dimension of visually impaired individuals’ psychological state. PLoS ONE 13, e0192323 (2018).
Ong, A. D., Kim, S., Young, S. & Steptoe, A. Positive affect and sleep: a systematic review. Sleep Med. Rev. 35, 21–32 (2017).
Kokune-Takahashi, A., Ayaki, M., Tsubota, K. & Negishi, K. Effects of cataract opacity and surgery on sleep quality. Rejuvenation Res 21, 53–60 (2018).
Feeny, S., Posso, A., McDonald, L., Chuyen, T. T. K. & Tung, S. T. Beyond monetary benefits of restoring sight in Vietnam: evaluating well-being gains from cataract surgery. PLoS ONE 13, e0192774 (2018).
Shimai, S., Otake, K., Utsuki, N., Ikemi, A. & Lyubomirsky, S. Development of a Japanese version of the Subjective Happiness Scale (SHS), and examination of its validity and reliability. Nihon Koshu Eisei Zasshi 51, 845–853 (2004).
Shimai, S., Yamamiya, Y. & Fukuda, S. Subjective happiness among Japanese adults: an upward tendency associated with age. Nihon Koshu Eisei Zasshi 65, 553–562 (2018).
Elliott, D. B., Bullimore, M. A., Patla, A. E. & Whitaker, D. Effect of a cataract simulation on clinical and real world vision. Br. J. Ophthalmol. 80, 799–804 (1996).
Chua, B. E., Mitchell, P. & Cumming, R. G. Effects of cataract type and location on visual function: the Blue Mountains Eye Study. Eye (Lond) 18, 765–772 (2004).
Bal, T., Coeckelbergh, T., Van Looveren, J., Rozema, J. J. & Tassignon, M. J. Influence of cataract morphology on straylight and contrast sensitivity and its relevance to fitness to drive. Ophthalmologica 225, 105–111 (2011).
Elliott, D. B., Gilchrist, J. & Whitaker, D. Contrast sensitivity and glare sensitivity changes with three types of cataract morphology: are these techniques necessary in a clinical evaluation of cataract?. Ophthalmic Physiol. Opt. 9, 25–30 (1989).
Stifter, E., Sacu, S. & Weghaupt, H. Functional vision with cataracts of different morphologies: comparative study. J. Cataract. Refract. Surg. 30, 1883–1891 (2004).
Zheng, L., Wu, X. H. & Lin, H. T. The effect of cataract surgery on sleep quality: a systematic review and meta-analysis. Int. J. Ophthalmol. 10, 1734–1741 (2017).
Erichsen, J. H., Brondsted, A. E. & Kessel, L. Effect of cataract surgery on regulation of circadian rhythms. J. Cataract. Refract. Surg. 41, 1997–2009 (2015).
Brickman, P., Coates, D. & Janoff-Bulman, R. Lottery winners and accident victims: is happiness relative?. J. Pers. Soc. Psychol. 36, 917–927 (1978).
Chylack, L. T. Jr. et al. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch. Ophthalmol. 111, 831–836. https://doi.org/10.1001/archopht.1993.01090060119035 (1993).
Sonja Lyubomirsky, H. S. L. A measure of subjective happiness: preliminary reliability and construct validation. Soc. Indic. Res. 46, 137–155 (1999).
Buysse, D. J., Reynolds, C. F. 3rd., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28, 193–213 (1989).
Doi, Y. et al. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res 97, 165–172 (2000).
Acknowledgements
We acknowledge the contributions of the following individuals to this study: Chisako Masui, the orthoptist of Keio University Hospital, and Lynda Charters for editing of this manuscript.
Author information
Authors and Affiliations
Contributions
E.Y., M.A., H.T., K.T. and K.N. made substantial contributions to conception and design. E.Y., N.N., H.A., K.S. and K.N. collected the data. E.Y. analyzed and interpreted data. E.Y. drafted the manuscript. M.A., H.T., N.N., H.A., K.S., K.T. and K.N. revised the manuscript critically for important intellectual content. E.E.Y., N.N., H.A., K.S. and K.N. administrated technical or material support. M.A., H.T., K.N., T.K., and K.T. and K.N. supervised. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yotsukura, E., Ayaki, M., Nezu, N. et al. Changes in patient subjective happiness and satisfaction with cataract surgery. Sci Rep 10, 17273 (2020). https://doi.org/10.1038/s41598-020-72846-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-72846-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.