Abstract
Further studies are required to investigate the impact of the COVID-19 pandemic on Parkinson’s disease (PD) progression. This study investigated the motor and non-motor progression of people with PD (PWP) at 6 months during the COVID-19 pandemic compared with that during the pre-pandemic period. Patients were recruited from Ain Shams University Hospitals, Cairo, in the period between April 2019 and December 2020. Fifty patients were included, of whom 17 and 33 patients were followed for 6 months before and during the pandemic, respectively. All patients were assessed at baseline and at 6 months using the MDS-UPDRS, Schwab and England scale (S&E), Hoehn and Yahr scale (H&Y), Berg Balance Scale, Timed Up and Go test (TUG), International Physical Activity Questionnaire, New Freezing of Gait Questionnaire, Non-Motor Symptoms Scale, and Beck Depression Inventory (BDI). Both groups were matched in age, gender, and disease characteristics. Patients followed during the pandemic showed more significant worsening of the total, part I and motor part of MDS-UPDRS, and balance scores (p < 0.001) than those followed during the pre-COVID-19 period. Gait (TUG), balance, and physical activity worsening were significantly correlated with baseline BDI, gait and balance scores, total and part I MDS-UPDRS scores, H&Y, and S&E OFF scores. Gait deterioration (TUG) was correlated with baseline physical activity (r = −0.510, p = 0.002). PWP showed worsening of motor and non-motor symptoms during the COVID-19 pandemic at the 6-month follow-up. Worsening of gait, balance, and physical activity was correlated with baseline motor and physical activity OFF scores.
Similar content being viewed by others
Introduction
Since the outbreak of the coronavirus disease 2019 (COVID-19) pandemic, individuals with Parkinson’s disease (PD) have been considered a vulnerable group to the effects of the COVID-19 pandemic, directly by infections with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and indirectly by pandemic-related restrictions, chronic stress, anxiety, physical inactivity, and compromised medical care. These effects included worsening of motor symptoms, higher mortality in advanced PD, worse anxiety and depression, impaired physical activity, and disruption of patients’ care1,2,3. Several recent studies have linked reduced physical activity and exercise to motor worsening during the pandemic, implying the significance of maintaining patients’ activity during restrictions4,5.
Moreover, it has been proposed that the COVID-19 pandemic may be followed by a higher incidence of neurodegenerative diseases; however, the evidence is insufficient to confirm that COVID-19 may trigger or accelerate neurodegeneration6. However, the impact of the COVID-19 pandemic and related measures on disease progression has not been explored. A recent retrospective study has reported a worsening of motor symptoms with a significant increase in motor disease progression during pandemic-related restrictions compared with that during the pre-pandemic period. The assessment was limited to ON-state and motor aspects7. Therefore, longitudinal studies are warranted to investigate the possibility of altered progression of motor and non-motor aspects of PD during the pandemic.
Accordingly, the current longitudinal study investigated the short-term motor and non-motor progression and related determinants of a cohort of people with PD (PWP) during the COVID-19 pandemic compared with the progression during the pre-pandemic period of another matched cohort.
Results
Fifty patients were included, of whom 17 and 33 patients were followed for 6 months before and during the pandemic, respectively. Both groups were matched for demographic and clinical characteristics except for longer disease duration (p = 0.007) and lower rigidity ON scores (p = 0.01) for patients followed during the pandemic (Table 1). Physical activity ((International Physical Activity Questionnaire [IPAQ]) was non-significantly lower in patients during the pandemic. All patients did not report symptoms suggestive of COVID-19 infection. Cronbach’s alpha coefficient of the questionnaires ranged from 0.75 to 0.98, indicating a satisfactory internal consistency.
Disease progression before and during the COVID-19 pandemic
Patients followed before the pandemic showed a moderately significant progression at 6 months of MDS-UPDRS-I (Non-Motor Aspects of Experiences of Daily Living [nM-EDL]) (p = 0.044) and OFF-state motor scores (p = 0.047). The Schwab and England Activities of Daily Living scale (S&E) OFF- and ON-state scores showed a significant progression (p = 0.04 and 0.011, respectively) although not H&Y. Postural Instability and Gait Disorder (PIGD) ON and OFF-states, axial OFF-state, and New Freezing of Gait Questionnaire (NFOG-Q) OFF-state scores showed a moderately significant progression. The total non-motor symptoms scale (NMSS) and IPAQ showed significant worsening (p < 0.001) (Supplementary Table 1). The corrected p-value showed no significant changes, except for NMSS and IPAQ scores.
Patients followed during the COVID-19 pandemic showed a significant marked worsening at 6 months of MDS-UPDRS total and all subscores, S&E and Hoehn and Yahr (H&Y) (p < 0.001), PIGD, NFOG-Q, Timed Up and Go test (TUG), Berg Balance Scale (BBS) in OFF and ON states, total NMSS, IPAQ, and Mini-Mental State Examination (MMSE) (p < 0.001) (Supplementary Table 2).
Compared with the patients followed before the pandemic, those followed during the pandemic had greater significant worsening of the total and motor MDS-UPDRS OFF- and ON-state scores, MDS-UPDRS part I (p < 0.001), rigidity OFF (p = 0.04) and ON-state scores (p < 0.001), bradykinesia ON-state scores (p < 0.001), BBS OFF- and ON-state scores (p < 0.001) (significant after Bonferroni correction), axial OFF-state scores, and TUG (p = 0.01, non-significant after Bonferroni correction). Levodopa equivalent daily dosage (LEDD), MMSE, NMSS, IPAQ, and PDQ showed similar changes in both groups (Table 2).
Correlations of disease progression during the pandemic
During the pandemic, the worsening of motor severity (H&Y) was correlated with disease duration (r = 0.500, p = 0.003), whereas motor complications (part IV) were directly correlated with baseline cognition (p = 0.02) and S&E (p = 0.03) and inversely correlated with depression and total and motor MDS-UPDRS scores (p = 0.04) (non-significant after Bonferroni correction); conversely, total and other MDS-UPDRS progression did not show significant correlations (Table 3).
Cognitive worsening was correlated with years of education, baseline MDS-UPDRS part II (r = −0.430, p = 0.01), PIGD (r = −0.370, p = 0.03), and axial scores (r = −0.370, p = 0.03). Total NMSS worsening was correlated with baseline NFOG-Q (r = 0.450, p = 0.01) and PIGD scores (r = 0.360, p = 0.04) (non-significant after Bonferroni correction). TUG (OFF), BBS (OFF), and IPAQ worsening were significantly correlated with baseline Beck Depression Inventory (BDI), gait (TUG) and balance (BBS) OFF scores, total and part I MDS-UPDRS scores, and H&Y and S&E scores. After Bonferroni correction, a significant correlation was noted between TUG and baseline OFF-state TUG, PIGD, axial, H&Y, S&E, and IPAQ scores; BBS and baseline OFF PIGD and NFOG-Q; and IPAQ and baseline MMSE, MDS-UPDRS-total and part II-OFF, BDI, TUG-OFF, and IPAQ scores (p ≤ 0.002) (Table 3).
On comparison between the two groups regarding the assessment scale scores after 6 months, significant worsening was noted in MDS-UPDRS-I in the patients followed during the COVID-19 period (p = 0.003) (Supplementary Table 3).
Discussion
Several cross-sectional studies have constantly described the worsening of motor and non-motor symptoms during the COVID-19 pandemic. However, its impact on disease progression was not adequately investigated. Distinctively, this longitudinal study explored disease progression during the pandemic and showed worsening of motor and non-motor symptoms over a 6-month follow-up during the pandemic compared with that during the pre-pandemic period. Gait, balance, and physical activity worsening were correlated with baseline motor and physical activity scores. The current study showed the possibility of deleterious effects of pandemic lockdown on disease progression in PWP.
The current findings are consistent with those of previous cross-sectional studies. An Indian study showed worsening of motor symptoms, especially bradykinesia in 69.2% of cases during the COVID-19 pandemic, followed by tremor, rigidity, and gait freezing8. Additionally, PWP reported worsening in mental health, quality of life, and physical inactivity during this pandemic5. These indirect effects of COVID-19 are more confirmed and may be more common and more harmful than the direct effects of viral infections1,9,10. The worsening of motor and non-motor symptoms has been attributed to stress, physical inactivity, pharmacodynamic effects, dramatic changes in routine, and social isolation11,12. The impact of stress on PD progression has been previously investigated and proven to negatively affect the course of the disease1,2,4.
Conversely, the impact on disease progression is not well investigated. However, a recent study by Ineichen et al. has reported increased motor disease progression during pandemic-related restrictions compared with that before the COVID-19 pandemic, which is consistent with the current study7. Similar to symptom worsening, more deterioration during the pandemic could be explained by stress, physical inactivity, and social isolation.
PWP are more vulnerable to recent stressors, which is attributed to more dopamine depletion and consequently reduced coping mechanisms for stress13. Moreover, chronic stress may induce oxidative damage to the cell membrane, as well as inflammatory and regulatory T-cell dysfunction, leading to a possible increase in midbrain dopaminergic neuron loss and motor symptom worsening14. Additionally, chronic stress accelerates dopaminergic cell loss in animal PD models and exacerbates the neuropathological changes15. The accompanying microglial activation and oxidative stress may mechanistically justify the stress-induced neurodegeneration in PD16.
Remarkably, gait (TUG), balance, and physical activity were markedly worsened during the pandemic, which was related to baseline motor and physical activity scores. Consistently, a recent study, which assessed 12 patients before and 2 months after lockdown, has shown moderate gait, falls, and balance worsening although not freezing of gait, despite being contacted by a multidisciplinary team17.
Approximately 29% of patients with PD are less physically active than the normal population, which are predicated by disease severity, gait, and impairment of activities of daily living18. Increased physical activity and exercise have a positive effect on motor and non-motor symptoms and probably PD disease progression19. Moreover, exercise may improve the progression of PD manifestations and enhance motor and cognitive circuit-related neuroplasticity20,21,22.
Despite there being no reported cases of SARS-CoV-2 infection, its direct effect on disease progression due to subclinical infection could not be totally excluded. An Italian study reported motor and non-motor deterioration that was attributed to infection and drug pharmacodynamic-related mechanisms. A quarter of patients with PD and COVID-19 had mild symptoms and recovered without treatment23.
SARS-CoV-2-related neurodegenerations, especially nigrostriatal degenerations, have been proposed owing to the possibility of neuro-invasion via the olfactory bulb, Angiotensin-Converting Enzyme 2 (ACE2) receptor expression by dopaminergic neurons, associated inflammatory and vascular changes that overlap with PD pathogenesis, and progression in addition to reported cases of SARS-CoV-2-related parkinsonism with dopamine transporter imaging abnormalities1,24. However, the impact of COVID-19 on neurodegeneration, including the development or increased progression of PD, has not yet been confirmed.
The strengths of the current study include the comprehensive assessment in the OFF and ON states and follow-up of patients with mild-to-moderate PD before and during the pandemic, with a comprehensive assessment of motor and non-motor symptoms and matched baseline characteristics of patients in both groups.
The current study has some limitations. The small number and short follow-up period, as well as the lack of confirmation or exclusion of SARS-CoV-2 infection using laboratory tests during assessments, are considered its limitations. Furthermore, our cohort included patients with mild-to-moderate PD who should be considered in the interpretation of our findings.
This study confirms the impact of the COVID-19 pandemic on the motor and non-motor symptoms of PD and demonstrates another possible effect, which is the short-term worsening of disease progression, implying the significance of managing related factors, including anxiety, chronic stress, and physical inactivity, and considering this effect in interpreting longitudinal studies during the pandemic.
Methods
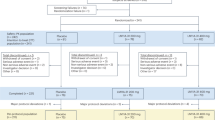
This is a retrospective analysis of the data from our longitudinal study (PDPRO-EGY, clinicalTrial.gov, NCT04062279) that investigated the progression of Egyptian patients with PD. Patients were recruited from the movement disorders outpatient clinic of Ain Shams University Hospitals (Cairo, Egypt) in the period between April 2019 and December 2020. Patients with PD who were diagnosed using the International Parkinson and Movement Disorders Society (MDS) diagnostic criteria25 and completed both baseline and 6-month follow-up assessments before or during the pandemic period were included and compared. Patients who completed baseline and follow-up assessments during the pandemic were included as the “one group” (from March to December 2020), whereas those who completed the follow-up before March 2020 (before lockdown procedures in Egypt) were included as the “control group.”
Patients excluded include patients with atypical or acquired parkinsonism, those who did not complete the follow-up assessment, those who were assessed in the pre-pandemic (baseline) and during the pandemic (6-month follow-up) periods, and those who underwent functional brain surgery (before or during the follow-up period).
Sampling and sample size
The sample size was calculated using an online calculator (https://www.calculator.net/sample-size-calculator.html), where for a 95% confidence level and a margin of error 5, the minimal sample size was estimated to be 16 patients for each group.
Ethical considerations
All participants provided written informed consent. The study was approved by the ethical committee of the Faculty of Medicine of Ain Shams University according to the Declaration of Helsinki.
Data collection
All patients were evaluated at baseline and at 6-month follow-up using the total and different parts of the MDS-UPDRS (parts include part I [nM-EDL], part II [motor aspects of daily living], part III [motor examination], and part IV [motor complications]), H&Y for disease severity, S&E for activities of daily living26, NFOG-Q27 for gait freezing, BBS28 for balance assessment, and TUG29 for gait and mobility assessment during the OFF and ON states. Other scales included the IPAQ-SF30 for physical activities, NMSS31 for non-motor symptoms evaluation, Arabic version of BDI32 for depression, Arabic version of PD questionnaire 3933 for quality of life, and MMSE34 for cognition. All patients have been evaluated in person by a trained physician. LEDD was calculated at baseline and follow-up as the sum of the daily dose of all dopaminergic agents35.
Statistical analysis
Data analysis was performed using IBM SPSS software package version 25.0 (IBM Corp., Armonk, NY). Qualitative data were described as frequencies and percentages and compared using the chi-square test, whereas quantitative data were presented as medians and interquartile ranges or means ± standard deviations and compared using either the Mann–Whitney U test or Student’s t test according to the distribution of the data, respectively. The Wilcoxon signed-rank test was used to compare baseline and follow-up data within each group. The Spearman correlation coefficient was used to evaluate the correlation between different variables. The significance was set at p < 0.05. Bonferroni correction was performed for the multiple comparisons and correlations, and an adjusted p-value was used. Cronbach’s α coefficient was used as a measure of the internal consistency of used questionnaires.
Data availability
The datasets generated during the current study will be made available from the corresponding author upon request.
References
Fearon, C. & Fasano, A. Parkinson’s disease and the COVID-19 pandemic. J. Parkinsons Dis. 11, 431–444 (2021).
Helmich, R. C. & Bloem, B. R. The impact of the COVID-19 pandemic on Parkinson’s disease: hidden sorrows and emerging opportunities. J. Parkinsons Dis. 10, 351–354 (2020).
Feeney, M. P. et al. The impact of COVID-19 and social distancing on people with Parkinson’s disease: a survey study. npj Parkinsons Dis. 7, 10 (2021).
van der Heide, A., Meinders, M. J., Bloem, B. R. & Helmich, R. C. The impact of the COVID-19 pandemic on psychological distress, physical activity, and symptom severity in Parkinson’s disease. J. Parkinsons Dis. 10, 1355–1364 (2020).
Shalash, A. et al. Mental health, physical activity, and quality of life in Parkinson’s disease during COVID-19 pandemic. Mov. Disord. 35, 1097–1099 (2020).
Krey, L., Huber, M. K., Hoglinger, G. U., Wegner, F. & Can, S.-C. Can SARS-CoV-2 Infection lead to neurodegeneration and Parkinson’s disease? Brain Sci. 11, 1654 (2021).
Ineichen, C., Baumann-Vogel, H., Sitzler, M., Waldvogel, D. & Baumann, C. R. Worsened Parkinson’s disease progression: impact of the COVID-19 pandemic. J. Parkinsons Dis. 11, 1579–1583 (2021).
Saluja, A., Parihar, J., Garg, D. & Dhamija, R. K. The impact of COVID-19 pandemic on disease severity and quality of life in Parkinson’s disease. Ann. Indian Acad. Neurol. 24, 217–226 (2021).
Chaudhry, Z. L. et al. ER Stress in COVID-19 and Parkinson’s disease: in vitro and in silico evidences. Brain Sci. 12. https://doi.org/10.3390/brainsci12040507 (2022).
Goerttler, T. et al. SARS-CoV-2, COVID-19 and Parkinson’s disease-many issues need to be clarified-A critical review. Brain Sci. 12. https://doi.org/10.3390/brainsci12040456 (2022).
Vignatelli, L. et al. The indirect impact of COVID-19 on major clinical outcomes of people with Parkinson’s disease or Parkinsonism: a cohort study. Front. Neurol. 13, 873925 (2022).
Hermanowicz, N. et al. Impact of isolation during the COVID-19 pandemic on the patient burden of Parkinson’s disease: a PMD alliance survey. Neuropsychiatr. Dis. Treat. 18, 633–643 (2022).
Douma, E. H. & de Kloet, E. R. Stress-induced plast. functioning ventral tegmental dopamine neurons. Neurosci. Biobehav. Rev. 108, 48–77 (2020).
Goldstein, D. S. Stress, allostatic load, catecholamines, and other neurotransmitters in neurodegenerative diseases. Cell Mol. Neurobiol. 32, 661–666 (2012).
Smith, L. K., Jadavji, N. M., Colwell, K. L., Katrina Perehudoff, S. & Metz, G. A. Stress accelerates neural degeneration and exaggerates motor symptoms in a rat model of Parkinson’s disease. Eur. J. Neurosci. 27, 2133–2146 (2008).
Sugama, S. et al. Chronic restraint stress triggers dopaminergic and noradrenergic neurodegeneration: possible role of chronic stress in the onset of Parkinson’s disease. Brain Behav. Immun. 51, 39–46 (2016).
Luis-Martínez, R. et al. Impact of social and mobility restrictions in Parkinson’s disease during COVID-19 lockdown. BMC Neurol. 21, 332 (2021).
van Nimwegen, M. V. et al. Physical inactivity in Parkinson’s disease. J. Neurol. 258, 2214–2221 (2011).
Bouça‐Machado, R. et al. Physical activity, exercise, and physiotherapy in Parkinson’s disease: defining the concepts. Mov. Disord. Clin. Pract. 7, 7–15 (2020).
Petzinger, G. M. et al. Exercise-enhanced neuroplasticity targeting motor and cognitive circuitry in Parkinson’s disease. Lancet Neurol. 12, 716–726 (2013).
Paul, K. C. et al. The association between lifestyle factors and Parkinson’s disease progression and mortality. Mov. Disord. 34, 58–66 (2019).
Amara, A. W. et al. Self-reported physical activity levels and clinical progression in early Parkinson’s disease. Parkinsonism Relat. Disord. 61, 118–125 (2019).
Cilia, R. et al. Effects of COVID-19 on Parkinson’s disease clinical features: a community-based case-control study. Mov. Disord. 35, 1287–1292 (2020).
Bouali-Benazzouz, R. & Benazzouz, A. Covid-19 infection and Parkinsonism: is there a link? Mov. Disord. 36, 1737–1743 (2021).
Postuma, R. B. et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 30, 1591–1601 (2015).
Goetz, C. G. et al. Movement Disorder Society-Sponsored Revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov. Disord. 23, 2129–2170 (2008).
Giladi, N. et al. Validation of the freezing of gait questionnaire in patients with Parkinson’s disease. Mov. Disord. 24, 655–661 (2009).
Berg, K. O., Wood-Dauphinee, S. L., Williams, J. I. & Maki, B. Measuring balance in the elderly: validation of an instrument. Can. J. Public Health 83, S7–S11 (1992).
Bohannon, R. W. Reference values for the timed up and go test: a descriptive meta-analysis. J. Geriatr. Phys. Ther. 29, 64–68 (2006).
Craig, C. L. et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 35, 1381–1395 (2003).
Chaudhuri, K. R. et al. The metric properties of a novel non-motor symptoms scale for Parkinson’s disease: results from an international pilot study. Mov. Disord. 22, 1901–1911 (2007).
Fawzi, M. H., Fawzi, M. M. & Abu-Hindi, W. Arabic version of the Major Depression Inventory as a diagnostic tool: reliability and concurrent and discriminant validity. East. Mediterr. Health J. Arabic version 18, 304–310 (2012).
Shalash, A. S. et al. Non-motor symptoms as predictors of quality of life in Egyptian patients with Parkinson’s disease: a cross-sectional study using a culturally adapted 39-Item Parkinson’s disease questionnaire. Front. Neurol. 9, 357 (2018).
Tuijl, J. P., Scholte, E. M., de Craen, A. J. & van der Mast, R. C. Screening for cognitive impairment in older general hospital patients: comparison of the six-Item Cognitive Impairment Test with the Mini-Mental State Examination. Int. J. Geriatr. Psychiatry 27, 755–762 (2012).
Tomlinson, C. L. et al. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov. Disord. 25, 2649–2653 (2010).
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
Research project: conception: A.S. and M.E., organization: A.S. and E.H., and execution: A.H., E.H., A.G., and A.S.; statistical analysis: design and execution: E.H. and A.S., and review and critique: A.G., M.E., and M.S.; thematic analysis: design and execution: A.H., E.H., and A.S., and review and critique: A.S., A.G., M.E., and M.S.; and manuscript: writing of the first draft: A.S., E.H.; and review and critique: A.S., E.H., A.G., M.E., and M.S.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shalash, A., Helmy, A., Salama, M. et al. A 6-month longitudinal study on worsening of Parkinson’s disease during the COVID-19 pandemic. npj Parkinsons Dis. 8, 111 (2022). https://doi.org/10.1038/s41531-022-00376-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41531-022-00376-x
This article is cited by
-
Predictors of stress resilience in Parkinson’s disease and associations with symptom progression
npj Parkinson's Disease (2024)