Abstract
Frailty is a state of increased vulnerability to stress resulting from physiological decline associated with aging. Topics of hypertension management and its association with frailty and cognitive function, recent studies of coronavirus disease 2019 infection (COVID-19) in elderly is discussed in this narrative review. While various guidelines for hypertension recommend that frailty is taken into account in treatment decisions, specific assessment tools and clinical decision criteria have not been explicitly established. Hypertension is prevalent in frail individuals, although a direct association has not been reported. Therefore, optimal blood pressure (BP) control is critical for managing cardiovascular risk reduction and preserving quality of life in frail hypertensive patients. BP typically decreases in later life or situations in which patients are dependent on nursing care. Mortality is reported to be high among frail patients with lower BP, raising questions about appropriate BP targets for frail patients. Cognitive decline is one of the domains of frailty, and is associated with a loss of autonomy, lack of self-management, and compromised quality of life. It remains to be clarified whether antihypertensive treatment is beneficial for cognitive function especially in older individuals. Increased severity and mortality of COVID-19 infection has been reported in older people. Clinical manifestations and biomarkers particular to older patients, and lifestyle changes including social isolation during the COVID-19 pandemic is reported. From the knowledge from recent literatures, future perspectives for holistic approach and management of frail older people is addressed.

Similar content being viewed by others
Introduction
Frailty is a state of increased vulnerability to stress resulting from physiological decline associated with aging [1]. Frailty is included in various hypertension guidelines [2, 3] for two major reasons. First, population aging in many societies is occurring at an unprecedented speed. In aging or aged communities, difficulties in older patient care are common. Many older people exhibit complex medical conditions, social loneliness, cognitive decline, polypharmacy, and frailty that should be considered when medical procedures and treatment are performed. Second, frailty is related to morbidity and mortality of various diseases, such as diabetes, chronic obstructive pulmonary diseases, chronic kidney diseases, depression, and hypertension. Moreover, frailty is a predictor of poor postoperative outcomes including mortality, longer in-hospital time, complications, and decline in activities of daily living (ADL).
In this mini review, current topics regarding frailty and its association with other medical conditions are discussed.
Frailty and blood pressure targets
Many randomized controlled trials have reported that intensive blood pressure (BP) control can be safely implemented in older patients, including the Hypertension in the Very Elderly Trial (HYVET) [4], Systolic Blood Pressure Intervention Trial (SPRINT) [5], and Strategy of Blood Pressure Intervention in the Elderly Hypertensive Patients (STEP) [6] trials. On the basis of the results of meta-analysis comparing the effects of BP-lowering treatment on the risk of major cardiovascular events in groups of patients stratified by age, risk reduction has been indicated in all age groups, with a greater effect reported in older patient groups [7]. Accumulating evidence indicates that older patients, even those > 80 years old, benefit from appropriate BP-lowering treatment. Although it is widely considered that age alone should not be a determinant for modifying BP targets, older people have many comorbidities, as well as higher rates of cognitive dysfunction and frailty which should be taken into account.
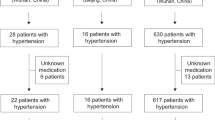
Recent studies have investigated optimal hypertension treatment for older patients with frailty (Fig. 1).
A cross-sectional study was performed in 599 subjects in the Nambu study cohort (average age: 78 years). Using the Kihon check list (a self-report questionnaire widely used in Japan [8]), frailty was diagnosed in 37% of patients. The adjusted odds ratios (ORs; 95% confidence interval [CI]) of each cardiovascular risk factor for frailty were as follows: systolic BP (each 10 mmHg increase) 0.83 (0.72–0.95), low density lipoprotein cholesterol (each 10 mg/dl increase) 0.96 (0.86–1.05), and body mass index (each 1 kg/m2 increase) 1.03 (0.97–1.10). The authors indicated that favorable cardiovascular risk profile, referred to as “reverse metabolic syndrome,” might be a risk for frailty [9]. In the same cohort, patients were prospectively followed up for 41 months and the associations of mortality with frailty and BP were evaluated. Among 49 patients who died, mortality rates were lowest in those with systolic BP < 140 mmHg and non-frailty, and highest in those with systolic BP < 140 mmHg and frailty [10]. The results indicated that frail patients have a higher risk of all-cause mortality than non-frail patients, especially those with lower BP, suggesting that frailty should be taken into account during BP management. The association between BP and mortality with the impact of frailty was evaluated in another longitudinal study. Among non-frail participants, a J-shaped association was found. On the other hand, for frail older adults, a tendency toward lower risk among those with systolic BP ≥ 130 mmHg was observed [11]. Recent systematic review and meta-analysis showed no mortality difference between frail individuals with systolic BP less than 140 mmHg and those with more than 140 mmHg, while lower mortality was observed in non-frail people with lower systolic BP [12].
In contrast, on the basis of the HYVET1 and SPRINT2 studies, it was proposed that antihypertensive treatment is beneficial for risk reduction of cardiovascular events and mortality in both robust and frail participants. Epidemiological studies reported that lower BP is harmful for cognition and increases mortality in very elderly patients with low levels of physical ability [13, 14]. The difficulty in determining target BP of frailty in older patients underlies in these conflicting results. A variety of scales and assessment tools for frailty have been developed (Table 1). The Cardiovascular Health Study scale is a biological model of frailty with five components: weight loss, exhaustion, low energy expenditure, slowness, and weakness. The Frailty Index is calculated as the number of deficits, consisting of symptoms, diseases, conditions, and disability. The Edmonton Frail Scale (EFS) is a simpler questionnaire combining social, physical, psychological, and physiological factors. The Kihon Checklist is similar to the EFS, which measures various domains of frailty with a questionnaire, and is widely used in Japan. Additionally, handgrip strength and walking speed alone have been used for assessing frailty in some studies. Variation in the instruments used in different studies makes it confusing to compare the results between studies, although validation of these assessment tools has been carried out [8, 15]. Moreover, frailty constitutes an accumulation of physical, cognitive, psychological, and social components. Frailty progresses as these components mutually interact with each other. Many previous studies did not clarify which of the components, including comorbidities, are prevalent in each patient with frailty. The heterogeneity of older patients with frailty makes it difficult to fit to a single algorithm for determining an appropriate BP target.
Several previous studies have presented proposals regarding the treatment of older patients with frailty. Benetos et al. used the Clinical Frailty Scale (CFS) to identify three different patient profiles of functional status and autonomy for ADL [16]. In each profile, antihypertensive treatment strategies that consider the benefit and risk of treatment are recommended. Liu et al. proposed management of hypertension in older people with two steps to define frailty (self-reported frailty tools and comprehensive geriatric assessment tool), and for those who are identified as frail, intervention of antihypertensive treatment and frailty are suggested [17]. Despite these assessment tools and proposal of management of BP in older hypertensives, comprehensive geriatric assessment (CGA) is not always performed in daily clinical practice. CFS demonstrates silhouette of patients representing particular functional status which physicians are able to evaluate frailty at a glance [18]. Calf circumference was a predictable marker of frailty [19]. Dementia Assessment Sheet for Community-based Integrated Care System 21-items (DASC-21) and 8-itmes (DASC-8) are simple questionnaire containing 21 or 8 questions evaluating cognition, ADL and instrumental ADL (IADL) associated with frailty and several CGA components [20, 21]. By utilizing these tools, frailty which is one of the important factors of BP management can be evaluated without taking much time.
Cognitive function and blood pressure
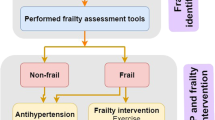
It is currently unclear whether antihypertensive treatment has preventative effects on dementia or cognitive decline (Fig. 2). A systematic review indicated that lowering BP with antihypertensive agents, compared with a control condition, was significantly associated with a lower risk of incident dementia and cognitive impairment [22, 23]. However, most of the participants in these studies were 60 to 70 years old. Among older patients, BP-lowering treatment was reported to have no positive effect on cognitive function. The Leiden 85-plus Study, which examined participants aged 85 years old and above, reported that lower BP during antihypertensive treatment was associated with increased risk of cognitive decline [14]. In the SCOPE study, elderly patients aged 70 to 89 years old with mild to moderately elevated BP were randomized to treatment with an angiotensin receptor blocker or placebo. No significant differences were found in mini mental state examination (MMSE) score decline or the proportion of patients who developed dementia after an average of 3.7 years of follow-up [24]. In the SPRINT-MIND study, among ambulatory adults with hypertension, treating to a systolic BP goal of less than 120 mmHg compared with a goal of less than 140 mmHg. Intensive BP control significantly reduced the risk of mild cognitive impairment (MCI) and the combined occurrence of mild cognitive impairment or probable dementia. However, it did not result in a significant reduction in the risk of probable dementia presumably with early termination of the study and fewer incidence of dementia [25].
Patients with dementia are excluded from most clinical trials, leaving uncertainty regarding the optimal treatment for preventing cognitive decline, and the incidence of dementia. Cognitive function was reported to deteriorate after 1 year of follow-up in patients with MCI or dementia whose clinical systolic BP was controlled under 110 mmHg [26]. The causal relationship between lower BP during antihypertensive treatment and cognitive decline is unknown, but detecting MCI in daily practice is challenging. Lower body mass index values are considered to characterize older hypertensive patients with cognitive impairment [27] implying careful observation of BP management among lean, older patients.
The associations of physical and mental frailty with BP were investigated in older patients in the SONIC study [28]. In people aged 70 ± 1 (n = 1,000), 80 ± 1 (n = 978), and 90 ± 1 (n = 272) years, BP, grip strength, gait speed, and cognitive function were examined on site. A lower systolic BP level was associated with a higher prevalence of physical frailty among 80-year-olds who were taking antihypertensive medication. Cognitive function was not associated with frailty among patients without antihypertensive medication. However, among those aged 70 years old, higher systolic BP and lower cognitive function were associated with frailty, while among 90-year-olds, the opposite result was shown.
Ishikawa et al. reported an inverse association with BP in patients with and without cognitive dysfunction [29]. In subjects with preserved cognitive function (MMSE ≥ 24 points), MMSE scores decreased with increases in systolic BP (B = −0.047 per 10 mmHg increase, P = 0.002) after adjusting for age, sex, body mass index, alcohol habit, smoking status, diabetes, history of stroke, and geriatric nutritional index. However, in subjects with reduced cognitive function (MMSE < 24 points), decreases in MMSE score were associated with reductions in systolic BP.
A systematic review and meta-analysis of the prevalence of MCI among hypertensive patients was conducted by Quin et al. The prevalence of MCI was 30%, with a sample of 47,179 hypertensive patients. Heterogeneity between studies was reported in ethnicity, study design (cross-sectional or cohort study), and assessment tools of cognition (MMSE or Montreal Cognitive Assessment [MoCA]) [30].
Frailty and coronavirus disease 2019 (COVID-19)
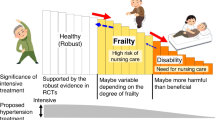
The coronavirus disease 2019 (COVID-19) pandemic has had a major global impact since 2019 when it first emerged in China. Because the severity and mortality rates of COVID-19 have been found to increase considerably with advancing age, identifying the characteristics of elderly patients with COVID-19 is important. The clinical manifestation of COVID-19 in elderly patients has been investigated in several studies (Fig. 3). In a meta-analysis conducted to investigate risk factors for severe cases in COVID-19, male, elderly (over 65 years of age), and obese patients, and those with any comorbidities, particularly hypertension, diabetes, and cardiovascular disease (CVD), were reported to be more likely to develop into severe cases. However, the association between hypertension, diabetes, and CVD and the severity of COVID-19 was reported to decrease with age [31]. Another meta-analysis reported that the overall prevalence of dementia among COVID-19 patients was 10% (7–13%), and was associated with increased mortality [32].
An association has been reported between COVID-19 severity and apolipoprotein E4 (ApoE4), which is a significant risk factor for Alzheimer’s disease and is also associated with atherosclerotic CVD. In one study, data from a community cohort in the United Kingdom were analyzed, and the ApoE e4e4 allele was found to increase the risk of severe COVID-19 infection, independent of preexisting dementia, cardiovascular disease, and type-2 diabetes [33]. In another study, ApoE4 was compared between asymptomatic and symptomatic patients with COVID-19, and significantly higher ApoE4 was detected in symptomatic patients (p = 0.03; OR 1.43, 95% CI 1.05–1.95) [34]. ApoE plays a pivotal role in cholesterol metabolism, but also moderates macrophage pro-/anti-inflammatory phenotypes and interacts with angiotensin-converting enzyme 2, which is highly expressed in type II alveolar cells in the lungs. These mechanisms may provide an explanation for ApoE carriers to have severe infection in COVID-19.
Previous studies have reported various difficulties in the diagnosis of COVID-19 in older patients. Elderly patients are less inclined to exhibit typical characteristics of COVID-19 such as fever, cough and myalgia, and less likely to exhibit typical findings on X-ray and computed tomography scans [31, 35].
Additionally, the pandemic has had negative impacts beyond the direct effects of COVID-19. Daily life was affected by coronavirus countermeasures for many older people. The subjective amount of daily movement, leg muscle strength, and meal size decreased among older adults with frailty during the COVID-19 pandemic in Japan. Decreases in subjective leg muscle strength were reported to be associated with frailty [36].
Future perspectives
Frailty has impacts on various medical conditions that are associated with higher rates of hospitalization, readmission, and mortality, leading to a vicious cycle of physical, mental, and social deterioration. Antihypertensive treatment can reduce stroke, cardiovascular events, and mortality in middle age patients and recent topics revealed it applies to older adults. Thus, older hypertensive patients can be treated in line with the target BP provided in guidelines albeit physicians should pay attention to how fit they are, if they can measure and record or take notes of their BP at home, and their medication adherence. It is important to consider frailty when treating older patients, and each patient must be managed individually in consideration of their complex and diverse characteristics.
References
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–62.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:1953–2041.
Warwick J, Falaschetti E, Rockwood K, Mitnitski A, Thijs L, Beckett N, et al. No evidence that frailty modifies the positive impact of antihypertensive treatment in very elderly people: an investigation of the impact of frailty upon treatment effect in the HYpertension in the Very Elderly Trial (HYVET) study, a double-blind, placebo-controlled study of antihypertensives in people with hypertension aged 80 and over. BMC Med. 2015;13:78.
Williamson JD, Supiano MA, Applegate WB, Berlowitz DR, Campbell RC, Chertow GM, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673–82.
Zhang W, Zhang S, Deng Y, Wu S, Ren J, Sun G, et al. Trial of intensive blood-pressure control in older patients with hypertension. N Engl J Med. 2021;385:1268–79.
The Blood Pressure Lowering Treatment Trialists’ Collaboration. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet. 2021;397:1625–36.
Satake S, Senda K, Hong YJ, Miura H, Endo H, Sakurai T, et al. Validity of the Kihon Checklist for assessing frailty status. Geriatrics Gerontol Int. 2016;16:709–15.
Matsuoka M, Inoue T, Shinjo T, Miiji A, Tamashiro M, Oba K, et al. Cardiovascular risk profile and frailty in Japanese outpatients: the Nambu Cohort Study. Hypertens Res. 2020;43:817–23.
Inoue T, Matsuoka M, Shinjo T, Tamashiro M, Oba K, Kakazu M, et al. Blood pressure, frailty status, and all-cause mortality in elderly hypertensives; The Nambu Cohort Study. Hypertens Res. 2022;45:146–54.
Kremer KM, Braisch U, Rothenbacher D, Denkinger M, Dallmeier D. Systolic blood pressure and mortality in community-dwelling older adults: frailty as an effect modifier. Hypertension. 2022;79:24–32.
Todd OM, Wilkinson C, Hale M, Wong NL, Hall M, Sheppard JP, et al. Is the association between blood pressure and mortality in older adults different with frailty? A systematic review and meta-analysis. Age Ageing. 2019;48:627–35.
Odden MC, Peralta CA, Haan MN, Covinsky KE. Rethinking the association of high blood pressure with mortality in elderly adults: the impact of frailty. Arch Intern Med. 2012;172:1162–8.
Streit S, Poortvliet RKE, Gussekloo J. Lower blood pressure during antihypertensive treatment is associated with higher all-cause mortality and accelerated cognitive decline in the oldest-old. Data from the Leiden 85-plus Study. Age Ageing. 2018;47:545–50.
Malmstrom TK, Miller DK, Morley JE. A comparison of four frailty models. J Am Geriatr Soc. 2014;62:721–6.
Benetos A, Bulpitt CJ, Petrovic M, Ungar A, Agabiti Rosei E, Cherubini A, et al. An expert opinion from the European Society of Hypertension-European Union Geriatric Medicine Society Working Group on the management of hypertension in very old, frail subjects. Hypertension. 2016;67:820–5.
Liu P, Li Y, Zhang Y, Mesbah SE, Ji T, Ma L. Frailty and hypertension in older adults: current understanding and future perspectives. Hypertens Res. 2020;43:1352–60.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–95.
Xu KY, Wang JJ, Chen J, Zhao X, Yuan LF, Zhang Q. Calf circumference predicts frailty in older adults: the Chinese longitudinal healthy longevity survey. BMC Geriatr. 2022;22:936.
Awata S, Sugiyama M, Ito K, Ura C, Miyamae F, Sakuma N, et al. Development of the dementia assessment sheet for community-based integrated care system. Geriatr Gerontol Int. 2016;16:123–31.
Toyoshima K, Araki A, Tamura Y, Ishikawa J, Kodera R, Oba K, et al. Use of dementia assessment sheet for community-based integrated care system 8-items (DASC-8) for the screening of frailty and components of comprehensive geriatric assessment. Geriatr Gerontol Int. 2020;20:1157–63.
Gupta A, Perdomo S, Billinger S, Beddhu S, Burns J, Gronseth G. Treatment of hypertension reduces cognitive decline in older adults: a systematic review and meta-analysis. BMJ Open. 2020;10:e038971.
Hughes D, Judge C, Murphy R, Loughlin E, Costello M, Whiteley W, et al. Association of blood pressure lowering with incident dementia or cognitive impairment: a systematic review and meta-analysis. JAMA. 2020;323:1934–44.
Lithell H, Hansson L, Skoog I, Elmfeldt D, Hofman A, Olofsson B, et al. The Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trial. J Hypertens. 2003;21:875–86.
Williamson JD, Pajewski NM, Auchus AP, Bryan RN, Chelune G, Cheung AK, et al. Effect of intensive vs standard blood pressure control on probable dementia: a randomized clinical trial. JAMA. 2019;321:553–61.
Mossello E, Pieraccioli M, Nesti N, Bulgaresi M, Lorenzi C, Caleri V, et al. Effects of low blood pressure in cognitively impaired elderly patients treated with antihypertensive drugs. JAMA Intern Med. 2015;175:578–85.
Sakakura K, Hoshide S, Ishikawa J, Momomura S, Kawakami M, Shimada K, et al. Association of body mass index with cognitive function in elderly hypertensive Japanese. Am J Hypertens. 2008;21:627–32.
Kabayama M, Kamide K, Gondo Y, Masui Y, Nakagawa T, Ogawa M, et al. The association of blood pressure with physical frailty and cognitive function in community-dwelling septuagenarians, octogenarians, and nonagenarians: the SONIC study. Hypertens Res. 2020;43:1421–9.
Ishikawa J, Seino S, Kitamura A, Toba A, Toyoshima K, Tamura Y, et al. The relationship between blood pressure and cognitive function. Int J Cardiol Cardiovasc Risk Prev. 2021;10:200104.
Qin J, He Z, Wu L, Wang W, Lin Q, Lin Y, et al. Prevalence of mild cognitive impairment in patients with hypertension: a systematic review and meta-analysis. Hypertens Res. 2021;44:1251–60.
Hu J, Wang Y. The clinical characteristics and risk factors of severe COVID-19. Gerontology. 2021;67:255–66.
July J, Pranata R. Prevalence of dementia and its impact on mortality in patients with coronavirus disease 2019: A systematic review and meta-analysis. Geriatr Gerontol Int. 2021;21:172–7.
Kuo CL, Pilling LC, Atkins JL, Masoli JAH, Delgado J, Kuchel GA, et al. APOE e4 genotype predicts severe COVID-19 in the UK Biobank community cohort. J Gerontol Ser A, Biol Sci Med Sci. 2020;75:2231–2.
Hubacek JA, Dlouha L, Dusek L, Majek O, Adamkova V. Apolipoprotein E4 allele in subjects with COVID-19. Gerontology. 2021;67:320–2.
Gómez-Belda AB, Fernández-Garcés M, Mateo-Sanchis E, Madrazo M, Carmona M, Piles-Roger L, et al. COVID-19 in older adults: what are the differences with younger patients? Geriatr Gerontol Int. 2021;21:60–65.
Shinohara T, Saida K, Tanaka S, Murayama A. Association between frailty and changes in lifestyle and physical or psychological conditions among older adults affected by the coronavirus disease 2019 countermeasures in Japan. Geriatr Gerontol Int. 2021;21:39–42.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Ser A, Biol Sci Med Sci. 2001;56:M146–156.
Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K. Validity and reliability of the Edmonton Frail Scale. Age Ageing. 2006;35:526–9.
Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal 2001;1:323–36.
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet 2019;394:1365–75.
Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14:392–7.
Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16:601–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Toba, A., Ishikawa, J. Current topics of frailty in association with hypertension and other medical conditions. Hypertens Res 46, 1188–1194 (2023). https://doi.org/10.1038/s41440-023-01200-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-023-01200-6