Abstract
Purpose
CCHS is an extremely rare congenital disorder requiring artificial ventilation as life support. Typically caused by heterozygous polyalanine repeat expansion mutations (PARMs) in the PHOX2B gene, identification of a relationship between PARM length and phenotype severity has enabled anticipatory management. However, for patients with non-PARMs in PHOX2B (NPARMs, ~10% of CCHS patients), a genotype–phenotype correlation has not been established. This comprehensive report of PHOX2B NPARMs and associated phenotypes, aims at elucidating potential genotype–phenotype correlations that will guide anticipatory management.
Methods
An international collaboration (clinical, commercial, and research laboratories) was established to collect/share information on novel and previously published PHOX2B NPARM cases. Variants were categorized by type and gene location. Categorical data were analyzed with chi-square and Fisher’s exact test; further pairwise comparisons were made on significant results.
Results
Three hundred two individuals with PHOX2B NPARMs were identified, including 139 previously unreported cases. Findings demonstrate significant associations between key phenotypic manifestations of CCHS and variant type, location, and predicted effect on protein function.
Conclusion
This study presents the largest cohort of PHOX2B NPARMs and associated phenotype data to date, enabling genotype–phenotype studies that will advance personalized, anticipatory management and help elucidate pathological mechanisms. Further characterization of PHOX2B NPARMs demands longitudinal clinical follow-up through international registries.
Similar content being viewed by others
INTRODUCTION
Congenital central hypoventilation syndrome (CCHS) (OMIM 209880) is a rare neurocristopathy and disorder in the autonomic control of breathing,1 with fewer than 2,000 published or reported cases.2 Clinical features of CCHS include a control of breathing deficit and hypoventilation, symptoms of autonomic nervous system (ANS) dysregulation (ANSD), and association in a subset of cases with anatomic ANSD (including Hirschsprung disease [HSCR] and neural crest tumors).2 In 2003, pathogenic variants in the paired-like homeobox 2B (PHOX2B) gene were identified in CCHS3,4 and are now considered requisite to a CCHS diagnosis.2 This gene encodes a transcription factor known to play a key role in the early embryologic development of the ANS5,6 including the sympathetic, parasympathetic, and enteric branches.7
Around 90% of individuals with CCHS will be heterozygous for a PHOX2B polyalanine repeat expansion mutation (PARM) in the third of three PHOX2B exons. The wild-type polyalanine repeat is 20 consecutive alanines on each allele. CCHS-associated PHOX2B PARMs have 24–33 alanine repeats on the affected allele. Among individuals with PARMs, those with longer expansions generally have more severe CCHS phenotypes, including need for continuous artificial ventilation (in contrast to asleep only), increased number of ANSD symptoms and affected organ systems,8,9 and incidence of neural crest tumors and HSCR.4,10 This established PHOX2B PARM genotype–CCHS phenotype relationship has allowed for anticipatory management (artificial ventilation needs for life support, screening for prolonged cardiac sinus pauses, HSCR, neural crest tumors, and more), leading to more customized and improved management based on the patient’s specific genotype.
In addition to PARMs, a diverse spectrum of variants located throughout the PHOX2B gene are also associated with CCHS. These variants, termed nonpolyalanine repeat mutations (NPARMs), cause the remaining ~10% of CCHS cases and have variable predicted impact on protein function. Based on existing literature, it is clear some, but not all, NPARMs result in severe phenotypes with high risk of extensive HSCR (aganglionosis of the large and in a subset the small intestine), malignant neural crest tumor, and need for continuous (awake and asleep) artificial ventilation.2,11,12 This literature also demonstrates that specific phenotypes and groupings of phenotypes within individuals (such as CCHS plus HSCR) may be more prevalent with specific types of NPARM variants, hinting at the potential to identify informative genotype–phenotype correlations in NPARM patients. However, due to the rarity of CCHS and in particular PHOX2B NPARMs, the phenotypes caused by specific NPARMs and types of NPARMs remain poorly characterized. As such, it is unknown if a clear genotype–phenotype relationship that could inform anticipatory management exists for NPARM patients. A better understanding of this relationship would require a more extensive cohort of PHOX2B NPARMs than previously published, and consideration of the potential deleterious effects of specific NPARM subtypes.
A large proportion of identified PHOX2B NPARMs are loss-of-function (LOF) variants, expected to lead to a state of haploinsufficiency. Recent work has demonstrated that some truncated PHOX2B proteins also exert dominant-negative effects13,14,15,16,17 on the wild-type protein, potentially exacerbating the phenotype. However, nonsense-mediated decay (NMD) is a physiological quality control pathway that will degrade messenger RNAs (mRNAs) resulting from premature truncation or frameshift.18,19 As many of the LOF PHOX2B NPARMs cause premature truncation, it is expected that NMD may play a pivotal role in limiting the potentially detrimental dominant-negative effects of the truncated proteins. We hypothesize that since LOF variants affecting the last exon of a gene are less likely to trigger NMD, this mechanism may be more effective at limiting the impact of early (exon 1 and exon 2) PHOX2B NPARMs.
The aim of this study was to more thoroughly explore the potential PHOX2B NPARM genotype–phenotype relationships, with the ultimate goal of optimizing and personalizing patient care and management. Given the large number of clinical, research, and commercial laboratories currently offering PHOX2B analysis and the rarity of patients with CCHS, we hypothesized that an expanded cohort of NPARMs for this analysis would require developing an international collaboration of PHOX2B testing labs. To evaluate the PHOX2B NPARM genotype–phenotype relationship, this study considered the expected protein effects of the different subtypes of PHOX2B NPARMs. We hypothesized that missense and in-frame insertion/deletion (indel) PHOX2B NPARMs may lead to a less severe phenotypic spectrum as compared to LOF variants (nonsense and frameshift variants). In light of the recent work demonstrating dominant-negative NPARM effects, we also hypothesized that LOF NPARMs in exon 3 may cause a more severe phenotypic spectrum than LOF NPARMs in exons 1 and 2, due to their likelihood to escape NMD mechanisms.
MATERIALS AND METHODS
Study design
All known laboratories worldwide that conduct PHOX2B testing were identified and contacted to request collaboration on this project. These included 49 laboratories (18 clinical academic laboratories, 20 commercial laboratories, 11 research laboratories), identified from www.genetests.org and peer-reviewed publications reporting a PHOX2B NPARM case. Two authors (A.Z., D.E.W.-M.) contacted the director of each laboratory to discuss the project, determine if they had identified any PHOX2B NPARMs, and if yes, to request participation. The lead site Ann & Robert H. Lurie Children’s Hospital of Chicago’s Institutional Review Board (IRB) provided oversight in accordance with regulations and permitted sharing of de-identified data between laboratories and the lead site through research collaboration agreements.
Genetic data
A full list of PHOX2B NPARMs contributed by the participating sites were recorded, including available information for the patient’s phenotype and PHOX2B genotype. Additionally, all published PHOX2B NPARMs as of 1 March 2020 were added to the master database for further analysis. The full list of PHOX2B variants were examined for their impact on the protein’s coding, and categorized as frameshift, missense, nonsense, stop loss, in-frame indels (insertions and deletions), full exon/gene deletion, and splice site variants according to traditional definitions. Of note, due to challenges involved with accurate sequence detection in the repetitive polyalanine tract region, it is essential to carefully assess each variant call in the PHOX2B gene to determine that the right variant nomenclature was assigned.4,19,20 This is especially relevant for published PHOX2B literature where inconsistent nomenclature usage may prevent accurate categorization of the variants.21 One case, previously reported as c.693_708ins16mers, was excluded from tables, figures, and analysis because precise genetic information on the variant was not obtainable to allow accurate prediction of the protein coding effect.22 Four cases23 were excluded from the tables, figures, and analysis due to both high population frequency of variants (gnomAD database)24 and previous documentation that indicated they were not likely to be pathogenic (ClinVar database).25 An additional two synonymous variants were removed from the tables, figures, and analysis since they were not predicted to impact transcript splicing, do not lead to any protein coding change, and therefore are more likely to be a benign genetic polymorphism.26 The remaining cohort includes 295 cases.
Phenotype data
For data collection, an Excel spreadsheet was provided to each laboratory director requesting de-identified phenotypic information. Additionally, available phenotype information for all published PHOX2B NPARMs as of 1 March 2020 were added to the master database. For PHOX2B NPARMs identified at the three primary study sites (Ann & Robert H. Lurie Children’s Hospital of Chicago [abbreviated Lurie Children’s Hospital], Rush University Medical Center, and Ambry Laboratories), pertinent data from laboratory order forms, available medical records, and shared email referrals or notes from phone and/or virtual consultation with one author (DEW-M) were included in the database.
PHOX2B fragment analysis, sequencing, and multiplex ligation-dependent probe amplification testing
For cases that were tested at our lead site, details regarding genetic testing methodology have been reported previously.4,19,27
PHOX2B NPARMs variant categorization
De-identified clinical information and PHOX2B genetic testing results were compiled from the various sources into one master spreadsheet for analysis purposes. With the aid of variant analysis software Alamut Visual version 2.14 (Interactive Biosoftware, Rouen, France), the NPARMs were separated into the following categories: missense, nonsense, frameshift, stop loss, in-frame indels (in-frame insertions, deletions, or duplications), full exon/gene deletions, and splice site variants. Variants were assessed with Alamut Visual using the PHOX2B hg19 reference transcript (NM_003924.3) and were additionally manually inspected and evaluated by the authors through standards and guidelines for interpretation of sequence variants established by the American College of Medical Genetics and Genomics and the Association for Molecular Pathology.28 All patients were grouped by NPARM variant category and associated phenotypes were considered for each group.
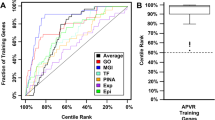
PHOX2B NPARM variant grouping by expected effect on protein function
In addition to the above variant categories, all NPARMS were manually inspected and grouped by a member of the study team (K.L.Y.) according to anticipated variant effects on function of the translated protein (Table 1). The analysis focuses on the potential impact of these four groups: (1) missense variants and in-frame indels, (2) LOF variants likely to trigger NMD due to their location in exons 1 and 2, (3) LOF variants in exon 3 that are not likely to trigger NMD, and (4) full exon/gene deletion (Table 1). These categories were used for additional analysis to determine if this type of variant grouping would allow better distinction between groupings that might afford anticipatory management.
Statistical methods
PHOX2B NPARMs were summarized by the variant classification, using mean with standard deviation or median with interquartile range (IQR) for continuous variables, and counts with percentages for categorical variables. Differences between variant classifications were evaluated with chi-square or Fisher’s exact test for categorical variables. Statistical significance was established at a significance level of 0.05 for two-tailed tests and no adjustments were made for multiplicity due to small sample size attributable to the rarity of CCHS and extreme rarity of NPARMs. Further post hoc testing was performed for pairwise comparisons of the significant variables, using a Bonferroni correction for multiple comparisons. All analyses were performed in R version 3.6.1.
Ethics statement
The lead site Ann & Robert H. Lurie Children’s Hospital of Chicago’s Institutional Review Board (IRB) provided oversight in accordance with regulations and permitted sharing of de-identified data between laboratories and the lead site, through research collaboration agreements. The study was approved by Ann & Robert H. Lurie Children’s Hospital of Chicago’s IRB (project number 2013-15273).
RESULTS
Patient cohort
Responses were received from 22 laboratories, including 9 clinical academic, 6 commercial, and 7 research laboratories (response rate = 45%). Among these, 11 laboratories had at least one PHOX2B NPARM case to contribute to the collaboration. Response rates from the clinical academic, commercial, and research laboratories were 50%, 30%, and 64%, respectively. Twenty-two percent of the NPARM samples were provided by the Molecular Diagnostics Laboratories at Lurie Children’s Hospital of Chicago (Northwestern University) and Rush University Medical Center, and 22% of NPARM samples were provided by Ambry Genetics, a commercial laboratory. Fourteen percent of the NPARM samples were provided by individual research laboratories worldwide. The remaining 42% of NPARMs were cases identified from the literature. Three hundred two individuals with PHOX2B NPARMs were identified; 139 (46%) of these were previously unreported in the literature. Among these, 295 patients were identified as having likely pathogenic PHOX2B NPARMs and were considered in further analysis. Two hundred six (70%) of the individuals were patients with the characteristic CCHS-related respiratory phenotype (hypoventilation/apnea). In the remaining 89 individuals, there was insufficient phenotype information available to confirm the respiratory phenotype, despite request for PHOX2B testing and confirmation of Hirschsprung disease and neural crest tumors. Among all PHOX2B NPARMS, there were 39 families where more than one affected family member had the pathogenic variant. In families where comprehensive phenotypic information was available for each of the family members who inherited the NPARM, we observed high penetrance of the variants in causing an observable respiratory phenotype, with variable expressivity of the other potentially accompanying features. The median (IQR) age at identification was 0.73 (0.09 to 3.48) years in published cases and 0.20 (0.08 to 8.25) years in laboratory referral cases (p = 0.30). The median (IQR) age at last reported clinical information was 3.00 (0.25 to 10.25) years in published cases and 1.86 (0.08 to 12.49) years in laboratory referral cases (p = 0.44).
Phenotypes associated with individual NPARMs
Among the 295, there were 135 unique NPARM variants identified, 58 (43%) of which have not been previously reported in the literature. While the majority of these NPARMs have only been reported in one patient, 45 (33%) of the unique NPARM variants have now been identified in more than one patient. A subset of the NPARMs seem to be repetitively identified, with up to 35 cases reported with the same NPARM (c.691_698dup). It is important to note that individual NPARMs (such as c.691_698dup) show variable expressivity of disease phenotype. Individual NPARMs were grouped to allow more complete information in consideration of possible phenotypes associated with specific NPARMs (Table S1; references for all citations in this table are provided in the Supplement).
Description of PHOX2B NPARM variant types
NPARMs were grouped by variant type and subcategorized by variant location. The number of previously and newly reported variants and cases for each category is presented in Table 2. Available phenotypic details associated with each category are provided in Table 3. Artificial ventilation in Tables 3 and 4 refers to clinical information indicating the patient’s level of needed respiratory life support. The “sleep only” column indicates those individuals where it was clear artificial ventilation was needed during sleep only rather than wakefulness and sleep.
Genotype–phenotype correlation for NPARMs grouped by predicted effect of protein
Table 4 provides a breakdown of phenotypic features based on predicted effect on translated protein (as defined in Table 1). Between the four grouped NPARM types, there are significant differences in prevalence for the following phenotypic features: respiratory hypoventilation (p = 0.012), later-onset CCHS (LO-CCHS) (diagnosis after one month of age) (p = 0.002), artificial ventilatory need of continuous ventilation versus sleep only (p < 0.001), gastrointestinal (GI) symptoms (p < 0.001), Hirschsprung disease (p = 0.001), extent of Hirschsprung disease (p = 0.006), and neural crest tumors (p = 0.041) (Table 4). Pairwise comparison of individual NPARM groupings during post hoc analysis identified several significant differences (Table 5). As no significant differences were identified between whole-gene/whole-exon deletions and other variant categories, the whole-gene/whole-exon category was not included in the reported post hoc results (Table 5).
DISCUSSION
These results represent the efforts of a collaboration between clinical, research, and commercial laboratories developed to advance knowledge and treatment of an extremely rare disorder. Since 2003 both clinical and research testing of the PHOX2B gene has been available. Prior to this report, 158 cases of disease-associated PHOX2B NPARMs have been identified and published in the literature (Table S1). The cohort presented here will nearly double the number of reported disease-associated PHOX2B NPARMs in the literature. Sharing of the knowledge about specific NPARMs that are associated with CCHS phenotypes will improve genetic diagnosis of the disease. Grouping individual patients by the genetic characteristics of individual NPARMs may allow us to use additional information to guide the clinical management of newly identified NPARM cases (Table S1). This expanded cohort has potential to both advance knowledge of disease mechanisms and allow improved anticipatory management for these vulnerable ventilator-dependent patients with CCHS.
Prior studies considering PHOX2B NPARMs have reported associations between traditional variant categories and risk of specific phenotypes.11,12,16,27,29 Our findings are in line with the findings of these previous publications, but substantially expand the size of the cohort and provide more detailed analysis based on the PHOX2B exon location of the variants, due to the predicted effects on NMD. For instance, our results support previous findings that patients with NPARMs in PHOX2B are at very high risk for tumors of neural crest origin. It expands on these findings by establishing that a wide variety of types of NPARMs, including frameshift, missense, nonsense, stop loss, and full exon or full gene deletions, can lead to these tumors. This is in contrast to the more common PARMs in PHOX2B, where only expansions of specific lengths seem to predispose to tumor risk.2 This knowledge can guide clinicians in suggesting plans for ongoing imaging in patients with PHOX2B NPARMs, potentially allowing earlier tumor detection and more effective intervention.
In addition to grouping variants by type (missense, nonsense, etc.), our study grouped the identified variants by expected impact on protein function to determine if such groupings could better inform anticipatory management of NPARM cases. These groupings were rendered based on a combination of outputs from genetic prediction software, prior cellular studies evaluating the cellular effects of specific NPARMs, and manual evaluation by a laboratory geneticist. Based on the results of our study, LOF variants located in exon 3 of PHOX2B are associated with a more severe clinical outcome as compared to missense and in-frame indels, or LOF variants located in exon 1 and 2. It is anticipated that these variants, occurring near the amino acids C-terminus, are less likely to undergo NMD and that the persistence of the aberrant PHOX2B protein may exert a dominant-negative effect on the function of the wild-type protein and serve to aggravate the cellular dysfunction. Of note, many of these variants in exon 3 are frameshift variants that also cause an extension of the resulting protein length. This is in line with previous in vitro study.16 Further, prior studies reported that frameshift variants in exon 3 result in a severe phenotype with extensive aganglionosis (HSCR) of the large and often small intestine, increased risk of malignant neural crest tumors, and need for continuous artificial ventilation but did not present a hypothesis of the possible mechanisms.2,11,12 Our results support these findings and expand knowledge on the expected phenotypic consequences of LOF variants, including frameshift and other PHOX2B exon 3 NPARMs.
Additionally, our study considered the phenotypic consequences of early LOF variants located in exon 1 and 2 of the PHOX2B gene. These variants may be more likely to trigger NMD of the aberrant transcript, leading to absence of the abnormal protein.18,30 This is expected to result in a functional effect similar to a heterozygous full-gene deletion, with potential for haploinsufficiency as the disease-causing mechanism. The existence of several familial cases of CCHS or LO-CCHS with heterozygous deletion of the PHOX2B gene strongly supports the potential of PHOX2B haploinsufficiency as a disease-causing mechanism.27 As in patients with whole-gene or whole-exon deletion of PHOX2B, these early LOF variants resulted in less risk for severe CCHS phenotype, including risk for tumors of neural crest origin in our analysis. This result is in line with previous reports that found frameshift NPARMs occurring in exons 1 and 2 to be associated with a milder form of CCHS and later average age of onset (LO-CCHS).12,31 Here we expand the knowledge of this to also include LOF variants that create an immediate premature stop codon (nonsense) in exons 1 and 2 of PHOX2B, as these variants together with frameshift variants in exons 1 and 2 are more likely to be associated with later-onset presentation. However, in vitro studies have shown that some nonsense variants occurring in this region may undergo rescue mechanisms and avoid complete LOF of the protein.32 Instead, these variants have been shown to result in proteins that localize to the nucleus and activate transcription of the same target genes as the wild-type protein, likely due to reinitiation of translation downstream from the premature stop codon.32 Additional in vitro studies of NPARMs are needed to determine their pathophysiological mechanism, which will allow for more accurate categorization of the variants, with the goal of improving our ability to anticipate development of certain features in patients with CCHS.
Despite the comprehensive nature of this patient cohort, we identify five limitations to this research. First, phenotypic frequencies reported in this study may underestimate their true prevalence at presentation. Clinicians and ordering laboratories often partially report phenotypic information on PHOX2B requisition forms, including positive symptoms and characteristics of the respiratory phenotype, and failing to confirm the absence of additional symptoms (e.g., Hirschsprung disease), as evidenced by blanks. Second, phenotype at the time of PHOX2B genetic testing, typically ordered in the first few days of life, is not necessarily representative of the child’s full phenotype potential (e.g., presence or absence of tumor or cardiac rhythm abnormalities), or evolution of ventilatory support.33,34,35,36 Though this may result in overestimation of the severity of the respiratory phenotype if only newborn information is included, incomplete phenotypic information is commonly encountered in studies with retrospective data acquisition, but the data are still extremely valuable for rare pediatric genetic conditions like CCHS. Third, variable follow-up length is an issue for laboratories as well as published case reports. However, ages at identification and ages at last reported clinical information were not statistically significantly different between published cases and laboratory referral cases. Nonetheless, a variable subset of patients with limited clinical information from lab requisition forms and published literature may have changes in the level of respiratory support, or emergence of neural crest tumors and cardiac rhythm abnormalities at a later age. Taken together, this might inadvertently lead to reporting bias and overestimation or underestimation of the effects of certain variants or categories of variants, hence the current recommendations for continual surveillance including cardiac rhythm abnormalities, neural crest tumors, and ventilatory needs awake and asleep. Fourth, the utility of additional analysis such as logistic regression and subgroup analysis by age was hindered by the incomplete phenotype reporting. Improved longitudinal collection of clinical data in association with PHOX2B gene testing has the potential to improve accuracy of CCHS phenotype disease prognostication and personalization of management. Fifth, due to the association of certain types of PHOX2B NPARMs with a more severe constellation of symptoms and inherent patient fragility, there is the potential for ascertainment bias, in which patients with a more severe CCHS phenotype will be more likely to require medical management, and this may have led to more frequent detection of more severe PHOX2B NPARMs. Despite these limitations, the variability/heterogeneity of this large cohort does not limit the feasibility and reliability of a genotype–phenotype correlation that can be used to advance personalized, anticipatory management and help elucidate pathological mechanisms.
In conclusion, our study outlines the immense genotypic and phenotypic variability associated with CCHS PHOX2B NPARM cases that makes the diagnosis and prediction of an individual’s disease course complex. It also highlights the need to rule out the presence of pathogenic PHOX2B variants in all suspected cases of CCHS, as the genetic information may allow more comprehensive management of the patients beginning in the neonatal period. Due to the propensity for the manifestation of LO-CCHS based on certain genetic variants of PHOX2B and the autosomal dominant inheritance pattern, it is important to implement parental testing (including assessment for mosaicism) once a proband has been identified to have a pathogenic PHOX2B variant. Efforts to more accurately genotype PHOX2B disease-associated variants in CCHS patients will enable us to obtain a more precise genotype–phenotype correlation among individuals with NPARMs, allowing for optimized care and outcomes, as well as an increased understanding of the pathogenic mechanisms underlying these various variant types. Results are meant to guide clinicians, genetic counselors, and families to understand the potential most severe phenotypic manifestations of each PHOX2B variant, with appreciation that there is always the potential for variable expressivity and penetrance. In this study, stratifying variants by type and predicted protein effect accounted for differences in prevalence of LO-CCHS, Hirschsprung disease, tumors of neural crest origin, and artificial ventilatory needs. More specifically, our data support the premise that LOF variants located in the exon 3 of PHOX2B are a strong predictor of a more severe CCHS clinical picture. In conclusion, due to the rarity of CCHS and the incomplete phenotypic features in neonatal CCHS patients, it is essential that adequate follow-up of the clinical course by specialty members of the medical team is maintained with continual longitudinal sharing of information across an international registry. As this valuable database (https://clinicaltrials.gov/ct2/show/NCT03088020) continues to grow, we expect accurate genotypic information on PHOX2B disease-associated variants to be instrumental in guiding personalized medical management of these patients with CCHS, with the ultimate aim of decreasing disease burden.
Data availability
The authors are supplying their data in Supplement Table S1 for public access.
References
Mellins, R. B., Balfour, H. H. Jr., Turino, G. M. & Winters, R. W. Failure of automatic control of ventilation (Ondine’s curse). Report of an infant born with this syndrome and review of the literature. Medicine (Baltimore). 49, 487–504 (1970).
Weese-Mayer, D. E. et al. An official ATS clinical policy statement: Congenital central hypoventilation syndrome: genetic basis, diagnosis, and management. Am. J. Respir. Crit. Care Med. 181, 626–644 (2010).
Amiel, J. et al. Polyalanine expansion and frameshift mutations of the paired-like homeobox gene PHOX2B in congenital central hypoventilation syndrome. Nat. Genet. 33, 459–461 (2003).
Weese-Mayer, D. E. et al. Idiopathic congenital central hypoventilation syndrome: analysis of genes pertinent to early autonomic nervous system embryologic development and identification of mutations in PHOX2b. Am. J. Med. Genet. A. 123A, 267–278 (2003).
Pattyn, A., Morin, X., Cremer, H., Goridis, C. & Brunet, J. F. Expression and interactions of the two closely related homeobox genes Phox2a and Phox2b during neurogenesis. Development. 124, 4065–4075 (1997).
Pattyn, A., Morin, X., Cremer, H., Goridis, C. & Brunet, J. F. The homeobox gene Phox2b is essential for the development of autonomic neural crest derivatives. Nature. 399, 366–370 (1999).
Howard, M. J. Mechanisms and perspectives on differentiation of autonomic neurons. Dev. Biol. 277, 271–286 (2005).
Weese-Mayer, D. E. et al. Case/control family study of autonomic nervous system dysfunction in idiopathic congenital central hypoventilation syndrome. Am. J. Med. Genet. 100, 237–245 (2001).
Marazita, M. L. et al. Genetic segregation analysis of autonomic nervous system dysfunction in families of probands with idiopathic congenital central hypoventilation syndrome. Am. J. Med. Genet. 100, 229–236 (2001).
Matera, I. et al. PHOX2B mutations and polyalanine expansions correlate with the severity of the respiratory phenotype and associated symptoms in both congenital and late onset central hypoventilation syndrome. J. Med. Genet. 41, 373–380 (2004).
Trochet, D. et al. PHOX2B genotype allows for prediction of tumor risk in congenital central hypoventilation syndrome. Am. J. Hum. Genet. 76, 421–426 (2005).
Berry-Kravis, E. M., Zhou, L., Rand, C. M. & Weese-Mayer, D. E. Congenital central hypoventilation syndrome: PHOX2B mutations and phenotype. Am. J. Respir. Crit. Care Med. 174, 1139–1144 (2006).
Nagashimada, M. et al. Autonomic neurocristopathy-associated mutations in PHOX2B dysregulate Sox10 expression. J. Clin. Invest. 122, 3145–3158 (2012).
Di Lascio, S., Bachetti, T., Saba, E., Ceccherini, I., Benfante, R. & Fornasari, D. Transcriptional dysregulation and impairment of PHOX2B auto-regulatory mechanism induced by polyalanine expansion mutations associated with congenital central hypoventilation syndrome. Neurobiol. Dis. 50, 187–200 (2013).
Di Lascio, S., Belperio, D., Benfante, R. & Fornasari, D. Alanine expansions associated with congenital central hypoventilation syndrome impair PHOX2B homeodomain-mediated dimerization and nuclear import. J. Biol. Chem. 291, 13375–13393 (2016).
Di Lascio, S. et al. Structural and functional differences in PHOX2B frameshift mutations underlie isolated or syndromic congenital central hypoventilation syndrome. Hum. Mutat. 39, 219–236 (2018).
Pei, D., Luther, W., Wang, W., Paw, B. H., Stewart, R. A. & George, R. E. Distinct neuroblastoma-associated alterations of PHOX2B impair sympathetic neuronal differentiation in zebrafish models. PLoS Genet. 9, e1003533 (2013).
Lindeboom, R. G. H., Vermeulen, M., Lehner, B. & Supek, F. The impact of nonsense-mediated mRNA decay on genetic disease, gene editing and cancer immunotherapy. Nat. Genet. 51, 1645–1651 (2019).
Jennings, L. J., Yu, M., Zhou, L., Rand, C. M., Berry-Kravis, E. M. & Weese-Mayer, D. E. Comparison of PHOX2B testing methods in the diagnosis of congenital central hypoventilation syndrome and mosaic carriers. Diagn. Mol. Pathol. 19, 224–231 (2010).
Horiuchi, H. et al. Sensitive detection of polyalanine expansions in PHOX2B by polymerase chain reaction using bisulfite-converted DNA. J. Mol. Diagn. 7, 638–640 (2005).
den Dunnen, J. T. et al. HGVS recommendations for the description of sequence variants: 2016 update. Hum. Mutat. 37, 564–569 (2016).
Ou-Yang, M. C. et al. Concomitant existence of total bowel aganglionosis and congenital central hypoventilation syndrome in a neonate with PHOX2B gene mutation. J. Pediatr. Surg. 42, e9–e11 (2007).
Bachetti, T. & Ceccherini, I. PHOX2B (paired‐like homeobox 2b). Atlas Genet. Cytogenet. Oncol. Haematol. 17, 740–745 (2013).
Karczewski, K. J. et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature. 581, 434–443 (2020).
Landrum, M. J. et al. ClinVar: improving access to variant interpretations and supporting evidence. Nucleic Acids Res. 46, D1062–D1067 (2018).
Raabe, E. H. et al. Prevalence and functional consequence of PHOX2B mutations in neuroblastoma. Oncogene. 27, 469–476 (2008).
Jennings, L. J. et al. Variable human phenotype associated with novel deletions of the PHOX2B gene. Pediatr. Pulmonol. 47, 153–161 (2012).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 17, 405–424 (2015).
Bachetti, T. & Ceccherini, I. Causative and common PHOX2B variants define a broad phenotypic spectrum. Clin. Genet. 97, 103–113 (2020).
Lindeboom, R. G., Supek, F. & Lehner, B. The rules and impact of nonsense-mediated mRNA decay in human cancers. Nat. Genet. 48, 1112–1118 (2016).
Bygarski, E., Paterson, M. & Lemire, E. G. Extreme intra-familial variability of congenital central hypoventilation syndrome: a case series. J. Med. Case Rep. 7, 117 (2013).
Cain, J. T. et al. Nonsense pathogenic variants in exon 1 of PHOX2B lead to translational reinitiation in congenital central hypoventilation syndrome. Am. J. Med. Genet. A. 173, 1200–1207 (2017).
Sasaki, A. et al. Novel PHOX2B mutations in congenital central hypoventilation syndrome. Pediatr. Int. 61, 393–396 (2019).
Low, K. J. et al. A case of congenital central hypoventilation syndrome in a three-generation family with non-polyalanine repeat PHOX2B mutation. Pediatr. Pulmonol. 49, E140–E143 (2014).
Byers, H. M., Chen, M., Gelfand, A. S., Ong, B., Jendras, M. & Glass, I. A. Expanding the phenotype of congenital central hypoventilation syndrome impacts management decisions. Am. J. Med. Genet. A. 176, 1398–1404 (2018).
Katwa, U. et al. Atypical presentations associated with non-polyalanine repeat PHOX2B mutations. Am. J. Med. Genet. A. 176, 1627–1631 (2018).
Acknowledgements
The authors appreciate the cooperation with the laboratories worldwide that contributed PHOX2B NPARMs to this manuscript. Funding sources include Northwestern University Feinberg School of Medicine Area of Scholarly Concentration (AOSC) Fellow (SMH) and the Chicago Community Trust Foundation PHOX2B Patent Fund (CMR).
Author information
Authors and Affiliations
Contributions
Conceptualization: A.Z., C.M.R., D.E.W-M. Data curation: A.Z., C.M.R., D.E.W-M., S.M.H., E.M.B-K., L.Z., V.S., P.R., L.J.J., M.Y., K.L.Y., I.C., T.B., M.P. Formal analysis: A.Z., C.M.R., D.E.W-M., S.M.H., K.L.Y. Funding acquisition: D.E.W-M., S.M.H., C.M.R. Investigation: A.Z., C.M.R., D.E.W-M., S.M.H., G.N., E.M.B-K., L.Z., V.S., P.R., L.J.J., M.Y., K.L.Y., I.C., T.B., M.P. Methodology: A.Z., C.M.R., D.E.W-M., S.M.H., E.M.B-K., K.L.Y. Project administration: A.Z., C.M.R., D.E.W-M. Resources: A.Z., C.M.R., D.E.W-M., E.M.B-K., L.Z., V.S., P.R., L.J.J., M.Y., K.L.Y., I.C., T.B., M.P. Supervision: A.Z., C.M.R., D.E.W-M. Validation: A.Z., C.M.R., D.E.W-M., K.L.Y. Visualization: A.Z., C.M.R., D.E.W-M., K.L.Y., S.M.H., E.M.B-K., I.C., T.B. Writing—original draft: A.Z., S.M.H., G.N., D.E.W-M., C.M.R., K.L.Y. Writing—review & editing: A.Z., C.M.R., D.E.W-M., K.L.Y., I.C., T.B., S.M.H., G.N., E.M.B-K., L.Z., V.S., P.R., L.J.J., M.Y., M.P.
Corresponding author
Ethics declarations
Ethics Declaration
The lead site Ann & Robert H. Lurie Children’s Hospital of Chicago’s Institutional Review Board (IRB) approved this study under project number 2013-15273 and provided oversight in accordance with regulations and permitted sharing of de-identified data between laboratories and the lead site, through research collaboration agreements. Informed consent was not required because the IRB waived this requirement for obtaining informed consent under 45 CFR 46.116(d).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhou, A., Rand, C.M., Hockney, S.M. et al. Paired-like homeobox gene (PHOX2B) nonpolyalanine repeat expansion mutations (NPARMs): genotype–phenotype correlation in congenital central hypoventilation syndrome (CCHS). Genet Med 23, 1656–1663 (2021). https://doi.org/10.1038/s41436-021-01178-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41436-021-01178-x
This article is cited by
-
Computer-aided diagnostic screen for Congenital Central Hypoventilation Syndrome with facial phenotype
Pediatric Research (2024)
-
Neurocognition as a biomarker in the rare autonomic disorders of CCHS and ROHHAD
Clinical Autonomic Research (2023)
-
Transitional care and clinical management of adolescents, young adults, and suspected new adult patients with congenital central hypoventilation syndrome
Clinical Autonomic Research (2023)