Abstract
Background/Objectives
To assess systemic associations of angioid streaks (AS) using a large US healthcare database.
Subjects/Methods
A retrospective cross-sectional study was conducted of patients diagnosed with AS in a large, national US insurer from 2000–2019. Cases were matched 1:5 to controls. The prevalence rates of established associated disease states and other systemic diseases were calculated and compared using logistic regression. Additionally, the rate of anti-VEGF treatment was assessed as a proxy for the incidence of choroidal neovascularization (CNV).
Results
One thousand eight hundred fifty-two cases of AS and 9028 matched controls were included. The rates of association between AS and the well-characterized conditions included: Pseudoxanthoma elasticum (PXE)—228 patients (12.3%), Ehlers–Danlos syndrome—18 patients (1.0%), Paget’s disease—6 patients (0.3%), hemoglobinopathies—30 patients (1.6%), and idiopathic—1573 patients (84.9%). There was a statistically higher prevalence of the following less classically associated diseases among patients with AS compared to controls: hereditary spherocytosis (1.7% vs. 0.6%, p < 0.001), connective tissue disease (1.0% vs 0.3%, p < 0.001) and non-exudative age-related macular degeneration (33.9% vs 10.6%, p < 0.001). Among 1442 eligible cases analyzed, 427 (29.6%) received at least 1 anti-VEGF injection with 338 (23.4%) patients having the injection after their AS diagnosis.
Conclusions
In the largest collection of AS patients to date, the classical teaching of systemic disease associations occur at rates far, far lower than previously reported. The association of AS with other less reported diseases highlights new potential associations and may contribute to the understanding of AS formation.
Similar content being viewed by others
Introduction
An angioid streak (AS) is a linear, crack-like dehiscence in a brittle, thickened and calcified Bruch’s membrane (BrM). Clinically, they are described as irregular jagged lines in the fundus that are reddish or brownish in appearance and often radiate from the optic nerve head and spread centrifugally to the periphery [1, 2] Mechanical stress is thought to cause breakage of the brittle BrM, leading to AS formation [3] In the early stages of AS, a thickening of BrM with a decrease of the pigment granules, pigment stripping, mottling or formation of pigment clumps in the retinal pigment epithelium (RPE) can occur. These findings may co-exist with a disruption in the overlying layers of the retina and the underlying choriocapillaris [4]. In advanced stages of disease, AS may cause RPE atrophy and affect photoreceptors [1, 5].
Angioid streaks may be associated with systemic diseases, which are classically described by the mnemonic, PEPSI, including Pseudoxanthoma elasticum (P), Ehlers–Danlos syndrome (E), Paget disease of the bone (P), Sickle cell disease (S) and Idiopathic (I) entities. The association of AS with systemic and ocular diseases is markedly important because some of these diseases are sight- or life-threatening [5]. Classically, studies have suggested that more than 50% of patients with AS have one of the underlying associated systemic disease that define PEPSI [5]. To date, the association between AS and systemic diseases has been primarily documented in case reports and case series, with the incidence of AS association in each disease extracted from selected disease-categorized cohorts [6,7,8,9,10,11,12,13,14,15,16,17,18,19].
Furthermore, choroidal neovascularization (CNV) is a frequent complication of AS [1]. Reports have suggested the incidence of secondary CNV formation can be as high as 86% in one eye, and up to 71% bilaterally [5, 20]. Additional studies have suggested a connection between AS and age-related macular degeneration (AMD), both of which can be complicated by CNV [21, 22]. In this study, we utilized a US medical claims database to determine the relative prevalence of disease-dependent associations among a cohort of AS patients. Systemic diseases assessed were based on previous reports in the literature [6,7,8,9,10,11,12,13,14,15,16,17,18,19]. Of note, we also evaluated the prevalence of non-exudative age-related macular degeneration (AMD) to evaluate the hypothesis that these diseases may have an overlapping pathophysiology. Next, we assessed the rate of anti-VEGF use in the AS cohort as a proxy for how frequently CNV occurs.
Materials/subjects and methods
Dataset
All data were abstracted from Optum’s de-identified Clinformatics® Data Mart Database which includes the medical claims of all beneficiaries from commercial and Medicare Advantage insurance plans obtained across all 50 states. Included within the database are all outpatient medical claims for office visit and their associated diagnoses, outpatient pharmaceutical prescriptions, and demographic data for each beneficiary during their enrollment in the insurance plan from April 1, 2000 to June 30, 2019. The University of Pennsylvania’s Institutional Review Board deemed this study exempt from review due to the de-identified nature of the data.
Cohorts
A cohort was created from all patients diagnosed with AS, as identified by ICD9 and ICD10 coding. Each patient was required to have at least 1 year in the database. Patients were excluded due to any history of a diagnosis of pathologic myopia or choroidal rupture as both diseases may have lacquer cracks and could be confused for AS. The initial part of the study then assessed how frequently each of pseudoxanthoma elasticum, Ehlers-Danlos syndrome, Paget’s disease, and sickle cell disease (which we included alpha and beta thalassemia in this group as hemoglobinopathies), the typical PEPSI conditions were found to be associated with AS. The next step in the analysis assessed less frequently thought of potential associations that had been published previously [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19, 23]. Please see Supplementary Table 1 for all the diseases included in this list as well as all of the ICD9 and ICD10 codes used throughout the study.
Next, to further assess how strong each of the associations found for the conditions analyzed above, a matched control group was created from all patients in the dataset who had at least one ophthalmology visit and did not have a diagnosis of AS. Cases were matched 1:5 to controls on age, sex, race, insurance eligibility period, and index year (year of office visit for controls or year of diagnosis for cases). Similar to cases, controls were excluded if they had less than 1 year in the insurance plan or had a diagnosis of AS, choroidal rupture or pathologic myopia. Conditional logistic regression was used to test differences in cross-sectional prevalence rates between cases and controls. Since many associations were being tested a Bonferroni correction was applied and all p values were adjusted such that only p values < 0.002 were considered significant.
Lastly, we assessed the impact of CNV in the AS cohort. To do this we assessed anti-VEGF use in all patients diagnosed on or after January 1, 2007. We further excluded any patients with additional diagnoses of anti-VEGF treated diseases. Statistical analysis was performed using SAS version 9.4 (SAS Institute) and R Version 3.5.1 (R Foundation for Statistical computing, Vienna, Austria).
Results
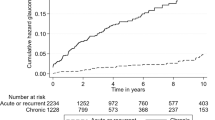
A total of 1852 cases (Fig. 1) met inclusion and exclusion criteria for evaluation. The mean age was 63.9 years of age for both groups. Nine thousand and twenty-eight controls were matched to the AS cases. The baseline characteristics of the AS cohort are demonstrated in Table 1. The number of patients and rates of association between AS and the well-characterized conditions of the PEPSI mnemonic are as follows: Pseudoxanthoma elasticum (PXE)—228 patients (12.3%), Ehlers–Danlos syndrome—18 patients (1.0%), Paget’s disease—6 patients (0.3%), hemoglobinopathies—30 patients (1.6%), and idiopathic, the largest group—1573 patients (84.9%). (See Table 2) Interestingly, all the diseases listed above occurred at a significantly higher rate in cases of AS than matched controls (p ≤ 0.001 for all comparisons), except Paget’s disease which was only slightly higher, but not significantly so (AS prevalence = 0.3%; Control prevalence = 0.2%, p = 0.43).
The prevalence rates of other previously documented systemic diseases among patients with AS versus controls are shown in Table 3. There was a statistically higher prevalence of the following less classically associated diseases among patients with AS compared to controls: hereditary spherocytosis (1.7% vs. 0.6%, p < 0.001), connective tissue disease (1.0% vs 0.3%, p < 0.001) and non-exudative age-related macular degeneration (33.9% vs 10.6%, p < 0.001) (Table 3).
One thousand four hundred and forty-two cases of AS were diagnosed after January 1, 2007, and did not have an ancillary anti-VEGF treated ocular diagnosis at any point before or after the AS diagnosis. Among these, 427 (29.6%) had at least 1 anti-VEGF injection (either before or after diagnosis), with 338 patients (23.4%) having the injection only after their AS diagnosis.
Discussion
The main objective for the present study was to validate the classic disease associations and to investigate the prevalence of other diseases among patients with AS. Using a large cohort of AS patients, we were able to confirm the strong association between Pseudoxanthoma elasticum (PXE) and AS: 12.3% of patients with angioid streaks carry a diagnosis of PXE. We were not however able to confirm the relative associations of the other classic PEPSI mnemonic diseases [5]. Of note, our study did not show a significant association between Paget’s disease and angioid streaks with controls only having a marginally lower prevalence rate (0.2%) compared to the rate within patients with angioid streaks (0.3%) (Table 2). Our study did show statistically higher rates of Ehlers–Danlos and hemoglobinopathies, which have historically been associated with AS [7,8,9,10,11, 13, 17, 23, 24], however, these diseases only occurred at rates of 1.0% and 1.6%, respectively. Furthermore, the rate of those AS with “idiopathic” AS was much, much higher (84.9%) than classically reported. The association of AS with other less reported diseases, like AMD may lend support to the possibility of other associations.
The “PEPSI” disease associations have been historically documented through case reports and case series. By using a large national database, our study aimed to validate these associations. Paget’s disease (osteitis deformans) has been described in case reports and diagnostic surveys with a prevalence rate of AS ranging from 1.4 to 15 percent with some studies suggesting its presence to represent a coincidence [6, 17, 18, 25, 26]. In Paget’s disease, bone deformities are associated with the binding of elastic fibers to calcium [7]. Terry et al. first reported an association of AS with Paget’s disease in 1934 [26]. Dabbs et al. described that among 70 patients with Paget’s disease of the bone, only one was found to have AS [18]. Our findings agree with the argument that any previous association was likely incidental as only 6 out of 1852 (0.3%) AS patients were found to have Paget’s disease, a rate similar to the control population (0.2%, p = 0.431)
Angioid streaks have also been reported in cases of sickle cell disease with variable frequency and are suggested to be a complication of the disease through either impaired iron metabolism, elastic tissue degeneration or calcium deposition at Bruch’s membrane [8, 23, 24]. The literature on the association between sickle cell-related hemoglobinopathies shows conflicting results and typically focused on screening for AS in sickle patients (i.e., the inverse of the question we asked, “what rate of AS patients are associated with sickle cell-related hemoglobinopathies”). When examining sickle cell patients, the prevalence rate has varied from as high as 22% [11], but more commonly has been in the 4–8.7% [7,8,9, 17] The results of our study (1.4% prevalence rate), however, are much more in line with those of Nagpal et al. who observed 5 (1.4%) cases of AS among 356 patients with sickle cell hemoglobinopathy [10] and Kent et al. screened 98 eyes with sickle cell disease and found no cases of angioid streaks [12].
The association between Ehler’s Danlos syndrome (EDS) and angioid streaks has been less frequently reported. Green et al. described the occurrence of angioid streaks in two patients of 15 with EDS [13]. A retrospective study of 21 patients with EDS showed no signs of AS [14]. Most recently, Singman et al. studied 284 patients with EDS and also found no cases of AS [15]. We found a significantly elevated prevalence rate of EDS in our sample compared to controls, but given the rate was only 1.0%, it is unclear if this association is overstated relative to its inclusion in the mnemonic.
PXE is an autosomal recessive multisystem disorder caused by mutations in the ABCC6 (ATP binding cassette family C member 6) gene that can be life threatening as patients can develop injury to the great vessels, which can lead to sudden death. PXE has been reported to be the most common systemic disease associated with AS and previously been reported to occur in 59–87% of patients with PXE [5, 16, 17]. Connor et al. described 74 patients with PXE with typical cutaneous changes, 63 (85%) of whom had AS [16]. Shields et al. described that among 56 patients with angioid streaks, 30 (54%) cases had PXE [17]. Not surprisingly then, our results confirmed this as the strongest association with PXE out of all systemic diseases assessed.
The association of PXE with AS may extend beyond simply having angioid streaks and may suggest a common pathogenic pathway as age-related macular degeneration [28]. Both AS/PXE and AMD have portions of the elastic lamina within the mid-segment of Bruch’s membrane that becomes thickened and calcified [2]. Patients with PXE have been shown to develop geographic atrophy with a pattern of progression similar to AMD [27]. Similarly, there seems to be an association of PXE with subretinal drusenoid deposits (SRDD) as one study found that 22 (52%) of 42 patients with PXE showed SRDD [28]. Another showed that 10 eyes of 16 PXE patients with CNV from angioid streaks also had SRDD and that there was a significant reduction in mean subfoveal choroidal thickness in PXE patients compared to controls [21]. Given that SRDD is a variant of AMD and a risk factor for atrophy progression, this again argues for a possible shared pathway [21, 28].
Our study showed a 33.9% prevalence of non-exudative age-related macular degeneration among patients with angioid streaks, a statistically higher rate compared to matched controls. This finding may reinforce the previously cited studies highlighting potential overlapping pathophysiology between age-related macular degeneration (AMD) and AS. Prior research studies have investigated the incidence of CNV formation in eyes with AS. Mansour et al. reported that exudative/hemorrhagic macular degeneration was found to have a significant association with three morphologic subgroups of AS eyes. However, it must be noted that the macular degeneration herein is distinct from AMD [22]. Namely, the degenerative events of AS eyes may be considered as a complication of CNV [29].
In this analysis, only the diagnosis of non-exudative AMD, including early, intermediate AMD and geographic atrophy (GA), had stringent removal of patients with possible CNV due to other causes. The different clinical stages of non-exudative AMD encompass the hallmark pathophysiologic events of ECM degeneration, deposit formation (i.e., drusen formation), RPE degeneration and atrophy [30]. These pathological events within the diagnosis of non-exudative AMD render the BrM and RPE weak and susceptible to damage by various mechanisms.
It is notable that in non-exudative AMD, the RPE-BrM complex is compromised by BrM thickening and activated calcification, contributing to BrM fragility [31, 32]. Meanwhile, it is also a disease of the outer retina-RPE, in which activation and migration of RPE cells lead to RPE degeneration and atrophy [33]. AS, on the other hand, are characterized by activated and dysfunctional mineralization of the elastin-rich membrane, leading to a thickened and brittle BrM. Concurrently, RPE is activated and migrate to other retinal layers. When the mechanical integrity of BrM is interrupted, the overlying RPE degenerates and atrophy ensues [5]. Based on this direct comparison, non-exudative AMD and AS share common findings of weakened BrM and underlying mechanisms of a dysfunctional RPE. Therefore, when the AS-like phenotype is found in non-exudative AMD eyes, it may herald future AMD progression and implicate the foci where GA or CNV may preferentially develop.
Hereditary spherocytosis is a membranopathy of intrinsic hemolytic anemia, in which disordered bone metabolism has been reported [34]. McLane et al. reported the presence of AS in four of five members of the second generation of a family with hereditary spherocytosis [35]. Sawda et al. described a patient with hereditary spherocytosis who demonstrated an anterior ischemic optic neuropathy and angioid streaks [36]. The influence of the disordered bone metabolism in hereditary spherocytosis on BrM metabolism such as calcification is still unclear but may be due to mineralization causing BrM to become more brittle. Overall, in Table 3, most of the diseases that possess significantly high prevalence rates of AS are categorized as connective tissue diseases and age-related basement membrane conditions such as senile elastosis, at rates equal to or higher than some of the classical disease associations [37]. The statistical analysis supports the hypothesis that the abnormal metabolism of connective tissue and ECM may lead to disruption or weakening of BrM and/or its mineralization, which contribute toward AS formation.
There are some limitations to our study. One limitation of this study is the inability to verify with medical chart level data any individual diagnosis due to the de-identified nature of the database. In addition, the insurance-based nature of the study limits its overall generalizability as it may not reflect patients from other insurers or patients who are uninsured. Another consideration that may have affected the study was the lack of mandated eye examinations after the index date; therefore, it is possible that additional diagnoses or CNV events may have been missed. In particular, for some patients a diagnosis of AS may precede other systemic diseases. In addition, the study does not account for the variable disease severity of certain systemic diseases with less clinically severe systemic findings that may be underdiagnosed and may also undercount disease states that are diagnosed after a patient has left the insurance plan. To reduce this risk, however, we mandated all patients have at least one year in the insurance plan for inclusion in the study.
Conclusion
In conclusion, we found that in the largest collection of patients with AS to date, the classical teaching of the rates of systemic disease associations do not occur at rates previously reported with only PXE having a similar prevalence rate to published reports. This study reveals an association of AS with other less reported diseases, including certain connective tissue diseases and non-exudative AMD, which could suggest other pathological mechanisms of AS formation.
Summary
What was known before
-
Angioid streaks (AS) may be associated with systemic diseases, some of which may be sight- or life threatening.
-
To date, the association between AS and systemic diseases has been primarily documented in case reports and case series, with the incidence of AS association in each disease extracted from selected disease-categorized cohorts.
What this study adds
-
In this study, we utilized a US medical claims database to determine the relative prevalence of disease-dependent associations among a cohort of angioid streak patients.
-
We found that in the largest collection of patients with AS to date, the classical teaching of the rates of systemic disease associations do not occur at rates previously reported with only PXE having a similar prevalence rate to published reports.
-
This study reveals an association of AS with other less reported diseases, including certain connective tissue diseases and non-exudative AMD, which could suggest other pathological mechanisms of AS formation.
Data availability
Data for this study were licensed from OptumInsight (Eden Park, MN, USA) by the University of Pennsylvania and due to contractual obligations are not permitted to be made freely available. It is available for licensing directly from the company.
References
Gliem M, Finger RP, Fimmers R, Brinkmann CK, Holz FG, Charbel Issa P. Treatment of choroidal neovascularization due to angioid streaks. Retina. 2013;33:1300–14.
Risseeuw S, Ossewaarde-van Norel J, van Buchem C, Spiering W, Imhof SM, van Leeuwen R. The extent of angioid streaks correlates with macular degeneration in pseudoxanthoma elasticum. Am J Ophthalmol. 2020;220:82–90.
Hagedoorn A. Angioid streaks and traumatic ruptures of Bruch’s membrane. Br J Ophthalmol. 1975;59:267.
Dreyer R, Green WR. The pathology of angioid streaks: a study of twenty-one cases. Trans Pa Acad Ophthalmol Otolaryngol. 1978;31:158–167.
Chatziralli I, Saitakis G, Dimitriou E, Chatzirallis A, Stoungioti S, Theodossiadis G, et al. ANGIOID STREAKS: a comprehensive review from pathophysiology to treatment. Retina. 2019;39:1–11.
Kerr NM. Ocular manifestations of juvenile Paget disease. Arch Ophthalmol. 2010;128:698.
Clarkson JG, Altman RD. Angioid streaks. Surv Ophthalmol. 1982;26:235–46.
Geeraets WJ, Guerry DP. Angioid streaks and sickle-cell disease. Am J Ophthalmol. 1960;49:450–70.
Hamilton AM, Pope FM, Condon PI, Slavin G, Sowter C, Ford S, et al. Angioid streaks in Jamaican patients with homozygous sickle cell disease. Br J Ophthalmol. 1981;65:341–7.
Nagpal KC, Asdourian G, Goldbaum M, Apple D, Goldberg MF. Angioid streaks and sickle haemoglobinopathies. Br J Ophthalmol. 1976;60:31–4.
Condon PI, Serjeant GR. Ocular findings of elderly cases of homozygous sickle-cell disease in Jamaica. Br J Ophthalmol. 1976;60:361–4.
Kent D, Arya R, Aclimandos WA, Bellingham AJ, Bird AC. Screening for OPHTHALMIC manifestations of sickle cell disease in the United Kingdom. Eye. 1994;8:618–22.
Green WR, Friedman-Kien A, Banfield WG. Angioid streaks in Ehlers-Danlos syndrome. Arch Ophthalmol. 1966;76:197–204.
Perez-Roustit S, Nguyen D-T, Xerri O, Robert M-P, De Vergnes N, Mincheva Z, et al. Manifestations ophtalmologiques des syndromes d’Ehlers–Danlos: À Propos D’UNE cohorte de 21 patients. J Français d’Ophtalmol. 2019;42:722–9.
Singman EL, Doyle JJ. Angioid streaks are not a common feature of Ehlers-Danlos syndrome. JAMA Ophthalmol. 2019;137:239.
Connor PJ, Juergens JL, Perry HO, Hollenhorst RW, Edwards JE. Pseudoxanthoma elasticum AND angioid streaks. Am J Med. 1961;30:537–43.
Shields JA, Federman JL, Tomer TL, Annesley WH. Angioid streaks. I. ophthalmoscopic variations and DIAGNOSTIC problems. Br J Ophthalmol. 1975;59:257–66.
Dabbs TR, Skjodt K. Prevalence of angioid streaks and other ocular complications of Paget’s disease of bone. Br J Ophthalmol. 1990;74:579–582.
Ketner S, Moradi IE, Rosenbaum PS. Angioid streaks in association with sickle thalassemia trait. JAMA Ophthalmol. 2015;133:e141770.
Lim JI, Bressler NM, Marsh MJ, Bressler SB. Laser treatment of choroidal neovascularization in patients with angioid streaks. Am J Ophthalmol. 1993;116:414–23.
Kumar V. Reticular pseudodrusen and thin choroid are associated with angioid streaks. Ophthalmic Surg, Lasers Imaging Retina. 2018;49:402–8.
Mansour AM, Shields JA, Annesley WH Jr, El-Baba F, Tasman W, Tomer TL. Macular degeneration in angioid streaks. Ophthalmologica. 1988;197:36–41.
Georgalas I, Papaconstantinou D, Koutsandrea C, Kalantzis G, Karagiannis D, Georgopoulos G, et al. Angioid streaks, clinical course, complications, and current therapeutic management. Ther Clin Risk Manag. 2008;81.5:81–9.
Jampol LM, Acheson R, Eagle RC, Serjeant G, O’Grady R. Calcification of Bruch’s membrane in angioid streaks with homozygous sickle cell disease. Arch Ophthalmol. 1987;105:93–8.
Scholz RO. Angioid streaks. Arch Ophthalmol. 1941;26:677–695.
Terry TL. Angioid streaks and osteitis deformans. Trans Am Ophthalmol Soc. 1934;32:555–573.
Gliem M, Müller PL, Birtel J, McGuinness MB, Finger RP, Herrmann P, et al. Quantitative fundus autofluorescence in pseudoxanthoma elasticum. Investig Opthalmol Vis Sci. 2017;58:6159.
Gliem M, Hendig D, Finger RP, Holz FG, Charbel Issa P. Reticular pseudodrusen associated with a diseased bruch membrane in pseudoxanthoma elasticum. JAMA Ophthalmol. 2015;133:581.
Verhoeff FH. Histological findings in a case of angioid streaks. Br J Ophthalmol. 1948;32:531–44.
Ferris FL, Wilkinson CP, Bird A, Chakravarthy U, Chew E, Csaky K, et al. Clinical classification of age-related macular degeneration. Ophthalmology. 2013;120:844–51.
Curcio CA, Saunders PL, Younger PW, Malek G. Peripapillary chorioretinal atrophy. Ophthalmology. 2000;107:334–43.
Tan AC, Pilgrim MG, Fearn S, Bertazzo S, Tsolaki E, Morrell AP, et al. Calcified nodules in retinal drusen are associated with disease progression in age-related macular degeneration. Sci Transl Med. 2018;10:eaat4544.
Sarks JP, Sarks SH, Killingsworth MC. Evolution of geographic atrophy of the retinal pigment epithelium. Eye. 1988;2:552–77.
Cesur M, Temiz F, Acıpayam C, Kılınc M, Seringec Akkececi N. Disordered bone metabolism in hereditary spherocytosis patients. Hematology. 2019;24:276–81.
McLane NJ, Grizzard WS, Kousseff BG, Hartmann RC, Sever RJ. Angioid streaks associated with hereditary spherocytosis. Am J Ophthalmol. 1984;97:444–9.
Sawada A, Oie S, Mochizuki K, Yamamoto T. Anterior ischemic optic neuropathy in patient with hereditary spherocytosis and coexisting angioid streaks. Eur J Ophthalmol. 2013;23:132–4.
Felsher Z. Observations on senile elastosis. J Investig Dermatol. 1961;37:163–5.
Funding
National Institutes of Health K23 Award (1K23EY025729 - 01) and University of Pennsylvania Core Grant for Vision Research (2P30EY001583). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Additional funding was provided by Research to Prevent Blindness and the Paul and Evanina Mackall Foundation. Funding from each of the above sources was received in the form of block research grants to the Scheie Eye Institute. None of the organizations had any role in the design or conduction of the study.
Author information
Authors and Affiliations
Contributions
Study idea: JN, YL. Study design: BM, BVB. Study conduction: BM, BVB. Results analysis: JN, YL BVB. Manuscript drafting: JN, YL, BVB. Critical revision of manuscript: JN, YL, BM, BVB.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nadelmann, J.B., Li, Y., McGeehan, B. et al. Systemic disease associations with angioid streaks in a large healthcare claims database. Eye 37, 1596–1601 (2023). https://doi.org/10.1038/s41433-022-02189-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02189-x