Abstract
Obtaining a rapid etiological diagnosis for infants with early-onset rare diseases remains a major challenge. These diseases often have a severe presentation and unknown prognosis, and the genetic causes are very heterogeneous. In a French hospital network, we assessed the feasibility of performing accelerated trio-genome sequencing (GS) with limited additional costs by integrating urgent requests into the routine workflow. In addition to evaluating our capacity for such an approach, this prospective multicentre pilot study was designed to identify pitfalls encountered during its implementation. Over 14 months, we included newborns and infants hospitalized in neonatal or paediatric intensive care units with probable genetic disease and in urgent need for etiological diagnosis to guide medical care. The duration of each step and the pitfalls were recorded. We analysed any deviation from the planned schedule and identified obstacles. Trio-GS was performed for 37 individuals, leading to a molecular diagnosis in 18/37 (49%), and 21/37 (57%) after reanalysis. Corrective measures and protocol adaptations resulted in a median duration of 42 days from blood sampling to report. Accelerated trio-GS is undeniably valuable for individuals in an urgent care context. Such a circuit should coexist with a rapid or ultra-rapid circuit, which, although more expensive, can be used in particularly urgent cases. The drop in GS costs should result in its generalized use for diagnostic purposes and lead to a reduction of the costs of rapid GS.
Similar content being viewed by others
Introduction
An estimated 5.7% of admissions to neonatal intensive care units (ICUs) could be due to chromosomal or monogenic disorders [1]. Obtaining a rapid etiological diagnosis remains a major challenge for guiding care management in this urgent context. In the absence of a clinical diagnosis, exome or genome sequencing (ES or GS) is now often recommended as a first-tier diagnostic test [2] because of the vast number of genetic diseases–over 8,000 [3, 4]–and their considerable clinical and genetic heterogeneity.
Clinical GS is less developed than clinical ES in most institutions but appears more suitable in an urgent context since no enrichment phase is needed. In 2012, Kingsmore et al. provided a proof of concept for GS in an ultra-rapid circuit, first retrospectively on two individuals, then prospectively on 5 individuals with a diagnosis in 2/7 (29%) in less than 50 hours [5]. To reduce the duration of bioinformatics analysis and variant interpretation, they targeted genes involved in nearly 600 recessive diseases. Two years later, they applied this strategy on “rapid” GS in 16 children in neonatal ICU, expanding the analysis to around 4,000 monogenic diseases [6]. They obtained a diagnostic rate of almost 70% in approximately 43 days. Since then, “rapid” ES and GS have been applied prospectively in a number of paediatric ICU cohorts. The median time to diagnosis using ES or GS ranges from 1 to 43 days and the diagnostic yield from 20% to 72% (Table 1) [4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26], showing that the definition of “rapid” ES or GS is not universal in the literature, and highly depends on the context (year of the study, country, resources). Some teams have succeeded in reducing turnaround time by optimizing phenotypic data collection or data interpretation. For example, Clark et al. have implemented a fully automated system to obtain a genetic disease diagnosis with a median turnaround time of about 20 h [27]. Because the arrival of samples cannot be planned, some authors used a full sequencing run for a single sample [8], while others allocated additional resources (in particular to enable a more flexible batching of samples) [21]. This allowed them to optimize the time to results but required a considerable extra upfront investment. In this article, we will use the term “accelerated” GS. We will refer to “rapid” when referring to the general literature on the subject, regardless of the actual turnaround time.
We report on the FASTGENOMICS pilot study in newborns and infants requiring an urgent diagnosis for care orientation. It was designed to evaluate the feasibility of implementing trio-GS to deliver a result in less than 45 days, while minimizing extra costs by adapting the organization to integrate urgent requests as a priority into the usual, not urgent workflow, and to identify the technical or organizational obstacles encountered.
Materials and methods
FASTGENOMICS is a French national, multicentre, prospective pilot study in newborns and infants suspected of genetic disease and hospitalized in neonatal or paediatric ICU.
Individuals
We included newborns and infants proposed for inclusion by their referring clinical geneticist from eight reference centers for developmental diseases across France under the four conditions: (1) hospitalized in ICU with an urgent need for an etiological diagnosis to guide medical care; (2) suspected genetic cause and no obvious clinical diagnosis; (3) proband and both biological parents available for blood samples; and (4) written informed consent from both parents. The inclusion was validated by the two clinical geneticists coordinating the project. After the genetic medical consultation, whole blood samples were collected from the proband and their parents. Inclusions were discontinued after 37 individuals had been enrolled, as provided in the financing plan.
From the end of December 2018 to February 2020, 37 newborns or infants (14 females, 23 males) were included. Twelve had ultrasound features during pregnancy and seven of them had normal prenatal array-CGH. The median age of probands at inclusion was 27 days. All were born from healthy parents, including four consanguineous couples. The overall clinical features of the probands are described in Table S1 and mainly included neonatal hypotonia (17/37), epilepsy (13/37), and/or multiple congenital abnormalities (7/37). One individual died before the results were available.
Methods
We implemented a dedicated accelerated circuit with a time limit for each step of the process and staff (a technician and a biologist), for whom FASTGENOMICS became a high priority. To evaluate the feasibility of this rapid process, while avoiding potential pitfalls and resolving existing issues, we measured the duration from the dispatch of the blood samples to the sending of the report and we recorded all unexpected and adverse events at each of the 8 steps in the process (Fig. 1). Additional methods can be found in the supplemental materials.
Step 1 – Sample reception. The inclusion center sent the blood samples to the coordinating lab (Dijon Bourgogne University Hospital) using a dedicated transporter. Estimated maximum duration: 2 calendar days.
Step 2 – Pre-analytic registration and techniques. After individuals were registered in the laboratory’s information system, standard procedures were followed to extract and qualify genomic DNA, as well as to genotype SNPs to ensure sample matching (Supplemental data). Estimated maximum duration: 8 calendar days.
Step 3 – Shipping of samples to the sequencing platform. The coordinating lab used a dedicated transporter to ship the DNA samples to the sequencing platform at the Centre National de Recherche en Génomique Humaine (CNRGH, Évry), avoiding deliveries during the weekend. Estimated maximum duration: 2 calendar days.
Step 4 – Sequencing. The preparation of the genomic DNA libraries was done according to manufacturer instructions (Supplemental data). Trio-GS was performed using a NovaSeq6000 (Illumina, CA, USA). Estimated maximum duration: 21 calendar days.
Step 5 – Bioinformatics analysis. The coordinating lab downloaded raw sequencing data from the CNRGH platform and transferred it to the computer cluster of the University of Burgundy (CCuB) to run bioinformatics analyses (Supplemental data). Estimated maximum duration: four calendar days.
Step 6 – Data interpretation. Data was independently interpreted by one cytogeneticist and two molecular geneticists (Supplemental data). Estimated maximum duration: 5 calendar days.
Step 7 – Multidisciplinary team meeting. All readers compared their results during a specific multidisciplinary team meeting, organized as quickly as possible, including at least two senior genomic geneticists and one clinical geneticist. Each selected variant was ranked into one of the five categories from the ACMG recommendations. Only the pathogenic and likely pathogenic results were considered etiological diagnoses. Variants of uncertain significance (VUS) were returned to the referring clinician when the multidisciplinary team estimated that the implication in the phenotype was very likely and/or when additional tests could be proposed to confirm the pathogenicity of the variants. Estimated maximum duration: 2 calendar days.
Step 8 – Communication of the results. The molecular diagnosis was emailed to the referring clinician. Estimated duration: 1 calendar day.
Steps 5 (bioinformatics) and 6 (interpretation) could be done during the weekend but steps 1 and 3 (transport), 2 and 4 (pre-analytic registration and techniques), or 7 (multidisciplinary team meeting) could not.
In order to calculate the minimum reliably achievable turnaround time of the analysis, we evaluated the duration that could be held for each of the eight steps of our diagnostic routine, with a prioritization over routine cases at each step, but without requiring additional staff. After adding up the estimated duration of each step, we found that the result should be returned to the clinician within 45 calendar days.
We divided the study into two phases: phase 1, including the first two months to identify the flaws in the initial experimental protocol; phase 2, covering the twelve following months and including adjustments in order to manage the obstacles and to reduce the waiting time for the remaining subjects.
Variant confirmation and parental segregation were performed by Sanger sequencing, qPCR or Multiplex Ligation-dependent Probe Amplification (MLPA) if IGV visualization was uncertain. All causal variants and VUS identified in this study were submitted to ClinVar (accession IDs in supplemental materials).
Limitation of extra costs
Extra costs were mainly limited by not requesting rapid sequencing to the platform. The costs of staff and consumables were compared when sequencing was part of their routine flow or not. Consumable costs covered DNA quantification, quality control, and normalization before library preparation, PCR-free library preparation for GS (Illumina TruSeq DNA PCR-free), quality control before sequencing, standard sequencing on a shared S4 V1.5 Illumina flow cell, or rapid sequencing on a dedicated S1 or SP V1.5 Illumina flow cell in order to reach at least 30X for each sample and bioinformatics analyses to produce FASTQ. Staff costs covered all the people involved in the steps above. Costs were expressed in euros excluding VAT. We also evaluated the additional resources needed per trio in the accelerated circuit set-up for this study as compared to the standard circuit of the lab.
Results
Process steps
Overall duration
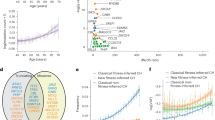
In this pilot study, which included 37 unrelated newborns or infants in neonatal or paediatric ICU, GS median duration was 42 days (ranging from 27 to 92 days) from the dispatch of the blood sample to the communication of the results to the referring clinician.
Ten individuals were included in phase 1 and 27 individuals in phase 2. During phase 1, the time required for steps 5 (bioinformatics analysis), 6 (data interpretation) and 8 (results to clinician) was shorter than or equal to the expected duration (Fig. 2, Table S2). We identified several recurring unexpected events that led to delays. Corrective measures or protocol adaptations (details in the discussion) led to complete resolution for steps 2 (pre-analytic registration and techniques) and 7 (multidisciplinary team meeting), and to a decrease in duration for step 4 (sequencing). Steps 1 and 3 (transport of samples) could not be improved within the study timeframe.
Finally, we were able to reduce the median duration from blood sampling to the communication of the results to the referring clinician from 68 days in phase 1 to 40 days in phase 2 (Fig. 2, Table S2), below our objective of 45 days.
Unexpected and adverse events
The times required from the dispatch of blood samples to the communication of the results for each case are presented in Fig. 2.
Step 1 – Sample reception. For individuals 3, 6, and 36, the transport from the inclusion center to the coordinating lab took 3, 6, and 4 days instead of 1 day.
Step 2 – Pre-analytic registration and techniques. For 8 individuals, the blood samples were received on Friday or the day before a public holiday, causing the extraction to take three calendar days. For 2 individuals, step 2 took respectively 9 and 12 days instead of 8, because the dedicated staff responsible for extracting DNA in phase 1 and sending the samples to the sequencing platform was temporarily absent.
Step 3 – Shipping of samples to the platform. For individual 37, the transport time from the coordinating lab to the sequencing platform took 3 days instead of 1.
Step 4 – Sequencing. During phase 1, sequencing exceeded the expected maximal duration (21 days) in all cases except for the first 2 individuals, who were treated on dedicated flow cells. For case 21, sequencing had to be performed a second time because the sequencing data was contaminated due to an equipment problem during the library preparation step, consequently adding 33 days to the analysis time.
Step 7 – Multidisciplinary team meeting. During phase 1, team meetings had to be delayed for cases 6, 9, and 10.
There were no delays in steps 5 (bioinformatics analysis), 6 (data interpretation), or 8 (communication of the results) (Fig. 2).
Molecular results
Twenty-five causal variants (pathogenic or likely pathogenic) were identified in 18/37 individuals (49%) and 10 VUS in 8/37 (22%) individuals (Table 2, Table S3). We found 34 single nucleotide variants (SNVs) or indels, 1 large intragenic deletion, 1 complex rearrangement, and 1 uniparental isodisomy. The uniparental isodisomy of chromosome 1 was found in case 22 after the identification of a homozygous variant inherited from the mother in a 2 Mb loss of heterozygosity region. We had to confirm the variant by Sanger sequencing for case 19 because some reads around it had a poor mapping quality score and by MLPA for case 27 to confirm the LAMA2 duplication. The complex rearrangement was suspected to be caused by the partial duplication of LAMA2 and TMEM244, followed by a partial deletion of LAMA2 and TMEM244 in the original copy of the genes (supplemental Figure S1). The groups with the highest rate of positive diagnoses were those with multiple congenital abnormalities (57%) or epilepsy (54%).
For some cases, variants classification was a long process or is still pending despite expert advice and/or additional investigations. For case 3, a missense VUS in PIGN was reclassified as probably pathogenic based on functional studies and on expert advice provided nine months after the provisional report, allowing us to propose a prenatal diagnosis to the family. For case 8, an X-linked variant in the PIGA gene inherited from the mother led to familial segregation, which was inconclusive, and was reclassified as probably pathogenic after functional studies. For cases 31 and 36, expression studies on muscle biopsy have been suggested to help reclassify compound heterozygous VUS in the TTN gene. For case 33, the identification of candidate variants in the SATB1 genes, not yet associated with a neurodevelopmental human condition at the time of the study, led us to submit it in GeneMatcher to collect similar cases [28] and allowed to identify a new disorder [29]. We, therefore, expect the final diagnostic rate to be nearly 57%.
Limitation of extra-costs
Extra-costs were mainly limited by not requesting a rapid sequencing to the platform, which would have cost 7900 € per trio (6300 € for consumables and 1600 € for staff), compared to 2590 € (2500 € for consumables and 90 € for staff) in their routine flow. The additional resources per trio of the accelerated circuit were 40 minutes of technician time (step 2), 10 minutes of bioinformatician time (step 5), 30 min of administrative time (steps 1, 3, and 7), and 50 min of geneticist time (steps 2 and 6). The cost of the bioinformatics adaptations made before the study was estimated at 7 h.
Discussion
“Rapid” ES or GS has already been tested in other centers, with a median duration ranging from 1 day to 6 weeks. A definition of “rapid” ES or GS is seriously lacking in the literature [11, 23]. We therefore decided to use the term of “accelerated” GS, to be in line with our main objective of integrating priority GS for neonates and children hospitalized in ICU in the diagnostic process on a national level (network of 8 French reference centers). This study was not designed to evaluate the costs, but to allow accelerated trio-GS without high additional expenses. Therefore, standard laboratory procedures were used as much as possible. Some changes to the usual routine organization were implemented before the study. While our team usually relies on ES for routine diagnosis, GS was preferred because it has been shown that GS is more effective for detecting exonic variants, structural variants (SVs) including CNVs (copy number variations), and balanced chromosomal rearrangements [30, 31]. In addition, GS is more suitable for urgent situations because of the shorter preparation time for samples before the sequencing itself, due to the absence of exon capture. The bioinformatics pipeline implemented for this study was adapted to reduce the computation time from 4 to 2 days.
The prospective investigation performed to identify barriers or organizational obstacles has helped shorten the process throughout the course of the study. While we were unable to meet the objective of 45 days from blood sampling to results during phase 1, with a median duration of 68 and a mean duration of 63 days, the results of the corrective measures were clearly visible during phase 2 (Fig. 2 and Table S2). As the company in charge of the transport of blood samples did not explain the reasons for the delays in steps 1 and 3, we were unable to address this issue. To minimize delays and meet deadlines, samples were tracked during each step, requiring frequent interactions between the referring clinician and the laboratory. To further reduce the sample shipment duration, we would have to switch to a more expensive contract, notably to handle deliveries on non-working days. To avoid both steps 1 and 3, we could also perform the analyses locally, which would require a sequencer per hospital. For step 2, we estimated at the beginning of the study that DNA would be extracted within one working day after the reception of the blood samples. This goal was not met during phase 1, so we revised the division and rotation of tasks to increase efficiency without interrupting the routine activity of the diagnostic laboratory. To further reduce the pre-analytic registration and techniques duration, duties on weekends and public holidays would have to be set up, to allow extraction, quality checks, and shipment of the samples for sequencing without waiting until the beginning of the following week. The main issue was the time required for sequencing (step 4), which almost consistently exceeded the expected maximum duration. The handling of samples was modified to set up a priority circuit with technician time dedicated to this project on the CNRGH platform. In addition, the high-throughput library preparation and sequencing workflow was modified to be able to include the samples received each week without delay. The coordinating lab also had to inform the platform managers in real time of the inclusion of samples into the flow to better organize GS in its activity. The obstacle for even faster sequencing is the threefold cost in terms of sequencers, consumables, and staff. It should be noted that in most studies on rapid circuits, sequencing was carried out on local dedicated platforms. France, however, has opted to establish a national network for genomics centralized on two platforms. The expected intense flow of samples to these platforms in the future may improve sequencing time without the need for a dedicated machine. Steps 5, 6, and 8, which were all performed by the coordinating lab, were successfully completed within the estimated time frame. Bioinformatics analysis (step 5) is limited by the available hardware and the software optimization. For example, the use of phenotypic-driven analysis and GPUs could further reduce the time needed for bioinformatics computing [32]. In phase 1, the multidisciplinary meeting (step 7) was planned during data interpretation (step 6). The short notice prevented quorum from being reached in time for 3 cases. In phase 2, there were no further delays for the step 7 thanks to a schedule planned as soon as the sequencing data was received (step 5). The duration of steps 6 to 8 depended on the availability of the geneticists, both when the data was available for interpretation and later when the interpretation was completed to plan the multidisciplinary meeting.
We can assume that our high diagnosis yield stems from the inclusion criteria requiring a genetic cause to be suspected. We found 34 SNVs or indels and 2 SVs. We have shown that the percentage of positive variants increases with additional investigations (asking for expert advice, extended familial segregation, functional studies…). After reevaluation, we have increased the molecular diagnostic rate from 18/37 (49%) to 21/37 individuals (57%). Interestingly, GS identified one case that could not have been resolved by ES. In case 27, we indeed identified a deletion in LAMA2 inherited from the father and a complex rearrangement leading to a disruption of LAMA2 inherited from the mother. ES would have identified the duplication in the rearrangement and the deletion but would not have provided a hypothesis for the underlying mechanism nor the link between the duplication and the loss-of-function of the gene.
In previous studies, “rapid” GS resulted in a potential change in patient management in 27% to 72% of positive cases, including changes in therapy, palliative care, targeted surveillance, genetic counseling, and prenatal diagnosis for future pregnancies [4, 7,8,9,10,11,12,13, 17, 33, 34]. The results of the FASTGENOMICS study show an undeniable clinical interest for patients, with an accelerated diagnosis that could lead to earlier care management decisions and adaptations (including therapeutics, active reanimation, consultation of a specialist in the pathology, reevaluation of surgical indications, complementary investigations and even discontinuation of medical care). Based on the literature, specific changes in therapeutics alone could potentially benefit 7/18 positive patients (39%). L-tyrosine has been suggested to be beneficial in nemaline myopathy (#256030, case 4) [35], although the effectiveness of this treatment has not been proven [36]. Interferon-α2a or -α2b have been shown to increase hemoglobin and decrease iron overload, and successful allogenic bone marrow transplantation has been described in cases resistant to interferon therapy in congenital dyserythropoietic anaemia type Ia (#224120, case 11) [37]. In some cases, the initiation of sodium channel blocker therapy is recommended for treating seizure in individuals with familial benign infantile seizures due to a SCN2A pathogenic variant (#607745, case 15) [38]. Avoiding valproic acid and divalproate is recommended in cases with mitochondrial DNA depletion syndrome 4 A (Alpers type) (#203700, case 18) because of the risk of precipitating liver disease [39]. Inclusion in a gene therapy trial (NCT01840657 and NCT03199469) can be proposed to improve neuromuscular and respiratory symptoms in children with MTM1-associated myotubular myopathy (#310400, case 20). Supplementation of oral galactose has showed clinical and metabolic improvements of glycosylation in CDG syndrome type It (#614921) (case 22) [40]. Vinpocetine or clonazepam have been reported in autosomal dominant epileptic encephalopathy type 43 (#617113, case 24) as having potential efficacy in reducing seizures [41, 42].
We have confirmed the importance of frequent interactions and solid communication, the risks of relying on a small team for specific tasks and the need to train backups, the impact on routine activities, and the importance of obtaining interpretations from both molecular geneticists and cytogeneticists for their expertize in SNVs, indels, and SVs. Speeding up the time to diagnosis using GS while including patients from multiple hospitals but relying on only one laboratory and one sequencing platform and while limiting additional costs presented considerable logistical challenges. Nonetheless, our collaborative community was able to accelerate access to GS in urgent situations and promote a unified approach across different sites in France through infrastructure organization, regular feedback, and sharing of expertise.
This pilot study demonstrated the feasibility of national accelerated diagnosis by trio-GS for newborns and infants requiring an urgent diagnostic orientation for their care, with limited additional cost. Since the extra costs are minor compared to those of the standard circuit, centers that already use ES or GS for diagnosis could implement such an accelerated circuit. A larger study is underway to investigate the impact of these results on patient care management in a larger cohort, including the present one, at short and medium term, in comparison with the classic circuit. Nevertheless, this accelerated circuit must certainly coexist with a rapid circuit, which, although more expensive, can be used in situations where the need for a diagnosis is particularly urgent.
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
FitzPatrick DR, Skeoch CH, Tolmie JL. Genetic aspects of admissions to a paediatric intensive care unit. Arch Dis Child. 1991;66:639–41.
Srivastava S, Love-Nichols JA, Dies KA, Ledbetter DH, Martin CL, Chung WK, et al. Meta-analysis and multidisciplinary consensus statement: exome sequencing is a first-tier clinical diagnostic test for individuals with neurodevelopmental disorders. Genet Med. 2019;21:2413–21.
OMIM. OMIM Entry Statistics. 2019. https://www.omim.org/statistics/entry
Farnaes L, Hildreth A, Sweeney NM, Clark MM, Chowdhury S, Nahas S, et al. Rapid whole-genome sequencing decreases infant morbidity and cost of hospitalization. NPJ Genom Med. 2018;3:10.
Saunders CJ, Miller NA, Soden SE, Dinwiddie DL, Noll A, Alnadi NA, et al. Rapid whole-genome sequencing for genetic disease diagnosis in neonatal intensive care units. Sci Transl Med. 2012;4:154ra135.
Soden SE, Saunders CJ, Willig LK, Farrow EG, Smith LD, Petrikin JE, et al. Effectiveness of exome and genome sequencing guided by acuity of illness for diagnosis of neurodevelopmental disorders. Sci Transl Med. 2014;6:265ra168.
Petrikin JE, Cakici JA, Clark MM, Willig LK, Sweeney NM, Farrow EG, et al. The NSIGHT1-randomized controlled trial: rapid whole-genome sequencing for accelerated etiologic diagnosis in critically ill infants. NPJ Genom Med. 2018;3:6.
Kingsmore SF, Cakici JA, Clark MM, Gaughran M, Feddock M, Batalov S, et al. A randomized, controlled trial of the analytic and diagnostic performance of singleton and trio, rapid genome and exome sequencing in Ill infants. Am J Hum Genet. 2019;105:719–33.
van Diemen CC, Kerstjens-Frederikse WS, Bergman KA, de Koning TJ, Sikkema-Raddatz B, van der Velde JK, et al. Rapid targeted genomics in critically Ill newborns. Pediatrics. 2017;140:e20162854.
Mestek-Boukhibar L, Clement E, Jones WD, Drury S, Ocaka L, Gagunashvili A, et al. Rapid Paediatric Sequencing (RaPS): comprehensive real-life workflow for rapid diagnosis of critically ill children. J Med Genet. 2018;55(Nov):721–8.
French CE, Delon I, Dolling H, Sanchis-Juan A, Shamardina O, Mégy K, et al. Whole genome sequencing reveals that genetic conditions are frequent in intensively ill children. Intensive Care Med. 2019;45:627–36.
Wang H, Lu Y, Dong X, Lu G, Cheng G, Qian Y, et al. Optimized trio genome sequencing (OTGS) as a first-tier genetic test in critically ill infants: practice in China. Hum Genet. 2020;139:473–82.
Sanford EF, Clark MM, Farnaes L, Williams MR, Perry JC, Ingulli EG, et al. Rapid whole genome sequencing has clinical utility in children in the PICU. Pediatr Crit Care Med. 2019;20:1007–20.
Meng L, Pammi M, Saronwala A, Magoulas P, Ghazi AR, Vetrini F, et al. Use of exome sequencing for infants in intensive care units: ascertainment of severe single-gene disorders and effect on medical management. JAMA Pediatr. 2017;171:e173438.
Elliott AM, du Souich C, Lehman A, Guella I, Evans DM, Candido T, et al. RAPIDOMICS: rapid genome-wide sequencing in a neonatal intensive care unit-successes and challenges. Eur J Pediatr. 2019;178:1207–18.
Gubbels CS, VanNoy GE, Madden JA, Copenheaver D, Yang S, Wojcik MH, et al. Prospective, phenotype-driven selection of critically ill neonates for rapid exome sequencing is associated with high diagnostic yield. Genet Med. 2020;22:736–44.
Willig LK, Petrikin JE, Smith LD, Saunders CJ, Thiffault I, Miller NA, et al. Whole-genome sequencing for identification of Mendelian disorders in critically ill infants: a retrospective analysis of diagnostic and clinical findings. Lancet Respir Med. 2015;3:377–87.
Powis Z, Hagman KDF, Blanco K, Au M, Graham JM, Singh K, et al. When moments matter: finding answers with rapid exome sequencing. Mol Genet Genom Med. 2020;8:e1027.
Carey AS, Schacht JP, Umandap C, Fasel D, Weng C, Cappell J, et al. Rapid exome sequencing in PICU patients with new-onset metabolic or neurological disorders. Pediatr Res. 2020;88:761–8.
Dimmock D, Caylor S, Waldman B, Benson W, Ashburner C, Carmichael JL, et al. Project Baby Bear: rapid precision care incorporating rWGS in 5 California children’s hospitals demonstrates improved clinical outcomes and reduced costs of care. Am J Hum Genet. 2021;108:1231–8.
Stark Z, Lunke S, Brett GR, Tan NB, Stapleton R, Kumble S, et al. Meeting the challenges of implementing rapid genomic testing in acute pediatric care. Genet Med. 2018;20:1554–63.
Petrikin JE, Willig LK, Smith LD, Kingsmore SF. Rapid whole genome sequencing and precision neonatology. Semin Perinatol. 2015;39:623–31.
Australian Genomics Health Alliance Acute Care Flagship, Lunke S, Eggers S, Wilson M, Patel C, Barnett CP, et al. Feasibility of ultra-rapid exome sequencing in critically ill infants and children with suspected monogenic conditions in the australian public health care system. JAMA 2020;323:2503–11.
Bourchany A, Thauvin-Robinet C, Lehalle D, Bruel A-L, Masurel-Paulet A, Jean N, et al. Reducing diagnostic turnaround times of exome sequencing for families requiring timely diagnoses. Eur J Med Genet. 2017;60:595–604.
Śmigiel R, Biela M, Szmyd K, Błoch M, Szmida E, Skiba P, et al. Rapid whole-exome sequencing as a diagnostic tool in a neonatal/pediatric intensive care unit. J Clin Med. 2020;9:2220.
Wang H, Qian Y, Lu Y, Qin Q, Lu G, Cheng G, et al. Clinical utility of 24-h rapid trio-exome sequencing for critically ill infants. NPJ Genom Med. 2020;5:20.
Clark MM, Hildreth A, Batalov S, Ding Y, Chowdhury S, Watkins K, et al. Diagnosis of genetic diseases in seriously ill children by rapid whole-genome sequencing and automated phenotyping and interpretation. Science Translational Medicine. 2019 Apr 24 [cited 2020 Aug 22]. https://stm.sciencemag.org/content/11/489/eaat6177.
Sobreira N, Schiettecatte F, Valle D, Hamosh A. GeneMatcher: a matching tool for connecting investigators with an interest in the same gene. Hum Mutat. 2015;36:928–30.
Hoed J, den, Boer E, de, Voisin N, Dingemans AJM, Guex N, Wiel L, et al. Mutation-specific pathophysiological mechanisms define different neurodevelopmental disorders associated with SATB1 dysfunction. Am J Hum Genet. 2021;108:346–56.
Redin C, Brand H, Collins RL, Kammin T, Mitchell E, Hodge JC, et al. The genomic landscape of balanced cytogenetic abnormalities associated with human congenital anomalies. Nat Genet. 2017;49:36–45.
Belkadi A, Bolze A, Itan Y, Cobat A, Vincent QB, Antipenko A, et al. Whole-genome sequencing is more powerful than whole-exome sequencing for detecting exome variants. Proc Natl Acad Sci USA. 2015;112:5473–8.
Wilton R, Szalay AS. Arioc: High-concurrency short-read alignment on multiple GPUs. PLoS Comput Biol. 2020;16:e1008383.
Stavropoulos DJ, Merico D, Jobling R, Bowdin S, Monfared N, Thiruvahindrapuram B, et al. Whole genome sequencing expands diagnostic utility and improves clinical management in pediatric medicine. NPJ Genom Med. 2016;1:15012.
Kernan KF, Ghaloul-Gonzalez L, Vockley J, Carcillo JA. Rapid whole genome sequencing and fulfilling the promise of precision pediatric critical care. Pediatr Crit Care Med. 2019;20:1085–6.
Ryan MM, Sy C, Rudge S, Ellaway C, Ketteridge D, Roddick LG, et al. Dietary L-tyrosine supplementation in nemaline myopathy. J Child Neurol. 2008;23:609–13.
Sztal TE, McKaige EA, Williams C, Oorschot V, Ramm G, Bryson-Richardson RJ. Testing of therapies in a novel nebulin nemaline myopathy model demonstrate a lack of efficacy. Acta Neuropathol Commun. 2018;6:40.
Tamary H, Dgany O. Congenital Dyserythropoietic Anemia Type I. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJ, Mirzaa G, et al., editors. GeneReviews®. Seattle (WA): University of Washington, Seattle; 1993 [cited 2021 Jul 23]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK5313/.
Wolff M, Brunklaus A, Zuberi SM. Phenotypic spectrum and genetics of SCN2A-related disorders, treatment options, and outcomes in epilepsy and beyond. Epilepsia 2019;60(Dec):S59–67.
Cohen BH, Chinnery PF, Copeland WC POLG-Related Disorders. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJ, Mirzaa G, et al., editors. GeneReviews®. Seattle (WA): University of Washington, Seattle; 1993 [cited 2021 Jul 23]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK26471/.
Perales-Clemente E, Liedtke K, Studinski A, Radenkovic S, Gavrilov D, Oglesbee D, et al. A new D-galactose treatment monitoring index for PGM1-CDG. J Inherit Metab Dis. 2021;44:1263–71.
Billakota S, Andresen JM, Gay BC, Stewart GR, Fedorov NB, Gerlach AC, et al. Personalized medicine: vinpocetine to reverse effects of GABRB3 mutation. Epilepsia 2019;60(Dec):2459–65.
Zhang Y, Lian Y, Xie N. Early onset epileptic encephalopathy with a novel GABRB3 mutation treated effectively with clonazepam: a case report. Med (Baltim). 2017;96(Dec):e9273.
Acknowledgements
We thank the families for taking part in the study, the CNRGH (Évry) for genome sequencing, the CCuB for technical support and management of the computing platform, and GeneMatcher for data sharing. Several authors are members of the ERN ITHACA. We acknowledge Suzan Rankin, Cyrille Chopelet and Jérémie Roquet for proofreading the manuscript.
Funding
This work was supported by grants from the Dijon Bourgogne University Hospital, the Regional Council of Bourgogne Franche-Comté, the Sanofi Genzyme laboratory and the European Union through the FEDER programs. This work was supported by the France Génomique National infrastructure, funded as part of the “Investissements d’Avenir” program managed by the Agence Nationale pour la Recherche (ANR-10-INBS-09). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
ASDP: data collection, data production, data analysis, manuscript writing, study coordination. AV/FTMT/ALB/PC/CP data analysis. RO data production, study conception. JFD study conception. AZ/MJ/TB/CF/AT/AS data collection, manuscript editing. BI/JD/SN/MG/MN/MV/SM/MF/AL/PR/YC/JVG/SS/LP/MB/CP/DB/CC data collection. CR data collection, data analysis, manuscript editing. AG/AP/AJ data collection, data analysis. RO/VC/CP/TJ/BF/DBD/CB/PG/ET data production. AB data production, manuscript editing. YD data production, manuscript editing, study conception. LF/CTR data collection, manuscript writing, study conception, study coordination.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the appropriate French ethics committee (2016-A01347-44).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Denommé-Pichon, AS., Vitobello, A., Olaso, R. et al. Accelerated genome sequencing with controlled costs for infants in intensive care units: a feasibility study in a French hospital network. Eur J Hum Genet 30, 567–576 (2022). https://doi.org/10.1038/s41431-021-00998-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-021-00998-4
This article is cited by
-
Rapid genomic sequencing for genetic disease diagnosis and therapy in intensive care units: a review
npj Genomic Medicine (2024)
-
The implementation of large-scale genomic screening or diagnostic programmes: A rapid evidence review
European Journal of Human Genetics (2023)
-
No gene to predict the future?
European Journal of Human Genetics (2022)