Abstract
Study design
Systematic review with meta-analysis.
Objectives
To explore temporal changes in incidence rates, demographic and injury characteristics of incident traumatic spinal cord injury (TSCI) in Nordic countries.
Methods
Peer-reviewed publications and periodic reports about epidemiology of TSCI in the Nordic countries (Denmark, Finland, Iceland, Norway, Sweden) are identified, reviewed and included in the meta-analysis. Data are stratified into 20-year intervals to allow for chronological comparisons. Pooled estimates are derived using random effects meta-analysis.
Results
Twenty-three data sources are included presenting a total of 5416 cases. The pooled incidence rate for 2001–2020 is 15.4 cases/million/year compared to 17.6 and 18.3 cases/million/year during the two previous 20-year intervals. The proportion of cases with TSCI in the 15–29 age-group decreases from 50% (1961–1980) to 20% (2001–2020), while it increases from 9% to 35% in 60+ age-group. Transportation-related injuries decrease from 44% (1961–1980) to 27% (2001–2020). Conversely, fall-related injuries increase from 32% (1961–1980) to 46% (2001–2020). The proportion of individuals with incomplete tetraplegia increases from 31% (1961–1980) to 43% (2001–2020), while complete paraplegia decreases from 25% to 16%.
Conclusion
The characteristics of TSCI in the Nordic countries have changed drastically over the last six decades, in line with clinical experiences, and limited research evidence from other countries. These changes indicate the need for adapting research focus, prevention strategies, design and provision of care, rehabilitation and community services towards older individuals, fall-related injuries, and incomplete injuries in Nordic countries and other settings internationally where such changes occur.
Similar content being viewed by others
Introduction
Advances in prehospital, acute care and rehabilitation services have contributed to higher survival rates, better management of consequences and more effective prevention of complications after traumatic spinal cord injury (TSCI) [1, 2]. It has been suggested that due to the increasing life expectancy of the general population, spinal cord injury (SCI) systems of care may be confronted with an increased number of elderly patients with an acute SCI [3]. Such changes in the demographic and injury characteristics necessitate adaptations in the systems of care.
It has been estimated that the global annual incidence of TSCI varies between 8 and 246 cases per million inhabitants [4]. A number of longitudinal cohort studies have reported temporal variations in demographic and injury characteristics of TSCI over the years [5, 6]. In 2004, a large study from the US Model SCI Systems (MSCIS) reported that during the period 1973–2003, the mean age at injury and proportion of women sustaining an TSCI increased progressively, but there was no systematic change in aetiology of injury and neurological classification (combination of level and completeness of injury) [5]. Despite the large cohort, the authors declared the limited generalisability of their findings even for the US, given the likely selection bias as <15% of all U.S. patients were treated within the MSCIS Units. Another study from the Netherlands showed that compared to 1994, in 2010 there were proportionally more individuals with tetraplegia, more individuals older than 60 years, and less individuals with motor complete lesions [7].
There are a number of systematic reviews exploring the incidence of TSCI on a global level [3, 6, 8, 9], but none specifically for the Nordic countries. Furthermore, to date, there is no systematic review that explores temporal changes of the TSCI demographic and injury characteristics in Nordic countries. With a population of ~30 million, the Nordic countries have similar public health systems and socioeconomic factors, with most of the countries (Denmark, Iceland, Norway, Sweden) contributing data to the recently developed Nordic SCI Registry (NordicSCIR) (http://www.nordicscir.no/). NordicSCIR was established with support from the Nordic council of ministers in 2017 to provide representative longitudinal data to identify incident trends, and inform the design/evaluation of existing and future prevention and SCI care programs in the Nordic countries.
The present systematic review aims to explore how the incidence rate, as well as the demographic and injury characteristics of incident TSCI in the Nordic countries have changed over time.
Methods
Design and procedures
The reporting of this systematic review follows the PRISMA guidelines (Preferred Reporting Items for Systematic Review and Meta-Analyses) [10].
Two authors (AD and MM) jointly developed the protocol, which was not registered, and did not change after the initiation of data extraction. AD and MM searched Scopus, Medline, SPORTdiscus and CINAHL for data sources meeting the following eligibility criteria: (1) cohort studies and case series; (2) presenting demographic and injury characteristics of incident cases with TSCI; (3) relating to a Nordic country, i.e. Denmark (including Faroe Islands and Greenland), Finland, Iceland, Norway, Sweden; and (4) written in English or in one of the Nordic languages. Because of the longitudinal focus of the review, there were no limits related to year of publication. Studies including only cases of a specific level or completeness of TSCI (e.g. cervical TSCI) are excluded from this systematic review, as these are not representative of the total TSCI cohort. Published systematic reviews were initially identified as a way to identify studies meeting the eligibility criteria, but were then excluded from analysis. Hand-searching methods included a screening of the reference lists of all included studies and all identified systematic reviews. Periodic reports and other grey literature meeting all four eligibility criteria were also identified through extensive search and personal communications with SCI experts in the Nordic countries. The final literature search was performed on November 15, 2020. The full list of search terms can be found in Appendix 1. As an example, the search in Scopus included: (“spinal injuries” OR “spinal cord injuries” OR “spinal cord injur*” OR “parapleg*” OR “spinal cord lesion*” OR “tetrapleg*” OR “quadrapleg*”) AND (“Denmark” OR “Danish” OR “Finland” OR “Finnish” OR “Iceland” OR “Iceland*” OR “Sweden” OR “Swedish” OR “Norway” OR “Norwegian” OR “Scandinav*”) AND (“epidemiolog*” OR “population-based” OR “incidence” OR “incident” OR “demograph*”).
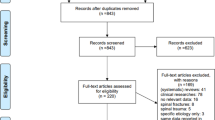
Two authors (AD and MM) jointly reviewed all records in a two-step process: the titles and abstracts of all identified articles were screened before a full-text review of the remaining records was undertaken. In cases of disagreement, consensus was reached through discussion. Figure 1 provides the PRISMA diagram and presents reasons for exclusion of data sources at each step of the review process. Over a two-year period (December 2018 to November 2020), we made extensive efforts to communicate with the authors of the original studies and with the governing bodies of established registries in order to identify grey literature, and to receive missing data and/ or data in a specific format that could facilitate meta-analysis.
Assessment of bias
Two reviewers independently assessed the quality of included data sources by using the quality rating scale for incidence and prevalence studies developed by Singh et al. [3]. The quality assessment score of the studies is determined by addressing 10 questions (Table 1) relating to sample representativeness, method of data collection, statistical method, presentation of outcomes, adequate definition of SCI and inclusion of persons dying at the site of injury. Data sources are assessed as having high (scores 8–10), medium (scores 5–7) or low (0–4) quality, based on how many of the 10 criteria they meet [3]. For the purposes of assessment of bias, each included registry is considered and evaluated as one data source, as the methodology of each registry remained unchanged over the study period. In cases of disagreement between the reviewers, consensus was reached through discussion.
Data extraction
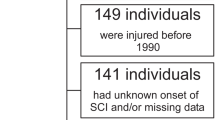
The first author (MM) with help from the last author (AD) extracted data from data sources into a standardised Microsoft Excel spreadsheet. Data are presented in one or more 20-year intervals: up to 1960, 1961–1980, 1981–2000 and 2001–2020. In cases where a study ranged over two or more intervals, the authors of the original studies were asked to provide data divided according to the intervals used in the current review. In one instance where the study period ranges equally over two intervals, the same data are presented in two 20-year intervals [11]. In cases where the same data were presented in multiple data sources, the most complete and suitable data source is included in the analysis.
Incidence rates are calculated as cases per million per year. Where necessary, the first author calculated the incidence rate following the method dictated by the Department of Health of Pennsylvania, by considering the population of the respective capture area at the time of study [12]. Cause of injury is presented according to the International Spinal Cord Society (ISCoS) Core Data Set version 2.0 [13] which includes response categories from the International Classification of External Causes of Injuries (ICECI). We could not apply the prioritisation of the ICECI in relation to the cause of injury, as these rules were not always implemented by the authors of the original data sources. Information about the level and completeness of lesion are presented in the following categories: complete tetraplegia, incomplete tetraplegia, complete paraplegia, incomplete paraplegia. In data sources where detailed data were presented, cases with neurological level between C1 and C8 are categorised as tetraplegia, T1-S5 as paraplegia, American Spinal Injury Association (ASIA) Impairment Scale (AIS) grade A as complete, AIS grades B–D as incomplete. In data sources where data were already presented in categories, these categories are used without being verified by us.
Statistical analysis
Descriptive data is presented as n and %. Stata version 16.0 (Stata Corp.) is used for analysis. Random effects meta-analysis is used to calculate pooled estimates of incidence following the random effects likelihood estimator method [14]. The one paediatric TSCI study is excluded from the analysis and is presented only as descriptive data [15]. Incidence rates of TSCI along with their 95% CIs are calculated. Confidence intervals were computed using the Wald method for Poisson rates [16].
Heterogeneity between studies is assessed with chi‐square test (Cochran’s Q test) and quantified with the I2 statistic. I2 scores are further categorised as low (25%), moderate (50%) and high (75%). In regard to incidence rate, subgroup analysis is performed based on the 20-year interval in accordance with the respective data source.
Sensitivity analysis was performed and included three aspects. First, removing one study at a time and checking if the within- or the between-20-year-interval group differences changed. Second, removing all studies from country at a time and checking how the meta-analysis results changed by 20-year interval as a result of that. Third, removing all studies from country at a time and checking if the incidence rates and CI 95% of the studies could be predicted out of the new results.
Results
Description of identified studies and quality assessment
In total, 23 data sources are included in the analysis, 13 research articles and 10 reports. Out of the 875 unique identified studies, 16 studies meet the inclusion criteria for this systematic review (Fig. 1) [11, 15, 17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34]. Three out of these studies present duplicate data, and are therefore excluded from analysis [26, 33, 34] (Appendix 2). Further, three annual reports from NordicSCIR about Sweden (Östergötland Region, as this is the only region in Sweden that contributed data to NordicSCIR) were excluded as these data were included in Webrehab reports. One single-year epidemiological study for the Stockholm region [23] reported data also presented in the quality registry Webrehab. Because of the rather small size of the region and of the overlapping period, and the difficulty to separate such data, we decided to include both sources. Ten reports linked to two quality registries NordicSCIR [29,30,31, 35] and WebRehab [32, 36] are identified. Study characteristics including authors, year of publication, incidence period, country, study design, setting, age limits and number of cases are presented in Appendix 2.
Table 1 presents the quality evaluation of the included studies. Four studies, all presenting data for the 2000-20 interval, are rated as being of good quality; six are rated as fair and five as poor quality. The most common flaws are related to the retrospective study design (8 sources), the exclusion of cases dying at the site of injury (14 sources), sampling bias (9 sources) and suboptimal methods to identify or confirm an SCI (8 sources).
Out of the 23 included data sources, one source contributes data for the time interval <1960, five sources for 1961–1980, five for 1981–2000, and 19 for 2001–2020. NordicSCIR annual reports provided data for 2017–2019, and Webrehab annual reports provided data for the period 2015–2019. Out of the 13 research studies, four are prospective and nine are population-based (six at a national and three at a regional level). Eleven out of the 13 research studies are published after 2000. There is one paediatric study which focuses on individuals 0–15 years old [15].
Because of the limited number of sources contributing data to the interval until 1960, and the unavailability of detailed data about demographic and injury characteristics, data related to that interval are presented in tables and figures, but comparisons between these data and data from other intervals are not meaningful and is therefore not performed. Also, three studies are only used in some calculations, because of the unavailability of detailed data [11, 19, 20].
A total of 5416 cases with TSCI are included in the analysis, out of which 1129 (20.8%) are female. The mean age for the study population is 47.7 years (SD = 19.7) and most cases are observed in the 30–59 years age-group (Table 2). About 14% of all TSCI cases present with complete tetraplegia (n = 703); 19% with complete paraplegia (n = 998); 35% with incomplete tetraplegia (n = 1945) and 22% with incomplete paraplegia (n = 1188).
Incidence
The pooled annual incidence rate for the years 1952–2020 is 15.9 per million (95% CI, 13.0–18.9) (Fig. 2).
Sex distribution
During the periods 1961–1980 and 1981–2000, the male to female ratio was 4:1, and changes to 3:1 during the last 20 years (2001–2020).
Age at injury
The proportion of cases in the age-group 15–29 years decreases over the years; from 50% in 1961–1980 to 36% in 1981–2000 and to 20% in 2001–2020. Conversely, the proportion of cases in the age-group 60+ years increases from 9% prior to 2000 to 35% in 2001–2020. In the 0–14 and 30–59 age-groups, except from small variations, the proportions remain rather unchanged over the years.
Cause of injury
Over the years, the largest change regarding cause of injury can be seen during the last 20-year interval where the proportion of individuals sustaining a TSCI of transportation related causes declined from 44% to 27%. Conversely, the proportion of individuals sustaining a TSCI through a fall increases by 14% (from 32% to 46%) in the period 2001–2020 when falls become the most common cause of TSCI. For other causes of injury, the proportions of assault (2%), and sports and recreational activities (11–14%) remain rather unchanged over the year periods.
Level and completeness of injury
From 1961–80 to 2001–20, there is a decline in the proportion of tetraplegia complete from 20% to 11%, and in paraplegia complete from 25% to 16%, respectively. Conversely, the largest increase occurs over the same periods by 12% and involves tetraplegia incomplete (from 31% to 43%). The proportion of paraplegia incomplete remains unchanged (22%). It is noteworthy that the proportion of cases with unspecified level and/or completeness of injury increases from 1–2% prior to 2000 to 8% in the period 2001–2020.
Sensitivity analysis
First, when removing one study at a time and checking if the within- or the between-20-year-interval group differences changed, the only observed change occurred when removing the single study in the period <1960, with test of group differences p value changing from p = 0.000 to p = 0.88. This indicates that the reason for the between group differences as indicated for the overall pooled analysis is due to the difference between the <1960 interval and the rest. Further, this indicates that the pooled incidence rates of the periods 1961–80, 1981–2000, and 2001–20 are not significantly different.
Second, when removing a country at a time in every 20-year interval, the pooled incidence changed for 5 points or more in two occasions. First, in 1981–2000 interval, when removing studies from Denmark, there was an increase of ~6 points in the pooled incidence. Second, in 1981–2000 interval, when removing the study from Norway, the pooled incidence dropped by ~5 points.
Third, when removing a country at a time, the new pooled incidence for each 20-year interval could predict the incidence rate of the removed country, in all cases in regard to Sweden and in most cases in regard to the other countries. More specifically, for Norway, Finland and Iceland the pooled incidence could largely predict the country incidence rate, except one 20-year interval period for each country with the corresponding country incidence being outside the upper limit of CI 95%. Regarding Denmark, the pooled incidence could not predict the country incidence for two intervals (1961–80, 2001–20), with the country incidence being outside the lower limit of CI 95%.
Discussion
The overall annual incidence of TSCI in the Nordic countries is comparable to that of many high-income countries as presented in global reviews [3, 6, 8, 9]. In accordance with previous research [4], we found that the limited availability of national population-based studies, as well as of uniform data sets and sampling criteria, hinder international comparisons. Despite the rather stable incidence rate of TSCI during the last 60 years, we did find an increasing number of cases presented in scientific publications and reports, as well as an increasing representation of countries and their respective regions in the 2001–20 interval. These aspects can be largely explained by the considerably higher number of studies contributing data to the 2001–20 interval, the higher number of high-quality studies, and the availability of data from quality registries during that period.
The current systematic review found a reduction in absolute numbers and rates of TSCI caused by transportation-related accidents over the period studied. This is true also for other countries, and can be attributed to a combination of effective prevention measures [37]. During recent decades, national authorities have invested heavily in the improvement of road traffic safety. At the same time, the wide application of technologies such as crumple zones, (obligatory) seat belts, air bags and advanced systems such as ABS (Anti-lock Breaking System) and ESC (Electronic Stability Control) has improved vehicle safety.
We also found an increase in the proportion of elderly sustaining a TSCI and an increase of TSCI caused by falls. Between 1960 and 2019, average life expectancy in the Nordic countries increased by 10 years [38], with similar increases taking place globally [39]. According to the WHO Global Report on Falls Prevention in Older Age, the cumulative effect of falls and resulting injuries among older persons in most countries has the potential to reach epidemic proportions that would consume a disproportionate amount of health care resources [40]. Falls are recognised as a complex multi-factorial phenomenon where impaired balance due to aging and comorbidities, environmental factors and risk taking behaviours play an important role [41]. Any strategies to prevent fall-related TSCI should align with the WHO Falls Prevention model within the Active Ageing Framework comprising the following three pillars: building awareness of the importance of falls prevention; improving the identification and assessment of risk factors and determinants of falls; and identifying and implementing realistic and effective interventions [40].
Clinical, policy and research implications
These changes in epidemiology of TSCI necessitate adaptations of care, rehabilitation and community services. While from the middle to the end of 20th century the characteristics of the TSCI population in the Nordic countries remained relatively stable with respect to age, cause and type of injury, our study shows that during the last 20 years there is a larger degree of diversity in people affected, including children, young adults, adults in the middle of their lives as well as senior citizens. These groups are likely to have different needs that rehabilitation and healthcare providers in general need to address.
Based on our finding of increasing proportion of older adults sustaining a TSCI, and the established correlation between higher age with higher prevalence of comorbidities [42], it is reasonable to expect higher numbers of individuals with an acute TSCI who have multiple pre-existing comorbidities. A higher prevalence of comorbidities and frailty of those injured may increase the risk of both in-hospital and long-term complications. This may have major consequences for care and rehabilitation settings in terms of human resources, required competencies and costs. Elderly patients have a higher risk of developing pressure ulcers, thromboembolic complications, respiratory infections and other complications from immobilisation and these risks may support the decision to intervene surgically. Further, there is a high need for collaboration involving disciplines other than Physical Medicine and Rehabilitation, such as Geriatrics and Internal Medicine.
Apart from the comorbidities that need to be addressed, there are other aspects that may require specific attention from rehabilitation professionals. For example, priorities for management of neurogenic bowel and bladder dysfunction may need to be reconsidered in terms of ease of use of assistive equipment, comfort and the potential long-term complications in relation to life expectancy. For example, the clinical dilemma about a person with tetraplegia reaching independence through intermittent catheterisation or the placement of an indwelling suprapubic catheter may become less problematic, as the higher risk of kidney failure from prolonged use is less relevant for an older person with fewer years to live [13, 43]. The management of pain, both nociceptive and neuropathic, needs to be addressed in relation to potential side-effects of medication and polypharmacy, as well as undesired consequences related to long-term use of medication. Older patients with SCI might also require different approaches to training, e.g. less dynamic and less sports oriented. Rehabilitation pace and expected progress may be slower, possibly due to lower capacity and higher risk for complications such as falls and stress fractures. Finally, with the rise in the proportion of incomplete injuries, there is an argument to increase the focus of rehabilitation services and technologies on walking training. Not only do in-patient care and rehabilitation have to adapt, but also community rehabilitation programmes, peer support, primary care and life-long follow-up.
Hsieh et al. [44] compared outcomes and utilisation of rehabilitation services between older and younger people in the U.S. during the first year after sustaining a SCI. Their findings showed that on admission, the youngest group presented predominately with paraplegia AIS A, B and C (43.5%), as compared to the oldest cohort that presented with AIS grade D (41%) and C1-4 AIS grades A, B and C [44]. Further, Hsieh et al. [44] reported that a higher proportion of those aged over 45 years of age were discharged to and living in nursing homes at 1 year post injury. Patients over 45 years were admitted faster to rehabilitation after injury, but their stay was longer. Further, patients over 45 years received fewer hours of post-discharge out-patient rehabilitation services compared to younger patients. The authors suggested that older patients need more effort to build strength and physical stamina, which indicates that ADL training maybe needs to be prioritised at a later stage in the rehabilitation process. The younger group had different motivation and goals, often related to returning to studies or work, while the older group were in or approached retirement [44]. The older group also seemed to have less interest in recreational therapy when compared to the younger group [44].
In Sweden and in other Nordic countries, the publicly provided welfare services and the social security systems cover an individual’s entire life course, i.e. from “the cradle to the grave” [45]. Despite this, there has been a prioritising of individuals of working age (younger than 65), with certain services and assistive equipment not being as readily available to those of higher age. For example, reimbursement for personal assistance services is limited or not available if injuries occur after the age of 65 in Sweden and 67 in Iceland, whilst Norway removed that age limit only in July 2020. Further, subsidies for car adaptations, special wheelchairs and scooters may also be limited for older citizens. The increasing proportion of elderly sustaining an SCI, and the higher number of comorbidities that coexist in this demographic, together with the increase in life expectancy in the general population and in individuals with SCI, necessitate further changes in the social security system that will ensure adequate support to older individuals.
In terms of prevention, previously the focus of primary prevention was to educate young people not to take unnecessary risks, especially related to dangerous driving, diving in shallow water, use of unsafe equipment and facilities in team sports, and use of protective equipment in recreational activities [46]. Now, more focus needs to be directed towards better adaptation of the environment, e.g. lighting, use of safety equipment, and avoidance of risk taking behaviours among the elderly [41]. Prevention of complications is still an important area of focus both in in-patient care and life-long. Last, given the reported benefits of centralised SCI care and rehabilitation [47] adaptations and improvements of systems of care based on the changing demographics of those injured may be easier implemented in centralised settings, which still poses a challenge for some countries in the Nordic region.
The Nordic countries have a long tradition in using health registries [48]. While registries are an excellent opportunity to provide clinical data on SCI characteristics collected in a uniform way, attention needs to be paid to data completeness and quality, given the concerning proportion of cases with unspecified aetiology and completeness of injury reported in this systematic review. NordicSCIR [31] is utilising regular quality assurance processes to reduce missing, inconsistent, duplicate and misclassified data. Further, in order to capture the full spectrum of TSCI, clear procedures are needed for identifying individuals with minimal deficits, individuals dying prior to hospital admission, those with severe concomitant injuries, and those non-consenting, as these may not always be included and described in studies and quality registry reports. During the last few years, major steps have been performed in the Nordic countries and internationally to facilitate access of researchers to archived registry and research data [48]. Beyond proper collection, annotation, and archiving, data stewardship includes the notion of FAIR data (data must be Findable, Accessible, Interoperable, and Reusable), with the goal that the data should be available to be re-used [49]. The process for researchers to access data should be as simple as possible, and issues related to transparency and data ownership should be addressed. These issues are not unique to the Nordic countries and therefore deserve international attention.
Limitations
The decision to divide time in 20-year intervals (rather than shorter ones) was taken out of convenience. It is likely that epidemiological changes occur in shorter intervals. In this systematic review, it is not possible to conduct more in-depth analysis, given the limited availability of comparable data. Overall, out of the 15 unique data sources, only four were of high quality. Another limitation is that we were not able to evaluate whether there were uniform definitions for level (i.e. tetraplegia and paraplegia) and completeness of injury within and between studies. The large variance in case identification and ascertainment methods that is illustrated in the quality assessment table contributes to the large heterogeneity reported in this study. Further, the inclusion of data from quality registries may have minimised the risk for publication bias, but has further contributed to heterogeneity. Sensitivity analysis showed that in most cases, the pooled incidence rate for each 20-year interval could predict the corresponding incidence rate for each country. It is important to notice that there are no statistics published before 1960 in any other Nordic country except Norway. Further, some studies are not included in all analysis because it is not possible to retrieve demographic data separately for the 20-year interval [11, 19, 20]. Last, one study is considered in two 20-year intervals, given that the breakdown of data is not available [11].
Conclusion
Characteristics of people sustaining a TSCI in Nordic countries have changed drastically over the last six decades. In the last 20 years, there is a higher proportion of injuries involving individuals older than 60 years, incomplete TSCI and fall-related injuries. These changes indicate the need for adapting research focus, prevention strategies, design and provision of services and rehabilitation in Nordic countries and other settings where such changes are observed. Uniform surveillance and registration systems in Nordic countries and globally, as well as open and easy processes for sharing registry data, will facilitate future research and international comparisons.
References
Chamberlain JD, Meier S, Mader L, von Groote PM, Brinkhof MW. Mortality and longevity after a spinal cord injury: systematic review and meta-analysis. Neuroepidemiology. 2015;44:182–98.
van den Berg MEL, Castellote JM, de Pedro-Cuesta J, Mahillo-Fernandez I. Survival after spinal cord injury: a systematic review. J Neurotrauma. 2010;27:1517–28.
Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol. 2014;6:309–31.
Furlan JC, Sakakibara BM, Miller WC, Krassioukov AV. Global incidence and prevalence of traumatic spinal cord injury. Can J Neurol Sci. 2013;40:456–64.
Jackson AB, Dijkers M, Devivo MJ, Poczatek RB. A demographic profile of new traumatic spinal cord injuries: change and stability over 30 years. Arch Phys Med Rehabil. 2004;85:1740–8.
Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord. 2014;52:110–6.
Nijendijk JH, Post MW, van Asbeck FW. Epidemiology of traumatic spinal cord injuries in the Netherlands in 2010. Spinal Cord. 2014;52:258–63.
Rahimi-Movaghar V, Sayyah MK, Akbari H, Khorramirouz R, Rasouli MR, Moradi-Lakeh M, et al. Epidemiology of traumatic spinal cord injury in developing countries: a systematic review. Neuroepidemiology. 2013;41:65–85.
Jazayeri SB, Beygi S, Shokraneh F, Hagen EM, Rahimi-Movaghar V. Incidence of traumatic spinal cord injury worldwide: a systematic review. Eur Spine J. 2015;24:905–18.
Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160.
Biering-Sørensen F, Pedersen V, Clausen S. Epidemiology of spinal cord lesions in Denmark. Paraplegia. 1990;28:105–18.
Pennsylvania Department of Health. Confidence Intervals for a Crude Rate. https://www.health.pa.gov/topics/HealthStatistics/Statistical-Resources/UnderstandingHealthStats/Documents/Confidence_Intervals_for_a_Crude_Rate.pdf: Commonwealth of Pennsylvania.
Biering-Sørensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, et al. International Spinal Cord Injury Core Data Set (version 2.0)-including standardization of reporting. Spinal Cord. 2017;55:759–64.
Hardy RJ, Thompson SG. A likelihood approach to meta-analysis with random effects. Stat Med. 1996;15:619–29.
Augutis M, Levi R. Pediatric spinal cord injury in Sweden: incidence, etiology and outcome. Spinal Cord. 2003;41:328–36.
Casella G, Berger RL. Statistical inference. 2nd ed. Duxbury Advanced Series, Pacific Grove, Calif. Duxbury; 2002.
Ahoniemi E, Alaranta H, Hokkinen EM, Valtonen K, Kautiainen H. Incidence of traumatic spinal cord injuries in Finland over a 30-year period. Spinal Cord. 2008;46:781–4.
Divanoglou A, Levi R. Incidence of traumatic spinal cord injury in Thessaloniki, Greece and Stockholm, Sweden: a prospective population-based study. Spinal Cord. 2009;47:796–801.
Gjone R, Nordlie L. Incidence of traumatic paraplegia and tetraplegia in Norway: a statistical survey of the years 1974 and 1975. Paraplegia. 1978;16:88–93.
Hagen EM, Eide GE, Rekand T, Gilhus NE, Gronning M. A 50-year follow-up of the incidence of traumatic spinal cord injuries in Western Norway. Spinal Cord. 2010;48:313–8.
Halvorsen A, Pettersen AL, Nilsen SM, Halle KK, Schaanning EE, Rekand T. Epidemiology of traumatic spinal cord injury in Norway in 2012–2016: a registry-based cross-sectional study. Spinal Cord. 2019;57:331–8.
Johansson E, Luoto TM, Vainionpää A, Kauppila AM, Kallinen M, Väärälä E, et al. Epidemiology of traumatic spinal cord injury in Finland. Spinal Cord. 2021;59:761–8.
Joseph C, Andersson N, Bjelak S, Giesecke K, Hultling C, Nilsson Wikmar L, et al. Incidence, aetiology and injury characteristics of traumatic spinal cord injury in Stockholm, Sweden: a prospective, population-based update. J Rehabil Med. 2017;49:431–6.
Knutsdottir S, Thorisdottir H, Sigvaldason K, Jonsson H Jr, Bjornsson A, Ingvarsson P. Epidemiology of traumatic spinal cord injuries in Iceland from 1975 to 2009. Spinal Cord. 2012;50:123–6.
Kristinsdottir EA, Knutsdottir S, Sigvaldason K, Jonsson H, Ingvarsson PE. [Epidemiology of Spinal Cord Injury in Iceland from 1975 to 2014]. Laeknabladid. 2016;102:491–6.
Koskinen E, Väärälä EM, Alén M, Kallinen M, Vainionpää A. [The incidence of spinal cord injuries is higher than expected]. Suomen lääkärilehti. 2017;72:2160–6.
Koskinen EA, Alen M, Väärälä EM, Rellman J, Kallinen M, Vainionpää A. Centralized spinal cord injury care in Finland: unveiling the hidden incidence of traumatic injuries. Spinal Cord. 2014;52:779–84.
Noe BB, Stapelfeldt CM, Parner ET, Mikkelsen EM. Survival after traumatic spinal cord injury in Denmark: a hospital-based study among patients injured in 1990–2012. Spinal Cord. 2017;55:373–7.
Halvorsen A, Pettersen AL [Annual Report 2017]. Section for medical quality registers [Internet]. 2018. Available from: https://stolav.no/fag-og-forskning/medisinske-kvalitetsregistre/norsk-ryggmargsskaderegister-norscir#rapporter.
Halvorsen A, Pettersen AL [Annual Report 2018]. Section for medical quality registers [Internet]. 2019. Available from: https://stolav.no/fag-og-forskning/medisinske-kvalitetsregistre/norsk-ryggmargsskaderegister-norscir#rapporter.
Halvorsen A, Pettersen AL [Annual Report 2019]. Section for medical quality registers [Internet]. 2020. Available from: https://stolav.no/fag-og-forskning/medisinske-kvalitetsregistre/norsk-ryggmargsskaderegister-norscir#rapporter.
WebRehab. [Annual Reports] 2015–2019. Available from: https://www.ucr.uu.se/webrehab/arsrapporter.
Sabre L, Hagen EM, Rekand T, Asser T, Kõrv J. Traumatic spinal cord injury in two European countries: why the differences? Eur J Neurol. 2013;20:293–9.
Hagen EM, Eide GE, Elgen I. Traumatic spinal cord injury among children and adolescents; a cohort study in western Norway. Spinal Cord. 2011;49:981–5.
Halvorsen A, Pettersen A, Hansen R, Biering-Sørensen F, Antepohl W, Schaanning E, et al. editors. Is the incidence of non-traumatic spinal cord injury rising in the Nordic countries? 2020.
Sunnerhagen KS, Flansbjer UB, Lannsjö M, Tölli A, Lundgren-Nilsson A. WebRehab: a Swedish database for quality control in rehabilitation. J Rehabil Med. 2014;46:958–62.
Traffic analysis, SCB. [Accidents reported dead, injured, cars in traffic, petrol deliveries, inhabitants and fatalities per 100,000 cars and inhabitants in the years 1950–2018]: Transportstyrelsen 2021. Available from: https://www.transportstyrelsen.se/sv/vagtrafik/statistik/olycksstatistik/statistik-over-vagtrafikolyckor/.
TheWorldBank. Life expectancy at birth, total (years) - Sweden, Norway, Iceland, Denmark, Finland 2021. Available from: https://data.worldbank.org/indicator/SP.DYN.LE00.IN?end=2019&locations=SE-NO-IS-DK-FI&start=1960&view=chart.
United Nations Department of Economic and Social Affairs Population Division. World Population Ageing: United Nations; 2019. Available from: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WorldPopulationAgeing2019-Highlights.pdf.
World Health Organization. WHO Global report on falls prevention in older age 2007. Available from: https://extranet.who.int/agefriendlyworld/wp-content/uploads/2014/06/WHo-Global-report-on-falls-prevention-in-older-age.pdf.
Bégin D, Morgan A, Macedo L, Richardson J, Wojkowski S. Risk-taking behaviors and falls in community-dwelling older adults: a scoping review protocol. JBI Evid Synth. 2021;19:2406–14.
Institute for Health Metrics and Evaluation. Global Burden of Disease: University of Washington; 2019. Available from: https://vizhub.healthdata.org/gbd-compare/.
Weld KJ, Dmochowski RR. Effect of bladder management on urological complications in spinal cord injured patients. J Urol. 2000;163:768–72.
Hsieh C-H, DeJong G, Groah S, Ballard PH, Horn SD, Tian W, et al. Comparing rehabilitation services and outcomes between older and younger people with spinal cord injury. Arch Phys Med Rehabilitation. 2013;94:S175–S86.
Ministry of Finance. The Swedish Model: Government Offices of Sweden; 2017. Available from: https://www.government.se/4a5336/contentassets/8416c4ff1410419090181fe503920390/the-swedish-model.pdf.
Bellon K, Kolakowsky-Hayner SA, Chen D, McDowell S, Bitterman B, Klaas SJ, et al. Evidence-based practice in primary prevention of spinal cord injury. Top Spinal Cord Inj Rehabil. 2013;19:25–30.
Divanoglou A, Westgren N, Bjelak S, Levi R. Medical conditions and outcomes at 1 year after acute traumatic spinal cord injury in a Greek and a Swedish region: a prospective, population-based study. Spinal Cord. 2010;48:470–6.
Smith Jervelund S, De Montgomery CJ. Nordic registry data: value, validity and future. Scand J Public Health. 2020;48:1–4.
Burgun A, Bernal-Delgado E, Kuchinke W, van Staa T, Cunningham J, Lettieri E, et al. Health data for public health: towards new ways of combining data sources to support research efforts in Europe. Yearb Med Inf. 2017;26:235–40.
Acknowledgements
We acknowledge all individuals who provided clarifications and additional information from published studies and SCI registries. We also acknowledge the participants of the Nordic Advanced Spinal Cord Injury Rehabilitation (NASCIR) Course for providing input in relation to the clinical implications of the findings of this systematic review. We thank Kenneth Chance-Larsen for valuable assistance with language editing and proofreading.
Author information
Authors and Affiliations
Contributions
AD conceived the idea, and designed the systematic review together with MM. MM with help from AD conducted the search and screened potentially eligible studies. MM with help from AD extracted the data and conducted the meta-analysis. AD and MM with assistance from WA, AH and ALP communicated with corresponding authors of identified sources to request clarifications and additional data. MM with help from AD developed all tables and figures. AD and MM conducted the assessment of bias. MM and AD wrote the manuscript with help from WA. AH and ALP contributed data from NordicSCIR and revised the manuscript. All authors have read and approved the submitted version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Moschovou, M., Antepohl, W., Halvorsen, A. et al. Temporal changes in demographic and injury characteristics of traumatic spinal cord injuries in Nordic countries - a systematic review with meta-analysis. Spinal Cord 60, 765–773 (2022). https://doi.org/10.1038/s41393-022-00772-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00772-3
This article is cited by
-
Return to work after traumatic spinal fractures and spinal cord injuries: a retrospective cohort study
Scientific Reports (2023)