Abstract
Study design
Cross-sectional study.
Objectives
The purpose was to reveal late health consequences and life issues after a traumatic spinal cord injury (tSCI) in North Macedonia (NM).
Setting
Community dwelling adults with tSCI in NM.
Methods
Persons that sustained tSCI in 1999–2005 were selected, physical examined and a questionnaire was administered. Descriptive statistics were conducted.
Results
From 203 eligible persons, 40 agreed to participate. Mean (range) age at time of injury was 36 (27–75) years and time since injury ranged 9–20 years. Around seventy percent reported current health problems, of which pain and spasm (>60%) were most prevalent, followed by urinary tract infections and pressure injuries. About 30% had never been to a medical specialist and ≈70% had only once been to physiotherapy after discharge from the primary inpatient period. Only one participant had a fully adjusted home for a person with a disability. Those with most severe tSCI (American Spinal Injury Association Impairment Scale (AIS) A, B, and C) seldom left their homes. About 50% were retired and/or unemployed, 50% were working.
Conclusion
This is the first study describing community-dwelling persons with a tSCI in NM. Our study revealed that persons with tSCI reported health issues mostly related to pain, spasms, urinary tract infections and pressure injuries. They lacked follow-ups, experienced physical barriers and poor inclusion in the society, and lacked financial support. Therefore, they were often socially isolated and fully dependent on their families. NM is in need of structured rehabilitation programs and better adaption for persons with reduced mobility.
Similar content being viewed by others
Introduction
A traumatic spinal cord injury (tSCI) is a life-long condition accompanied by sequela and different organ systems issues. Mobility is a challenge due to paresis or paralysis. With the overuse of the intact parts of the body, musculoskeletal pain in the upper extremities often emerges [1]. In addition, neuropathic pain and spasticity/spasms are predominant ailments [2]. Other consequences of severe tSCI to the upper thoracic and cervical levels are pneumonia and atelectasis. Studies have shown that respiratory problem is a leading cause of death [3]. Urinary tract infections (UTIs) are common due to urinary dysfunction (neurogenic bladder), and serious conditions such as renal lithiasis and failure can occur [4]. SCI leads to varying degree of neurogenic bowel dysfunction and constipation [5] as well as significantly reduced quality of life [6]. Pressure injuries are common complications that follows lack of sensation and immobility and are one of the leading causes of re-hospitalization [7]. As a result of the musculoskeletal system’s disuse and changes in hormonal and autonomic systems, osteoporosis develops with fragility fractures as a common consequence [8]. Sexual function is commonly impaired in both men and women suffering from SCI with 95% of men having ejaculatory problems leading to impaired fertility [9]. Metabolic, hormonal and immunological changes increase the risk of developing diabetes mellitus type II, cardiovascular issues, and the susceptibility to infections [10, 11].
Most of these secondary conditions could, when recognized by the health-care system, be prevented or better managed to prevent further disability To our knowledge, there is no previous description of community-dwelling life of a persons with tSCI in North Macedonia (NM). In this study, we wanted to investigate persons injured with tSCI 1999–2005 in NM to reveal their late health issues, use of aids and health services.
Methods
Study design
Cross-sectional study.
Participants
Two hundred and three patients above 18 years of age and citizens of NM treated for a tSCI at the Clinic for Traumatology, Orthopedics, Anesthesia, Reanimation, and Intensive care Unit and Emergency Center (TOARILUC)—Mother Teresa, Skopje, NM, between 1999 and 2005 were identified. A thorough description of methodological issues in this respect has previously been published [12]. A letter with an invitation to participate in the study was sent to all 203 persons. Due to the first authors’ first-hand knowledge of the country and language, the data collection was carried out by her in NM. Initially, 23 persons responded and participated in the study; seven came to TOARILUC, while the remaining 16 persons were seen to in their respective homes. Due to the low number of responders, an additional of 60 persons with tSCI were contacted at their registered home addresses. Due to language barriers, home visits were mainly carried out in areas where ethnic Macedonians live. Of these, ten had migrated to foreign countries, and ten changed their addresses, 14 were found to be non-existing addresses, and two persons were dead. Of the remaining 24 persons with tSCI, 17 accepted to participate, and seven refused. After verbal and written information about the study, all participants signed an informed consent form in accordance with the Declaration of Helsinki. The study was approved by the Regional Ethical committee Norway (no 2014/2041/REK Sør-Øst A) and local authorities in NM.
Study outcome
A questionnaire was administered and clinical examination (see Supplementary Material) were conducted in 2015-2016. The International Spinal Cord Injury Data Sets [13,14,15,16,17,18,19,20,21,22,23,24] and International Standards for Neurological Classification of SCI (ISNCSCI) [24] were used as well as a purpose made structured interview with predefined fixed questions (see Supplementary Material) based on a study by Lidal et al. [3]. Patients were grouped and analysed in four subgroups according to neurological level of injury (NLI) and American Spinal Injury Association Impairment Scale (AIS) grade as recommended [21]; C1-8 AIS A, B, and C (I), Th1-S3 AIS A, B, and C (II), and AIS D any NLI (III). We added information about AIS E (IV). For evaluation of satisfaction with psychological health, emotions and mood, physical health and satisfaction with life, we used a numeric rating scale range 0–10 with zero being no influence and ten being maximum influence based on the International SCI Quality of Life and Pain Basic Datasets [13, 21].
Data analyses
The statistical analyses were performed with SPSS version 25 (Chicago, IL). Descriptive statistics include percentages, range, median, mean, and standard deviation (SD). One-way ANOVA were performed to compare multiple groups. We considered p values < 0.05 to indicate statistical significance.
Results
Characteristics of the study participants
Forty persons were included (32 males and 8 females) in this study (Table 1). Age at the time of the interview ranged from 27 to 75 years. The most common aetiologies were traffic accidents (16 car accidents, one motorcycle accident and one pedestrian accident), followed by falls. Medical records included diagnosis (International Classification of Diseases ICD-10), but no documentation regarding neurological classification at the time of injury. However, clinical examination of the neurological status done as part of this study, revealed that 25 participants had neurologic deficits (AIS A, B, C, or D), whereas 15 persons had no neurological deficit (AIS E) according to ISNCSCI. These 15 reported having had some neurologic deficit at the time of injury. When grouped as recommended [21], neurological subgroups were as follows: C1-8 AIS ABC (I) two participants, Th1-S3 AIS ABC (II) four participants, AIS D any level (III) 19 participants, and AIS E (IV) 15 participants. Half of the participants smoked regularly at the time of interview; all in Groups I (C1-8 AIS ABC) and II (Th1-S3 AIS ABC).
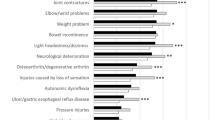
Long-term health issues
The three most frequent current health issues were reported to be spasticity/spasms (68%), pain (60%), and UTIs (38%) (Table 2). All persons with tetraplegia and 63% of the persons with paraplegia experienced spasticity/spasms every day. Groups III and IV (AIS D any level and E) experienced spasticity/spasms when tired at night or when it was cold. Massage, Diazepam (n = 4) and Magnesium (n = 1) was used for treatment of spasticity/spasms by persons with more complete injuries (AIS A, B, C). Pain was a common problem with a prevalence of 100% (AIS A), ≈80%, ≈60% (AIS D), and ≈50% (AIS E). Persons from groups I (C1-8 AIS ABC) and II (Th1-S3 AIS ABC) described pain as a mix of pain, stiffness, and spasticity/spasms. Pain localizations were lower back, hips, knees, shoulders, and arms. Only one patient contacted the health service for his shoulder-pain, others perceived their pain in the shoulders, elbows and hands as normal. The influence of pain on daily activities and mood, graded 0–10 (10 is maximum), revealed that more than half scored above five on both scales. Regarding the influence of pain on sleep, most participants scored above five, except those with AIS E (group IV) who indicated less than four on the scale [13]. Sixteen persons used daily pain relief medications (nonsteroid anti-inflammatory drugs and paracetamol). Current (n = 2) and or previous UTI was reported by 38% of the total study group, the problem more common among persons in groups I (C1-8 AIS ABC) and II (Th1-S3 AIS ABC). Nine participants reported to have UTIs more than twice per year. They usually treated themselves with antibiotics. Three had surgery for nephrolithiasis. Current pressure injuries were experienced by two person with tetraplegia (Group I (C1-8 AIS ABC) and four persons with paraplegia Group II (Th1-S3 AIS ABC). Four of the six pressure injuries had been surgically treated. Since the tSCI, 25% of the participants had had a pressure injury at some point on sacrum and heels. Patients felt that whatever preventive actions (pressure relief, inspections, and padding) they took, they still developed new pressure injuries.
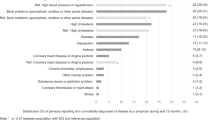
The participants reported cardiovascular health issues: Hypertension (35%), arrhythmia (15%), deep venous thrombosis (10%), and hypotension (8%). Diabetes mellitus type II was reported by four participants (10%), one person had hypercholesterolemia. Previous pulmonary tract infections were reported by four persons with incomplete SCI, AIS B and D (group II and III).
Five participants (15%) had been diagnosed with osteoporosis by Dual-Energy X-ray Absorptiometry (DEXA) scan, of these two reported having had a fracture after the tSCI. Four had experienced fragility fractures 7–15 years after the tSCI, and eight participants had contractures of the lower extremities or hands.
The following gastrointestinal issues were reported: Gastritis (n = 5), cholelitiasis (n = 3), hernia inguinalis (n = 1) and fissura- (n = 1) and fistula-ani (n = 1). Regarding sexuality issues, two persons used Prostaglandin E1 intra-cavernosal injection and one Sildenafil tablets for erection. One male with paraplegia was in contact with a fertility doctor. The remaining participants did not want to answer any questions about sexuality related issues.
Mobility aids and transport
Many participants had a wheelchair for indoor use, and crutches and sticks were common aids among those with less severe injuries. Two persons tried using leg orthoses for walking the first year following injury, but stopped due to falls. For persons needing wheelchair or crutches, mobility outside of the home seemed to be very difficult and almost non-existing in NM. Persons with tetraplegia barely left their homes. Persons with paraplegia rarely went outside with the wheelchair and were always with an accompanying person. Persons with mobility aids did not use public transport. Only one home was fully adjusted for a person with a disability, and the same person had a custom-made car. Others had only support handles in the bathroom and were dependent on other family members for daily life.
Social life, employment, and life satisfaction
Four persons had an improvement in education after the injury and three persons kept the same job as before the tSCI. About fifty percent were working at the study interview, 18% received an old age pension, and five persons received state support of 150 euros a month. Among the most severely injured (AIS A, B, C). only one person was working. Their social contacts consisted mostly of the people they lived with and old friends visiting. According to the International SCI Quality of Life Basic Data Set, Group III (AIS D any level) and IV (AIS E) were more satisfied with their lives, emotions and mood, but less satisfied with the physical health. Participants in group I (C1-8 AIS ABC) were less satisfied with their mood, emotions and mental health, but were more satisfied with life and physical health (Fig. 1) [21]. Participants who were employed or pensioners reported higher life satisfaction than the unemployed
Health-care utilization
The participants with the most severe injuries (group I, C1-8 AIS ABC) never or rarely went to a medical specialist and 35% of all the participants had never been to a specialist (Table 3). They preferred self-diagnosing and self-treatment. About seventy percent had received physiotherapy only once after the accident, and did not receive more appointments due to personal financial reasons. Fifty percent of the participants were satisfied with the health system, 30% neutral, 15% were unsatisfied with the health system and 5% did not answer. A quarter of the participants regarded their General Practioner as a professional with good medical knowledge of tSCI. Those who rated their satisfaction with health care to be low, related this to the lack of assistive aids they needed, lack of regular physiotherapy, expensive medications, not having an outside wheelchair or home support/adjustments.
Discussion
This study is the first to present details with community-dwelling persons living with a tSCI in NM and their long-term health consequences. The participants’ most common health issues were pain, spasms, UTIs and pressure injuries. We also revealed that persons with tSCI were often isolated and did not have specific follow-ups or rehabilitation health services in NM. Participation in society was limited, and their financial situation and public support were poor.
Mean age at time of injury was 36 (range 27–75) years, similar to studies in other countries, although the mean age has been increasing in the latest decades [25]. In the Scandinavian countries, the age is approaching 60 years [26]. Only six persons were AIS grade A, B or C, 19 AIS D, and 15 AIS E. We speculate that the lack of severely injured participants in our study group could be due to the high mortality rate among persons with tSCI AIS grade A, B or C in NM.
Around seventy percent reported current health problems. Nowadays, the medical issues of persons with tSCI are very well recognized worldwide. In line with many reports, the NM study group seemed to have the same long-term ailments as many other persons with tSCI globally, the most frequent secondary health conditions being, spasms, pain, UTIs, and pressure injuries [27]. Spasms and pain were reported to be the most demanding symptoms that persons with tSCI in NM face. Spasticity treatment in this study group included massage or diazepam, unlike the many other available treatment options such as baclofen or botulinum toxin, commonly ordained in many other countries [28]. Patients perceived their pain in the arms and shoulders as normal and they self-medicated when needed. Self-medication for pain has been reported for chronic pain in other countries as well, in a recent review self-medication was found favorable when appropriately used [29]. UTI were reported by 38% of our participants, and was reported as one of the most frequent health complaints among individuals with tSCI in other studies [4, 27]. In group I (C1-8 AIS ABC), all reported to have UTIs more than twice per year, but again they were mostly self-diagnosed and self-medicated. Pressure injuries were a challenge for all persons in group I (C1-8 AIS ABC) despite adhering to prevention strategies, similar to findings in other studies [30, 31]. In our study group, none of those with osteoporosis and/or fractures received medication [8]. We found a lower rate of persons who had experienced fractures compared to other studies [1, 8], probably because of our small sample size and high numbers of persons with AIS E. We also speculate that a reason may be that our participants had limited activities outdoors.
In addition to health issues, social inclusion and participation, for example employment, is important. Life satisfaction is known to be associated with health issues and participation [32]. About fifty percent of all participants were employed, thirty-five percent were employed in Group IV (AIS E), while the most severely injured were all fully dependent on their families in every aspect of life, including economically. NM does not have public access for wheelchair users in every institution and the sidewalks are generally blocked by cars. Thus, independent movement for persons with tSCI is almost impossible, which is a possible reason why the study participants always were accompanied by another person outdoors. The wheelchair they received as social support, one every 5 years, reported to be of poor indoor-use quality. In accordance with a previous study, persons stopped using leg orthoses for walking due to frequent falls the first year following injury [33]. State support was reported to be ~150 euros/month (2016), which is insufficient for living. Not every person with a disability is eligible for state support, which is also difficult to obtain, so family often have to support the individual with SCI.
Our participants responded with low scores for mood, psychiatric satisfaction and emotions, low scores of mental health is also found among persons with SCI in Serbia and Norway [34, 35]. Participants with more severe injuries used the health services less. A reason might be that they diagnosed and treated themselves because of difficulties in having access to health services—and not so much because of dissatisfaction with the health-care system.
In our study AIS E is overrepresented especially compared to AIS A, B, and C. One possible explanation could be that persons with more severe injuries did not survive 10+ years. It is interesting, however, that individuals with AIS E considered being neurological intact [36], reported neurological related health issues, including neuropathic pain and spasticity. Surprisingly, persons classified as AIS D or E (groups III and IV) visited medical specialists more often than the participants with AIS A, B, or C. A natural explanation is that being more mobile means easier access. A previous study reported that persons with AIS E injury had high incidence of suicide [37], thus indicating that this group of patients’ challenges often can be overseen or underdiagnosed.
Strengths and limitations
One of the major strengths of this study was that all the patients had been initially treated at the Mother Teresa hospital, which was the only hospital treating tSCI in NM during our study inclusion period. Missing information on mortality and lack of address registers influenced the recruiting process. Another limitation was that the study invitations were in the NM (official) language. NM has 25% citizens of Albanian ethnicity and thus the language barriers could be a possible reason for the invitee not responding to the invitation. However, 10% of the responders were of Albanian ethnicity. The prevalence of health consequences are influenced by limitations in self-reporting, and the fact that many participants evaluated symptoms by themselves without having been confirmed by a physician. For further methodological challenges, please see our previous publication [12].
Conclusions
This report provides an insight into challenges people with a tSCI face in NM, highlighting socioeconomic implications with limited services to those living with a SCI. Persons living in NM with a long-standing tSCI reported health-issues mostly related to pain, spasms, UTI, and pressure injuries. Our study revealed that persons with tSCI in NM did not have specific follow-ups or rehabilitation and poor inclusion in the society and little or no public support. Because of financial and physical barriers, they were often socially isolated and fully dependent on their families. NM needs to establish specialized rehabilitation programs to improve the management of SCI and reduce long-term health consequences of persons with tSCI—and also to find better solutions to improve the patients’ possibilities to participate in society. Most importantly, our results has pointed to specific health issues, gaps in health services, obstacles for participation, and challenging living conditions that can be useful when planning for improvements of treatment and rehabilitation of people with SCI in NM. The current study can also inspire for further investigations of different aspect of SCI in the Balkans.
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Jakimovska VM, Kostovski E, Biering-Sorensen F, Lidal IB. Fractures and musculoskeletal ailments in persons 20+ years after a traumatic spinal cord injury in Norway. Spinal Cord Ser Cases. 2018;4:76.
Charlifue S, Jha A, Lammertse D. Aging with spinal cord injury. Phys Med Rehabil Clin N Am. 2010;21:383–402.
Lidal IB, Snekkevik H, Aamodt G, Hjeltnes N, Biering-Sorensen F, Stanghelle JK. Mortality after spinal cord injury in Norway. J Rehabil Med. 2007;39:145–51.
Manack A, Motsko SP, Haag-Molkenteller C, Dmochowski RR, Goehring EL Jr., Nguyen-Khoa BA, et al. Epidemiology and healthcare utilization of neurogenic bladder patients in a US claims database. Neurourol Urodyn. 2011;30:395–401.
Coggrave MJ, Norton C. The need for manual evacuation and oral laxatives in the management of neurogenic bowel dysfunction after spinal cord injury: a randomized controlled trial of a stepwise protocol. Spinal Cord. 2010;48:504–10.
Byrne CM, Pager CK, Rex J, Roberts R, Solomon MJ. Assessment of quality of life in the treatment of patients with neuropathic fecal incontinence. Dis Colon Rectum. 2002;45:1431–6.
Cardenas DD, Hoffman JM, Kirshblum S, McKinley W. Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil. 2004;85:1757–63.
Cirnigliaro CM, Myslinski MJ, La Fountaine MF, Kirshblum SC, Forrest GF, Bauman WA. Bone loss at the distal femur and proximal tibia in persons with spinal cord injury: imaging approaches, risk of fracture, and potential treatment options. Osteoporos Int. 2017;28:747–65.
Hess MJ, Hough S. Impact of spinal cord injury on sexuality: broad-based clinical practice intervention and practical application. J Spinal Cord Med. 2012;35:211–8.
Bauman WA, Spungen AM. Carbohydrate and lipid metabolism in chronic spinal cord injury. J Spinal Cord Med. 2001;24:266–77.
Brommer B, Engel O, Kopp MA, Watzlawick R, Muller S, Pruss H, et al. Spinal cord injury-induced immune deficiency syndrome enhances infection susceptibility dependent on lesion level. Brain. 2016;139:692–707.
Kostovski E, Miloshevska Jakimovska V, Lidal IB, Biering-Sørensen F. Cross-sectional and prospective data-collection in North Macedonia—methodological considerations. Spinal Cord Ser Cases. 2019;5:58.
Widerstrom-Noga E, Biering-Sorensen F, Bryce TN, Cardenas DD, Finnerup NB, Jensen MP, et al. The International Spinal Cord Injury Pain Basic Data Set (version 2.0). Spinal Cord. 2014;52:282–6.
DeVivo M, Biering-Sorensen F, Charlifue S, Noonan V, Post M, Stripling T, et al. International Spinal Cord Injury Core Data Set. Spinal Cord. 2006;44:535–40.
Biering-Sorensen F, Alexander MS, van Asbeck FWA, Donovan W, Krassioukov A, Post MWM. Version 1.1 of the international spinal cord injury skin and thermoregulation function basic data set. Spinal Cord. 2017;55:566–9.
Post MW, Charlifue S, Biering-Sørensen F, Catz A, Dijkers MP, Horsewell J, et al. Development of the International spinal cord injury activities and participation basic data set. Spinal Cord. 2016;54:530–4.
Karlsson AK, Krassioukov A, Alexander MS, Donovan W, Biering-Sorensen F. International spinal cord injury skin and thermoregulation function basic data set. Spinal Cord. 2012;50:512–6.
Krogh K, Perkash I, Stiens SA, Biering-Sorensen F. International bowel function basic spinal cord injury data set. Spinal Cord. 2009;47:230–4.
Biering-Sorensen F, Craggs M, Kennelly M, Schick E, Wyndaele JJ. International lower urinary tract function basic spinal cord injury data set. Spinal Cord. 2008;46:325–30.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
Charlifue S, Post MW, Biering-Sorensen F, Catz A, Dijkers M, Geyh S, et al. International spinal cord injury quality of life basic data set. Spinal Cord. 2012;50:672–5.
Dvorak MF, Wing PC, Fehlings MG, Vaccaro AR, Itshayek E, Biering-Sorensen F, et al. International spinal cord injury spinal column injury basic data set. Spinal Cord. 2012;50:817–21.
Dvorak MF, Itshayek E, Fehlings MG, Vaccaro AR, Wing PC, Biering-Sorensen F, et al. International Spinal Cord Injury: spinal interventions and surgical procedures basic data set. Spinal Cord. 2015;53:155–65.
Biering-Sorensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, et al. International spinal cord injury core data set (version 2.0)-including standardization of reporting. Spinal Cord. 2017;55:759–64.
McCaughey EJ, Purcell M, McLean AN, Fraser MH, Bewick A, Borotkanics RJ, et al. Changing demographics of spinal cord injury over a 20-year period: a longitudinal population-based study in Scotland. Spinal Cord. 2016;54:270–6.
Halvorsen A, Pettersen AL, Nilsen SM, Halle KK, Schaanning EE, Rekand T. Epidemiology of traumatic spinal cord injury in Norway in 2012–2016: a registry-based cross-sectional study. Spinal Cord. 2019;57:331–8.
Biering-Sorensen F, Bickenbach JE, El Masry WS, Officer A, von Groote PM. ISCoS-WHO collaboration. International Perspectives of Spinal Cord Injury (IPSCI) report. Spinal Cord. 2011;49:679–83.
Kirshblum S. Treatment alternatives for spinal cord injury related spasticity. J Spinal Cord Med. 1999;22:199–217.
Perrot S, Cittée J, Louis P, Quentin B, Robert C, Milon JY, et al. Self-medication in pain management: The state of the art of pharmacists’ role for optimal Over-The-Counter analgesic use. Eur J Pain. 2019;23:1747–62.
Gelis A, Dupeyron A, Legros P, Benaim C, Pelissier J, Fattal C. Pressure ulcer risk factors in persons with spinal cord injury part 2: the chronic stage. Spinal Cord. 2009;47:651–61.
Zakrasek EC, Creasey G, Crew JD. Pressure ulcers in people with spinal cord injury in developing nations. Spinal Cord. 2015;53:7–13.
Erosa NA, Berry JW, Elliott TR, Underhill AT, Fine PR. Predicting quality of life 5 years after medical discharge for traumatic spinal cord injury. Br J Health Psychol. 2014;19:688–700.
Hawran S, Biering-Sørensen F. The use of long leg calipers for paraplegic patients: a follow-up study of patients discharged 1973-82. Spinal Cord. 1996;34:666–8.
Jakimovska VM, Kostovski E, Biering-Sorensen F, Lidal IB. Psychological distress and user experiences with health care provision in persons living with spinal cord injury for more than 20 years. Spinal Cord. 2017;55:864–9.
Trgovcevic S, Milicevic M, Nedovic G, Jovanic G. Health condition and quality of life in persons with spinal cord injury. Iran J Public health. 2014;43:1229–38.
Waring WP 3rd, Biering-Sorensen F, Burns S, Donovan W, Graves D, Jha A, et al. 2009 review and revisions of the international standards for the neurological classification of spinal cord injury. J Spinal Cord Med. 2010;33:346–52.
Hartkopp A, Bronnum-Hansen H, Seidenschnur AM, Biering-Sorensen F. Suicide in a spinal cord injured population: its relation to functional status. Arch Phys Med Rehabil. 1998;79:1356–61.
Acknowledgements
We want to thank the study participants, Sunnaas Rehabilitation Hospital, employees at TOARILUC, and the QUOTA program.
Funding
The study was supported by the Quota program, Norway.
Author information
Authors and Affiliations
Contributions
VJ was responsible for designing and writing the protocol, inclusion of participants, extracting and analysing data, interpreting results and writing the paper. FBS, IBL, and EK contributed to designing the protocol, analysing data interpreting results, and providing feedback on the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteer were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Jakimovska, V.M., Biering-Sørensen, F., Lidal, I.B. et al. Community dwelling life- and health issues among persons living with chronic spinal cord injury in North Macedonia. Spinal Cord 60, 245–250 (2022). https://doi.org/10.1038/s41393-021-00688-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00688-4