Abstract
Study design
Animal proof of principle study.
Objectives
Bladder and bowel dysfunction are common after spinal cord injury (SCI) and in the elderly. Neurokinin 2 receptor agonists are known to produce on-demand urination and defecation in adult SCI rats. This study compared the ability of a neurokinin 2 receptor (NK2R) agonist to produce bladder and colorectal contractions in both young adult and aged SCI rats.
Setting
Dignify Therapeutics and Integrated Laboratory Systems, Durham, NC USA.
Methods
Bladder and colorectal pressure and voiding efficiency were measured in response to the NK2R agonist, [Lys5,Me,Leu9,Nle10]-NKA(4-10) (LMN-NKA), in anesthetized animals. The potency and efficacy of LMN-NKA was examined in young adult and aged SCI (T3 or T9 transected) rats, with young adult and aged spinal intact rats included as controls.
Results
LMN-NKA (3–300 μg/kg i.v.) produced dose-dependent increases in bladder and colorectal pressure in all anesthetized rats. No differences in the bladder or colorectal pressure responses or voiding efficiency were observed with age or after SCI. The level of SCI did not change the pharmacodynamic responses to the agonist.
Conclusions
An NK2R agonist produced similar responses in young adult and aged SCI rats, suggesting this class of agonists could be used as a potential therapy to induce on-demand urination and defecation in aged populations, with or without SCI.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) disrupts voluntary control of the bladder and bowel. Acute SCI results in a paralyzed, or a reflexive, bladder and bowel, and poor colonic motility. Over time, individuals with injuries above the sacral spinal level develop weak, involuntary, ineffective bladder contractions, often accompanied by bladder sphincter dyssynergia [1, 2], urinary retention, and overflow urinary incontinence (i.e., neurogenic bladder). SCI-induced bowel dysfunction leads to constipation and fecal impaction accompanied by an increase in the incidence of fecal incontinence in individuals with weak anal sphincters and pelvic floor muscles [3] (i.e., neurogenic bowel). The inability to voluntarily, and independently, control urination and defecation significantly impairs quality of life. A complicating factor involved with neurogenic bladder and bowel dysfunction in individuals with SCI rostral to the sympathetic outflow from the spinal cord (i.e., rostral to T6) is autonomic dysreflexia, which is a marked and potentially harmful elevation in blood pressure that is often associated with bladder catheterization and bowel evacuation [4].
Aging is also associated with bladder and bowel dysfunction, such as increased fibrosis of the bladder that reduces bladder capacity and contractility [5,6,7]. These changes increase the residual volume of urine and cause more frequent voiding. In addition, the sphincters and pelvic floor muscles weaken with age, leading to increased episodes of urinary and fecal incontinence. Incontinence severely decreases an individual’s quality of life and often results in an inability to live independently.
The average age of persons acquiring an SCI has increased from ~29 years in the 1970s to 43 years in 2015 [8]. Life expectancy of people with paraplegia is similar to that of the general population and is decreased by ~10 years in those with tetraplegia [6, 8]. Given that SCIs are mainly acquired by adults, and these adults eventually join the aged population, it is important to understand the relationship between SCI and aging, particularly with respect to potential pharmaceutical treatments.
A pharmaceutical product that could be used repeatedly, on-demand, to initiate urination and defecation by directly contracting the bladder and/or bowel could greatly improve independence and quality of life of aged as well as SCI individuals. Neurokinin 2 receptors (NK2R) are expressed on bladder and bowel smooth muscle and activation of NK2Rs induces smooth muscle contraction [9,10,11,12]. Previous studies in young adult, anesthetized, intact, and SCI animals showed that NK2R agonists, such as [Lys5,Me,Leu9,Nle10]-NKA(4-10) (LMN-NKA) increase bladder and colorectal pressures [13,14,15], resulting in urination and defecation in awake animals [16, 17].
The present studies were designed to determine if NK2R-meditated bladder and colorectal responses were similar in aged, compared to young adult, SCI rats. The studies compared the potency and efficacy of LMN-NKA in anesthetized young adult vs. aged SCI rats, with age-matched, spinal intact rats included as controls.
Methods
Female and male Fischer Brown Norway rats (30 young adult and 46 aged, National Institute of Aging rodent colony) were maintained under standard conditions of laboratory housing with unlimited access to food and water. Details of the animal numbers/group are shown in the figures and are reported in Supplemental File 1. Young adult rats were 2–4 months old and aged rats were 16–20 months old. Body weights for young adult and aged females were 200–230 and 230–340 g, respectively; and weights for males were 310–410 and 460-570 g, respectively. All experiments conformed with NIH Guidelines for the Care and Use of Laboratory Animals and were approved by the Integrated Laboratory Systems Animal Care and Use Committee.
Spinal cord injury (SCI)
Acute SCI was performed as a single surgical produce without recovery from anesthesia. Using aseptic procedures, the skin and muscle over the upper-middle thoracic vertebrae were incised, the spinal cord was exposed by a laminectomy, and the spinal cord was transected at T3 or T9 [16]. Spinal intact rats were naïve and did not receive a sham surgical procedure.
Cystometry and manometry studies
Rats were anesthetized with subcutaneous urethane (1.0–1.2 g/kg).
Blood pressure was monitored continuously via a cannula inserted into the carotid artery. Bladder and colorectal pressures were monitored as previously described [15]. A flared tipped catheter (PE50) was inserted into the bladder via a small incision made in the dome and secured in place with suture. The catheter was then connected to an infusion pump (Harvard Apparatus; Perfusion Pump PhD2000) via a three-way stopcock to allow bladder filling (0.04–0.1 ml/min with 0.9% saline) and removal of residual volume. Bladder pressure was monitored using a pressure transducer (Utah Medical Products; DelTran II) connected to a bridge amplifier (Transbridge 4M, World Precision Instruments). Bladder capacity was determined by filling the bladder with saline until fluid leaked through the urethra, the leaked volume was measured and recorded as the voided volume. The bladder was then carefully emptied via a 1 mL syringe attached to the stopcock to measure the residual volume. Subsequently, the bladder was filled to 70% of capacity, and vehicle or ascending doses of LMN-NKA were administered. When voiding/leaking occurred, bladder voiding pressure was recorded, and the voiding efficiency (VE) (voided volume/(voided volume + residual volume) × 100%) was calculated. Colorectal pressure was monitored via a balloon catheter inserted ~3 cm into the rectum through the anus and connected to a pressure transducer (Utah Medical Products; DelTran II) and bridge amplifier (Transbridge 4M, World Precision Instruments).
The NK2R agonist LMN-NKA (Bachem, CA) was administered via intravenous bolus injection through a cannula placed in the jugular vein. Cumulative doses were separated by at least 20 min to allow for responses to recover to pre-dose baseline. Intravenous saline was administered as a vehicle control.
Data analysis
Bladder and colorectal pressures were recorded via LabChart software through a PowerLab/8SP data acquisition system (version 7 and 8; ADInstruments, Australia). Measurements included baseline pressure, maximal pressure, time to voiding, and VE. Voiding responder rate was determined as the number of rats voiding (≥0.04 mL)/number of rats tested × 100%, for vehicle and each drug dose. Because no differences in responses to LMN-NKA were observed in intact or SCI male and female rats, (bladder pressures in males and females were compared using two-way ANOVA and no sex differences were observed, p = 0.63 and p = 0.31, for intact and SCI rats, respectively) data from males and females were combined. Data were analyzed using Excel (Microsoft, Redmond, WA) and Prism 6 (GraphPad Software Inc., San Diego, CA). Statistical analysis of parametric data was performed using a one-way or a two-way ANOVA, with Dunnett’s or Tukey’s multiple comparisons tests, as appropriate. Values are expressed as the mean + standard deviation (SD).
Results
Spinal intact young adult and aged rats
Although bladder capacity/body weight ratios were larger in aged rats compared to the young adults (aged 1.7 + 0.76, young adults 1.1 + 0.87, p = 0.007), there was no difference in baseline voiding pressures, blood pressure, or heart rate (p > 0.05). When the bladder was filled to 70% capacity, administration of LMN-NKA (0.1–300 μg/kg) induced dose-related voiding within 2 min of dosing. Figure 1 shows dose–response relationships for bladder pressure (1A), VE (1B) and colorectal pressure (1C) in young adult and aged rats in response to cumulative doses of LMN-NKA. A statistically significant increase in bladder pressure and VE was observed following LMN-NKA doses of 3–300 μg/kg, (p < 0.05), and there was no difference between young adult and aged rats, (p > 0.05). The onset of bladder contractions was rapid, with peak responses within 1 min, and all responses returned to baseline by ~5 min post dose. The bladder voiding pressure was 30–44 mmHg in young adult and aged rats, and the voiding responder rate was 92–100% following LMN-NKA dosing (3–300 μg/kg). Colorectal pressure was also increased (p < 0.05), with peak responses occurring 2–4 min post dose which returned to baseline by 30 min. No differences in colorectal pressures were observed in young adult and aged rats (Fig. 1C, e.g., colorectal pressure response to 30 μg/kg LMN-NKA was 57.3 + 10.8 and 54.2 + 15.7, in the young adult and aged group, respectively, p > 0.05). At doses 30–300 μg/kg LMN-NKA the balloon catheter was expelled therefore a full dose-response could not be obtained in the young adult intact rats.
A–C Intact young adult and aged rats, D–F aged SCI rats, and G–I young adult SCI. Drug-induced voiding was examined at 70% of the bladder capacity. Data are mean + SD. The number of rats/groups is indicated in parentheses in each graph. V vehicle. A two-way ANOVA and Tukey’s multiple comparison test was used to identify differences between the treatment groups. A–C A dose-related increase in response was seen for all measures and groups (bladder pressure and voiding efficiency both p < 0.0001, colorectal pressure p < 0.05). No age-related differences were observed in spinal intact rats. D–F All measures and groups showed a dose-related increase in responses (bladder pressure, voiding efficiency, and colorectal pressure all p < 0.0001, one-way or two-way ANOVA). No differences were observed between T3 and T9 SCI for bladder pressure or voiding efficiency (p > 0.05, 0.1–300 μg/kg). G–I A dose-related increase in response was seen for bladder pressure and voiding efficiency (p < 0.0001), drug-induced colorectal pressure did not reach statistical significance (p = 0.97, one-way ANOVA), probably due to the small N for this measure. No differences were observed between T3 and T9 SCI (p = 0.77 and p = 0.06 for bladder pressure and voiding efficiency, respectively). Bars and asterisk (*) indicate the doses of LMN-NKA that were different to vehicle. A full dose-response could not be obtained in the young adult intact (1C) and T9 SCI (1I) groups as the balloon catheter was expelled at the higher doses. The numbers of rats studied for the colorectal pressure and T3 SCI groups were limited due to the lack of availability of rats from the NIA rodent colony or commercial sources.
Acute T3 or T9 SCI in aged rats
Although bladder capacity/body weight ratio increased after SCI in aged rats (intact 1.7 + 0.76; T9 SCI 2.4 + 0.91; and T3 SCI 2.3 + 0.66, p < 0.01), baseline bladder pressure, blood pressure, and heart rate were not statistically different for any group (p > 0.05 for all measures). Administration of LMN-NKA (0.1–300 μg/kg) induced dose-related voiding within 2 min, at bladder pressures of 36–41 mmHg in aged SCI rats (Figs. 1D and 2). LMN-NKA (3–300 μg/kg) induced a statistically significant increase in VE in aged SCI rats, and the voiding responder rate was 85–100%. No significant differences were seen between T3 or T9, aged spinal injured rats. Colorectal pressure was recorded in one T3 and four T9 SCI-aged rats. LMN-NKA induced a dose-related increase in colorectal pressure with peak responses 2–4 min post dose and activity returned to baseline by ~30 min post dose (Figs. 1F and 2). The balloon catheter was expelled at higher doses resulting in only N = 1 for T9 SCI at doses of 30–300 μg/kg (Fig. 1F). There was no difference (p = 0.39) in the increase in colorectal pressure between intact aged rats (Fig. 1C) and aged SCI rats (Fig. 1F). LMN-NKA induced transient hypotension in aged rats at doses of 10–300 μg/kg, (Fig. 3A), but there was no statistically significant difference in blood pressure responses related to the level of SCI (p = 0.70). Importantly, LMN-NKA-induced hypertension was not observed in any of the animals, including those with T3 spinal transection (Fig. 3A).
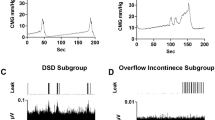
LMN-NKA (10 μg/kg IV) induced a rapid increase in bladder and colorectal pressure, with the main response returning to near baseline pressure by 5 min post dose. Voiding occurred within 2 min and coincided with the peak bladder pressure. No drug-induced increase in blood pressure was observed. Arrow indicates the time of dosing. Asterisk (*) indicates voiding.
Graphs show the percentage change in mean arterial pressure (MAP) in spinal intact, T3 and T9 acute SCI-aged (A) and young adult (B) rats. Blood pressure values were recorded continuously via the carotid artery and the effect of vehicle and LMN-NKA was expressed as a change from baseline values immediately before each dose. No change in baseline blood pressure was seen throughout the experiment. *LMN-NKA (10–300 μg/kg) induced a significant reduction in blood pressure (~15–20%) (p < 0.0001) in both aged and young adult rats. In aged rats the hypotensive effect of LMN-NKA was not different between intact, T9 and T3 SCI (p > 0.05) rats. In young adult rats, the hypotensive effect of LMN-NKA was not different between intact and T9 SCI (p > 0.05) rats (A). The LMN-NKA-induced hypotension was different (p > 0.001) in the T3 SCI group compared to the intact young adult rats (at 1–10 μg/kg) and the T9 SCI group (at 3–30 μg/kg), two-way analysis with Tukey’s multiple comparison test; however, no difference in the LMN-NKA-induced hypotension was observed between intact, T3 and T9 SCI was found at the higher doses (100–300 μg/kg), see B. V vehicle. Data are the mean + SD, N = 6–12/dose/group, except N = 3 for 0.1 μg/kg dose in the T3 SCI group.
Acute T3 or T9 SCI in young adult rats
A larger bladder capacity/body weight ratio was observed in young adult SCI, compared to intact young adult rats (intact 1.1 + 0.87; T9 SCI 2.2 + 0.18; and T3 SCI 2.8 + 0.49 (p < 0.001). There were no significant differences in bladder voiding pressure, baseline blood pressure or heart rate in intact young adult compared to young adult SCI rats (p > 0.05 for all measures). Neither acute spinal transection, nor the level of spinal transection, changed the ability of LMN-NKA to induce an increase in bladder pressure (32–44 mmHg) that was sufficient to elicit efficient voiding (Figs. 1G, H, >60% VE at doses 3–300 μg/kg) with a responder rate of 92–100%). In addition, there was no statistically significant difference in LMN-NKA-induced VE in young adult intact and SCI rats (compare Fig. 1B and H). LMN-NKA also induced increases in colorectal pressure in young rats after acute SCI at the T9 level (Fig. 1F, I). (Colorectal pressure was not recorded in animals with T3 SCI.) A full dose-response could not be obtained in the young adult T9 SCI (Fig. 1I) group as the balloon catheter was expelled at the higher doses. LMN-NKA produced a transient hypotension (10–20% change over baseline) at doses between 10 and 300 μg/kg (Fig. 3B), independent of age. At doses of 3–30 μg/kg hypotension was greater in young adult T3 SCI rats compared to intact and T9 young adults (Fig. 3B).
Discussion
Morphological and neural changes in the aging bladder may result in inefficient voiding and incontinence [6, 18]. Zhao et al. [19] reported that the aged rat bladder has an increased bladder capacity with increased spontaneous activity and residual volume. These findings were supported in the current study. Importantly, these physiological differences did not change the ability of the NK2R agonist to increase bladder voiding pressures and VE in aged, compared to young adult, rats.
The present study demonstrates that administration of the NK2R agonist LMN-NKA induces a bladder contraction that is sufficient to produce urination in anesthetized young adult and aged rats. LMN-NKA-induced increases in bladder pressure and VE were not statistically different in young adult SCI compared to aged SCI rats, nor in intact young adult and aged control rats. LMN-NKA also increased colorectal pressure between 30 and 60 mmHg across all doses and treatment groups. The level of SCI (T3 or T9) did not affect the ability of LMN-NKA to induce bladder and colorectal contractions. These results indicate that activation of NK2R receptors produces similar effects on the bladder and rectum of young adult and aged SCI rats. The present studies also provide preliminary evidence that hypertension associated with autonomic dysreflexia was not elicited by LMN-NKA-induced bladder or colorectal contractions in anesthetized rats with T3 spinal transection, although anesthesia may have blunted cardiovascular responses. Further studies examining the effect of NK2R agonists on cardiovascular function in awake preclinical models should be conducted to verify the lack of hypertension being triggered by drug-induced bladder or colorectal contractions.
NK2Rs are expressed at several sites in the micturition pathway, including the bladder and urethral smooth muscle [11, 12], and NK2R agonists induce bladder contractions that are accompanied by voiding. The current data confirm that LMN-NKA induces bladder contractions of sufficient intensity to overcome any urethral resistance in anesthetized spinal intact and acute aged SCI rats. This finding suggests that NK2R agonists can elicit bladder emptying despite the assumed presence of bladder sphincter dyssynergia that has been reported to develop after SCI [20, 21], but marked differences between sphincter function in rats vs. humans are apparent [1, 22, 23]. In the present studies, the maximum LMN-NKA-induced bladder voiding pressure was higher than the voiding/leak pressure recorded during baseline cystometry, suggesting that there was a small increase in urethral resistance, possibly caused by activation of NK2R on the urethral smooth muscle. Regardless, LMN-NKA induced urination, with an 80% VE, in young adult SCI and aged SCI rats under anesthesia. In addition, twice daily, drug-induced voiding with NK2R agonists across a 30-day period in young adult, T9 SCI rats resulted in no significant changes in bladder weights or capacity [16], suggesting that high pressure voiding did not occur over this time period. However, additional preclinical studies are warranted to evaluate the long-term effects of NK2R agonists on urethral function in vivo, and especially in SCI models with bladder-sphincter dyssynergia, since high pressure voiding can be harmful over an extended period of time.
Many individuals with SCI also have neurogenic bowel dysfunction manifested by symptoms of constipation, fecal incontinence, and abdominal pain, all of which restrict daily activities and impair quality of life. A longitudinal study in SCI individuals examined patterns of neurogenic bowel dysfunction and bowel management over 20 years [6]. The findings show that, over time, the proportion of individuals needing >30 min for each defecation, using laxatives, and the proportion of those that considered they were severely constipated, significantly increased. Bowel habits generally stabilize around 6 months post SCI [5, 6]. Therefore, the need for bowel management after SCI is lifelong. Similarly, bowel dysfunction is more prevalent in the elderly [24, 25].
In anesthetized young adult and aged rats, LMN-NKA was equally effective in increasing colorectal pressure, and SCI did not change the drug-induced pressure response. The LMN-NKA induced increase in colorectal pressure at higher doses often expelled the colorectal balloon catheter, making it difficult to record the pressures. NK2Rs have also been reported on the internal anal sphincter, and therefore an NK2R agonist might theoretically induce anorectal dyssynergia [26]. However, preliminary studies have shown robust defecation in intact aged rats and young adult chronic SCI rats, suggesting minimal, if any, drug-induced contraction of the anal sphincter ([16] and Lesley Marson, personal communication, September 2020). In addition, no attenuation nor sensitization of NK2R-induced defecation was seen after 30 days repeated administration of LMN-NKA in young rats with SCI [16]. Unpublished observations from our laboratory indicate that NK2R agonist-induced colorectal contractions are accompanied by anal relaxation in the rat, consistent with activation of intrinsic rectoanal inhibitory reflexes (Lesley Marson, personal communication, September 2020).
While our current and prior studies have not shown any obvious sex difference in NK2R agonist-induced defecation in rats, this should be examined further in human subjects. NK2R expression in the colon may increase with age in post-menopausal women, and NK2R mediated contractions were greater in human colon preparations from females compared to male subjects [27]. While administration of LMN-NKA did not increase blood pressure in young adult or aged T3 SCI rats, future studies should monitor cardiovascular parameters in the elderly and individuals with SCI above T6 who may be at risk of developing autonomic dysreflexia.
Conclusions
Despite morphological changes and increased bladder capacity after SCI and with aging, NK2R agonist-induced bladder and colorectal contractions were of sufficient strength to produce efficient voiding and colorectal pressure increases that are predicted to induce defecation. As expected for an agent producing direct smooth muscle contraction, the level of the SCI (T3 vs. T9) did not alter NK2R-induced bladder contraction or VE. These studies support the concept that selective NK2R agonists have potential as a novel class of therapeutics to produce on-demand urination and defecation in the aged SCI population.
Data archiving
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Bacsu CD, Chan L, Tse V. Diagnosing detrusor sphincter dyssynergia in the neurological patient. BJU Int. 2012;109:31–4.
Taweel WA, Seyam R. Neurogenic bladder in spinal cord injury patients. Res Rep Urol. 2015;7:85–99.
Hughes M. Bowel management in spinal cord injury patients. Clin Colon Rectal Surg. 2014;27:113–5.
Inskip JA, Lucci VM, McGrath MS, Willms R, Claydon VE. A Community perspective on bowel management and quality of lfe after spinal cord injury: The influence of autonomic dysreflexia. J Neurotrauma. 2018;35:1091–105.
Siroky MB. The aging bladder. Rev Urol. 2004;6:S3–7.
Nielsen SD, Faaborg PM, Finnerup NB, Christensen P, Krogh K. Ageing with neurogenic bowel dysfunction. Spinal Cord. 2017;55:769–73.
Ranson RN, Saffrey MJ. Neurogenic mechanisms in bladder and bowel ageing. Biogerontology. 2015;16:265–84.
National SCI Statistical Center (NSCISC). https://www.nscisc.uab.edu/.
Schmidt PT, Lordal M, Gazelius B, Hellstrom PM. Tachykinins potently stimulate human small bowel blood flow: a laser Doppler flowmetry study in humans. Gut. 2003;52:53–6.
Nakamura A, Tanaka T, Imanishi A, Kawamoto M, Toyoda M, Mizojiri G, et al. Bidirectional regulation of human colonic smooth muscle contractility by tachykinin NK(2) receptors. J Pharm Sci. 2011;117:106–15.
Giuliani S, Patacchini R, Barbanti G, Turini D, Rovero P, Quartara L, et al. Characterization of the tachykinin neurokinin-2 receptor in the human urinary bladder by means of selective receptor antagonists and peptidase inhibitors. J Pharm Exp Ther. 1993;267:590–5.
Palea S, Corsi M, Artibani W, Ostard E, Pietra C. Pharmacological characterization of tachykinin NK2 receptors on isolated human urinary bladder, prostatic urethra and prostate. J Pharm Exp Ther. 1996;277:700–5.
Rupniak NMJ, Katofiasc M, Marson L, Thor KB. NK2 and NK1 receptor-mediated effects of NKA and analogs on colon, bladder, and arterial pressure in anesthetized dogs. Naunyn-Schmiedebergs Arch Pharmacol. 2018;391:299–308.
Kullmann FA, Katofiasc M, Thor KB, Marson L. Pharmacodynamic evaluation of Lys(5), MeLeu(9), Nle(10)-NKA(4-10) prokinetic effects on bladder and colon activity in acute spinal cord transected and spinally intact rats. Naunyn-Schmiedebergs Arch Pharmacol. 2017;390:163–73.
Marson L, Thor KB, Katofiasc M, Burgard EC, Rupniak NMJ. Prokinetic effects of neurokinin-2 receptor agonists on the bladder and rectum of rats with acute spinal cord transection. Eur J Pharmacol. 2018;819:261–9.
Marson L, Piatt RK 2nd, Katofiasc MA, Bobbitt C, Thor KB. Chronic, twice-daily dosing of an NK2 receptor agonist [Lys(5),MeLeu(9),Nle(10)]-NKA(4-10), produces consistent drug-induced micturition and defecation in chronic spinal rats. J Neurotrauma. 2020;37:868–87.
Rupniak NMJ, Katofiasc M, Walz A, Thor KB, Burgard EC. [Lys(5),MeLeu(9),Nle(10)]-NKA(4-10) Elicits NK2 receptor-mediated micturition and defecation, and NK1 receptor-mediated emesis and hypotension, in conscious dogs. J Pharm Exp Ther. 2018;366:136–44.
Birder LA, Kullmann AF, Chapple CR. The aging bladder insights from animal models. Asian J Urol. 2018;5:135–40.
Zhao W, Aboushwareb T, Turner C, Mathis C, Bennett C, Sonntag WE, et al. Impaired bladder function in aging male rats. J Urol. 2010;184:378–85.
Agrawal M, Joshi M. Urodynamic patterns after traumatic spinal cord injury. J Spinal Cord Med. 2015;38:128–33.
Stoffel JT. Detrusor sphincter dyssynergia: a review of physiology, diagnosis, and treatment strategies. Transl Androl Urol. 2016;5:127–35.
Dolber PC, Gu B, Zhang X, Fraser MO, Thor KB, Reiter JP. Activation of the external urethral sphincter central pattern generator by a 5-HT(1A) receptor agonist in rats with chronic spinal cord injury. Am J Physiol Regul Integr Comp Physiol. 2007;292:R1699–706.
Gu B, Fraser MO, Thor KB, Dolber PC. Induction of bladder sphincter dyssynergia by kappa-2 opioid receptor agonists in the female rat. J Urol. 2004;171:472–7.
Deb B, Prichard DO, Bharucha AE. Constipation and fecal incontinence in the elderly. Curr Gastroenterol Rep. 2020;22:54–70.
Dumic I, Nordin T, Jecmenica M, Stojkovic-Lalosevic M, Milosavljevic T, Milovanovic T Gastrointestinal. Tract disorders in older age. Canadian J Gastroenterol Hepatol. 2019;6757524:1–19.
Tichenor SD, Buxton ILO, Johnson P, O’Driscoll K, Keef KD. Excitatory motor innervation in the canine rectoanal region: Role of changing receptor populations. Br J Pharmacol. 2002;137:1321–9.
Drimousis S, Markus I, Murphy TV, Perera DS, Phan-Thien KC, Zhang L, et al. Gender-related differences of tachykinin NK(2) receptor expression and activity in human colonic smooth muscle. J Pharm Exp Ther. 2020;375:28–39.
Acknowledgements
The authors would like to thank Nadia Rupniak and Ed Burgard for helpful discussion of the data. We gratefully acknowledge Integrated Laboratory Systems for their collaboration.
Funding
This study was supported by NIH grant AG057243.
Author information
Authors and Affiliations
Contributions
LM conceived, oversaw, conducted the studies and participated in the data analysis and did the major write up of the manuscript. RP was involved in data collection and data analysis. JBC was involved in data collection and data analysis. KBT conceived the studies and reviewed the data. All authors reviewed and contributed to editing the manuscript.
Corresponding author
Ethics declarations
Competing interests
LM, RP, JBC, and KBT are employed by Dignify Therapeutics. LM and KBT have equity ownership in Dignify Therapeutics.
Ethical statement
All procedures performed on animals were in accordance with the ethical standards of the Integrated Laboratory Systems animal care and use committees and followed the NIH Guidelines for the Care and Use of Laboratory Animals. We certify that all applicable institutional and governmental regulations concerning the ethical use of animals were followed during the course of this research. This article does not contain any studies with human participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Marson, L., Piatt, R., Cook, J.B. et al. Neurokinin 2 receptor-mediated bladder and colorectal responses in aged spinal cord injured rats. Spinal Cord 59, 1013–1017 (2021). https://doi.org/10.1038/s41393-021-00684-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-021-00684-8