Abstract
Background
We investigated the understudied influence of maternal diet quality, food timing, and their interactions during pregnancy on offspring metabolic health.
Methods
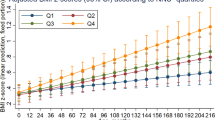
Maternal diet at 26–28 weeks’ gestation was assessed using a 24-h recall and adherence to the modified-healthy-eating-index (HEI-SGP) reflects diet quality. Predominant night-eating (PNE) was defined as consuming >50% of total daily energy intake from 19:00 to 06:59. Outcomes were offspring composite metabolic syndrome score and its components measured at age 6 years. Multivariable linear regressions adjusted for relevant maternal and child covariates assessed associations of diet quality and PNE with these outcomes.
Results
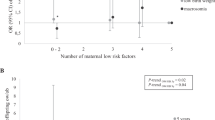
Up to 758 mother-child pairs were included. The mean(SD) maternal HEI-SGP score was 52.3(13.7) points (theoretical range: 0-100) and 15% of the mothers demonstrated PNE. Maternal diet quality showed inverse relationship with offspring Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) [β(95% CI): –0.08(–0.15, –0.02) per-10-point HEI-SGP increment; P = 0.012]. Maternal PNE was associated with a higher offspring HOMA-IR [0.28(0.06, 0.50); P = 0.012], with similar estimates after adjustment for children’s BMI and diet quality; the association was stronger for boys (P-interaction<0.001) and among mothers with lower diet quality (<median HEI-SGP) (P-interaction = 0.062).
Conclusions
Maternal PNE and low dietary quality were associated with a higher level of insulin resistance in early childhood, especially among boys.
Impact
-
We demonstrated that maternal predominant night-eating behavior and low-quality diet are associated with higher offspring insulin resistance.
-
Maternal low-quality diet and predominant night-eating behavior synergistically interact to influence offspring insulin resistance, particularly among boys.
-
While maternal diet quality and food timing impact the mother’s health, their influence on offspring long-term health outcomes through developmental programming is not well understood.
-
Our findings highlight the significance of maternal food timing and calls for further studies on its influence on child health through developmental programming. Targeting both dietary quality and food timing during pregnancy could be a promising intervention strategy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data are available upon request to the GUSTO team for researchers who meet the criteria for access to confidential data.
References
Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
Noubiap, J. J. et al. Global, regional, and country estimates of metabolic syndrome burden in children and adolescents in 2020: a systematic review and modelling analysis. Lancet Child Adolesc. Health 6, 158–170 (2022).
Georgesen, S. E. The Complex Problem of Childhood Obesity. West. J. Nurs. Res. 36, 579–580 (2014).
Gluckman, P. D., Buklijas, T. & Hanson, M. A. Chapter 1 - The Developmental Origins of Health and Disease (DOHaD) Concept: Past, Present, and Future. in The Epigenome and Developmental Origins of Health and Disease (ed. Rosenfeld, C. S.) 1–15 (Academic Press, Boston, 2016). https://doi.org/10.1016/B978-0-12-801383-0.00001-3.
Schoenaker, D. A., Soedamah-Muthu, S. S. & Mishra, G. D. The association between dietary factors and gestational hypertension and pre-eclampsia: a systematic review and meta-analysis of observational studies. BMC Med 12, 157 (2014).
Pang, W. W. et al. Higher Maternal Dietary Protein Intake Is Associated with a Higher Risk of Gestational Diabetes Mellitus in a Multiethnic Asian Cohort. J. Nutr. 147, 653–660 (2017).
Maslova, E. et al. Maternal protein intake during pregnancy and offspring overweight 20 y later. Am. J. Clin. Nutr. 100, 1139–1148 (2014).
Chen, L.-W. et al. Associations of maternal macronutrient intake during pregnancy with infant BMI peak characteristics and childhood BMI. Am. J. Clin. Nutr. 105, 705–713 (2017).
Cespedes, E. M. & Hu, F. B. Dietary patterns: from nutritional epidemiologic analysis to national guidelines. Am. J. Clin. Nutr. 101, 899–900 (2015).
Johnston, J. D., Ordovás, J. M., Scheer, F. A. & Turek, F. W. Circadian rhythms, metabolism, and chrononutrition in rodents and humans123. Adv. Nutr. 7, 399–406 (2016).
Berry, S. E. et al. Human postprandial responses to food and potential for precision nutrition. Nat. Med. 26, 964–973 (2020).
Acosta-Rodríguez, V. A., Rijo-Ferreira, F., Green, C. B. & Takahashi, J. S. Importance of circadian timing for aging and longevity. Nat. Commun. 12, 2862 (2021).
Soh, S.-E. et al. Cohort profile: Growing Up in Singapore towards healthy outcomes (GUSTO) birth cohort study. Int. J. Epidemiol. 43, 1401–1409 (2014).
Wright, K. P. et al. Entrainment of the human circadian clock to the natural light-dark cycle. Curr. Biol. CB 23, 1554–1558 (2013).
Washington, DC: U.S. Naval Observatory, 2016. Table of Sunrise/Sunset, Moonrise/Moonset, or Twilight Times for an Entire Year. https://aa.usno.navy.mil/calculated/rstt/year?ID=AA&year=2024&task=0&lat=1.3&lon=103.8&label=&tz=8&tz_sign=1&submit=Get+Data.
Han, C. Y. et al. A healthy eating index to measure diet quality in pregnant women in Singapore: a cross-sectional study. BMC Nutr. 1, 39 (2015).
Ong, Y. Y. et al. Cardiometabolic Profile of Different Body Composition Phenotypes in Children. J. Clin. Endocrinol. Metab. 106, e2015–e2024 (2021).
Ahrens, W. et al. Metabolic syndrome in young children: Definitions and results of the IDEFICS study. Int. J. Obes. 38, S4–S14 (2014).
Matthews, D. R. et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419 (1985).
Yin, J. et al. Insulin resistance determined by Homeostasis Model Assessment (HOMA) and associations with metabolic syndrome among Chinese children and teenagers. Diabetol. Metab. Syndr. 5, 71 (2013).
Ong, Y. Y. et al. Timing of introduction of complementary foods, breastfeeding, and child cardiometabolic risk: a prospective multiethnic Asian cohort study. Am. J. Clin. Nutr. 117, 83–92 (2023).
Chen, L.-W. et al. Maternal dietary quality, inflammatory potential and childhood adiposity: an individual participant data pooled analysis of seven European cohorts in the ALPHABET consortium. BMC Med. 19, 1–14 (2021).
Loy, S. L. et al. Associations of circadian eating pattern and diet quality with substantial postpartum weight retention. Nutrients 11, 2686 (2019).
Loy, S. L. et al. Maternal night-fasting interval during pregnancy is directly associated with neonatal head circumference and adiposity in girls but not boys. J. Nutr. 147, 1384–1391 (2017).
Padmapriya, N. et al. Associations of physical activity and sedentary behavior during pregnancy with gestational diabetes mellitus among Asian women in Singapore. BMC Pregnancy Childbirth 17, 364 (2017).
Rolands, M. R. et al. Development and evaluation of a diet quality index for preschool-aged children in an Asian population: The growing Up in Singapore towards healthy outcomes cohort. J. Acad. Nutr. Diet. 123, 299–308.e3 (2023).
Francis, E. C., Dabelea, D., Shankar, K. & Perng, W. Maternal diet quality during pregnancy is associated with biomarkers of metabolic risk among male offspring. Diabetologia 64, 2478–2490 (2021).
Loy, S. L. et al. Maternal circadian eating time and frequency are associated with blood glucose concentrations during pregnancy. J. Nutr. 147, 70–77 (2017).
Lakka, T. A. et al. A 2 year physical activity and dietary intervention attenuates the increase in insulin resistance in a general population of children: the PANIC study. Diabetologia 63, 2270–2281 (2020).
Chen, Y.-E., Loy, S. L. & Chen, L.-W. Chrononutrition during pregnancy and its association with maternal and offspring outcomes: A systematic review and meta-analysis of ramadan and non-ramadan studies. Nutrients 15, 756 (2023).
Loy, S. L. et al. Predominantly night-time feeding and maternal glycaemic levels during pregnancy. Br. J. Nutr. 115, 1563–1570 (2016).
Deniz, Ç. D., Özler, S., Sayın, F. K. & Eryılmaz, M. A. Associations between night eating syndrome and metabolic parameters in pregnant women. Turk. J. Obstet. Gynecol. 16, 107–111 (2019).
Gontijo, C. A. et al. Higher energy intake at night effects daily energy distribution and contributes to excessive weight gain during pregnancy. Nutrition 74, 110756 (2020).
Koop, S. & Oster, H. Eat, sleep, repeat – endocrine regulation of behavioural circadian rhythms. FEBS J. 289, 6543–6558 (2022).
Wehrens, S. M. T. et al. Meal timing regulates the human circadian system. Curr. Biol. 27, 1768–1775.e3 (2017).
Ruddick-Collins, L. C., Morgan, P. J. & Johnstone, A. M. Mealtime: A circadian disruptor and determinant of energy balance? J. Neuroendocrinol. 32, e12886 (2020).
Hood, M. M., Reutrakul, S. & Crowley, S. J. Night eating in patients with type 2 diabetes. Associations with glycemic control, eating patterns, sleep, and mood. Appetite 79, 91–96 (2014).
Bermúdez-Millán, A. et al. Night eating among latinos with diabetes: Exploring associations with heart rate variability, eating patterns, and sleep. J. Nutr. Educ. Behav. 54, 449–454 (2022).
Paul, H. A., Bomhof, M. R., Vogel, H. J. & Reimer, R. A. Diet-induced changes in maternal gut microbiota and metabolomic profiles influence programming of offspring obesity risk in rats. Sci. Rep. 6, 20683 (2016).
Godfrey, K. M. et al. Epigenetic gene promoter methylation at birth is associated with child’s later adiposity. Diabetes 60, 1528–1534 (2011).
Heijmans, B. T. et al. Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proc. Natl. Acad. Sci. 105, 17046–17049 (2008).
Giugliano, D., Ceriello, A. & Esposito, K. The effects of diet on inflammation: emphasis on the metabolic syndrome. J. Am. Coll. Cardiol. 48, 677–685 (2006).
Tajaddini, A., Kendig, M. D., Prates, K. V., Westbrook, R. F. & Morris, M. J. Male rat offspring are more impacted by maternal obesity induced by cafeteria diet than females—additive effect of postweaning diet. Int. J. Mol. Sci. 23, 1442 (2022).
Ricart, W. et al. Maternal glucose tolerance status influences the risk of macrosomia in male but not in female fetuses. J. Epidemiol. Community Health 63, 64–68 (2009).
Chen, L.-W. et al. Maternal macronutrient intake during pregnancy is associated with neonatal abdominal adiposity: The growing up in Singapore towards healthy outcomes (GUSTO) study. J. Nutr. 146, 1571–1579 (2016).
Chen, L.-W. et al. Associations of maternal dietary inflammatory potential and quality with offspring birth outcomes: An individual participant data pooled analysis of 7 European cohorts in the ALPHABET consortium. PLoS Med. 18, e1003491 (2021).
Rojas-Gómez, A. et al. Pregnancy homocysteine and cobalamin status predict childhood metabolic health in the offspring. Pediatr. Res. 93, 633–642 (2023).
Pedersen, J. F. Ultrasound evidence of sexual difference in fetal size in first trimester. Br. Med. J. 281, 1253 (1980).
Bukowski, R. et al. Human sexual size dimorphism in early pregnancy. Am. J. Epidemiol. 165, 1216–1218 (2007).
Eriksson, J. G., Kajantie, E., Osmond, C., Thornburg, K. & Barker, D. J. P. Boys live dangerously in the womb. Am. J. Hum. Biol. 22, 330–335 (2010).
Finan, B. et al. Targeted estrogen delivery reverses the metabolic syndrome. Nat. Med. 18, 1847–1856 (2012).
Igarashi, M. et al. Female-dominant estrogen production in healthy children before adrenarche. Endocr. Connect. 10, 1221–1226 (2021).
Tian, S. et al. Prevalence of prediabetes risk in offspring born to mothers with hyperandrogenism. eBioMedicine 16, 275–283 (2017).
Aiken, C. E. & Ozanne, S. E. Sex differences in developmental programming models. Reproduction 145, R1–R13 (2013).
Savard, C. et al. Trimester-specific assessment of diet quality in a sample of Canadian pregnant women. Int. J. Environ. Res. Public. Health 16, 311 (2019).
Tao, M.-H., Liu, J.-L. & Nguyen, U.-S. D. T. Trends in diet quality by race/ethnicity among adults in the United States for 2011–2018. Nutrients 14, 4178 (2022).
Loy, S. L. et al. Chrononutrition during pregnancy: A review on maternal night-time eating. Nutrients 12, 2783 (2020).
Acknowledgements
We would like to thank the GUSTO study group, which includes Allan Sheppard, Amutha Chinnadurai, Anne Eng Neo Goh, Anne Rifkin-Graboi, Anqi Qiu, Arijit Biswas, Bee Wah Lee, Birit F.P. Broekman, Boon Long Quah, Borys Shuter, Chai Kiat Chng, Cheryl Ngo, Choon Looi Bong, Christiani Jeyakumar Henry, Claudia Chi, Cornelia Yin Ing Chee, Yam Thiam Daniel Goh, Doris Fok, E Shyong Tai, Elaine Tham, Elaine Quah Phaik Ling, Evelyn Chung Ning Law, Evelyn Xiu Ling Loo, Fabian Yap, Falk Mueller-Riemenschneider, George Seow Heong Yeo, Helen Chen, Heng Hao Tan, Hugo P S van Bever, Iliana Magiati, Inez Bik Yun Wong, Ivy Yee-Man Lau, Izzuddin Bin Mohd Aris, Jeevesh Kapur, Jenny L. Richmond, Jerry Kok Yen Chan, Joanna D. Holbrook, Joanne Yoong, Joao N. Ferreira., Jonathan Tze Liang Choo, Jonathan Y. Bernard, Joshua J. Gooley, Keith M. Godfrey, Kenneth Kwek, Kok Hian Tan, Krishnamoorthy Niduvaje, Kuan Jin Lee, Leher Singh, Lieng Hsi Ling, Lin Lin Su, Ling-Wei Chen, Lourdes Mary Daniel, Lynette P Shek, Marielle V. Fortier, Mark Hanson, Mary Foong-Fong Chong, Mary Rauff, Mei Chien Chua, Melvin Khee-Shing Leow, Michael Meaney, Mya Thway Tint, Neerja Karnani, Ngee Lek, Oon Hoe Teoh, P. C. Wong, Paulin Tay Straughan, Peter D. Gluckman, Pratibha Agarwal, Queenie Ling Jun Li, Rob M. van Dam, Salome A. Rebello, Seang-Mei Saw, See Ling Loy, S. Sendhil Velan, Seng Bin Ang, Shang Chee Chong, Sharon Ng, Shiao-Yng Chan, Shirong Cai, Shu-E Soh, Sok Bee Lim, Stella Tsotsi, Chin-Ying Stephen Hsu, Sue Anne Toh, Swee Chye Quek, Victor Samuel Rajadurai, Walter Stunkel, Wayne Cutfield, Wee Meng Han, Wei Wei Pang, Yap-Seng Chong, Yin Bun Cheung, Yiong Huak Chan and Yung Seng Lee. The study is supported by the National Research Foundation (NRF) under the Open Fund-Large Collaborative Grant (OF-LCG; MOH-000504; MOH-000504-05 THEME 4) administered by the Singapore Ministry of Health’s National Medical Research Council (NMRC) and the Agency for Science, Technology and Research (A*STAR). In RIE2025, GUSTO is supported by funding from the NRF’s Human Health and Potential (HHP) Domain, under the Human Potential Program. KMG is supported by the UK Medical Research Council (MC_UU_12011/4), the National Institute for Health Research (NIHR Senior Investigator (NF-SI-0515-10042) and NIHR Southampton Biomedical Research Center (NIHR203319)) and the European Union (Erasmus+ Program ImpENSA 598488-EPP-1-2018-1-DE-EPPKA2-CBHE-JP). L-WC is supported by grants (MOST110-2314-B-002-290-MY2; NSTC112-2314-B-002-322-MY3) from the Ministry of Science and Technology (now the National Science and Technology Council) and receives further financial support from the National Taiwan University Higher Education Sprout Project (111L7304, 111L7306, 110L7418, 110L881002) within the framework of the Higher Education Sprout Project by the Ministry of Education. For the purpose of Open Access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising from this submission.
Author information
Authors and Affiliations
Contributions
L.W.C. conceptualized the current study, conducted formal statistical analysis, and wrote the first draft of the manuscript. S.L.L., M.T.T., N.M., Y.Y.O., J.Y.T. contributed to data acquisition and curation. P.D.G., K.H.T., Y.S.C, K.M.G., J.G.E., F.Y., Y.S.L., and M.F.F.C. designed and led the GUSTO cohort study. All authors interpreted the findings and revised drafts of the manuscript. All authors read and approved the final version of the manuscript submitted for publication.
Corresponding author
Ethics declarations
Competing interests
K.M.G. and Y.S.C. are part of an academic consortium that has received research funding from Société Des Produits Nestlé S.A., Abbott Nutrition, Danone and BenevolentAI Bio Ltd, and are co-inventors on patents filed on nutritional factors and metabolic risk outside the submitted work. K.M.G. has received reimbursement for speaking at a Nestle Nutrition Institute conference. All other authors have no competing interests to declare that are relevant to the content of this article.
Consent to publish
This study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All participants provided informed consent upon recruitment, and the study was approved by the Domain Specific Review Board of Singapore National Healthcare Group (D/2009/021) and the Centralised Institutional Review Board of SingHealth (2018/2767).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, LW., Loy, S.L., Tint, M.T. et al. Maternal pregnancy diet quality, night eating, and offspring metabolic health: the GUSTO study. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03574-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03574-w