Abstract
Although hypertension constitutes a substantial burden in conflict-affected areas, little is known about its prevalence, control, and management in Gaza. This study aims to estimate the prevalence and correlates of hypertension, its diagnosis and control among adults in Gaza. We conducted a representative, cross-sectional, anonymous, household survey of 4576 persons older than 40 years in Gaza in mid-2020. Data were collected through face-to-face interviews, anthropometric, and blood pressure measurements. Hypertension was defined in anyone with an average systolic blood pressure ≥140 mmHg or average diastolic blood pressure ≥90 mmHg from two consecutive readings or a hypertension diagnosis. The mean age of participants was 56.9 ± 10.5 years, 54.0% were female and 68.5% were Palestinian refugees. The prevalence of hypertension was 56.5%, of whom 71.5% had been diagnosed. Hypertension was significantly higher among older participants, refugees, ex-smokers, those who were overweight or obese, and had other co-morbidities including mental illnesses. Two-thirds (68.3%) of those with hypertension were on treatment with one in three (35.6%) having their hypertension controlled. Having controlled hypertension was significantly higher in females, those receiving all medications for high blood pressure and those who never or rarely added salt to food. Investing in comprehensive but cost-effective initiatives that strengthen the prevention, early detection and timely treatment of hypertension in conflict settings is critical. It is essential to better understand the underlying barriers behind the lack of control and develop multi-sectoral programs to address these barriers.
Similar content being viewed by others
Introduction
Evidence suggests that noncommunicable diseases (NCDs) have replaced infectious diseases as leading causes of morbidity and mortality in protracted conflict settings [1, 2]. Political instability, high stress levels, forced migration, and health system prioritization of lifesaving interventions can hamper NCD management and prevention [1]. Socioeconomic vulnerabilities such as overcrowding, low quality housing, and poor infrastructure can impede physical activity and access to nutritious food and also increase psychological distress, while coping strategies may include increased smoking and alcohol use [2].
The Gaza Strip is a narrow sliver of land (45 km long) between Israel, Egypt, and the Mediterranean Sea, home to around 2 million people, making it one of the world’s most densely populated areas [3]. According to the Palestinian Central Bureau of Statistics (PCBS) two thirds of Gaza’s inhabitants (66%) are refugees [3], most having been forcibly displaced from their original villages and cities following the Arab–Israeli conflict of 1948. Around 40% of the refugees in Gaza live in one of the eight refugee camps [3] but all refugees have the same civil legal status and entitlements as non-refugees, including access to social services, employment, and other rights. However, expropriation of land has created a condition of dispossession that has further compromised Palestinians’ abilities to withstand the deliberate de-development strategy pursued by Israel, through punitive economic and military policies. Israel still has overall sovereignty of Gaza, controlling its borders, economy, movement of goods and people, electricity, communications, and security—the key aspects of Palestinians’ lives [4].
The key socioeconomic and environmental determinants of health for the entire Gaza population have been negatively affected by the ongoing conflict which has continued for more than seven decades. This includes 16 years of strict blockade and economic collapse, which has increased health-related vulnerabilities. Gaza suffers from a high NCD burden [5] in the context of occupation, poverty, profound psychosocial distress, and limited access to health services. Nearly half of the households in Gaza are food insecure [3, 6], and 80% of the population is highly reliant on external assistance, particularly food. The United Nations Office for the Coordination of Humanitarian Affairs has repeatedly described the situation in Gaza as a chronic emergency and a protracted human dignity crisis [7].
The Gazan healthcare system is largely fragmented, poorly governed and under-funded, composed of mixed public/private/humanitarian services provided by the Ministry of Health, the United Nations Relief and Works Agency for Palestine Refugees in the Near East (UNRWA), nongovernmental organizations, and private for-profit operators [8]. While the Ministry of Health serves medically insured refugees and non-refugees, UNRWA, provides social services including health to the refugee population in Gaza. Nearly 40% of total health expenditure in Gaza is out-of-pocket [8]. Despite that health insurance coverage is widespread (more than 90% of households), still it does not meet people’s needs; few medicines are covered by insurance (if available at all), and there are limited specialist services and long waiting lists [4]. While people are ordinarily able to access basic health services, access becomes challenging during renewed outbreaks of conflict, and access to advanced services outside Gaza (such as radiotherapy, advanced cardiac and neurosurgery) remains limited [4]. Despite the limited available resources, inefficiencies in the health care system are still common and resources are unnecessarily wasted due to duplication, fragmentation and ineffective coordination including weak referral systems among service providers [8].
Hypertension is one of the most important risk factors for NCDs, and a recent systematic review found that hypertension constitutes a substantial burden in humanitarian settings [2]. However, its prevalence, risk factors and management in Gaza is poorly investigated. One survey conducted in 2017 reported that 28.4% of the adult population in Gaza had hypertension, but this study was limited by its non-representative sample and suboptimal methodology for measuring blood pressure [9]. Furthermore, a broader understanding of the hypertension cascade of care in Gaza is urgently needed to identify barriers and quantify unmet needs to diagnosis, treatment, and control. We therefore aimed to estimate the prevalence and correlates of hypertension among adults in Gaza, including an assessment of sociodemographic inequalities across the cascade of care.
Subjects and methods
Design and sampling
We conducted a representative, cross-sectional, anonymous, household survey of persons older than 40 years living in all five governorates of the Gaza Strip. We used the 2017 Population and Housing Census as the sampling frame to select enumeration areas (the primary sampling units) from each sampling stratum (North Gaza, Gaza, Dier Al Balah, Khan Yunis, and Rafah governorates) using a systematic cluster random sampling method. We calculated the sample size as 4520 participants from 2443 households based on an estimated prevalence of coronary artery disease (11.3%) [9], a response rate of 90.0%, and design effect of 1.5.
We selected 163 clusters proportionate to the size of the population in the five governorates. In each cluster, the PCBS provided a starting point and data collectors approached every 10th household until 15 were sampled. In each household, we interviewed one eligible male and one eligible female older than 40 years old. If multiple eligible participants of the same sex lived in the same household, we randomly selected one based on a Kish selection grid. We replaced non-respondent or ineligible households using the same selection criteria.
We trained interviewers for four days prior to data collection between March and July 2020, which was delayed for eight weeks due to COVID-19 lockdown measures. A pair of interviewers visited each household and obtained verbal informed consent prior to data collection. We checked participants’ responses for completeness daily, included built-in quality control measures into our survey, and revisited subset of 220 households to verify responses. Where interviewers identified urgent clinical support required for participants, a referral pathway was put in place for to link them to accredited service providers. The study was approved by the Imperial College Research Ethics Committee (20IC5733), the American University of Beirut Institutional Review Board, and the Gaza Helsinki Committee (PHRC/HC/483/19).
Survey
We adapted our survey from previously validated surveys, prioritizing those conducted on Palestinian or Arab populations. Briefly, we collected information on participants’ demographics, social assistance, food insecurity (based on the Food Insecurity Experience Scale [10], mental wellbeing (based on the General Health Questionnaire-12 [11] and self-rated health. We asked diagnostic, management, and health service utilization questions about diabetes, hypertension, raised total cholesterol, cardiovascular diseases, chronic respiratory diseases, and cancer [12]. We assessed physical activity (based on the International Physical Activity Questionnaire short form [13], salt intake, tobacco use (based on the World Health Organization-WHO Steps Survey [14] and a detailed semi-quantitative food frequency questionnaire [14, 15] as key NCD risk factors.
We measured height to the nearest centimeter using a Seca 217 stadiometer (Seca GmbH & Co, Hamburg, Germany) and weight to the nearest 10 g using an adult, portable electronic Seca 876 scale. We measured waist circumference mid-way between the lateral lower rib margin and the iliac crest using a Seca 201 meter. We measured blood pressure using the Omron M3 automatic upper arm blood pressure device (Omron Healthcare Co., Ltd. Kyoto, Japan). We developed written guidelines on blood pressure measurement which were used to train data collectors. We ensured participants were at rest for at least 10 min, had abstained from exercising, smoking or drinking coffee for at least 30 min prior to measurement, had removed clothes that could constrict blood vessels, had an empty bladder, and sat straight in a relaxed position with uncrossed legs with their left arm at the heart level. We also ensured an appropriate size positioned one inch above the elbow, which the forearm supported on a table with an upward palm upward, and at least five minutes interval between the two blood pressure readings.
We took the average weight, height, and waist circumference from two consecutive readings. For both systolic blood pressure (SBP) and diastolic blood pressure (DBP), we also relied on two readings. Where there were inconsistencies between the two readings (more than 5 mmHg), we performed a third measurement. For each participant, average SBP and DBP was computed as the average of the recorded readings. The average blood pressure measures were those computed from all readings (two consecutive, or three if inconsistencies) performed. We excluded pregnant women (n = 12) and participants who had an amputation (n = 26) from anthropometric measurements.
Measures
Three outcome measures, reflecting the cascade of care, were total hypertension, diagnosed hypertension, and controlled hypertension. Participants were classified as hypertensive if having an average SBP ≥ 140 mmHg or average DBP ≥ 90 mmHg or a hypertension diagnosis. We defined diagnosed hypertension as anyone being informed by a doctor or other health worker that they had hypertension, or if they had taken medication for hypertension as prescribed by their doctor or another health care worker in the previous 2 weeks. We defined treated hypertension as taking, within the past 2 weeks, prescribed antihypertensive medications. We defined controlled hypertension as anyone with diagnosed hypertension with <140 mmHg systolic and <90 mmHg diastolic blood pressure readings.
Sociodemographic independent variables included age (10 year brackets), refugee status (refugee/non-refugee), sex (male/female), governorate (North Gaza/Gaza/Deir Al Balah/Khan Younis/Rafah), education (basic/intermediate/secondary or higher), wealth quintiles based on household assets, income per capita, household size, crowding index (<1/2–3/>3 people per room), locality (camp/non-camp), marital status (not married/engaged or married), employment (yes/no), food insecurity (secure [score 0–3]/mild-to-moderately insecure [4–6]/severely insecure [7,8]), health insurance (yes/no), and past-year social assistance (yes/no).
Risk factor independent variables included physical activity (low/moderate/high, based on the metabolic equivalent minutes per week), tobacco (never/current/quit), the Dietary Interventions to Stop Hypertension (DASH) index [16], and salt addition to food (always/often/sometimes/rarely/never). Independent variables included the presence of a co-morbidity (defined as the presence of at least one disease: diabetes (yes/no), elevated cholesterol (yes/no), heart attack/chest pain (yes/no), stroke (yes/no), cancer (yes/no) pulmonary disease (yes/no), body mass index (underweight [<18.5 kg/m2]/normal [18.5–24.9]/overweight [25.0–29.9]/obese [>30.0]), mental wellbeing (minimal mental illness or psychosocial distress [score <5]/mild [6,7]/moderate-severe [>7]), self-rated health (not good or not good at all/half-half/good or very good) [17].
Statistical analysis
We performed descriptive statistics to characterize our sample, stratified by sex, and to present the cascade of hypertension care. We used multiple logistic regression models to assess the crude and adjusted associations between independent variables and each outcome (total hypertension, diagnosed hypertension, controlled hypertension). Variables were selected based on potential risk factors, previously identified in the literature, related to hypertension regardless of their statistical association with the outcome [18]. We presented models clustered at the household level. We presented odds ratios, their 95% confidence interval (95% CI) and p value. We also presented the effect modification of age and sex on the prevalence, diagnosis, and control of hypertension. We calculated variance inflation factor to test for multicollinearity. Around 5% of data were excluded from the models due to missing data. We ran the models with and without missing data and found no differences in our findings so present models with missing data. We used Stata 15 (StataCorp) and Statistical Package for Social Sciences (SPSS) 25 (IBM) for these analyses.
Results
Sample characteristics
We obtained a 96.6% response rate and included 4576 participants, of whom 54.0% were females and 68.5% were refugees. Sample characteristics stratified by sex and having versus not having hypertension are detailed in Tables 1A and 1B. The mean age of participants was 56.9 ± 10.5 years, most resided in Gaza (34.4%) and in urban/semi-urban localities (85.7%), 41.6% had secondary or higher educational attainment, and 82.1% were unemployed. Males were significantly older, had higher educational attainment and were more likely to be employed. At the household level, the median monthly income was 804.7 New Israeli Shekels (NIS) (interquartile range [IQR] 516.7–1400.0 NIS) (USD 230.13, IQR 147.85–400.64) and mean household size was 6.27 ± 3.18. Only 42.9% of participants were food secure (Table 1A). Because of the harsh economic status, 77.1% of participants received some sort of assistance in the past 12 months. Most participants had health insurance (83.8%). Physical inactivity was prominent, 52.5% of male participants and 70.2% of female participants reported practicing low physical activity.
Self-reported prevalence of other NCD co-morbidities was 46.8% (Table 1A). Table 2 also shows that 25.8% of all participants reported having diabetes and 22.3% reported having elevated cholesterol level. Significant differences were found between males and females regarding self-reported heart attack, stroke, and cancer (Table 2). Male participants were more likely to report having heart attacks (13.3%) and strokes (5.9%) while less likely to report cancer (1.7%) as opposed to their female counterparts (Table 2).
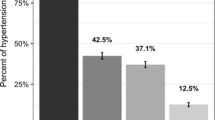
Hypertension cascade
The hypertension cascade of care is illustrated in Fig. 1. The total prevalence of hypertension in the study population (systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg) was 56.5% (n = 2586), of whom 71.5% (n = 1849) had been diagnosed, 68.3% (n = 1767) of all those with hypertension were on treatment, and 35.6% (n = 920) were controlled. Indeed, 34.3% (n = 887) of treated hypertensive were controlled, while 1.3% (n = 33) of the untreated were controlled. Of the diagnosed with hypertension (n = 1849), the majority were on treatment (n = 1767) reaching a high proportion of 95.6%, and half of those who were diagnosed and under treatment had their blood pressure controlled (n = 887). However, using the cut off points of ≥130/≥80 mmHg for diagnosis of hypertension, the 56.5% total prevalence observed in the study population is substantially increased to 79.5%; 77.4% among females and 81.98% among males.
The crude and adjusted odds of having hypertension are shown in Table 3. In the adjusted model, significantly higher odds of having hypertension were found among those who were older, refugees, had lower educational attainment, were ex-smokers, overweight or obese, had other co-morbidities, and had mild or moderate-to-severe mental illness. Geographical inequalities were also evident; living in Gaza governorate was associated with higher odds of hypertension than living in Khan Yunis governorate. All three age groups (50–59 years, 60–69 years, 70+ plus) had higher odds of hypertension than those aged 40–49 years and this relationship appeared stronger with the advances in age.
The crude and adjusted odds of having diagnosed hypertension compared to those with undiagnosed hypertension are shown in Table 4. In the adjusted model, significantly higher odds of diagnosed hypertension were found among those who were older, female, refugees, obese, had other co-morbidities, were engaged or married, had low physical activity, had moderate-to-severe mental illness, and who never added salt to food. Associations by age groups again showed a dose-dependent relationship.
Table 5 presents crude and adjusted odds of having controlled hypertension compared to those with uncontrolled hypertension. In the adjusted model, significantly higher odds of controlled hypertension were found among those who were female, mild-to-moderately food insecure, obese, had other co-morbidities, had received all medications for high blood pressure over the past year, did not use traditional home remedies for their blood pressure, and never or rarely added salt or salty sauces to food.
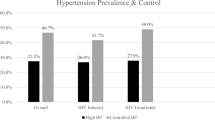
Figure 2 shows the effect modification of age and sex on hypertension prevalence, diagnosis and control. With the final model adjustments, we observe that males of younger age have higher risk of having hypertension than women, but the trend reverses for females over 70 years old. Conversely, females in all age categories have a higher chance of being diagnosed with hypertension than their male counterparts, and for all those diagnosed with hypertension, females also have an overall higher chance of controlling their blood pressure than their males counterparts (however the limited sample size increased the confidence interval in this group).
Discussion
To the best of our knowledge, this is the first representative, comprehensive household survey which explores the hypertension cascade in the Gaza Strip. Unlike other studies conducted in Gaza which were conducted at health facility level and focused on certain aspects of hypertension such as control or risk factors, it focuses on assessing hypertension cascade in the community. Surveying people at their households allowed for the inclusion of marginalized people who face barriers in accessing health care. Our 96.6% response rate is in spite of the difficulties faced with political uncertainties and COVID-19 restrictions, and is similar to other household surveys conducted in the Gaza Strip [3] and the demographics of our sample closely match the most recent national census conducted in 2017 [3]. We therefore have confidence in the representativeness of our sample and the external validity of our results and believe that these data provide an accurate reflection of the population burden of hypertension. Conclusions drawn from the paper can be inferred to analogous conflict-affected settings which usually lack such evidence. Moreover, findings of this study can help policy makers and actors to identify key points of intervention required to control hypertension at the prevention and management fronts in this challenging setting and also in humanitarian context.
Our findings show that over half of the sample had hypertension (using the cut off points of ≥140/≥90 mmHg), of whom about 70% reported being diagnosed and a third found to have their hypertension controlled. Projecting our results onto the full Gazan population, we estimate that the Gaza Strip has ~181,131 residents with hypertension, of whom 51,621 have not yet been diagnosed and 65,069 (including those undiagnosed) do not have their hypertension controlled. Our estimates of hypertension prevalence (56.5%) are over double previous estimates drawn from health facility data in the Gaza Strip [19] which report a prevalence of 27.1% among refugees aged 40 years and older and reflect substantial unmet need across the cascade of care and considerable scope to improve hypertension detection and management across the healthcare system. It is essential to scale up the current facility-based screening program and to launch outreach screening programs to reach more people in the community, including those who do not physically visit health facilities due to various accessibility barriers. Also, it is important to advocate to include hypertension community screening in the PCBS periodic household surveys in order to identify undiagnosed cases.
Our findings underscore important psychosocial and contextual correlates associated with the development of hypertension and suggest that these particularly vulnerable categories need to be proactively targeted in health promotion and screening programs as they are more at risk for developing hypertension (Table 3). Beside paying greater attention to those who are at greater risks for developing hypertension in health promotion and screening programs, including those who are older in age, refugees, those with lower educational attainment, ex-smokers, those who are overweight, or had other co-morbidities or mental illness, it is important to address the root causes of their vulnerabilities through launching a multi-sectoral prevention strategy to improve socioeconomic and environmental determinants of health.
We have identified an unprecedented burden of hypertension in this vulnerable population exposed to protracted conflict, Israeli occupation, profound poverty, psychological distress, and substandard living conditions. Although the prevalence of hypertension is going down world-wide [2], it is going up in Gaza [2], possibly due to the compounded socioeconomic and political challenges Gazans face for several decades. Conflict is consistently associated with hypertension in the academic literature [2] and this poses challenging barriers to overcome primary and secondary hypertension prevention efforts in the Gaza Strip. Opportunities for physical activity and nutritious food [4, 6] are severely restricted in a setting like the Gaza Strip where the population is highly dependent on social assistance to meet their healthcare and wider living needs. Men perform more poorly across the cascade of care than women, which may partly reflect greater interactions by women with the healthcare system for routine check-ups in reproductive and child health [19, 20]. Also, the opportunity for being diagnosed is higher among refugees who are served by UNRWA which provides free-of-charge and better regulated services [8].
Our findings identify that the undiagnosed Gazan population were predominantly younger, male, non-refugees, who are physically inactive, obese, and have poor mental health. These subgroups should be given priority in screening programs and measures targeting their health seeking behaviors. The revealed poor control status among people with hypertension is consistent with the literature which shows similar results in Gaza [20, 21]. It is worth noting that controlling hypertension is an outcome of interplay of many factors including individual, contextual and health services related factors and requires concerted multi-faceted actions at different levels. These include improving the quality of services, better adherence of patients with treatments, encompassing pharmaceutical and nonpharmaceutical approaches aimed at life-style changes together with adequate follow up and monitoring [22]. Addressing the social and conflict related determinants of poor health in this population is also crucial.
The worryingly high percentage of undiagnosed hypertension and the poor control status have substantial short- and long-term adverse complications for the residents of the Gaza Strip. However, increasingly limited financial resources and the ongoing war-like context has created tremendous constraints to accessibility and implementation of community-based screening programs [4]. Investing in comprehensive but cost-effective NCD management initiatives that mix pharmaceutical and non-pharmaceutical approaches that aim to strengthen early detection and timely treatment is critical [23]. Affordable and effective treatments for hypertension have large benefits on coronary heart disease, stroke, and renal disease and are important strategies to mitigate the burden of NCDs more generally in Gaza. Given that the majority of people diagnosed with hypertension were receiving medications demonstrates that the fragmented Gazan healthcare system can procure and prescribe anti-hypertensive medication, but this requires improvements in effectiveness. It is, however, a testimony to the resilience of organizations like UNRWA who maintain services in the face of tremendous political instability and uncertainty [24]. Major challenges may therefore center on primary prevention through behavior risk factor modification, screening methods to better detect the large numbers of undiagnosed people with hypertension, and high levels of adherence from both healthcare providers and patients to maintain good control.
We have shown that insights into hypertension prevalence and risk factors are characterized by intersecting, long-term compounded vulnerabilities resulting from protracted crisis and political turbulence, economic hardship, weak services provision, and inadequate governance which combined have exacerbate health vulnerabilities. The study is, however, not without its limitations. The cross-sectional design precludes causal inferences and the self-reported nature of many variables, including reporting a hypertension diagnosis, may be prone to recall or social desirability biases. However, we ensured to prioritize validated survey questions to minimize such biases and believe that these results will play a crucial role in the public health and health service approach to hypertension in the Gaza Strip. Also, menopause, a risk factor for cardiovascular disease, was not adjusted for in our analysis. Moreover, because this survey relied on self-reported responses, we did not collect data about the types of anti-hypertension medication and the control rate of different medications.
This study has a plethora of important research and policy implications. The richness of the data collected will provide the basis for our ongoing work to model reductions in disease burden and their cost-benefits, which is vital in the context of desperate financial challenges to healthcare in Palestine. The study provides insights into NCD prevalence and risk factors in areas characterized by intersecting, long-term compounded vulnerabilities resulting from protracted crisis and political turbulence, economic hardship, weak services provision, and inadequate governance which combine to exacerbate health vulnerabilities including the development of NCDs. Although the prevalence reported in this study for the different stages of the cascade of care seem superior than the worldwide and region trends recently reported [25, 26] actions are needed to generate better prevention of hypertension and improvement in its diagnosis and control [27]. Controlling hypertension and NCDs more broadly requires concerted multi-faceted actions at different levels, some of these much beyond the traditional boundaries of the health care system. Health promotion policies and programs that tackle the risk factors of hypertension, together with strategic surveillance and monitoring, is especially important given that the current basic package of health services is excessively curative. It is also essential to scale up NCD screening programs and implement proactive and community-level targeted outreach. Such targeting can be guided by our model estimates e.g., targeting younger, male refugees who are overweight and have poor mental health, and can be used to evaluate existing programs for their impact on inequalities. This study’s data and further analytical modeling techniques, modeling potential impacts of different interventions to reduce NCDs, can be used as ways to target the most cost-effective policies and interventions to reduce the development of hypertension and improve its screening and management.
Further research can also elicit the extent of out-of-pocket spending and its implications for healthcare delivery and quality. It is essential to study in more depth the underlying barriers behind the lack of hypertension control, to check for guideline implementation, and to set multi-sectoral programs to address these barriers.
Summary table
What is known about the topic?
-
Hypertension is now a leading cause of death and disability in protracted conflict settings, including Gaza.
-
Little is known about the prevalence and management of hypertension in Gaza.
What this study adds
-
This study provides the first robust, validated, and representative measure of hypertension in Gaza.
-
Of 4756 respondents, 56.5% had hypertension of which 71.5% had been diagnosed.
-
Profound sociodemographic inequalities exist in the prevalence and control of hypertension in this population.
Data availability
De-identified participant data will be made available, upon reasonable request, following assessment from the corresponding authors. Datasets will be made available following publication of this manuscript. To request data, please contact Dr. Bassam Abu Hamad at babuhamad@staff.alquds.edu.
References
Aebischer Perone S, Martinez E, du Mortier S, Rossi R, Pahud M, Urbaniak V, et al. Non-communicable diseases in humanitarian settings: ten essential questions. Confl Health. 2017;11:17 https://doi.org/10.1186/s13031-017-0119-8.
Jawad M, Vamos EP, Najim M, Roberts B, Millett C. Impact of armed conflict on cardiovascular disease risk: a systematic review. Heart. 2019;105:1388–94. https://doi.org/10.1136/heartjnl-2018-314459.
Palestinian Bureau of Statistics PCBS. Preliminary results of the population, housing and establishments census, 2017 PCBS, Ramallah. 2018. https://bit.ly/2GAlTU1.
Abu Hamad B, Jones N, Gercama I. Adolescent access to health services in fragile and conflict-affected contexts: the case of the Gaza Strip. Confl Health. 2021;15:40 https://doi.org/10.1186/s13031-021-00379-0.
Ellulu MS. Obesity, hypertension, and type-2 diabetes mellitus: the interrelationships and the determinants among adults in Gaza City, Palestine. Osong Public Health Res Perspect. 2018;9:289–98. https://doi.org/10.24171/j.phrp.2018.9.6.02.
Abu Hamad B, Jones N, Samuels F. Mental health and psychosocial challenges facing adolescent girls in conflict-affected settings: the case of the Gaza Strip. Arab J Psychiatr. 2020;31:169–80.
United Nations Office for the Coordination of Humanitarian Affairs (OCHA). Overview of Access of Palestinians from Gaza in 2016 OCHA. 2017.
United Nations Population Fund UNFPA. Palestine 2030. Demographic Change: Opportunities for Development. Palestine: UNFPA. 2016.
Jamee Shahwan A, Abed Y, Desormais I, Magne J, Preux PM, Aboyans V, et al. Epidemiology of coronary artery disease and stroke and associated risk factors in Gaza community –Palestine. PLoS One. 2019;14:e0211131 https://doi.org/10.1371/journal.pone.0211131.
Cafiero C, Viviani S, Nord M. Food security measurement in a global context: the food insecurity experience scale. Measurement. 2018;116:146–52.
Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27:191–7. https://doi.org/10.1017/s0033291796004242.
Sibai A, Tohme R, Mahfoud Z, Chaaya M, Hwalla N. Non-communicable diseases and behavioral risk factor survey: comparison of estimates based on cell phone interviews with face to face interviews. WHO Lebanon office Beirut, Lebanon: Final report submitted to World Health Organization-Lebanon office. 2009.
IPAQ. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ) – Short and Long Forms. 2005.
World Health Organization WHO. The WHO STEPwise approach to noncommunicable disease risk factor surveillance manual 2017.
Hamdan M, Monteagudo C, Lorenzo-Tovar ML, Tur JA, Olea-Serrano F, Mariscal-Arcas M. Development and validation of a nutritional questionnaire for the Palestine population. Public Health Nutr. 2014;17:2512–8. https://doi.org/10.1017/s1368980013002711.
Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168:713–20. https://doi.org/10.1001/archinte.168.7.713.
Abdulrahim S, El Asmar K. Is self-rated health a valid measure to use in social inequities and health research? Evidence from the PAPFAM women’s data in six Arab countries. Int J Equity Health. 2012;11:53 https://doi.org/10.1186/1475-9276-11-53.
Cuffee Y, Ogedegbe C, Williams NJ, Ogedegbe G, Schoenthaler A. Psychosocial risk factors for hypertension: an update of the literature. Curr Hypertens Rep. 2014;16:483 https://doi.org/10.1007/s11906-014-0483-3.
United Nations Relief and Works Agency for Palestine Refugees in the Near East UNRWA. Department of Health—Annual Report - 2020 UNRWA. 2021. https://www.unrwa.org/2020UNRWAHealthAnnualReport.
Elkahtib Z. Patients’ satisfaction with the non-communicable diseases services provided at UNRWA health centres in Gaza governorates: a cross-sectional study. Lancet 2018;391:S52 https://doi.org/10.1016/s0140-6736(18)30418-5.
World Health Organization. Country cooperation strategy for WHO and the Occupied Palestinian Territory: 2017–2020 World Health Organization. Regional Office for the Eastern Mediterranean. 2017.
Khdour MR, Hallak HO, Shaeen M, Jarab AS, Al-Shahed QN. Prevalence, awareness, treatment and control of hypertension in the Palestinian population. J Hum Hypertens. 2013;27:623–8. https://doi.org/10.1038/jhh.2013.26.
Akl C, Akik C, Ghattas H, Obermeyer CM. The cascade of care in managing hypertension in the Arab world: a systematic assessment of the evidence on awareness, treatment and control. BMC Public Health. 2020;20:835 https://doi.org/10.1186/s12889-020-08678-6.
World Health Organization. Noncommunicable diseases 2021. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases.
Abed Y, Abu-Haddaf S Risk factors of hypertension at UNRWA primary health care centers in Gaza governorates. International Scholarly Research Notices. 2013;2013.
Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80. Epub 20210824. https://doi.org/10.1016/s0140-6736(21)01330-1.
Datta BK, Ansa BE, Husain MJ. An analytical model of population level uncontrolled hypertension management: a care cascade approach. J Hum Hypertens. 2022;36:726–31. https://doi.org/10.1038/s41371-021-00572-x.
Acknowledgements
We would like to thank the Palestinian Central Bureau of Statistics for their methodological support, and the tremendous efforts of our data collectors and field supervisors in the Gaza Strip who showed courage, resilience, and dedication to conduct this survey in the most challenging of circumstances. The authors would like to express their deepest appreciation to the participants who contributed to this study. Participants were most generous in sharing their time and experiences.
Funding
This study was jointly funded by the UK’s Department for International Development (DFID), the Medical Research Council (MRC), the Economic and Social Research Council (ESRC) and Wellcome Trust’s Health Systems Research Initiative (HSRI) (MR/S012877/1).
Author information
Authors and Affiliations
Contributions
All authors have made substantive intellectual contributions to this project. EV, CM, JY, MJ, SB, HG, BA, and ZJ conceptualized the study. EV, CM, JY, MJ, SB, HG, and BA acquired the funding for this study. CM, JY, MJ, SB, HG, BA, and ZJ developed the research tools and methodology. HG, RA, GS, MR, ZJ, and BA curated the data. HG, ZJ, GS, MR, BA and RA conducted the formal data analysis. BH, ZJ, RA, GS, MR, HG, and MJ performed the investigation. ZJ, GS, MR, BA, MJ, and HG wrote the first draft of this manuscript. All authors reviewed and edited the draft and agreed to submit the manuscript for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the Imperial College Research Ethics Committee (20IC5733), the American University of Beirut Institutional Review Board, and the Gaza Helsinki Committee (PHRC/HC/483/19).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abu Hamad, B.A., Jamaluddine, Z., Safadi, G. et al. The hypertension cascade of care in the midst of conflict: the case of the Gaza Strip. J Hum Hypertens 37, 957–968 (2023). https://doi.org/10.1038/s41371-022-00783-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-022-00783-w