Abstract
Introduction
Obstructive sleep apnea (OSA) and severe obesity share a common pathophysiological phenomenon, systemic and tissue hypoxia. Hypoxaemia modifies microRNA expression, particularly, extracellular vesicles microRNAs which are involved in the progression of cardiovascular diseases, metabolic syndrome and cancer. We aim to evaluate extracellular vesicle miRNAs among patients with severe obesity with and without OSA and the effect of OSA and severe obesity treatment: continuous positive airway pressure (CPAP) and bariatric surgery.
Methods
Patients were selected from the Epigenetics Modification in Morbid Obesity and Obstructive Sleep Apnea (EPIMOOSA) study (NCT03995836), a prospective observational study of patients undergoing bariatric surgery. Patients were divided into OSA (Apnea-hyponea index (AHI) > 10) and non-OSA (AHI < 10). Patients with OSA were treated with CPAP for 6 months. Then, all patients had bariatric surgery and re-evaluated 12 months later. At each visit, blood samples were obtained for biobanking. Subsequently, extracellular vesicles were extracted, and then, miRNA expression was analysed.
Results
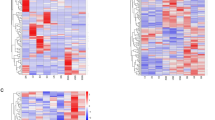
15 patients with OSA and 9 without OSA completed the protocol. At baseline, patients with OSA showed higher miR16, miR126 and miR320 (p < 0.05) and lower miR223 expression (p < 0.05) than those without OSA. In patients with severe obesity and OSA, after 6 months with CPAP, we observed a significant decrease in miR21 (p < 0.01), miR126 (p < 0.001) and miR320 (p < 0.001), with no changes in any miRNA in patients without OSA. No changes were detected in any miRNA after 6 months of bariatric surgery in patients with or without OSA.
Conclusion
Co-existance of OSA and severe obesity alters the profile of extracellular vesicle miRNAs. Bariatric surgery and weight loss did not reverse this effect meanwhile the treatment with CPAP in patients with severe obesity and OSA showed a recovery outcome in those extracellular vesicle miRNAs. Those facts remark the need for OSA screening in patients with severe obesity.
Clinical trial registration
The study has also been registered at ClinicalTrials.gov identifier: NCT03995836.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data are avalaible upon request.
References
Prevalence of obesity among adults, BMI >= 30 (crude estimate) (%). In. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/prevalence-of-obesity-among-adults-bmi-=-30-(crude-estimate)-(-).
Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81.
Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP. Pathophysiology of sleep apnea. Physiol Rev. 2010;90:47–112.
Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price NJ, Dinges DF, et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol. 2004;43:678–83.
Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116:281–97.
Feng S, Cong S, Zhang X, Bao X, Wang W, Li H, et al. MicroRNA-192 targeting retinoblastoma 1 inhibits cell proliferation and induces cell apoptosis in lung cancer cells. Nucleic Acids Res. 2011;39:6669–78.
Gagan J, Dey BK, Layer R, Yan Z, Dutta A. MicroRNA-378 targets the myogenic repressor MyoR during myoblast differentiation. J Biol Chem. 2011;286:19431–8.
Chan JA, Krichevsky AM, Kosik KS. MicroRNA-21 is an antiapoptotic factor in human glioblastoma cells. Cancer Res. 2005;65:6029–33.
Chen JJ, Zhao B, Zhao J, Li S. Potential roles of exosomal MicroRNAs as diagnostic biomarkers and therapeutic application in Alzheimer’s disease. Neural Plastic. 2017;2017:7027380.
Kalra H, Drummen GP, Mathivanan S. Focus on extracellular vesicles: introducing the next small big thing. Int J Mol Sci. 2016;17:170.
Hugel B, Martinez MC, Kunzelmann C, Freyssinet JM. Membrane microparticles: two sides of the coin. Physiology. 2005;20:22–7.
Trayhurn P. Hypoxia and adipose tissue function and dysfunction in obesity. Physiol Rev. 2013;93:1–21.
Kulshreshtha R, Ferracin M, Wojcik SE, Garzon R, Alder H, Agosto-Perez FJ, et al. A microRNA signature of hypoxia. Mol Cell Biol. 2007;27:1859–67.
Ivan M, Harris AL, Martelli F, Kulshreshtha R. Hypoxia response and microRNAs: no longer two separate worlds. J Cell Mol Med. 2008;12:1426–31.
Lacedonia D, Scioscia G, Palladino GP, Gallo C, Carpagnano GE, Sabato R, et al. MicroRNA expression profile during different conditions of hypoxia. Oncotarget. 2018;9:35114–22.
Lázaro J, Clavería P, Cabrejas C, Fernando J, Daga B, Ordoñez B, et al. Epigenetics dysfunction in morbid obesity with or without obstructive sleep apnoea: the EPIMOOSA study. Respir Res. 2020;21:42.
Lloberes P, Durán-Cantolla J, Martínez-García M, Marín J, Ferrer A, Corral J, et al. Diagnóstico y tratamiento del síndrome de apneas-hipopneas del sueño. Archiv Bronconeumol. 2011;47:143–56.
Sanz-Rubio D, Martin-Burriel I, Gil A, Cubero P, Forner M, Khalyfa A, et al. Stability of circulating exosomal miRNAs in healthy subjects. Sci Rep. 2018;8:10306.
Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–8.
Dixon JB, Schachter LM, O’Brien PE. Predicting sleep apnea and excessive day sleepiness in the severely obese: indicators for polysomnography. Chest. 2003;123:1134–41.
Kositanurit W, Muntham D, Udomsawaengsup S, Chirakalwasan N. Prevalence and associated factors of obstructive sleep apnea in morbidly obese patients undergoing bariatric surgery. Sleep Breath. 2018;22:251–6.
Lecube A, Sampol G, Lloberes P, Romero O, Mesa J, Morell F, et al. Asymptomatic sleep-disordered breathing in premenopausal women awaiting bariatric surgery. Obes Surg. 2010;20:454–61.
Peromaa-Haavisto P, Tuomilehto H, Kossi J, Virtanen J, Luostarinen M, Pihlajamaki J, et al. Obstructive sleep apnea: the effect of bariatric surgery after 12 months. A prospective multicenter trial. Sleep Med. 2017;35:85–90.
Sharkey KM, Machan JT, Tosi C, Roye GD, Harrington D, Millman RP. Predicting obstructive sleep apnea among women candidates for bariatric surgery. Journal of women’s health. 2010;19:1833–41.
Dewan NA, Nieto FJ, Somers VK. Intermittent hypoxemia and OSA: implications for comorbidities. Chest. 2015;147:266–74.
Dacal Quintas R, Tumbeiro Novoa M, Alves Perez MT, Santalla Martinez ML, Acuna Fernandez A, Marcos Velazquez P. Obstructive sleep apnea in normal weight patients: characteristics and comparison with overweight and obese patients. Archiv Bronconeumol. 2013;49:513–7.
Lecube A, de Hollanda A, Calanas A, Vilarrasa N, Rubio MA, Breton I, et al. Trends in bariatric surgery in spain in the twenty-first century: baseline results and 1-month follow up of the RICIBA, a National Registry. Obesity Surg. 2016;26:1836–42.
Durán J, Esnaola S, Rubio R, Rubio R, Iztueta A. Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med. 2001;163:685–9.
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–5.
Kolotkin RL, LaMonte MJ, Walker JM, Cloward TV, Davidson LE, Crosby RD. Predicting sleep apnea in bariatric surgery patients. Surg Obes Relat Dis. 2011;7:605–10.
Freitas LS, Silveira AC, Martins FC, Costa-Hong V, Lebkuchen A, Cardozo KHM, et al. Severe obstructive sleep apnea is associated with circulating microRNAs related to heart failure, myocardial ischemia, and cancer proliferation. Sleep Breath. 2020;24:1463–72.
Yang X, Niu X, Xiao Y, Lin K, Chen X. MiRNA expression profiles in healthy OSAHS and OSAHS with arterial hypertension: potential diagnostic and early warning markers. Respir Res. 2018;19:194.
Tian R, Wang J, Yan H, Wu J, Xu Q, Zhan X, et al. Differential expression of miR16 in glioblastoma and glioblastoma stem cells: their correlation with proliferation, differentiation, metastasis and prognosis. Oncogene 2017;36:5861–73.
Zhang HJ, Zhang YN, Teng ZY. Downregulation of miR16 protects H9c2(21) cells against hypoxia/reoxygenation damage by targeting CIAPIN1 and regulating the NFkappaB pathway. Mol Med Rep. 2019;20:3113–22.
Zeng Y, Zhang X, Kang K, Chen J, Wu Z, Huang J, et al. MicroRNA-223 attenuates hypoxia-induced vascular remodeling by targeting RhoB/MLC2 in pulmonary arterial smooth muscle cells. Sci Rep. 2016;6:24900.
Hijmans JG, Diehl KJ, Bammert TD, Kavlich PJ, Lincenberg GM, Greiner JJ, et al. Association between hypertension and circulating vascular-related microRNAs. J Hum Hypertens. 2018;32:440–7.
Kontaraki JE, Marketou ME, Zacharis EA, Parthenakis FI, Vardas PE. MicroRNA-9 and microRNA-126 expression levels in patients with essential hypertension: potential markers of target-organ damage. J Am Soc Hypertens. 2014;8:368–75.
Karolina DS, Tavintharan S, Armugam A, Sepramaniam S, Pek SL, Wong MT, et al. Circulating miRNA profiles in patients with metabolic syndrome. J Clin Endocrinol Metab. 2012;97:E2271–6.
Khalyfa A, Marin JM, Qiao Z, Rubio DS, Kheirandish-Gozal L, Gozal D. Plasma exosomes in OSA patients promote endothelial senescence: effect of long-term adherent continuous positive airway pressure. Sleep. 2020;43:zsz217.
Santamaria-Martos F, Benitez I, Ortega F, Zapater A, Giron C, Pinilla L, et al. Circulating microRNA profile as a potential biomarker for obstructive sleep apnea diagnosis. Sci Rep. 2019;9:13456.
Khalyfa A, Gozal D, Masa JF, Marin JM, Qiao Z, Corral J, et al. Sleep-disordered breathing, circulating exosomes, and insulin sensitivity in adipocytes. Int J Obes. 2018;42:1127–39.
Sanchez-de-la-Torre M, Khalyfa A, Sanchez-de-la-Torre A, Martinez-Alonso M, Martinez-Garcia MA, Barcelo A, et al. Precision medicine in patients with resistant hypertension and obstructive sleep apnea: blood pressure response to continuous positive airway pressure treatment. J Am Coll Cardiol. 2015;66:1023–32.
Bhattacharjee R, Khalyfa A, Khalyfa AA, Mokhlesi B, Kheirandish-Gozal L, Almendros I, et al. Exosomal cargo properties, endothelial function and treatment of obesity hypoventilation syndrome: a proof of concept study. J Clin Sleep Med. 2018;14:797–807.
O’Brien PE, Hindle A, Brennan L, Skinner S, Burton P, Smith A, et al. Long-term outcomes after bariatric surgery: a systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-centre review of 20-year outcomes after adjustable gastric banding. Obes Surg. 2019;29:3–14.
Adams TD, Davidson LE, Hunt SC. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2018;378:93–6.
Hubal MJ, Nadler EP, Ferrante SC, Barberio MD, Suh JH, Wang J, et al. Circulating adipocyte-derived exosomal MicroRNAs associated with decreased insulin resistance after gastric bypass. Obesity. 2017;25:102–10.
Bae YU, Kim Y, Lee H, Kim H, Jeon JS, Noh H, et al. Bariatric surgery alters microRNA content of circulating exosomes in patients with obesity. Obesity. 2019;27:264–71.
Alkandari A, Ashrafian H, Sathyapalan T, Sedman P, Darzi A, Holmes E, et al. Improved physiology and metabolic flux after Roux-en-Y gastric bypass is associated with temporal changes in the circulating microRNAome: a longitudinal study in humans. BMC Obes. 2018;5:20.
Hohensinner PJ, Kaun C, Ebenbauer B, Hackl M, Demyanets S, Richter D, et al. Reduction of premature aging markers after gastric bypass surgery in morbidly obese patients. Obes Surg. 2018;28:2804–10.
Lirun K, Sewe M, Yong W. A Pilot Study: the effect of Roux-en-Y gastric bypass on the serum microRNAs of the type 2 diabetes patient. Obes Surg. 2015;25:2386–92.
Wu Q, Li JV, Seyfried F, le Roux CW, Ashrafian H, Athanasiou T, et al. Metabolic phenotype-microRNA data fusion analysis of the systemic consequences of Roux-en-Y gastric bypass surgery. Int J Obes. 2015;39:1126–34.
Yeh CL, Cheng IC, Hou YC, Wang W, Yeh SL. MicroRNA-125a-3p expression in abdominal adipose tissues is associated with insulin signalling gene expressions in morbid obesity: observations in Taiwanese. Asia Pac J Clin Nutr. 2014;23:331–7.
Zhu Z, Yin J, Li DC, Mao ZQ. Role of microRNAs in the treatment of type 2 diabetes mellitus with Roux-en-Y gastric bypass. Braz J Med Biol Res. 2017;50:e5817.
Ortega FJ, Moreno M, Mercader JM, Moreno-Navarrete JM, Fuentes-Batllevell N, Sabater M, et al. Inflammation triggers specific microRNA profiles in human adipocytes and macrophages and in their supernatants. Clin Epigenet. 2015;7:49.
Wang Y, Wang DS, Cheng YS, Jia BL, Yu G, Yin XQ, et al. Expression of microRNA-448 and SIRT1 and prognosis of obese type 2 diabetic mellitus patients after laparoscopic bariatric surgery. Cell Physiol Biochem. 2018;45:935–50.
Dahlman I, Belarbi Y, Laurencikiene J, Pettersson AM, Arner P, Kulyte A. Comprehensive functional screening of miRNAs involved in fat cell insulin sensitivity among women. Am J Physiol Endocrinol Metab. 2017;312:E482–94.
Nardelli C, Iaffaldano L, Pilone V, Labruna G, Ferrigno M, Carlomagno N, et al. Changes in the microRNA profile observed in the subcutaneous adipose tissue of obese patients after laparoscopic adjustable gastric banding. J Obes. 2017;2017:6754734.
Nunez Lopez YO, Coen PM, Goodpaster BH, Seyhan AA. Gastric bypass surgery with exercise alters plasma microRNAs that predict improvements in cardiometabolic risk. Int J Obes. 2017;41:1121–30.
Ortega FJ, Mercader JM, Moreno-Navarrete JM, Nonell L, Puigdecanet E, Rodriquez-Hermosa JI, et al. Surgery-induced weight loss is associated with the downregulation of genes targeted by microRNAs in adipose tissue. J Clin Endocrinol Metab. 2015;100:E1467–76.
Blum A, Yehuda H, Geron N, Meerson A. Elevated levels of miR-122 in serum may contribute to improved endothelial function and lower oncologic risk following bariatric surgery.Isr Med Assoc J. 2017;19:620–4.
Acknowledgements
To my colleagues in the pulmonology department at Royo Villanova Hospital.
Funding
This research project has received grants from the Instituto Carlos III, Madrid, Spain PI15/01940, PI18/01524, PI21/01954), the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR-2017), and the Aragon Society of the Respiratory System (SADAR-2016).
Author information
Authors and Affiliations
Contributions
JL conceived, designed, wrote and approved the final version. DSR contributed to the design, writing, lab work and revised the paper. PC, CC, JF and AC contributed to acquire data. JMM contributed to the design, writing and revision of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study has been approved by the Aragon Institute of Health Sciences (Ethics Committee for Clinical Research of Aragon number: 23/2014). In accordance with recommendations from the Declaration of Human Rights, the Helsinki Conference and the IACS, patients must sign the informed consent form before being enroled in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lázaro, J., Sanz-Rubio, D., Clavería, P. et al. Effect of positive pressure ventilation and bariatric surgery on extracellular vesicle microRNAs in patients with severe obesity and obstructive sleep apnea. Int J Obes 47, 24–32 (2023). https://doi.org/10.1038/s41366-022-01230-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01230-z