Abstract
In 2000, the authors found endemic infections of mouse hepatitis virus, minute virus of mice, Syphacia obvelata, and Myobia musculi among mice in a large barrier facility at the University of Mainz. To eliminate the infections, they subdivided the facility into two distinct hygiene units. However, architectural constraints made it impossible to completely separate the HVAC systems of both hygiene units and to establish adequate personnel locks. To compensate for these suboptimal barrier conditions of the two newly established units, the authors replaced the open-top caging and open-servicing system with filter-top cages that were manipulated in cage-changing stations. The authors then depopulated the two units in series, independently eliminating the contaminated mice and restocking the units with SPF animals. In spite of the high infection pressure and the suboptimal barrier conditions, the authors had only a single case of recontamination.
Similar content being viewed by others
Main
Mouse strains with defined genetic mutations continue to play a pivotal role in biomedical research. In the year 2000 alone, an estimated 25 million mice were used in biomedical experiments1. Since intercurrent infections of laboratory mice with pathogenic microorganisms can severely confound experimental results2, murine facilities have to be adequately protected against specific infections and must establish suitable microbiological monitoring programs3,4. The classical model for protecting laboratory rodents against infection involves three elements: physical barriers supplied by separate HEPA-filtered HVAC systems that provide positive pressure for the inhibition of airborne infections, autoclaves for the sterilization of animal supply material, and wet or dry personnel locks. If, in spite of all countermeasures, a specific pathogen infiltrates such a barrier facility, the common strategy for decontamination involves complete depopulation of the unit and subsequent restocking with pathogen-free rodents. This drastic strategy clearly has the best chance of success; however, it requires that animal housing be completely (albeit temporarily) cleared, potentially presenting serious problems for researchers who use mice.
Filter-top and individually ventilated cages (microisolator cages) strictly serviced in cage-changing stations are now well established as efficient physical barriers against microorganisms. The efficacy of microisolator cages in slowing the spread of even highly infective laboratory animal pathogens has been demonstrated in several controlled studies5,6,7,8. However, controlled studies involve specific and well-defined cage-changing and sanitation procedures and are thus of only limited value for predicting the suitability of microisolator caging systems under less-controlled real-world conditions.
Here we report the elimination of two viral pathogens (mouse hepatitis virus (MHV) and minute virus of mice (MVM)) and two parasites (the pinworm Syphacia obvelata and the fur mite Myobia musculi) from a mouse facility by separating the area into two units with suboptimal barrier protection and independently sanitizing each unit by depopulation and restocking. It is likely that the success of the decontamination process resulted largely from the replacement of the previous open-top caging and open-servicing system by filter-top cages and strict servicing in cage-changing stations.
Methods
Housing
We housed laboratory mice in the Central Laboratory Animal Facility of the Johannes Gutenberg University of Mainz in an area referred to as the '13th-Floor Facility'. We maintained room climate according to the recommendations of the German Animal Welfare Act (temperature of 22 °C ± 2 °C, relative humidity of 55% ± 10%, illumination program with 12-h lights on and 12-h lights off). We fed the mice standard extruded diets (Ssniff Spezialdiäten GmbH, Soest, Germany) and tap water (quality-controlled according to Deutsche Trinkwasserverordnung) and housed them in type-2 cages with wood shavings as bedding material (Ssniff Spezialdiäten GmbH).
Hygiene management
We autoclaved all caging material in the same building (20 min, 118 °C) and then transported it to the mouse facility. During transportation the material was protected by a cover sheet to prevent contamination. We verified correct function of the autoclave quarterly. We introduced thermolabile materials into the facility after intensive cleaning and subsequent disinfection with 80% alcohol. Every two days, we disinfected and sanitized the floors of the animal facilities with Terralin (Schülke & Mayr, Norderstedt, Germany). Distinct barrier facilities were strictly separated at the personnel level and all animal rooms of a particular barrier were serviced without special hygienic precautions for the staff.
In contaminated areas, we housed mice in open-top type-2 cages (Ebeco, Castrop-Rauxel, Germany) and serviced them openly. No specific personnel locks were available in these contaminated areas, but protective coats and over-shoes were provided at the door to each room.
In sanitized areas, all cages were protected by filter-tops (Ebeco, Castrop-Rauxel, Germany) and all murine manipulations were performed in cage-changing stations (Tecniplast, Varese, Italy). We manipulated the rodents using forceps (disinfected with 80% alcohol) and protective gloves. The inner surface of the cage-changing stations was disinfected with 80% alcohol and the gloves were changed after each strain and each rack. In the decontaminated areas, we established one-way personnel locks where the animal care technicians and researchers were required to wear protective clothing and shoes as well as one-way face and hair masks prior to entering the housing areas. The provisional personnel locks allowed us to separate protective clothing from normal clothes, but lacked architecturally separated 'clean' and 'dirty' areas, as requested for lege artis locks.
Microbiological surveillance
We obtained murine blood samples from the tail vein and prepared serum according to standard procedures. We detected specific viral antibodies in the murine sera by ELISA technology using virus-coated plates purchased from Charles River Nederland (Maastricht, Netherlands). Serum samples that tested positive in the ELISA screening reaction were retested by a commercial laboratory (Biodoc, Hannover, Germany) using an immunofluorescence technique. We detected S. obvelata and M. musculi ova by microscopic analysis of anal and fur tape preparations, respectively. We tested all females that received embryo transfers for the presence of MHV- and MVM-specific antibodies, as well as for S. obvelata and M. musculi ova ∼7 weeks after embryo transfer.
We performed routine serological and parasitological testing in accordance with FELASA recommendations4. Briefly, we performed quarterly serological testing for MHV, mouse rotavirus, MVM, mouse parvovirus, pneumonia virus of mice, Sendai virus, and Theiler's murine encephalomyelitis virus, as well as parasitological analyses. We did not apply a sentinel system, instead randomly chosing samples from mice on all racks and in all rooms. Sample sizes constituted ∼3–5% of all cages (one sample per cage).
Antiparasite treatment
In 2000, we launched an ivermectin-based antiparasitic therapy9,10 in the contaminated mouse housing area and continued oral ivermectin therapy in contaminated areas until depopulation. We did not use antiparasitic treatment in areas restocked with pathogen-free mice.
Embryo transfer technology
To rederive contaminated mouse strains, we obtained two-cell-stage embryos from contaminated donor females. Integrity of the zona pellucida was controlled by microscopical inspection and zona-intact embryos were subjected to an enzymatic treatment using a 0.25% trypsin solution (Sigma-Aldrich, Steinheim, Germany) followed by ∼10 rinsing steps. We transferred embryos to pseudopregnant Crl:NMRI (Charles River, Sulzfeld, Germany) females according to standard protocols11. We housed rederived pathogen-free mouse strains in centralized breeding areas in the same building and then transferred them as needed to the experimental areas of the 13th-Floor Facility.
Cleaning and disinfection of contaminated areas
Areas previously used for the housing of contaminated mice were intensively cleaned by steam blasting at a temperature of 80 °C. Since formaldehyde or H2O2 fumigation12 or specific antiparasite disinfection could not be used for decontamination for safety reasons, we disinfected animal rooms by multiple spray treatments using 80% ethanol.
Results
Creation of provisional units
At the beginning of the year 2000, we established a microbiological monitoring system for the rodent facilities of the University of Mainz and found that the experimental animal facility (13th-Floor Facility), which housed ∼9,000 mice, was endemically contaminated with MHV, MVM, S. obvelata, and M. musculi. The viral and parasitic infections were in all animal rooms, and MHV and MVM showed prevalence rates of ∼100% and ∼10%, respectively.
To decontaminate the 13th-Floor Facility, we decided to provisionally separate the area into two distinct hygiene units, referred to as the '13th-Floor City' and '13th-Floor Clinic' (Fig. 1), and to independently eliminate the infections in these two units using a conventional depopulation and rederivation strategy. However, technical restrictions made it impossible to (1) separate the two corridors formerly connecting the 13th-Floor City and 13th-Floor Clinic in an air-proof way (Fig. 1, black arrows); (2) completely disconnect the HVAC systems of the newly created units; or (3) control for the air pressure between the two units. Thus, cross-contamination of both units by airborne pathogens could not safely be excluded. A further deficit of the two newly established hygiene barrier units (13th-Floor City and 13th-Floor Clinic) was the lack of appropriate two-way personnel locks. Instead, we established provisory one-way personnel locks at the entrance of each unit (Fig. 1).
The black line indicates the dimensions of the original facility, while the dotted black line shows how the facility was separated into two distinct units, referred to as the '13th-Floor City' and '13th-Floor Clinic'. Doors connecting the 13th-Floor City and 13th-Floor Clinic (black arrows) were permanently closed and sealed with silicone. Provisory 'one-way personnel locks' (asterisks) were established for both units. The rooms marked X, Y, and Z were each ventilated by independent HVAC systems. All ventilation systems had maximal-supply air filtration levels of EU7 (filtration efficiency = 80–90%). The air flow rates were 10–15 changes/hour for ventilation systems X and Z, and 6–10 changes/hour for ventilation system Y. We attempted to establish a positive air-pressure differential in the decontaminated rooms and a negative-pressure differential in the contaminated rooms; technical difficulties, however, made this unachievable in some cases (black circle: entrance to respective units, white arrows: emergency exits). The open circle indicates animal room 1306, where MHV recontamination occurred.
Embryo transfer for eradication of MHV and MVM infections
Between January 2001 and December 2003 we rederived a total of 75 murine strains by embryo transfer. The recipient females were housed in centralized breeding areas located in the same building as the 13th-Floor Facility and were tested for MHV, MVM, mites, and pinworms at weaning. Importantly, neither MHV- or MVM-specific antibodies nor parasite infections could be detected in any of the recipient females (N = 376). In full accordance with this result, no viral or parasite infections could be detected in the centralized breeding areas by routine microbiological monitoring.
Depopulation and restocking of mouse rooms
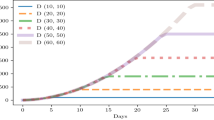
By transfering mouse strains to centralized breeding areas, the total number of mice originally housed in the 13th-Floor City and 13th-Floor Clinic was continuously reduced. In August 2001 (Fig. 2) we completely depopulated the 13th-Floor City and cleaned and disinfected all housing and service rooms as described earlier. In November 2001 we started to restock the unit with pathogen-free mice. We established filter-top cages and cage-changing stations prior to bringing the 13th-Floor City back into operation under SPF conditions. As already mentioned, the rationale of this measure was to compensate for the barrier deficits of this unit.
The black and white triangles and arrows represent time points for when the 13th-Floor City and 13th-Floor Clinic were depopulated of contaminated mice and restocked with pathogen-free animals, respectively. The horizontal double-arrow shows the span of time during which contaminated mice in the 13th-Floor Clinic and already sanitized animals in the 13th-Floor City coexisted. The vertical double-arrow shows the time point of MHV re-contamination of room 1306 (see Figure 1 for room location) in the 13th-Floor City. Please note that the total number of mice housed in the 13th-Floor City and 13th-Floor Clinic never dropped below 4,600 mice.
In January 2003, we eliminated the contaminated mice in the 13th-Floor Clinic and cleaned and disinfected all rooms in this unit. In July 2003 we restarted operations in the unit by introducing pathogen-free mice housed in filter-top cages and strictly serviced in cage-changing stations. In this context it should be mentioned that the procedures conducted with SPF mice in decontaminated areas (13th-Floor City and 13th-Floor Clinic) included breeding experiments, although the breeding quantity was significantly reduced as compared to the pre-separation facility.
Recontamination
Since depopulating and restocking the 13th-Floor City or 13th-Floor Clinic, we have not detected recontamination with MVM, S. obvelata, or M. musculi. Furthermore, we have not detected MHV recontamination in the 13th-Floor Clinic. In June 2002, we did detect a single case of MHV recontamination in the 13th-Floor City by routine serological testing. This infection appeared 7 months after we repopulated the unit with SPF mice and affected only room 1306 (Fig. 2). After detecting the recontamination, we performed MHV-specific serum analyses on all cages of the affected and neighboring mouse rooms. The additional tests showed that the majority of cages in room 1306 (but no cages of the neighboring rooms) had been infected with the viral pathogen. Based on this result, we immediately moved all mice housed in room 1306 to an external facility and once again disinfected room 1306 and restocked it with pathogen-free mice. Since then (last testing on 17 December 2006), no further cases of MHV reactivity have been detected in the 13th-Floor City.
Discussion
In 2000, we found that our rodent facilities at the University of Mainz were endemically contaminated with two viral and two parasitic infections. Since there had been no microbiological monitoring of newly imported mouse strains prior to organizational centralization, the contaminations most likely originated from imported mice. The open-top caging system in use at the time on the 13th-Floor Facility likely contributed to the rapid distribution of the four pathogens to all animal rooms.
The conventional strategy for decontamination of a facility is to completely depopulate it and then restock the area with SPF animals. However, this strategy would have required temporary closing of the housing area, causing severe problems for researchers at the university. We therefore opted to follow an alternative sanitization strategy characterized by the provisory subdivision of the 13th-Floor Facility into two distinct units that were then independently depopulated, sanitized, and restocked. Because we sanitized and reconstituted the two new units in succession, we were able to continuously use the facility for biomedical research throughout the process such that the total number of mice housed in the 13th-Floor City or 13th-Floor Clinic never dropped below 4,600 (Fig. 2).
Our alternative decontamination process was risky because it required that rederived and contaminated animals coexist in neighboring units for 15 months. The infection risk was further enhanced by the fact that it was not possible to completely separate the HVAC systems of the two newly established units or to establish adequate two-way personnel locks. Suboptimal personnel and HVAC barrier conditions have previously been shown to play a critical role in protection against pathogens13,14. However, our results show that it is possible to compensate for these suboptimal conditions and achieve success by using filter-top cages and servicing cages in cage-changing stations. Successfully decontaminating the mouse facility without shutting down research benefited the University of Mainz enormously because it significantly contributed to the consolidation of biomedical research. Still, the capital necessary for filter-tops (∼4,000), special filter-top cage lids (∼4,000), and cage-changing stations (6) totaled about 250,000 €, but represented a worthwhile investment into the laboratory animal facility.
Contaminated strains were successfully rederived by embryo transfer, underscoring the suitability of this method for resolving the problems of contaminated mouse strains15,16,17. Decontamination of the facility was supplemented by continuous oral application of ivermectin to all contaminated mice9. The aim of this antiparasitic treatment was not to eliminate the infections but to reduce the ova load in contaminated areas. Notice should be taken that mite ova are short-lived18, but pinworm ova are extremely long-lived and resistant to disinfection10, factors that can often lead to recontaminations.
The single case of recontamination that occured during the whole decontamination procedure involved MHV. Since this recontamination coincided with the time period in which the 13th-Floor City had already been restocked with mice but before the decontamination and restocking of the 13th-Floor Clinic, we presume that the recontamination with MHV was caused by cross-contamination between the units. This conclusion is further supported by the fact that all contaminated mice in the 13th-Floor Clinic were housed in open-top cages and handled openly during recontamination, strongly favoring the spread of airborne infections19. We have no satisfactory explanation for how the MHV infection may have infiltrated the filter-top protected cages in room 1306. Other sources of MHV infection, however, can be excluded with high probability because we had established a strict quarantine and microbiological control of newly imported strains and because there were no other MHV-contaminated facilities within the same building at the time that MHV re-emerged in room 1306.
Given the high infectivity and airborne infection routes of MHV and S. obvelata, as well as the high environmental resistance of MVM, high infection pressure, and barrier deficits present during the decontamination and restocking process, our observed frequency of recontamination must be considered extremely low. We are convinced that this low incidence of recontamination was the result of filter-top cages and cage-changing stations in the clean units. However, the general restrictions of non-controlled field studies make it impossible to support this conclusion with unequivocal statistical evidence.
References
Malakoff, D. The rise of the mouse, biomedicine's model mammal. Science 288(5464), 248–253 (2000).
Baker, D.G. Natural pathogens of laboratory mice, rats, and rabbits and their effects on research. Clin. Microbiol. Rev. 11(2), 231–266 (1998).
Yamamoto, H. et al. Microbiological contamination in genetically modified animals and proposals for a microbiological test standard for national universities in Japan. Exp. Anim. 50(5), 397–407 (2001).
Nicklas, W. et al. Recommendations for the health monitoring of rodent and rabbit colonies in breeding and experimental units. Lab. Anim. 36(1), 20–42 (2002).
Wescott, R.B., Malczewski, A. & Van Hoosier, G.L. The influence of filter top caging on the transmission of pinworm infections in mice. Lab. Anim. Sci. 26(5), 742–745 (1976).
Sedlacek, R.S. & Mason, K.A. A simple and inexpensive method for maintaining a defined flora mouse colony. Lab. Anim. Sci. 27(5Pt1), 667–670 (1977).
Dillehay, D.L., Lehner, N.D. & Huerkamp, M.J. The effectiveness of a microisolator cage system and sentinel mice for controlling and detecting MHV and Sendai virus infections. Lab. Anim. Sci. 40(4), 367–370 (1990).
Lipman, N.S., Corning, B.F. & Saifuddin, M. Evaluation of isolator caging systems for protection of mice against challenge with mouse hepatitis virus. Lab. Anim. 27(2), 134–140 (1993).
Klement, P., Augustine, J.M., Delaney, K.H., Klement, G. & Weitz, J.I. An oral ivermectin regimen that eradicates pinworms (Syphacia spp.) in laboratory rats and mice. Lab. Anim. Sci. 46(3), 286–290 (1996).
Pritchett, K.R. & Johnston, N.A. A review of treatments for the eradication of pinworm infections from laboratory rodent colonies. Contemp. Top. Lab. Anim. Sci. 41(2), 36–46 (2002).
Nagy, A., Gertsenstein, M., Vintersten, K. & Behringer, R. Manipulating the Mouse Embryo. A Laboratory Manual, 3rd Edn. (Cold Spring Harbor Laboratory Press, Cold Spring Harbor, NY, 2003).
Sebesteny, A., Milite, G. & Martelossi, P. Microbiologically monitored fumigation of a newly built SPF laboratory rodent facility. Lab. Anim. 26(2), 132–139 (1992).
Homberger, F.R. & Thomann, P.E. Transmission of murine viruses and mycoplasma in laboratory mouse colonies with respect to housing conditions. Lab. Anim. 28(2), 113–120 (1994).
Clough, G., Wallace, J., Gamble, M.R., Merryweather, E.R. & Bailey, E. A positive, individually ventilated caging system: a local barrier system to protect both animals and personnel. Lab. Anim. 29(2), 139–151 (1995).
Reetz, I.C., Wullenweber-Schmidt, M., Kraft, V. & Hedrich, H.J. Rederivation of inbred strains of mice by means of embryo transfer. Lab. Anim. Sci. 38(6), 696–701 (1988).
Morrell, J.M. Techniques of embryo transfer and facility decontamination used to improve the health and welfare of transgenic mice. Lab. Anim. 33(3), 201–206 (1999).
Van Keuren, M.L. & Saunders, T.L. Rederivation of transgenic and gene-targeted mice by embryo transfer. Transgenic Res. 13(4), 363–371 (2004).
Conole, J., Wilkinson, M.J. & McKellar, Q.A. Some observations on the pharmacological properties of ivermectin during treatment of a mite infestation in mice. Contemp. Top. Lab. Anim. Sci. 42(4), 42–45 (2003).
Shek, W.R., Pritchett K.R., Clifford, C.B. & White, W.J. Large-scale rodent production methods make vendor barrier rooms unlikely to have persistent low-prevalence parvoviral infections. Contemp. Top. Lab. Anim. Sci. 44(4), 37–42 (2005).
Acknowledgements
This work was supported by grants to K.R. (8312-38 62 61/527) and Ulrich Förstermann (8312-38 62 61/428) from the Stiftung Rheinland-Pfalz für Innovation. The authors appreciate the intensive support of Manfred Blessing, Ulrich Förstermann, and Matthias Reddehase, and the excellent work of the animal technicians of the Central Laboratory Animal Facility.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Wiese, E., Maurer, S., Steige, G. et al. Decontamination of a barrier facility using microisolator cages and provisional partitioning. Lab Anim 36, 31–35 (2007). https://doi.org/10.1038/laban0707-31
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/laban0707-31
This article is cited by
-
Partial phenotype conversion and differential trait response to conditions of husbandry in mice
Journal of Comparative Physiology B (2018)