Abstract
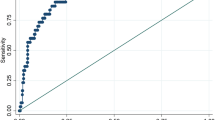
We aimed to evaluate the performance of blood pressure-to-height ratio (BPHR) and establish their optimal thresholds for elevated blood pressure (BP) among children aged 6 to 17 years in Chongqing, China. Data were collected from 11 029 children and adolescents aged 6–17 years in 12 schools in Chongqing according to multistage stratified cluster sampling method. The gold standard for elevated BP was defined as systolic blood pressure (SBP) and/or diastolic blood pressure (DBP) ⩾95th percentile for gender, age and height. The diagnostic performance of systolic BPHR (SBPHR) and diastolic BPHR (DBPHR) to screen for elevated BP was evaluated through receiver-operating characteristic curves (including the area under the curve (AUC) and its 95% confidence interval, sensitivity and specificity). The prevalence of elevated BP in children and adolescents in Chongqing was 10.36% by SBP and/or DBP ⩾95th percentile for gender, age and height. The optimal thresholds of SBPHR/DBPHR for identifying elevated BP were 0.86/0.58 for boys and 0.85/0.57 for girls among children aged 6 to 8 years, 0.81/0.53 for boys and 0.80/0.52 for girls among children aged 9 to 11 years and 0.71/0.45 for boys and 0.72/0.47 for girls among adolescents aged 12–17 years, respectively. Across gender and the specified age groups, AUC ranged from 0.82 to 0.88, sensitivity were above 0.94 and the specificities were over 0.7. The positive predictive values ranged from 0.30 to 0.38 and the negative predictive values were ⩾0.99. BPHR, with uniform values across broad age groups (6–8, 9–11 and 12–17 years) for boys and for girls is a simple indicator to screen elevated BP in children and adolescents in Chongqing.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Feber J, Ahmed M . Hypertension in children: new trends and challenges. Clin Sci (Lond) 2010; 119: 151–161.
McCrindlle BW . Assessment and management of hypertension in children and adolescents. Nat Rev Cardiol 2010; 7: 155–163.
Xi B, Liang Y, Mi J . Hypertension trends in Chinese children in the national surveys,1993 to 2009. Int J Cardiol 2013; 165: 577–579.
Lu Q, Ma CM, Yin FZ, Liu BW, Lou DH, Liu XL . How to simplify the diagnostic criteria of hypertension in adolescents. J Hum Hypertens 2011; 25: 159–163.
Lurbe E, Ingelfinger JR . Blood pressure in children and adolescents: current insights. J Hypertens 2016; 34: 178–183.
Chiolero A, Bovet P, Paradis G . Screening for elevated blood pressure in children and adolescents. JAMA Pediatr 2013; 167: 266–273.
Moyer VA . Screening for primary hypertension in children and adolescents: U.S. preventive services task force recommendation statement. Ann Intern Med 2013; 132: 613–619.
Hansen ML, Gunn PW, Kaelber DC . Underdiagnosis of hypertension in children and adolescents. JAMA 2007; 298: 874–879.
Lu Q, Ma C, Yin F, Wang R, Lou D, Liu X . Blood pressure-to-height ratio as a screening measure for identifying children with hypertension. Eur J Pediatr 2013; 172: 99–105.
Xi B, Zhang M, Zhang T, Liang Y, Li S, Steffen LM . Hypertension screening using blood pressure to height ratio. Pediatr 2014; 134: 106–111.
Guo X, Zheng L, Li Y, Zhang X, Yu S, Sun Y . Blood pressure to height ratio: a novel method for detecting hypertension in paediatric age groups. Paediatr Child Health 2013; 18: 65–69.
Mourato FA, Nadruz W Jr, Moser LR, de Lima Filho JL, Mattos SS . A modified blood pressure to height ratio improves accuracy for hypertension in childhood. Am J Hypertens 2015; 28: 409–413.
Kelishadi R, Bahreynian M, Heshmat R, Motlagh ME, Djalalinia S, Naji F et al. Accuracy of blood pressure-to-height ratio to define elevated blood pressure in children and adolescents: the CASPIAN-IV Study. Pediatr Cardiol 2016; 37: 378–385.
Ahmed A, Ali SW, Massodi S, Bhat MA . Blood pressure-to-height ratio as a screening tool for hypertension in children. Indian Pediatr 2016; 53: 137–139.
Outdili Z, Marti-Soler H, Simonetti GD, Bovet P, Paccaud F, Burnier M et al. Performance of blood pressure-to-height ratio at a single screening visit for the identification of hypertension in children. J Hypertens 2014; 32: 1068–1074.
Xi B, Zhang M, Zhang T, Li S, Steffen LM . Simplification of childhood hypertension definition using blood pressure to height ratio among US youths aged 8–17 years, NHANES 1999–2012. Int J Cardiol 2015; 180: 210–213.
Cao XY, Cao XH, Dou YR, Zhang YN, Pu KY . Comparison of the urban and rural students’ physique of Chongqing in 2008. Chin J Sch Health 2009; 30: 769–770.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Pediatrics 2004; 114: 555–576.
Zou KH, O’Malley AJ, Mauri L . Receiver-operating characteristic analysis for evaluating diagnostic tests and predictive models. Circulation 2007; 115: 654–657.
Youngstrom EA . A primer on receiver operating characteristic analysis and diagnostic efficiency statistics for pediatric psychology: we are ready to ROC. J Pediatr Psychol 2014; 39: 204–221.
Xu Y . Report of the Chinese National Survey on Students’ Constitution and Health in 2010. Chin J Sch Health 2011; 32: 1025–1026.
Liang JJ, Chen YJ, Jin Y, Yang WH, Mai JC, Ma J et al. Comparison of adiposity measures in the identification of children with elevated blood pressure in Guangzhou, China. J Hum Hypertens 2015; 29: 732–736.
Yin X, Liu Q, Bovet P, Ma C, Xi B . Performance of blood pressure-to-height ratio as a screening tool for elevated blood pressure in pediatric population: a systematic meta-analysis. J Hum Hypertens 2016; 30: 697–702.
Halligan S, Altman DG, Mallett S . Disadvantages of using the area under the receiver operating characteristic curve to assess imaging tests: a discussion and proposal for an alternative approach. Eur Radiol 2015; 25: 932–939.
Ma C, Kelishadi R, Hong YM, Bovet P, Khadilkar A, Nawarycz T et al. Performance of eleven simplified methods for the identification of elevated blood pressure in children and adolescents. Hypertension 2016; 68: 614–620.
Xi B, Zong X, Kelishadi R, Hong YM, Khadilkar A, Steffen LM et al. Establishing international blood pressure references among nonoverweight children and adolescents aged 6 to 17 Years. Circulation 2016; 133: 398–408.
Acknowledgements
We are grateful to the Institute of Child and Adolescent Health, School of Public Health, Peking University for giving us chance to participate in the study. We are also grateful to the school leaders, teachers and students of 12 schools who actively cooperated with the investigations. We are particularly grateful to Professor Rahul Malhotra (from Health Services and Systems Research Head of Research, Center for Ageing Research and Education, Duke-NUS Medical School) for revising the manuscript. This study was supported by the Research Special Fund for Public Welfare Industry of Health (No. 201202010). The study was approved by Biomedical Ethics Committee of Peking University and Medical Research Ethics Committee of Chongqing Medical University. All subjects gave informed consent.
Author contributions
HW conceived and designed the study. HW, LYW, QL, XTC and JJJ participated in the field studies and data collection. LYW and HW analyzed the data and drafted the manuscript. QL and RM revised the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Journal of Human Hypertension website
Supplementary information
Rights and permissions
About this article
Cite this article
Wang, L., Liu, Q., Cheng, X. et al. Blood pressure-to-height ratio as a screening indicator of elevated blood pressure among children and adolescents in Chongqing, China. J Hum Hypertens 31, 438–443 (2017). https://doi.org/10.1038/jhh.2016.89
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2016.89
This article is cited by
-
Trends and Status of the Prevalence of Elevated Blood Pressure in Children and Adolescents in China: a Systematic Review and Meta-analysis
Current Hypertension Reports (2019)