Abstract
For patients with hypertension, an individual risk prediction tool for cardiovascular disease based on on-treatment blood pressure is needed and would be useful. The objective of this study was to establish a 3-year risk prediction model for cardiovascular disease based on data from 13 052 patients with no history of cardiovascular disease in the Olmesartan Mega study to determine the relationship between Cardiovascular Endpoints and Blood Pressure Goal Achievement study. To develop dynamic prediction models including on-treatment blood pressure, a Cox proportional hazard model using the sliding landmarking method with three landmark points (6, 12 and 18 months from baseline) was used. The prediction model included blood pressure (<130/85 mm Hg, ⩾130/85 to <140/90 mm Hg, ⩾140/90 to <160/100 mm Hg and ⩾160/100 mm Hg) as a time-dependent covariate and well-known baseline risk factors (sex, age, smoking, family history of coronary artery disease and diabetes) as covariates. The 3-year risk assessment chart was constructed using the combination of all risk factors in the prediction model, and six different colors were displayed on each chart corresponding to the predicted probability of cardiovascular disease. Judging from the chart, if an elderly man with diabetes and other risk factors had a blood pressure of <130/85 mm Hg at 6 months, the risk of cardiovascular disease would be 8.0%, whereas the risk would be 8.6% if he had a blood pressure of ⩾130/85 to <140/90 mm Hg. The risk assessment chart developed from the large-scale observational study data would help physicians to more easily assess the cardiovascular disease risk for hypertensive patients on antihypertensive treatments.
Similar content being viewed by others
Introduction
The identification of risk factors for future cardiovascular disease (CVD) and the development of risk prediction models are objectives of medical research. In clinical practice, the assessment of absolute risk in individual patients is important for determining treatment decisions, and a simplified tool to assess individual absolute risk (ie, risk assessment chart) would be useful. Some risk assessment charts using baseline risk factors and laboratory data from the general population have been proposed.1, 2 The number of hypertensive patients is approximately 40 million in Japan,3 which makes it the largest population being treated in clinical practice. Therefore, an absolute risk assessment chart designed specifically for hypertensive patients would be widely useful and clinically beneficial. Conventional risk assessment charts aid in quantifying future (long term) CVD risk in the general population; however, these tools might not be appropriate for assessing risk and improving adherence to treatment in patients undergoing treatment. The risk assessment of patients on antihypertensive treatment should be based on their on-treatment blood pressure (BP). For patients to actually obtain the benefits of maintaining good BP control, the assessment of short-term risk, rather than long-term risk, might be more effective initially.
Using data from the Olmesartan Mega study to determine the relationship between Cardiovascular Endpoints and Blood pressure Goal Achievement (OMEGA) study,4 a post-marketing study for the angiotensin receptor blocker olmesartan, we previously evaluated the association between achieved BP and CVD with the aim of identifying baseline risk factors.5 In this analysis, we developed a risk prediction model for CVD using baseline risk factors and the BP reported during the study. At present, few absolute risk assessment charts for hypertensive patients have been developed, and no chart using on-treatment BP is available. We consider that our risk assessment chart would aid in instructing patients who have started medical treatment and in improving their adherence to treatment.
Methods
Study design
The OMEGA study was initiated in July 2005 as a post-marketing surveillance study by Sankyo (presently Daiichi Sankyo, Tokyo, Japan) in compliance with the regulations of the Japanese Ministry of Health, Labour and Welfare. The study protocol was approved by the Ethical Committee of Sankyo. The protocol conformed to the pharmaceutical affairs laws of Japan, and it was approved by the Ministry of Health, Labour and Welfare of Japan before commencement. This study conformed to the Declaration of Helsinki and was carried out at registered medical institutions according to Good Post-marketing Study Practice in Japan. Details of the study design and the baseline clinical characteristics of the patients have been reported previously.4 In summary, eligible patients were male or female outpatients aged 50–79 years with physician-diagnosed hypertension who had not been treated with olmesartan. Exclusion criteria were a history of myocardial infarction, stroke, coronary artery bypass grafting or percutaneous coronary intervention within 6 months before enrollment, as well as scheduled coronary intervention, congenital or rheumatic heart disease, severe arrhythmia, severe hepatic or renal disease, cancer that was under treatment and pregnancy or the potential to become pregnant. Each patient was informed of the purpose and methods of the study, as well as their right to withdraw from the study at any time and the measures taken for confidentiality. After providing written informed consent and being prescribed olmesartan (typically 10 or 20 mg per day) at the physician’s discretion, the patients were enrolled in an electronic data capturing system.
Study patients
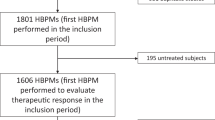
Between July 2005 and March 2007, 15 313 patients from 2219 facilities were registered in the OMEGA study, and data were collected from 15 255 of those patients. Out of the 15 255 patients, 14 721 were enrolled in the analysis data set and 534 who failed to meet the eligibility criteria, had missing data or withdrew their consent to participate were excluded. To consider primary prevention, 13 052 patients with no history of CVD from the analysis data set of the OMEGA study were included in this analysis.
End points
The end points were stroke (cerebral infarction, cerebral hemorrhage and subarachnoid hemorrhage), coronary heart disease (myocardial infarction and angina pectoris requiring cardiovascular intervention or hospitalization) and sudden death. CVD was defined as a composite of these three end points. The diagnostic criteria for the various end points were described in detail previously.4, 5
Statistical analysis
The outcome considered in this analysis was CVD. The Cox proportional hazard model was used to establish the 3-year risk prediction model for CVD. To develop dynamic prediction models with on-treatment BP levels, the sliding landmarking method with three landmark time points (6, 12 and 18 months from baseline) was used. The prediction models included on-treatment BP levels (<130/85 mm Hg, ⩾130/85 to <140/90 mm Hg, ⩾140/90 to <160/100 mm Hg and ⩾160/100 mm Hg) at each time point and baseline risk factors as covariates. We selected the baseline risk factors from the CV risk factors defined in JSH2014 (ie, smoking, dyslipidemia, obesity (body mass index >25), metabolic syndrome, family history of coronary artery disease and diabetes) using a backward elimination method with a criterion of P<0.05 for retention, while including sex and age in the model. BP values after 6 months were imputed using the last observation carried forward method, and patients with missing covariate values were excluded from the development of prediction models. The performance of each prediction model was evaluated in terms of both discrimination and calibration. Harrell's c-index for the time-to-event data and its 95% bootstrap confidence interval based on 1000 resamplings were estimated as a discrimination measure, and the Hosmer–Lemeshow χ2-tests with nine degrees of freedom for the time-to-event data were conducted as a calibration measure.6, 7, 8 As an internal validation of the prediction models, the c-index corrected for its optimism was estimated by repeating the model evaluation process with the bootstrapping method.9 The 3-year risk assessment chart was constructed by the combination of all risk factors in the prediction model, and six different colors were displayed on each chart corresponding to the predicted probability of CVD. All statistical analyses were conducted using SAS release 9.2 (SAS Institute, Cary, NC, USA). All P-values are two-sided, and values under 5% were considered statistically significant.
Results
Study profile and baseline characteristics
The baseline characteristics of the 13 052 patients are shown in Table 1. Women accounted for 50.6% of the patients. The mean age was 64.5±8.2 years, the mean body mass index was 24.8±3.6 kg m−2, and the mean baseline systolic BP and diastolic BP were 158.1±17.7 and 89.4±12.1 mm Hg, respectively. The mean follow-up period was 2.7 years.
Antihypertensive treatment and blood pressure change
The mean daily dose of olmesartan at baseline and after 36 months was 17.2±5.5 mg (5 mg in 1.2%, 10 mg in 29.0%, 20 mg in 68.2% and 40 mg in 1.6%) and 17.2±8.5 mg (0 mg in 8.9%, 5 mg in 1.5%, 10 mg in 18.6%, 20 mg in 65.1% and 40 mg in 5.8%), respectively. The mean duration of dosing was 925.9±392.1 days. The number of patients receiving treatment with antihypertensive drugs other than olmesartan was 4785 (36.7%) at the start of olmesartan treatment and 3549 (55.1%) after 36 months. The mean BP (systolic BP/diastolic BP) was 158.1/89.4 mm Hg at baseline and 137.5/79.1 mm Hg after 6 months of administration, 136.9/78.5 mm Hg after 12 months, 135.8/77.7 mm Hg after 18 months and 134.1/76.3 mm Hg after 36 months.
CVD events and the incidence of CVD
The number of events during the follow-up period and the incidence of events per 1000 person-years are shown in Table 2. CVD occurred in 195 out of the 13 052 patients, with an incidence of 5.58/1000 person-years. The CVD events were stroke in 96 patients (2.74/1000 person-years), coronary heart disease in 94 patients (2.68/1000 person-years) and sudden death in 10 patients (0.28/1000 person-years).
Prediction models and risk assessment charts
The details of our prediction models are shown in Table 3A. When the landmark time point was set at 6 months, the significant factors were sex, age, smoking, family history of coronary artery disease and diabetes. Of these factors, the hazard ratio (HR) for diabetes was the highest (HR: 2.15, 95% CI: 1.53–3.03). All of the prediction models (6-, 12- and 18-month models) that include these factors showed moderate discriminative ability (c-index=0.683, (95% CI: 0.648–0.738), 0.654 (95% CI:0.618–0.723) and 0.679 (95% CI: 0.644–0.749)) and good calibration ability (χ2=7.61 (P=0.574), 9.68 (P=0.377) and 6.19 (P=0.721)), respectively (Table 3B). The internally validated c-index corrected for its optimism was not very different from the apparent performance (c-index=0.664, 0.623 and 0.636, respectively).
The 3-year risk assessment chart was constructed as shown in Figures 1, 2, 3. The figures in each cell on each chart represent the predictive probability of CVD during the last period (from each landmark time to 3 years). Six different colors are displayed, one each corresponding to a specific predicted probability (<1%, ⩾1 to <2%, ⩾2 to <3%, ⩾3 to <5%, ⩾5 to <10% and ⩾10%). As shown in Figure 1, if an elderly patient with diabetes and two other baseline risk factors (smoking and a family history of coronary artery disease) had no experience of CVD and had BP of ⩾130/85 and <140/90 mm Hg at 6 months, the predictive probability of CVD within the last 2.5 years would be 8.6% in men and 6.0% in women. However, for a diabetic patient who had the same profile as the above-mentioned patient, but had achieved BP of under 130/80 mm Hg at 6 months, the predictive probability of CVD within the last 2.5 years would be as low as 8.0% in men and 5.5% in women, indicating a lower probability than for those who had not achieved a lower BP in a diabetic population.
Discussion
Because hypertension has been reported as a risk factor for future strokes,2, 10 BP control is important to prevent those events. However, the percentage of hypertensive patients achieving the target BP level is low, and according to the report of the Japan Guideline Assessment Panel-2, only approximately 50% of patients receiving antihypertensive treatment achieve the target BP level defined by JSH2014.11, 12 A possible reason for the low target BP achievement is low patient adherence to antihypertensive treatment.13 Therefore, in daily clinical practice, it is important for physicians to make patients understand their own risk and to motivate patients to adhere to the treatment. The quantitative measure for each patient’s risk is useful in such patient education.
Recently, the assessment of absolute risk in hypertensive patients has been given important consideration, and this risk is increasingly taken into account in the treatment approach; however, few reports have discussed methods to systematically assess the absolute risk. As previously stated, conventional risk assessment charts designed for use in the general population1, 2 are considered beneficial for individuals who are preparing to start antihypertensive treatment, but these charts might not be appropriate for patients who have already been on antihypertensive treatment, in terms of raising their awareness of risk reduction by the treatment.
Against this background, the practice guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology published in 201314 have proposed a chart assessing the absolute risk in hypertensive patients on the basis of baseline BP and risk factors. This chart is considered useful for the physician’s decision-making process for treatment and for instructing patients to improve their attitudes toward treatment. However, the use of only baseline BP in assessing absolute risk might not be sufficient because BP values in hypertensive patients can fluctuate after receiving antihypertensive treatment. Therefore, we consider that risk assessment using on-treatment BP is needed to improve patient motivation and adherence by helping patients to visualize the benefits of risk reduction. Another study has suggested that self-measured pulse pressure might also be a useful predictor of cardiovascular risk, independent of mean BP, in elderly patients.15 Although we did not measure pulse pressure in the present study, it might be worth considering in future studies.
In the present analysis, we developed a dynamic prediction model and produced an absolute risk assessment chart that enables assessment of changes in absolute risk during the follow-up period. In the practical application, physicians could show this chart to their patients who are preparing to start antihypertensive treatment to help the patients understand the absolute risk after 6 months according to the degree of antihypertensive effects. After treatment is initiated, the absolute risk is to be assessed every 6 months with the risk assessment chart, to maintain patient understanding of the importance of continuous treatment. By applying the chart in this way, patients can have a grasp of their own risk, and we believe that awareness of the importance of continuous therapy would further improve patient adherence.
By using the risk assessment chart, the effects of risk factors other than BP could be considered. Using diabetes as an example, as shown in the rightmost column of Figure 1, the absolute risk for the male diabetic patients with three baseline risk factors (age ⩾65 years, smoking and family history of coronary artery disease) is higher than that of the male non-diabetic patient even if the patients achieve a BP of under 130/85 mm Hg at 6 months (8.0–13.7% for diabetic patients, 3.8–6.6% for non-diabetic patients, respectively). This result suggests that a lower target BP is preferable for diabetic patients, and this finding is consistent with the target BP defined in JSH2014 (ie, <140/90 mm Hg for non-diabetic patients, <130/80 mm Hg for diabetic patients).10 The effect of smoking could also be assessed. As also shown in the rightmost column of Figure 1, the absolute risk for male smokers with three baseline risk factors (age ⩾65 years, diabetes and family history of coronary artery disease) and BP of under 130/85 mm Hg at 6 months is nearly the same as the risk for non-smokers with the same baseline risk factors and BP of above 160/100 mm Hg at 6 months (8.0% for smokers, 8.1% for non-smokers, respectively). This result might indicate that quitting smoking has the same level of effect on CVD prevention as BP lowering. We also conducted an analysis using a different category for age (ie, <65, ⩾65 to <75 and ⩾75 years) to investigate the effect of age. However, the results were rarely different (data not shown), which could be partly because there were no patients aged more than 80 years in the OMEGA study.
This study has some limitations and requires further consideration. First, we assessed the absolute risk during a period of 3 years because the median follow-up period of the study was approximately 3 years. Compared with that of other risk assessment charts, 3 years is a relatively short period. However, we consider that the prediction of events in a short-term period is also important in the actual patient population. A second limitation is the relevance of the risk factors included in the analysis. In the present analysis, the risk factors were selected using a statistical method to prepare a simple and easy-to-use assessment tool, and only BP was selected as a time-dependent risk factor because there were not sufficient longitudinal data for other risk factors that were not scheduled in the study protocol. Other factors such as body mass index, metabolic syndrome and dyslipidemia that were excluded from this analysis are also important. Regarding dyslipidemia, in a previous article related to the OMEGA study, we have reported that complications of dyslipidemia at baseline are not a risk factor for CVD and stroke but are a risk factor for coronary heart disease and that statin use has a preventive effect;16 however, this finding is based on information at baseline, and the relationship between dyslipidemia and statin use during the follow-up period remains unclear. In another article, we have reported that increased lipid levels during follow-up are associated with increased CVD risk, even in hypertensive patients.17 Therefore, we believe that it is important to consider complications of dyslipidemia and the role of statin use in terms of prevention of CVD events. Nevertheless, the predictive ability of each factor should be examined when developing a prediction model. The addition of those factors into the present model showed no marked improvement in the predictive ability. When the models were assessed on the basis of the information criteria for predictive modeling (ie, Akaike's information criterion), the results showed that the value of Akaike's information criterion of the selected model was smaller than that of the full model (2414.646 vs 2420.583), suggesting the better quality of the selected model. Therefore, we consider that the risk factors selected for the model are appropriate in terms of the prediction of CVD events. A third limitation is the generalizability of the charts. The present analysis used the data of patients undergoing olmesartan-based treatment, who are considered to be representative of those receiving antihypertensive treatment with an angiotensin receptor blocker, and therefore, our model could be used to quantify risk in this population to some degree. However, external validation is needed to verify our model in a more general hypertensive population.
The dynamic prediction model and risk assessment chart developed from the large-scale observational study data would help physicians to more easily assess the CVD risk for hypertensive patients on angiotensin receptor blocker-based antihypertensive treatment.
References
NIPPON DATA 80 Research Group. Risk assessment chart for death from cardiovascular disease based on a 19-year follow-up study of a Japanese representative population - NIPPON DATA 80. Circ J 2006; 70: 1249–1255.
Ishikawa S, Matsumoto M, Kayaba K, Gotoh T, Nago N, Tsutsumi A, Kajii E, Jichi Medical School (JMS) Cohort Study Group. Risk charts illustrating the 10-year risk of stroke among residents of Japanese rural communities: The JMS Cohort Study. J Epidemiol 2009; 19: 101–106.
The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res 2014; 37: 253–392.
Teramoto T, Fujita T, Kawamori R, Miyazaki S, Teramukai S, Igarashi M . OMEGA study: design, baseline data, metabolic syndrome prevalence in a large-scale observational study of hypertensive patients: The Olmesartan Mega Study to Determine the Relationship between Cardiovascular Endpoints and Blood Pressure Goal Achievement Study. Hypertens Res 2008; 31: 2011–2017.
Teramoto T, Kawamori R, Miyazaki S, Teramukai S, Shirayama M, Hiramatsu K, Kobayashi F . OMEGA Study Group. Relationship between achieved blood pressure, dietary habits and cardiovascular disease in hypertensive patients treated with olmesartan: the OMEGA study. Hypertens Res 2012; 35: 1136–1144.
Harrell FE Jr, Lee KL, Mark DB . Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 1996; 15: 361–387.
Pencina MJ, D’Agostino RB . Overall C as a measure of discrimination in survival analysis: model specific population value and confidence interval estimation. Stat Med 2004; 23: 2109–2123.
D’Agostino RB, Nam BH . Handbook of Statistics. Elsevier: Amsterdam. 2004, 1–25.
Steyerberg EW, Harrell FE Jr, Borsboom GJ, Eijkemans MJ, Vergouwe Y, Habbema JD . Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol 2001; 54: 774–781.
Yatsuya S, Iso H, Yamagishi K, Kokubo Y, Saito I, Suzuki K, Sawada N, Inoue M, Tsugane S . Development of a point-based prediction model for the incidence of total stroke: Japan public health center study. Stroke 2013; 44: 1295–1302.
Teramoto T, Fujita T . Present state and question of lifestyle diseases and pharmacological treatment in Japan – Japan Guideline Assessment Panel-2 (J-GAP2). Prog Med 2010; 30: 1437–1449.
Balijepalli C, Bramlage P, Lösch C, Zemmrich C, Humphries KH, Moebus S . Prevalence and control of high blood pressure in primary care: results from the German Metabolic and Cardiovascular Risk Study (GEMCAS). Hypertens Res 2014; 37: 580–584.
Matsumura K, Arima H, Tominaga M, Ohtsubo T, Sasaguri T, Fujii K, Fukuhara M, Uezono K, Morinaga Y, Ohta Y, Otonari T, Kawasaki J, Kato I, Tsuchihashi T . Comfort Investigators. Impact of antihypertensive medication adherence on blood pressure control in hypertension: the COMFORT study. QJM 2013; 106: 909–914.
ESH/ESC Task Force for the Management of Arterial Hypertension. 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens 2013; 31: 1925–1938.
Aparicio LS, Thijs L, Asayama K, Barochiner J, Boggia J, Gu YM, Cuffaro PE, Liu YP, Niiranen TJ, Ohkubo T, Johansson JK, Kikuya M, Hozawa A, Tsuji I, Imai Y, Sandoya E, Stergiou GS, Waisman GD, Staessen JA . International Database on Home blood pressure in relation to Cardiovascular Outcome (IDHOCO) Investigators. Reference frame for home pulse pressure based on cardiovascular risk in 6470 subjects from 5 populations. Hypertens Res 2014; 37: 672–678.
Teramoto T, Kawamori R, Miyazaki S, Teramukai S, Mori Y, Okuda Y, Hiramatsu K, OMEGA Study Group. Risk factors for primary prevention of cardiovascular disease and risk reduction by lipid control: the OMEGA study risk factor sub-analysis. Clin Exp Hypertens 2014; 36: 236–243.
Teramoto T, Kawamori R, Miyazaki S, Teramukai S, Sato Y, Okuda Y, Shirayama M . Lipid and blood pressure control for the prevention of cardiovascular disease in hypertensive patients: a subanalysis of the OMEGA study. J Atheroscler Thromb 2015; 22: 62–75.
Acknowledgements
We are grateful to the patients, physicians and medical staff who participated in the OMEGA study and thank their co-workers for their support of the OMEGA study. We also thank Prof. Ikuo Saito for his valuable comments on this paper. The OMEGA study was sponsored by Daiichi (Tokyo, Japan). The study was registered at http://www.clinicaltrials.jp/ with the unique trial number JapicCTI-050002.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The OMEGA study was sponsored by Daiichi Sankyo (Tokyo, Japan). ST has received a consulting fee from Daiichi Sankyo. TT has received research funds from Daiichi Sankyo. YO and MS are employees of Daiichi Sankyo. The remaining authors declare no conflicts of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Teramukai, S., Okuda, Y., Miyazaki, S. et al. Dynamic prediction model and risk assessment chart for cardiovascular disease based on on-treatment blood pressure and baseline risk factors. Hypertens Res 39, 113–118 (2016). https://doi.org/10.1038/hr.2015.120
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.120
Keywords
This article is cited by
-
The validity of electronic health data for measuring smoking status: a systematic review and meta-analysis
BMC Medical Informatics and Decision Making (2024)
-
Dynamic prediction for clinically relevant pancreatic fistula: a novel prediction model for laparoscopic pancreaticoduodenectomy
BMC Surgery (2021)
-
The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019)
Hypertension Research (2019)
-
Sex differences and the prognosis of depressive and nondepressive patients with cardiovascular risk factors: the Japan Morning Surge–Home Blood Pressure (J-HOP) study
Hypertension Research (2018)
-
An interesting cross-talk between the glucagon-like peptide-1 receptor axis and angiotensin receptor pathway for modulation of renal sodium handling in obesity
Hypertension Research (2018)