Abstract
Previous studies have shown that renin–angiotensin (Ang) system vaccines may be effective for the treatment of hypertension, but their efficacy for the prevention of renal disease is unclear. The aim of this study was to compare the effects of an Ang II type 1 (AT1) receptor vaccine with an Ang II receptor blocker (ARB) and a vasodilator on blood pressure (BP) and renal injury in the L-NAME nephropathy model. Male spontaneously hypertensive rats (SHRs) were divided into six groups and treated transiently with three injections of vehicle or AT1 receptor vaccine (0.1 mg) at age 4, 6 and 8 weeks, or continuously with candesartan cilexetil (0.1 mg kg−1 per day) or hydralazine hydrochloride (5 mg kg−1 per day), then administered NG-nitro-L-arginine methyl ester (L-NAME) from age 18 to 21 weeks to induce renal injury. Vaccination against the AT1 receptor caused a significant increase in AT1 receptor titers, and a sustained decrease in BP. L-NAME treatment resulted in a marked increase in proteinuria in the control groups, which was completely suppressed in the AT1 vaccine-treated group, and glomerular injury scores were also significantly decreased. Real-time RT-PCR and immunofluorescence studies revealed increased renin mRNA, and increased glomerular expression of nephrin. Comparable results were seen in rats treated continuously with the ARB candesartan, but not with hydralazine. These results suggest that transient AT1 vaccination is as effective as continuous treatment with ARB, not only for the attenuation of hypertension, but also for the prevention of L-NAME-induced nephropathy in SHR.
Similar content being viewed by others
Introduction
The renin–angiotensin (Ang) system (RAS) has a central role in the control of systemic blood pressure (BP). It is also known to have an important role in the pathogenesis of hypertensive renal injury, which is one of the leading causes of chronic kidney disease throughout the world.1 Analysis of the epidemiological data from dialysis registries has shown that the incidence of end-stage renal disease due to hypertensive nephrosclerosis is progressively increasing in Japan and other countries,2, 3 therefore new strategies for prevention and treatment of hypertensive renal disease are urgently required.
Previous studies have shown that the use of RAS inhibitors, such as Ang-converting enzyme inhibitors and Ang receptor blockers (ARBs), are effective for inhibiting the progression of established renal disease.4, 5 Recent studies have suggested that the use of RAS inhibitors may also be effective in preventing new-onset of chronic kidney disease, particularly in patients with diabetes.6, 7 These results suggest the possibility that early inhibition of the RAS may be an effective strategy for prevention of chronic kidney disease. However, despite the increasing availability of different types of RAS inhibitors for over 20 years, the number of patients with chronic kidney disease is still increasing throughout the world, which suggests that other, non-pharmacological approaches may be required. One potential candidate is vaccination, which has recently been shown in a phase IIa study to be safe and effective for the treatment of essential hypertension.8
Immunotherapy against the RAS was first attempted in humans 1951.9 Further studies showed that anti-renin vaccines caused a significant and sustained decrease in BP, but could also induce autoimmune renal disease in animal models.10 A vaccine against Ang I was tested in a phase IIa clinical trial, and was found to be safe, but did not effectively cause a decrease in BP in patients with essential hypertension.11 In contrast, the study by Tissot et al.8 using a vaccine against Ang II showed a small, but significant, decrease in both systolic and diastolic BP in patients with mild-to-moderate hypertension. Furthermore, Zhu et al.12 reported that a vaccine against the Ang II type 1 (AT1) receptor was effective in reducing BP in rats.
These results suggest that vaccination against the RAS may be an effective future strategy for the treatment of hypertension. At present, the efficacy of RAS vaccination for the prevention of renal disease is unclear. The aim of this study was therefore to examine the efficacy of vaccination against the AT1 receptor in preventing nephropathy in the spontaneously hypertensive rat (SHR)/NG-nitro-L-arginine methyl ester (L-NAME) model of hypertensive nephrosclerosis, and the mechanism of these effects.
Methods
AT1 receptor vaccine preparation
The seven-amino-acid peptide sequence corresponding to amino acids 181–187 in the second extracellular loop of rat AT1a receptor (AFHYESR),12 was synthesized by Medical & Biological Laboratories. (Aichi, Japan). The carrier protein used in this study was Keyhole Limpet Haemocyanin (KLH). Coupling of the peptide to the carrier protein was performed using the crosslinker m-maleimidobenzoyl-N-hydroxysuccinimide ester method. 100 μl of the conjugate containing 0.1 mg peptide were used as a dose for immunization of each animal.
Animal treatment protocols
Studies were performed on male SHRs aged 3 weeks, which were obtained from Charles River Laboratories Japan (Kanagawa, Japan). Candesartan cilexetil (TCV-116) was a kind gift from Takeda Pharmaceutical (Osaka, Japan). All animals were cared for in accordance with the Animal Experimentation Guidelines of the Keio University School of Medicine.
Protocol 1: Preliminary studies for antibody titer measurement and antihypertensive drug dose determination
For the preliminary studies, SHRs were divided into six groups (n=6 per group). Rats in groups P1–P4 were treated with 0, 1, 3 or 6 injections of 0.1 ml KLH-conjugated AT1 receptor peptide (peptide content 0.1 mg) coupled with the same volume Freund’s adjuvant every 2 weeks from age 4 weeks. Rats in groups P5 and P6 were treated with hydralazine hydrochloride (5 mg kg−1 per day in drinking water) or candesartan cilexetil (0.1 mg kg−1 per day in drinking water) from age 4 weeks until the end of the study. BP measurements were used to confirm that these doses of hydralazine and candesartan produced similar reductions in BPs as the AT1 vaccine-treated rats. Blood samples were obtained from the left ventricle under anesthesia for enzyme-linked immunosorbent assay analysis. BPs were measured every week from age 4 weeks by tail-cuff measurement, and confirmed by telemetry at age 18 weeks.
Protocol 2: Assessment of prevention of renal injury by AT1 vaccination
SHRs were randomly divided into six groups as follows (n=5–10 per group): SHRs in groups 1 and 2 were control SHRs. SHRs in group 3 and 4 were injected with KLH vehicle alone or AT1 receptor vaccine at 4, 6 and 8 weeks of age. SHRs in group 5 and 6 were orally administered hydralazine or candesartan as in protocol 1. In all 10 weeks after the final vaccination, groups 2–6 were administered the nitric oxide synthase inhibitor, NG-nitro-L-arginine methyl ester (L-NAME, 100 mg l−1) in drinking water from 18 to 21 weeks of age to induce proteinuria and renal injury, as reported by us previously.13 The animals were euthanized at 21 weeks of age for examination of renal, cardiac and aortic histology by light microscopy.
Protocol 3: Long-term observation of the effects of AT1 vaccination
Male SHRs were randomly divided into two groups (n=12). Rats in AT1 vaccine group were injected with AT1 vaccine at 4, 6 and 8 weeks of age. Indirect systolic blood pressure (SBP) was monitored once every 2 weeks. Blood samples were obtained periodically from the left ventricle for the measurement of antibody titers until age 1 year.
BP measurement and biochemical studies
Indirect SBP was monitored by a standard tail-cuff technique using a Natsume KN-210 manometer (Natsume, Tokyo, Japan). In some experiments, arterial BPs were measured by telemetry using the TA11PA-C40 telemetric transducer (Data Sciences International, St Paul, Minnesota), as recommended by the manufacturer. Measurements were performed during a 2-h period (from 0900 hours to 1100 hours), and the results were the average values of these measurements. In some experiments, the 2 h measurements were performed in the evening (from 2100 hours to 2300 hours). A total of 24 h urine collection was performed weekly in metabolic cages from 18 to 21 weeks of age. Urinary protein concentrations and serum chemistries were determined as reported previously.13 Plasma immunoreactive aldosterone concentration was determined by radioimmunoassay using a commercial kit (TFB, Tokyo, Japan). Cross-reactivity of the antibodies with corticosterone was <0.03%.
Determination of antibody titers by enzyme-linked immunosorbent assay
Ninety-six-well microtiter plates were coated overnight at 4 °C with 0.1 μg per well vaccine peptide in PBS. Sera from rats were diluted over a range from 100- to 62 500-fold in PBS buffer, and added to each well. After the incubation for 60 min at room temperature, the plate was rinsed with PBS buffer. Goat anti-rat IgG (whole molecule)—peroxidase antibody was added to each well. The color generated following reaction between the peroxidase and TMB substrate was determined using a Model 550 plate reader. The titer end-point was defined as the titer, which gave an absorbance value less than twice that of the negative control.12
Histological studies
The kidneys, hearts and thoracic aortas from animals were weighed, then fixed in 4% paraformaldehyde, and embedded in paraffin blocks. Histological sections were stained and scored as described previously.14, 15
Immunofluorescence staining
Immunofluorescence staining of nephrin and podocin expression were performed on the cryostat sections of kidneys using polyclonal anti-nephrin (Progen Biotechnik GmbH, Heidelberg, Germany, 1:50) and anti-podocin antibodies (Immuno-Biological Laboratories. Gunma, Japan, 1:50).14, 15
Quantitation of renal RAS mRNAs by real-time reverse transcription (RT) PCR
Total RNAs were extracted from the kidneys, and analyzed by real-time RT-PCR.13
Determination of response to Ang II in vivo
In order to assess the response to administration of Ang II in vivo, the BPs of rats at age 18 weeks were monitored by telemetry before and immediately after a bolus i.v. injection of Ang II (10 μg kg−1) via the tail vein.
Determination of response to Ang II in vitro
The response to Ang II in vitro was assessed using rat aortic vascular smooth muscle cells (VSMCs). IgG were affinity-purified from sera of 14-week-old AT1 vaccinated rats using the Melon Gel IgG Spin Purification Kit (Thermo Fisher Scientific, Surrey, UK) according to the manufacturer's protocol. IgG purified from AT1 vaccinated rats were added to serum-starved VSMC (at 1:200 dilution) for 1 h at 37 °C. Next, VSMCs were stimulated with or without Ang II (10 nmol l−1) for 5 min, and phosphorylation of ERK1/2 was analyzed by western blot analysis.
Statistical analysis
Results were expressed as the mean±s.e.m. Statistical comparisons were made by ANOVA. P-values <0.05 were considered to be statistically significant.
Results
Preliminary studies
In the preliminary studies (protocol 1), the effects of 0, 1, 3 and 6 injections of AT1 vaccine on AT1 receptor antibody titers were examined at age 6, 10, 14 and 21 weeks. In the P4 group, antibody titer measurements were performed at age 14 weeks after the final injection of AT1 vaccine. As shown in Table 1, a single injection of the AT1 vaccine caused increased antibody titers but these levels were significantly lower than the titers produced by 3 or 6 injections. Measurement of SBP by both the tail-cuff and telemetry methods confirmed that the values of SBP were somewhat reduced in the rats with 1 injection compared with rats with no injection of AT1 vaccine, but the results did not attain statistical significance. The telemetry BP measurements were performed in the morning (from 0900 hours to 1100 hours), and the data presented are the average of the measurements during a 2-h period. In some experiments, measurements were performed from 2100 hours to 2300 hours, but no differences were found compared with the morning measurements. In contrast, both three and six injections of AT1 vaccine produced similar increases in AT1 antibody titers, and the same decreases in systolic BP.
Effects of AT1 vaccination on SBP
In the next experiment (protocol 2), the effects of AT1 vaccination on SBP and L-NAME-induced renal injury were examined. Before the first vaccination or administration of antihypertensive drugs, SBP levels of all groups were equal. After vaccination, there was a significant decrease in SBP of the AT1 vaccine group (group 4) when compared with the control group (group 2), starting at age 9 weeks and continuing until the end of the study (Figure 1). No significant differences in SBP were found between the control group (group 2) and the KLH vehicle-vaccinated group (group 3). The SBP levels of the hydralazine group (group 5) and the candesartan group (group 6) were comparable to the AT1 vaccine group throughout the study.
Effect of Ang II type 1 (AT1) vaccination on systolic blood pressure in L-NAME-treated spontaneously hypertensive rat. Cont: control; Keyhole Limpet Haemocyanin (KLH): rats injected with KLH vehicle; AT1-V: rats injected with AT1 receptor vaccine; Hydra: rats treated continuously with hydralazine; Cand: rats treated continuously with candesartan; L-NAME: treated with L-NAME from 18 to 21 weeks of age. *P<0.05, **P<0.01 vs. KLH.
Effects of AT1 vaccination on L-NAME-induced proteinuria and renal injury
Before the administration of L-NAME, at 18 weeks of age, urine protein of all groups was within the normal range for rats of this age (values of urine protein are ∼30–50 mg per 100 g per day in untreated normotensive Wistar–Kyoto rats13), but urine protein levels of the AT1 vaccine and candesartan group were already significantly less than the control groups. After the administration of L-NAME, a dramatic increase in proteinuria was seen in the control and vehicle groups. This increase in proteinuria was completely suppressed in the vaccine group and the candesartan group, but not in the hydralazine group (Figure 2a). BUN level increased after L-NAME administration and this increase was attenuated in the vaccine group and the candesartan group (Figure 2b). A similar trend was found for serum creatinine, but the results did not attain statistical significance.
Effect of Ang II type 1 (AT1) vaccination on renal injury in L-NAME-treated spontaneously hypertensive rat. Effects on (a) urine protein, (b) blood urea nitrogen (BUN) and serum creatinine (Cr), (c) renal histological scores, (d) plasma renin activity (PRA) and plasma aldosterone concentration (PAC). Abbreviations of the different groups as in Figure 1. *P<0.05, vs. Keyhole Limpet Haemocyanin (KLH); ,†P<0.05 vs. Hydra.
Effects of AT1 vaccination on the histopathological changes of the kidneys, thoracic aortas and hearts
Examination of renal histology revealed that L-NAME treatment resulted in marked glomerulosclerosis and vascular injury (Figure 3). In the AT1 vaccine group, the glomerular and vascular injury scores were significantly suppressed compared with the control, vehicle and hydralazine groups (Figure 2c). Examination of thoracic aortas indicated that media/lumen ratios of the AT1 vaccine group were lower than those of the vehicle and the hydralazine groups. Heart weight/body weight ratios were also significantly suppressed compared with the hydralazine group (Table 2).
Light microscopy of renal histology in the different groups. Representative photomicrographs of paraformaldehyde-fixed sections stained with PAS are shown. Original magnification: × 200. Insets show details of vascular injury. A full color version of this figure is available at the Hypertension Research journal online.
Effects of AT1 vaccination on the components of the RAS
Administration of L-NAME was found to cause a marked increase in the PRA, as reported previously (Figure 2d). Plasma aldosterone concentration also appeared to be elevated after L-NAME administration, and this appeared to be suppressed in the vaccine group, but the results did not attain statistical significance. Real-time RT-PCR studies revealed that the renal renin mRNA expression in the AT1 vaccine group and the candesartan group were significantly increased compared with the vehicle group (Table 3). In contrast, no differences in expression of Ang-converting enzyme, AT1 and AT2 mRNA levels were found between the different groups.
Effects of AT1 vaccination on glomerular slit membrane protein expression
Immunofluorescence studies revealed that expression of the slit membrane protein nephrin was significantly increased in the AT1 vaccine and the candesartan groups, but not in the hydralazine group (Figures 4a and b). Expression of podocin also appeared to be somewhat increased, but the result did not attain statistical significance (Figures 4c and d).
Results of immunofluorescence studies. (a, c) Representative photomicrographs changes in (a) nephrin, (c) podocin expression in the different groups. (b, d) Quantitation of (b) nephrin and (d) podocin stained area. %: percentage of total glomerular area. Abbreviations of the different groups as in Figure 1. *P<0.05, vs. Keyhole Limpet Haemocyanin (KLH) †P<0.05 vs. Hydra.
Effects of AT1 vaccination on responses to Ang II in vivo and in vitro
Studies were performed to examine the responses of the AT1 vaccine-treated rats to Ang II in vivo and in vitro. In the in vivo study, injection of Ang II resulted in a marked increase in SBP in the KLH vehicle-treated rats. This increase of SBP was significantly suppressed in AT1 vaccine-treated rats (Figures 5a and b). The effects of addition of affinity purified IgG obtained from the serum of the KLH vehicle-treated and AT1 vaccine-treated rats on Ang II-induced ERK phosphorylation were examined in vitro using cultured VSMCs. These studies revealed that phosphorylation of ERK was suppressed in VSMCs incubated with IgG antibody obtained from the serum of AT1 receptor vaccinated rats (Figures 5c and d).
Effects of Ang II type 1 (AT1) vaccination on responses to angiotensin II (Ang II) in vivo and in vitro. (a) Representative tracing of blood pressure reaction after Ang II infusion. (b) Quantitation of changes in systolic blood pressure before and after Ang II infusion. (c) Representative image of western blot analysis of ERK1/2 phosphorylation after addition of Ang II in vascular smooth muscle cells. (d) Quantitation of levels of phospho-ERK1/2 (p-ERK1/2) before and after addition of Ang II. Keyhole Limpet Haemocyanin (KLH): rats injected with KLH vehicle; AT1-V: rats injected with AT1 receptor vaccine. *P<0.05, **P<0.01 vs. Ang II (−); †P<0.05 vs. the respective groups. A full color version of this figure is available at the Hypertension Research journal online.
Long-term observation of the effects of AT1 vaccination on BP and antibody titers
In the third experiment (protocol 3), the long-term effects of AT1 vaccination on BP and antibody titers were examined. As shown in Figure 6a, SBP level increased markedly with age from age 3 weeks in the vehicle-treated group, and reached a plateau of ∼230 mm Hg. SBP was significantly lower in the AT1-vaccinated group from age 9 weeks. However, the difference in BPs gradually declined with time, and no significant difference was found after age 33 weeks. Antibody titers measurement revealed similar trend. As shown in Figure 6b, the antibody titers reached a peak at ∼12 weeks (4 weeks after the third vaccination), and gradually declined over several months.
Discussion
The results of the present study indicate that vaccination against AT1 receptor not only decreases BP, but also significantly prevents the development of L-NAME-induced renal injury in the SHR model. In particular, assessment of proteinuria and examination of glomerular and vascular lesions suggested that both proteinuria and histological injury were attenuated by transient AT1 vaccination as effectively as continuous treatment with candesartan, and more effectively than continuous treatment with hydralazine.
It is known that oral administration of the nitric oxide synthase inhibitor, L-NAME, induces hypertension, proteinuria, glomerulosclerosis in rats,16 and that the renal lesions are especially prominent in L-NAME-treated SHR.17 For these reasons, the L-NAME/SHR model has been considered an animal model for human hypertensive nephrosclerosis, which is a leading cause of end-stage renal disease throughout the world.13, 18
In this study, urine protein increased markedly after administration of L-NAME, and this increase was not significantly attenuated in the hydralazine-treated group, despite a similar reduction of BP compared with the other treated groups. In contrast, the proteinuria was completely suppressed in the AT1 vaccine group and the candesartan group, confirming the effectiveness of RAS inhibition for the suppression of proteinuria in this model.
At present, the contribution of BP-independent mechanisms in the reduction of proteinuria by RAS blockade is still not clearly defined. It has been suggested that increased expression of the slit membrane nephrin may contribute to the antiproteinuric actions of RAS inhibitors. Jia et al.19 reported that Ang II infusion causes decreased nephrin expression, while Davis et al.20 reported that treatment with ARB caused increased glomerular nephrin expression and reduced albuminuria. These effects were not found with an equally hypotensive dose of the calcium channel blockers amlodipine and verapamil. It is therefore interesting that the nephrin expression was equally preserved by vaccination against AT1 receptor, as well as by administration of ARB in our study. Podocin expression has also been reported to be upregulated by ARB treatment.21 In this study, both AT1 receptor vaccination and ARB treatment caused a small increase in podocin expression, however, the results did not attain statistical significance.
The changes in BP and antibody titers appeared to be compatible with the notion that the antibody produced by AT1 receptor vaccination directly inhibited AT1 receptor and induced the antihypertensive effect. In order to verify this hypothesis, we carried out in vivo and in vitro experiments to examine the effects of AT1 vaccination on responses to Ang II. Both in vivo and in vitro study confirmed that AT1 vaccination increased AT1 antibody titers and reduced the responses to Ang II, suggesting that these inhibitory antibodies provided sustained protection against the effects of Ang II. On the other hand, we and others have shown that transient inhibition of the RAS during the ‘prehypertensive phase’ (∼3–10 weeks of age in rats), results in a sustained decrease in BP,22, 23, 24 possibly by attenuation of the ‘reno-vascular amplifier’ mechanism, which may drive the progression from prehypertension to hypertension.25 The possibility that suppression of this ‘reno-vascular amplifier’ may have contributed to the sustained suppression of hypertension cannot be completely ruled out.
In our preliminary study, we found that three injections of AT1 receptor vaccine were almost as effective as six injections for both lowering the BP and increasing the antibody titer. A single injection appeared to have a lesser effect. However, it should be noted that, although the AT1 receptor titer values declined over several months, they were still detectable at the end of the study at age 52 weeks. Therefore, it is possible that subsequent single ‘booster’ injections may be sufficient to maintain AT1 antibody titers for continuation of AT1 blockade, but this hypothesis remains to be tested. In the clinical study by Tissot et al.8 using a vaccine against Ang II, the antibody titers in hypertensive patients were similarly maintained for several months, suggesting the possibility that vaccination once every few months could be sufficient to maintain the antihypertensive effect. Further studies are required to determine the optimum timing and dose of vaccination for future clinical use.
At present, the optimum target for vaccination against the RAS is unclear.26, 27 As mentioned in the Introduction, initial attempts to use a vaccine against renin were abandoned because of the side-effect of interstitial nephritis in animal models. In the present study, we did not observe any interstitial changes in the kidney, and the parameters of renal injury were clearly improved in the AT1 vaccine-treated rats. Moreover, we have observed that longevity also seems to be increased in AT1-vaccinated rats (unpublished observations). Although vaccines against Ang I and Ang II have been independently determined to be without major side effects in Phase II studies, the antihypertensive actions have not always been clear. One potential concern in using the AT1 receptor as a target for vaccination is the possibility of developing agonistic antibodies. It has been suggested that such antibodies may contribute to the worsening of hypertension in preeclampsia.28, 29 The results of our in vivo and in vitro studies suggested that agonistic antibodies were not produced in this model, however, the safety in humans is unclear, and should be investigated in further studies.
In summary, the results of this study suggest that AT1 receptor vaccination has the potential to develop into an effective therapy for prevention of renal injury, particularly in patients with hypertensive nephrosclerosis. Because of the increasing number of patients with hypertension throughout the world, further studies are warranted to examine if these results may be applicable to prevention of hypertensive renal disease in humans.
References
Hill GS . Hypertensive nephrosclerosis. Curr Opin Nephrol Hypertens 2008; 17: 266–270.
Nakai S, Suzuki K, Masakane I, Wada A, Itami N, Ogata S, Kimata N, Shigematsu T, Shinoda T, Syouji T, Taniguchi M, Tsuchida K, Nakamoto H, Nishi S, Nishi H, Hashimoto S, Hasegawa T, Hanafusa N, Hamano T, Fujii N, Marubayashi S, Morita O, Yamagata K, Wakai K, Watanabe Y, Iseki K, Tsubakihara Y . Overview of regular dialysis treatment in Japan (as of 31 December 2008). Ther Apher Dial 2010; 14: 505–540.
USRDS. Annual Data Report: Atlas of end-stage renal disease in the United States. National Institutes of Health, National Institutes of Diabetes and Digestive and Kidney Diseases: Bethesda, 2007.
Berl T . Review: renal protection by inhibition of the renin-angiotensin-aldosterone system. J Renin Angiotensin Aldosterone Syst 2009; 10: 1–8.
Stojiljkovic L, Behnia R . Role of renin angiotensin system inhibitors in cardiovascular and renal protection: a lesson from clinical trials. Curr Pharm Des 2007; 13: 1335–1345.
Ruggenenti P, Perticucci E, Cravedi P, Gambara V, Costantini M, Sharma SK, Perna A, Remuzzi G . Role of remission clinics in the longitudinal treatment of CKD. J Am Soc Nephrol 2008; 19: 1213–1224.
Haller H, Ito S, Izzo Jr JL, Januszewicz A, Katayama S, Menne J, Mimran A, Rabelink TJ, Ritz E, Ruilope LM, Rump LC, Viberti G . Olmesartan for the delay or prevention of microalbuminuria in type 2 diabetes. N Engl J Med 2011; 364: 907–917.
Tissot AC, Maurer P, Nussberger J, Sabat R, Pfister T, Ignatenko S, Volk HD, Stocker H, Muller P, Jennings GT, Wagner F, Bachmann MF . Effect of immunisation against angiotensin II with CYT006-AngQb on ambulatory blood pressure: a double-blind, randomised, placebo-controlled phase IIa study. Lancet 2008; 371: 821–827.
Goldblatt H, Haas E, Lamfrom H . Antirenin in man and animals. Trans Assoc Am Physicians 1951; 64: 122–125.
Michel JB, Sayah S, Guettier C, Nussberger J, Philippe M, Gonzalez MF, Carelli C, Galen FX, Menard J, Corvol P . Physiological and immunopathological consequences of active immunization of spontaneously hypertensive and normotensive rats against murine renin. Circulation 1990; 81: 1899–1910.
Brown MJ, Coltart J, Gunewardena K, Ritter JM, Auton TR, Glover JF . Randomized double-blind placebo-controlled study of an angiotensin immunotherapeutic vaccine (PMD3117) in hypertensive subjects. Clin Sci (Lond) 2004; 107: 167–173.
Zhu F, Liao YH, Li LD, Cheng M, Wei F, Wei YM, Wang M . Target organ protection from a novel angiotensin II receptor (AT1) vaccine ATR12181 in spontaneously hypertensive rats. Cell Mol Immunol 2006; 3: 107–114.
Ishiguro K, Sasamura H, Sakamaki Y, Itoh H, Saruta T . Developmental activity of the renin-angiotensin system during the ‘critical period’ modulates later L-NAME-induced hypertension and renal injury. Hypertens Res 2007; 30: 63–75.
Ishiguro K, Hayashi K, Sasamura H, Sakamaki Y, Itoh H . ‘Pulse’ treatment with high-dose angiotensin blocker reverses renal arteriolar hypertrophy and regresses hypertension. Hypertension 2009; 53: 83–89.
Hayashi K, Sasamura H, Ishiguro K, Sakamaki Y, Azegami T, Itoh H . Regression of glomerulosclerosis in response to transient treatment with angiotensin II blockers is attenuated by blockade of matrix metalloproteinase-2. Kidney Int 2010; 78: 69–78.
Baylis C, Mitruka B, Deng A . Chronic blockade of nitric oxide synthesis in the rat produces systemic hypertension and glomerular damage. J Clin Invest 1992; 90: 278–281.
Toba H, Nakagawa Y, Miki S, Shimizu T, Yoshimura A, Inoue R, Asayama J, Kobara M, Nakata T . Calcium channel blockades exhibit anti-inflammatory and antioxidative effects by augmentation of endothelial nitric oxide synthase and the inhibition of angiotensin converting enzyme in the N(G)-nitro-L-arginine methyl ester-induced hypertensive rat aorta: vasoprotective effects beyond the blood pressure-lowering effects of amlodipine and manidipine. Hypertens Res 2005; 28: 689–700.
Jover B, Mimran A . Nitric oxide inhibition and renal alterations. J Cardiovasc Pharmacol 2001; 38 (Suppl 2): S65–S70.
Jia J, Ding G, Zhu J, Chen C, Liang W, Franki N, Singhal PC . Angiotensin II infusion induces nephrin expression changes and podocyte apoptosis. Am J Nephrol 2008; 28: 500–507.
Davis BJ, Cao Z, de Gasparo M, Kawachi H, Cooper ME, Allen TJ . Disparate effects of angiotensin II antagonists and calcium channel blockers on albuminuria in experimental diabetes and hypertension: potential role of nephrin. J Hypertens 2003; 21: 209–216.
Fukuda A, Fujimoto S, Iwatsubo S, Kawachi H, Kitamura K . Effects of mineralocorticoid and angiotensin II receptor blockers on proteinuria and glomerular podocyte protein expression in a model of minimal change nephrotic syndrome. Nephrology (Carlton) 2010; 15: 321–326.
Harrap SB, Van der Merwe WM, Griffin SA, Macpherson F, Lever AF . Brief angiotensin converting enzyme inhibitor treatment in young spontaneously hypertensive rats reduces blood pressure long-term. Hypertension 1990; 16: 603–614.
Zhang L, Edwards DG, Berecek KH . Effects of early captopril treatment and its removal on plasma angiotensin converting enzyme (ACE) activity and arginine vasopressin in hypertensive rats (SHR) and normotensive rats (WKY). Clin Exp Hypertens 1996; 18: 201–226.
Nakaya H, Sasamura H, Kitamura Y, Amemiya T, Konishi K, Hayashi M, Saruta T . Effects of angiotensin inhibitors on renal injury and angiotensin receptor expression in early hypertensive nephrosclerosis. Hypertens Res 1999; 22: 303–312.
Sasamura H, Hayashi K, Ishiguro K, Nakaya H, Saruta T, Itoh H . Prevention and regression of hypertension: role of renal microvascular protection. Hypertens Res 2009; 32: 658–664.
Brown MJ . Therapeutic potential of vaccines in the management of hypertension. Drugs 2008; 68: 2557–2560.
Gradman AH, Pinto R . Vaccination: a novel strategy for inhibiting the renin-angiotensin-aldosterone system. Curr Hypertens Rep 2008; 10: 473–479.
Xia Y, Zhou CC, Ramin SM, Kellems RE . Angiotensin receptors, autoimmunity, and preeclampsia. J Immunol 2007; 179: 3391–3395.
Herse F, Staff AC, Hering L, Muller DN, Luft FC, Dechend R . AT1-receptor autoantibodies and uteroplacental RAS in pregnancy and pre-eclampsia. J Mol Med 2008; 86: 697–703.
Acknowledgements
This study was supported by Grants for Scientific Research (20590984, 2155542, 20680105) from the Ministry of Education, Culture, Sports, Science and Technology (MEXT) of Japan, the Nateglinide Memorial Toyoshima Research and Education Fund and the Salt Science Foundation, Tokyo, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Azegami, T., Sasamura, H., Hayashi, K. et al. Vaccination against the angiotensin type 1 receptor for the prevention of L-NAME-induced nephropathy. Hypertens Res 35, 492–499 (2012). https://doi.org/10.1038/hr.2011.212
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2011.212
Keywords
This article is cited by
-
Challenges in the development of novel therapies, vaccines and siRNAs for the treatment of hypertension
Hypertension Research (2023)
-
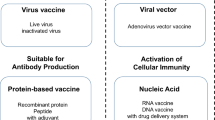
Therapeutic vaccine for chronic diseases after the COVID-19 Era
Hypertension Research (2021)
-
Vaccines against components of the renin–angiotensin system
Heart Failure Reviews (2021)
-
Pre-emptive medicine for hypertension and its prospects
Hypertension Research (2019)
-
Therapeutic Vaccines for Hypertension: a New Option for Clinical Practice
Current Hypertension Reports (2018)