Abstract
Purpose:
Joubert syndrome (JS) is a genetically and clinically heterogeneous ciliopathy characterized by distinct cerebellar and brainstem malformations resulting in the diagnostic “molar tooth sign” on brain imaging. To date, more than 30 JS genes have been identified, but these do not account for all patients.
Methods:
In our cohort of 100 patients with JS from 86 families, we prospectively performed extensive clinical evaluation and provided molecular diagnosis using a targeted 27-gene Molecular Inversion Probes panel followed by whole-exome sequencing (WES).
Results:
We identified the causative gene in 94% of the families; 126 (27 novel) unique potentially pathogenic variants were found in 20 genes, including KIAA0753 and CELSR2, which had not previously been associated with JS. Genotype–phenotype correlation revealed the absence of retinal degeneration in patients with TMEM67, C5orf52, or KIAA0586 variants. Chorioretinal coloboma was associated with a decreased risk for retinal degeneration and increased risk for liver disease. TMEM67 was frequently associated with kidney disease.
Conclusion:
In JS, WES significantly increases the yield for molecular diagnosis, which is essential for reproductive counseling and the option of preimplantation and prenatal diagnosis as well as medical management and prognostic counseling for the age-dependent and progressive organ-specific manifestations, including retinal, liver, and kidney disease.
Genet Med advance online publication 26 January 2017
Similar content being viewed by others
Introduction
Joubert syndrome (JS; OMIM 213300) was first described in 1969 based on the neurological features of episodic hyperpnea, abnormal eye movements, ataxia, cognitive impairment, and agenesis of the cerebellar vermis.1 Advances in brain imaging subsequently identified the “molar tooth sign” as a diagnostic finding in JS. The molar tooth sign occurs because of a distinctive set of cerebellum and midbrain abnormalities and is apparent on axial brain magnetic resonance (MR) images obtained through the junction of the midbrain and pons.2,3,4 Typical clinical features of JS within the first months of life include hypotonia, abnormal respiratory pattern, abnormal eye movements, and developmental delay. Although some patients with JS have only neurological abnormalities, others have multisystem organ involvement including fibrocystic kidney and liver disease, retinal dystrophy, chorioretinal colobomas, occipital encephalocele, and polydactyly.2,5 This clinical heterogeneity led to the use of the term “Joubert syndrome and related disorders,” which includes Senior-Løken and COACH (colobomas, “oligophrenia” for cognitive impairment, ataxia, cerebellar vermis hypoplasia, and hepatic fibrosis) syndromes.2,4 More recently, the term JS has been recommended to refer to all patients with the “molar tooth sign,” with or without extraneurological system involvement.6 In this article, for simplicity, “JS” includes Senior-Løken and COACH syndromes.
After identification of the subcellular localizations and functions of the proteins defective in JS, the disorder was recognized as a disorder of the nonmotile cilia, or a “ciliopathy.”7,8 Ciliopathies have overlapping features, including fibrocystic diseases of the kidneys and liver, retinal degeneration, obesity, structural and functional defects of the central nervous system and the eyes, abnormal bone growth, abnormal sidedness of internal organs, and polydactyly.5,7 Like other syndromic ciliopathies, such as Bardet-Biedl (OMIM 209900) and Meckel (OMIM 249000) syndromes, JS is genetically highly heterogeneous. To date, more than 30 genes have been identified as causing JS, and many patients remain undiagnosed, suggesting further genetic heterogeneity.2
The clinical diagnosis of JS is based on the presence of the “molar tooth sign”; molecular genetic diagnosis of the syndrome remains challenging owing to the large number of genetic causes and highly variable multisystem manifestations. Here, we present the molecular genetic findings of our cohort of 100 JS patients from 86 families in the context of extraneurological organ-system manifestations, including retina, kidney, and liver disease.
Materials and Methods
Patients
All patients were prospectively evaluated at the National Institutes of Health (NIH) Clinical Center, between 2003 and 2014, under the intramural NIH research protocol “Clinical and Molecular Investigations Into Ciliopathies” (ClinicalTrials.gov, NCT00068224), approved by the National Human Genome Research Institute Institutional Review Board. For recruitment, the study was advertised to patients and families by the Joubert Syndrome & Related Disorders Foundation as a natural-history study aiming to describe the individual organ-system involvement in JS, including kidney and liver disease. Patients and/or their parents gave written, informed consent. Enrollment criterion was clinical diagnosis of JS including Senior-Løken and COACH syndromes. All patients were evaluated at the NIH Clinical Center by a single pediatrician–clinical geneticist (M.G.-A.); evaluations included medical history, family history, physical examination, review of medical records, review of brain MR images, high-resolution abdominal ultrasonography, formal neurocognitive evaluations, electroencephalogram, complete ophthalmic examination, and comprehensive blood and urine chemistries. Blood samples for DNA analysis were collected from all patients and parents, when available.
The patients were classified as having chorioretinal coloboma, retinal degeneration, kidney disease, and liver disease based on clinical and laboratory evaluations performed at the NIH Clinical Center. Retinal degeneration was diagnosed based on typical findings on NIH retinal examination after dilation of the pupils; when available, electroretinography findings and findings on past eye examinations were also used for decision making. Liver disease was defined as elevation of liver enzymes and/or increased echogenicity of the liver and/or splenomegaly on abdominal ultrasonography. Kidney disease was defined as elevated serum creatinine and cystatin-C and/or abnormal findings on renal ultrasonography, including loss of corticomedullary distinction, increased or decreased kidney size, and presence of cystic changes. Patients with accessory digits, including small skin tags of the upper or lower extremities, were classified as having polydactyly. All available brain MR images were qualitatively evaluated by a team of five physicians—two pediatric neuroradiologists, one adult neuroradiologist, one pediatric neurologist, and one pediatric clinical geneticist (M.G.-A.)—as a group to achieve consensus. Twelve families were represented by more than one affected individual; data analysis to determine prevalence of manifestations and genotype–phenotype correlations was based on one affected individual for each family.
Molecular inversion probes
Molecular inversion probe (MIP) technology was developed for the genotyping of single-nucleotide polymorphisms.9 This method was then modified for genomic regions of interest in targeted sequencing.10 MIPs are probes that anchor targeted regions and are circularized after polymerization and ligation to prepare the sequencing library. MIP capture has been demonstrated to be a robust technology for high-throughput sequencing of targeted regions11 and used with success to identify mutations in different disorders.12,13
We applied this method for direct sequencing of MIP-derived amplicons of the coding exons of 27 genes associated with JS (AHI1, ARL13B, B9D1, B9D2, C2CD3, C5orf42, CC2D2A, CEP290, CEP41, CSPP1, IFT172, INPP5E, KIF7, MKS1, NPHP1, OFD1, RPGRIP1L, TCTN1, TCTN2, TCTN3, TMEM138, TMEM216, TMEM231, TMEM237, TMEM67, TTC21B, and ZNF423). The coding regions of these genes were sequenced by combining a MIP capture method and next-generation sequencing. For this approach,14 which was performed at the University of Washington, we used 100 ng of genomic DNA; the captured DNA was amplified by PCR and sequenced on either an Illumina HiSeq or a MiSeq platform. Sequence reads were mapped using the Burrows-Wheeler Aligner (V.0.5.9). Variants were called using the Genome Analysis Toolkit (V.2.5–2) and annotated with SeattleSeq (http://snp.gs.washington.edu/SeattleSeqAnnotation138/).
Whole-exome sequencing
Genomic DNA was obtained from leukocytes using standard protocols. For exome sequencing we used the HiSeq2000 (Illumina, San Diego, CA),15 which used 101-bp paired-end read sequencing. Image analysis and base calling were performed using Illumina Genome Analyzer Pipeline software (versions 1.13.48.0) with default parameters. Reads were aligned to a human reference sequence (UCSC assembly hg19, NCBI build 37) using a package called Efficient Large-scale Alignment of Nucleotide Databases (Illumina). Genotypes were called at all positions where there were high-quality sequence bases using a Bayesian algorithm called the Most Probable Genotype,16 and variants were filtered using the graphical software tool VarSifter v1.5.17 The database dbSNP (http://www.ncbi.nlm.nih.gov/snp/) covers the 1.22% of the human genome corresponding to the Consensus Conserved Domain Sequences and more than 1,000 noncoding RNAs.
Genomic DNA sequencing
Genomic DNA was obtained from leukocytes using standard protocols. For dideoxy sequencing of genomic DNA, primers were designed to cover areas of variants identified by WES. Direct sequencing of the PCR amplification products was performed using BigDye 3.1 Terminator chemistry (Applied Biosystems, Austin, TX) and separated on an ABI 3130xl genetic analyzer (Applied Biosystems). Data were evaluated using Sequencher v5.0 software (Gene Codes, Ann Arbor, MI).
Statistical analysis
Statistical methods for associations between one extraneurological organ disease and another and between genes and extraneurological organ disease included the chi-squared test, Fisher’s test (with Bonferroni correction), odds ratio point estimates, and confidence intervals (without Bonferroni correction) applied to 2 × 2 tables of presence/absence. Age comparisons between various groups involved t-tests, with associated tests for equality of variance. Statistical analyses were performed using SAS version 9.4.
Results
Patient cohort
Phone interviews were conducted (by M.G.-A.) with 120 patients from 105 families. Fifteen families could not travel to the NIH Clinical Center in Bethesda, Maryland; in some cases, this was due to the severity of their child’s JS, which required intensive care. The remaining 105 patients from 90 families all underwent weeklong clinical evaluations at the NIH Clinical Center. Most families were residing in the United States; a few families traveled from Canada, Europe, or Australia. Representative brain MR images are shown in Figure 1 . In our review of the brain MR images, we observed that eight patients from six families did not have the “molar tooth sign,” including three patients with classic kidney and retinal features of Senior-Løken syndrome (Supplementary Table S3 online, patients 290, 462, and 463). We included these three Senior-Løken patients in this paper but excluded the remaining five patients without the molar tooth sign whose clinical features were nonspecific.
Brain magnetic resonance (MR) images showing diagnostic findings of Joubert syndrome (JS) in comparison to normal findings. (a) Axial brain MR image obtained at the level of the junction of the midbrain and pons showing the “molar tooth sign” (circle) and hypoplastic cerebellar vermis (arrows) in comparison to normal (c). (b) Sagittal brain MR image demonstrating hypoplasia of the cerebellar vermis (circle) and enlarged fourth ventricle (asterisk) with rostral displacement of the fastigium in comparison to normal (d).
Molecular genetic findings for each of the 100 patients with JS, as well as major clinical features, including retinal degeneration, coloboma, polydactyly, and kidney and liver disease (see “Materials and Methods” for definitions), and details of the variants (with CADD scores18) are summarized in Supplementary Table S3 online. Twelve families contributed more than 1 child, 11 families had 2 (families 6, 7, 8, 18, 24, 29, 36, 65, 68, and 81; Supplementary Table S3 online), and 2 families had 3 JS siblings (families 16 and 66; Supplementary Table S3 online). There were 43 females and 57 males. Ages ranged from 0.6 to 36 years (9.2 ± 7.5 years) (Supplementary Table S3 online). Twenty-seven percent of patients presented with neurodevelopmental symptoms, including hypotonia and developmental delay, but did not have any other organ-system abnormalities outside the central nervous system. Retinal degeneration was detected in 19%, coloboma in 30%, postaxial polydactyly in 13%, fibrocystic kidney disease in 34%, and liver disease in 41% (Supplementary Table S3 online, Figure 2a ).
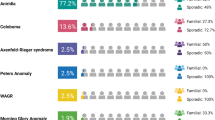
Extraneurological organ-system involvement in our cohort with Joubert syndrome (JS). (a) Prevalence of kidney disease, liver disease, chorioretinal coloboma, retinal degeneration, and polydactyly in our cohort with JS. (b) Prevalence of combinations of extraneurological organ-system disease with causative genes indicated. (c) Prevalence of extraneurological manifestations in patients with JS with mutations in the six most common JS genes in our cohort. CNS, central nervous system.
Molecular genetic findings
Of the 100 patients (86 families), 12 patients (9 families) obtained a molecular diagnosis during their clinical diagnostic evaluation prior to the NIH visit, all via clinical gene panel sequencing for JS. As a part of the NIH study, the MIPs panel14 of 27 genes was performed in 98 patients from 85 families, including the 9 families with a prior molecular diagnosis (Supplementary Figure S1 online). The MIPs panel identified the potentially pathogenic variants in 39 of the 85 families (46%). In family 12, the MIPs panel identified one of the two variants (Supplementary Table S3 online). WES was performed for patients and parents from 40 families, including the one family that did not undergo MIPs panel analysis (Supplementary Table S3 online). The average coverage of all the samples is approximately 80×, with a minimum of 40× and a maximum of 123× (Supplementary Figure S2 online). Using WES, we identified potential pathogenic variants in 35 of the 40 families (88%) (Supplementary Figure S1 online).
For 5 families, the potential molecular genetic cause of JS could not be identified by MIPs or WES (Supplementary Table S3 online). Of the 81 families with identified gene variants, 2 had hemizygous variants in the X-linked OFD1. At least two variants were identified in all but 3 of the 77 families with autosomal recessively inherited JS genes. Only one variant was identified in 2 families with TMEM67 and in 1 family with C5orfF42 (Supplementary Table S3 online). Homozygous mutations were detected in 9 of 81 families. There was known consanguinity in only 1 family (Supplementary Table S3 online, family 18).
Overall, we identified a total 126 unique (156 alleles), potentially pathogenic variants in 20 genes; 27 of these variants were novel (Supplementary Table S3 online, Figure 3a and Supplementary Figures S1 and S3 online). The MIPs panel detected 52 truncating and 27 missense variants, and WES resulted in identification of 42 truncating and 32 missense variants (Supplementary Table S3 online). Two of these 20 genes were not previously known to cause JS, including CELSR2, which was not previously associated with any human disease (more details in refs. 19), and KIAA0753 (data unpublished), which was recently reported to cause oral-facial-digital syndrome type VI.20 The CELSR2 variant’s minor allele frequencies (MAF) are extremely low in the ExAC (Exome Aggregation Consortium) database (NM_001408: c.1150G>A; p.(Ala384Thr) MAF: 0.0000829 and NM_001408: c.6908C>T; p.(Thr2303Met) MAF: 0.00002476), whereas the KIAA0753 variants are not found in the ExAC database.
The relative frequencies of genetic causes in the NIH cohort with Joubert syndrome (JS). (a) Pie charts showing the prevalence of genetic causes in the entire NIH JS cohort in comparison to subsets without extraneurological disease (b), liver disease (c), coloboma (d), kidney disease (e), retinal degeneration (f), and polydactyly (g).
Clinical and molecular correlations
The prevalence of combinations of extraneurological organ-system disease in subsets of patients with JS and the causative genes for each group are depicted in Figure 2b . The prevalence of the genetic causes for subsets of our cohort of JS with liver disease, coloboma, kidney disease, retinal degeneration, and polydactyly are shown in Figure 3b – g . Detailed results of statistical analysis searching for correlations among individual extraneurological organ diseases and for genotype–phenotype correlations are listed in Supplementary Tables S1 and S2 online.
For 26 patients, no disease features were identified outside the central nervous system; they did not have chorioretinal coloboma, polydactyly, evidence of retinal degeneration, fibrocystic kidney disease, or liver fibrosis, at least at the age when they were examined at the NIH Clinical Center ( Figure 2a , b and Figure 3b ). Among these individuals with JS with no apparent nonneurological findings, the most common genetic causes were C5orf42 (27%), CC2D2A (17%), and KIAA0586 (17%) (Supplementary Table S3 online, Figures 2b and 3b ).
Of the 30 JS patients with coloboma, only 2 had retinal degeneration, and both of them had variants in CEP290 (Supplementary Table S3 online). Of the 30 patients with coloboma, 18 (60%) had liver disease; in comparison, liver disease occurred in 34% (24/70) of patients without coloboma. Four of the 22 patients with TMEM67-related JS had liver disease in the absence of coloboma, including one sib pair (Supplementary Table S3 online). In the 30 patients with JS with coloboma, variants in nine genes were identified; TMEM67 was most common (54%), followed by CEP290 (8%) and KIAA0586 (8%) (Supplementary Table S3 online, Figure 3d ). Of the patients with coloboma and identifiable genetic cause, only those with TMEM67 variants had liver disease; none of the patients with coloboma with variants in the remaining eight genes had liver disease (Supplementary Table S3 online). The genetic cause remains unknown in 7% of patients with coloboma and liver disease ( Figure 2B ).
Kidney disease was diagnosed in 32 of 100 patients; 9 of these 32 (28%) had retinal degeneration (Supplementary Table S3 online). Of the 20 patients with retinal degeneration, 9 (45%) had kidney disease. In the group of 23 JS patients with kidney disease but no retinal degeneration, TMEM67 variants were the most common potential genetic causes, accounting for 43% of these families. Of the 22 patients with TMEM67 variants, 11 (50%) had kidney disease (Supplementary Table S3 online, Figures 2b , c and 3e ). Patients with kidney disease and retinal degeneration had variants in five genes, including CEP290 (38%), AHI1 (25%), and NPHP1 (12.5%) (Supplementary Table S3 online, Figure 2b ). Retinal degeneration was not seen in patients with variants in TMEM67 (n = 22), C5orf42 (n = 14), or KIAA0586 (n = 6). None of the 14 patients with C5orf42 variants had kidney disease.
Postaxial polydactyly was present in 13 of 100 patients from 11 of 86 families (Supplementary Table S3 online, Figure 2a , b ). Potentially pathogenic variants in six genes were detected in patients with polydactyly, with the most common one being C5orf42 (27%) (Supplementary Table S3 online, Figure 3g ). Four of five patients with C5orf42 variants had liver disease in addition to polydactyly. The patient with CEP164 variants had polydactyly, liver disease, severe retinal degeneration, and nephronophthisis.
Discussion
WES improves diagnosis of JS
The extreme genetic heterogeneity of JS presents a challenge for molecular genetic diagnosis. In addition, because the genotype–phenotype correlations in JS are limited, tiered Sanger sequencing of individual genes is generally not a practical option. The ethnic background of the patient may assist in prioritizing certain genes in only a few populations. For instance, common founder pathogenic variants in specific JS genes are known to occur in French Canadians (C5orf42, several variants)21 Ashkenazi Jews (TMEM216 p.(Arg73Leu)),22 and Hutterites (TMEM237 p.(Arg18*)).23 Therefore, in the majority of patients with JS, no specific clues exist regarding which of the more than 30 genetic causes is responsible in a given patient. Our molecular genetic diagnosis rate of 94% is significantly higher in comparison to the yield of prior reports based on targeted next-generation sequencing methods (i.e., 43 and 62%).14 This might be due not only to our approach of combining MIP and WES but also to the fact that we performed WES for families instead of just probands.24 If costs preclude WES, certain JS genes may be prioritized using the currently available prevalence data of the known genes combined with specific genotype information and, in some cases, ethnic background.
We identified potentially pathogenic variants in 20 different JS genes. Variants in six genes were seen in two-thirds of the families: TMEM67 (20%), C5orf42 (14%) and CC2D2A (11%), CEP290 (8%), AHI1 (7%), and KIAA0586 (7%). Each of the remaining 14 genes accounted for a small proportion of the families, ranging from 1–6%: MKS1 (6%), INPP5E (4%), NPHP1 (2%), TMEM216 (2%), OFD1 (2%), CSPP1 (2%), TMEM231 (1%), KIF7 (1%), B9D1 (1%), CEP164 (1%), RPGRIP1L (1%), TMEM237 (1%), KIAA0753 (1%), and CELSR2 (1%). In the large cohort of 375 families with JS collected worldwide and reported by Bachmann-Gagescu et al,14 in which KIAA0586 was not sequenced, variants in TMEM67, C5orf42, CC2D2A, CEP290, and AHI1 were also the most prevalent causes, suggesting that these six genes are likely to be the most prevalent JS genes across various populations. It is important to note, however, that some families with JS were enrolled in both our study and Bachmann-Gagescu’s study.14 Similarly, in a smaller cohort of northern European patients with JS, variants in C5orf42, TMEM67, and AHI1 were also common causes, whereas variants in CEP290 were less common. Therefore, if WES or large gene panels are not feasible because of cost or availability, then prioritization of these six most prevalent genes may be considered.
We were able to identify biallelic potential pathogenic variants in 96% of the solved families, whereas variants in only one allele were identified in two families with TMEM67 and one family with C5orf42. The TMEM67 variants in families 6 and 15 (Supplementary Table S3 online) were already known to be associated with COACH syndrome (also known as JS with congenital hepatic fibrosis),25 and the single variant identified in C5orf42 (family 20) was previously associated with JS.14 The fact that these single variants were already reported to cause the same phenotype supports the molecular diagnosis of TMEM67 and C5orf42 mutations in these families. Indeed, the second variant could be a copy-number variant (not detectable by our methods) or may be located in regions not targeted by our sequencing approaches (e.g., intron, untranslated regions, and promoters).
Comprehensive multisystem evaluation of patients with JS for extraneurological manifestations
This study describes the first large cohort of patients with JS who prospectively underwent comprehensive multisystem evaluations at a single center. Hence, we can present our molecular genetic findings in the context of comprehensive clinical data on the extraneurological manifestations of JS, including retinal degeneration and fibrocystic kidney and liver disease (Supplementary Table S3 online, Figures 2 and 3 ). Consistent with the findings of prior studies,14,26 the majority of patients with JS in this cohort had extraneurologic organ involvement; only 27% had JS without extraneurological manifestations.
Among the extraneurological manifestations of JS, certain patterns of involvement have been recognized for years. Coloboma is often associated with liver disease (COACH syndrome) and retinal degeneration is often associated with kidney disease (Senior-Løken syndrome).2,27,28 Consistent with the former finding, Bachmann-Gagescu et al.14 found that the odds of liver fibrosis developing in JS patients with coloboma were 6.5 times the odds of liver fibrosis developing in those without coloboma. In our cohort, coloboma and liver disease also occurred together, but the association was weaker (OR: 2.7, 95% CI: 0.85 to 5.52), probably because of differences in the ascertainment and sizes of the two cohorts. In our cohort, retinal degeneration was less strongly associated with kidney disease (OR: 2.3, 95% CI: 0.77 to 7.05) than in Bachmann-Gagescu’s study (OR: 3.0, 95% CI: 1.7 to 5.2),14 possibly because we were more likely to identify mild retinal degeneration cases at the NIH Clinical Center. In addition to these two associations, patients with JS in our cohort exhibited many other combinations of extraneurological disease (Supplementary Table S3 online, Figure 2b ), illustrating the extensive clinical variability of JS.
Based on retinal examinations performed at the NIH Clinical Center, our data showed that patients with chorioretinal coloboma were less likely to have retinal degeneration in comparison to those without coloboma (OR: 0.27, 95% CI: 0.06 to 1.31). (Supplementary Table S3 online, Figure 2c , Supplementary Tables S1 and S2 online). This negative association, not previously reported, may provide reassurance for families with young children with JS with coloboma.
Although the association of coloboma and liver disease in JS has been recognized for many years, the relatively common occurrence of kidney disease in patients with the combination of coloboma and liver disease has not been emphasized. Kidney disease was present in 50% of our cohort of 22 patients with TMEM67 variants. Among our 23 patients with JS with kidney disease but without retinal degeneration, TMEM67 variants were the most common potential genetic cause, accounting for 43% of families (Supplementary Table S3 online, Figures 2b , c and 3e ).
As expected, our search for correlations between specific genes and phenotypes showed strong correlations of coloboma with TMEM67 (OR: 22.2, 95% CI: 5.50 to 89.3) and of liver disease with TMEM67 (OR: 42.1, 95% CI: 5.22 to 340), which remained significant after Bonferroni correction. Other correlations (not significant after Bonferroni correction) included AHI1 with retinal degeneration (OR: 11.3, 95% CI: 1.86 to 68.9), CEP290 with kidney disease (OR: 14.6, 95% CI: 1.66 to 128), and CEP290 with retinal degeneration (OR: 7.44, 95% CI: 1.48 to 37.5). A negative correlation was identified between C5orf42 and kidney disease (OR: 0.06, 95% CI: 0.00 to 1.08).
In the 12 families with multiple affected siblings, the sibships were concordant in terms of their extraneurological organ-system involvement. In one family with three affected daughters due to TMEM231 variants, only one had elevated liver enzymes and the etiology may have been unrelated to JS (Supplementary Table S3 online). This finding might suggest that, in our cohort, modifier genes are less significant. However, this will require further study of a larger cohort of unrelated patients with the same genotype.
The JS group of ciliopathies exhibits wide variability in extraneurological manifestations, ranging from polydactyly to coloboma associated with liver disease complicated by severe portal hypertension to early-onset blindness associated with chronic progressive kidney disease that requires kidney transplantation in childhood.5 Therefore, molecular genetic diagnosis is essential for reproductive counseling in JS as well as prognostic counseling and medical management of individual organ-system involvement, including retina, kidney, and liver disease. As with other syndromic ciliopathies, such as Bardet-Biedl and Meckel syndromes, the molecular genetic diagnostic approach to JS represents a challenge because of extreme genetic heterogeneity. In addition, lack of clear and broadly applicable genotype–phenotype correlations makes prioritized single-gene sequencing impractical. Targeted gene panels commonly used in clinical practice are also relatively limited in their yield because new causes of JS continue to be discovered. Therefore, WES (when it becomes less expensive and more widely available) is preferable owing to its high diagnostic yield. If WES is not possible, then updated JS gene panels are preferable in most cases. The few exceptions include prioritizing TMEM67 sequencing in patients with JS with coloboma and CEP290 and AHI1 in those with severe retinal degeneration. In addition, targeted analysis of TMEM216 in Ashkenazi Jewish individuals and C5orf42 in French Canadians would be reasonable. In the absence of these phenotypic clues, prioritization of the most prevalent six JS genes (TMEM67, C5orf52, CC2D2A, CEP290, AHI1, and KIAA0586), which account for more than half of the individuals with JS in most populations, may be reasonable.
Limitations
This study was advertised to patients and families by the Joubert Syndrome & Related Disorders Foundation, which could introduce a bias for most connected and most research-focused families. Our JS cohort may be relatively enriched by patients with extraneurological issues, especially kidney and liver disease, because the comprehensive liver and kidney evaluations performed at the NIH Clinical Center may have attracted patients with these manifestations. However, our study also offered formal neurocognitive testing as well as other general investigations, including DNA sequencing, sleep studies, echocardiograms, and hormone evaluations, which may have minimized this bias. In fact, although the ratio of patients with TMEM67-related JS in our cohort was higher than that in other recently published cohorts,14,27,29 the five most commonly mutated genes in our cohort were the same as those in another large cohort.14 In addition, a weeklong evaluation is a significant time commitment, which may have led to sampling bias for families that were able to take time for a weeklong visit or selecting for patients with the most medical problems, for whom families are desperate for more information. Very severely affected patients with JS who required intensive care such as mechanical ventilation at the time of the study might be underrepresented in our study because they could not travel to Bethesda, Maryland. In addition, the overall frequency of retinal degeneration, liver disease, and kidney disease might have been underestimated in this cross-sectional study because these manifestations may develop as a patient gets older. Overall, we found potential disease-causing variants in all but five families. This may be explained by mutations in genes not yet associated with primary cilium. It is also possible that the potential disease-causing variants may not be detected by our method because it cannot detect copy-number variants and variants in noncoding parts of DNA, including deep intronic areas, intergenic regions, and some untranslated regions.
Disclosure
The authors declare no conflict of interest.
References
Joubert M, Eisenring JJ, Andermann F. Familial dysgenesis of the vermis: a syndrome of hyperventilation, abnormal eye movements and retardation. Neurology 1968;18:302–303.
Parisi M, Glass I. Joubert syndrome and related disorders. In: Pagon RA, Adam MP, Ardinger HH, et al. (eds). GeneReviews. University of Washington: Seattle, WA, 1993.
Parisi MA, Dobyns WB. Human malformations of the midbrain and hindbrain: review and proposed classification scheme. Mol Genet Metab 2003;80:36–53.
Gleeson JG, Keeler LC, Parisi MA, et al. Molar tooth sign of the midbrain-hindbrain junction: occurrence in multiple distinct syndromes. Am J Med Genet A 2004;125A:125–34; discussion 117.
Gunay-Aygun M. Liver and kidney disease in ciliopathies. Am J Med Genet C Semin Med Genet 2009;151C:296–306.
Romani M, Micalizzi A, Valente EM. Joubert syndrome: congenital cerebellar ataxia with the molar tooth. Lancet Neurol 2013;12:894–905.
Hildebrandt F, Benzing T, Katsanis N. Ciliopathies. N Engl J Med 2011;364:1533–1543.
Szymanska K, Johnson CA. The transition zone: an essential functional compartment of cilia. Cilia 2012;1:10.
Teer JK, Bonnycastle LL, Chines PS, et al.; NISC Comparative Sequencing Program. Systematic comparison of three genomic enrichment methods for massively parallel DNA sequencing. Genome Res 2010;20:1420–1431.
Hardenbol P, Banér J, Jain M, et al. Multiplexed genotyping with sequence-tagged molecular inversion probes. Nat Biotechnol 2003;21:673–678.
Porreca GJ, Zhang K, Li JB, et al. Multiplex amplification of large sets of human exons. Nat Methods 2007;4:931–936.
O’Roak BJ, Vives L, Fu W, et al. Multiplex targeted sequencing identifies recurrently mutated genes in autism spectrum disorders. Science 2012;338:1619–1622.
Shen P, Wang W, Krishnakumar S, et al. High-quality DNA sequence capture of 524 disease candidate genes. Proc Natl Acad Sci USA 2011;108:6549–6554.
Bachmann-Gagescu R, Dempsey JC, Phelps IG, et al.; University of Washington Center for Mendelian Genomics. Joubert syndrome: a model for untangling recessive disorders with extreme genetic heterogeneity. J Med Genet 2015;52:514–522.
Bentley DR, Balasubramanian S, Swerdlow HP, et al. Accurate whole human genome sequencing using reversible terminator chemistry. Nature 2008;456:53–59.
Teer JK, Mullikin JC. Exome sequencing: the sweet spot before whole genomes. Hum Mol Genet 2010;19(R2):R145–R151.
Teer JK, Green ED, Mullikin JC, Biesecker LG. VarSifter: visualizing and analyzing exome-scale sequence variation data on a desktop computer. Bioinformatics 2012;28:599–600.
Kircher M, Witten DM, Jain P, O’Roak BJ, Cooper GM, Shendure J. A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet 2014;46:310–315.
Vilboux T, Malicdan MCV, Roney J, et al. CELSR2, encoding a planar cell polarity protein, is a putative gene in Joubert syndrome with cortical heterotopia, microophthalmia, and growth hormone deficiency. Am J Med Genet A 2017. doi: 10.1002/ajmg.a.38005.
Chevrier V, Bruel AL, Van Dam TJ, et al. OFIP/KIAA0753 forms a complex with OFD1 and FOR20 at pericentriolar satellites and centrosomes and is mutated in one individual with oral-facial-digital syndrome. Hum Mol Genet 2016;25:497–513.
Srour M, Schwartzentruber J, Hamdan FF, et al.; FORGE Canada Consortium. Mutations in C5ORF42 cause Joubert syndrome in the French Canadian population. Am J Hum Genet 2012;90:693–700.
Edvardson S, Shaag A, Zenvirt S, et al. Joubert syndrome 2 (JBTS2) in Ashkenazi Jews is associated with a TMEM216 mutation. Am J Hum Genet 2010;86:93–97.
Huang L, Szymanska K, Jensen VL, et al. TMEM237 is mutated in individuals with a Joubert syndrome related disorder and expands the role of the TMEM family at the ciliary transition zone. Am J Hum Genet 2011;89:713–730.
Peng G, Fan Y, Palculict TB, et al. Rare variant detection using family-based sequencing analysis. Proc Natl Acad Sci USA 2013;110:3985–3990.
Doherty D, Parisi MA, Finn LS, et al. Mutations in 3 genes (MKS3, CC2D2A and RPGRIP1L) cause COACH syndrome (Joubert syndrome with congenital hepatic fibrosis). J Med Genet 2010;47:8–21.
Kroes HY, Monroe GR, van der Zwaag B, et al. Joubert syndrome: genotyping a Northern European patient cohort. Eur J Hum Genet 2016;24:214–220.
Saraiva JM, Baraitser M. Joubert syndrome: a review. Am J Med Genet 1992;43:726–731.
Satran D, Pierpont ME, Dobyns WB. Cerebello-oculo-renal syndromes including Arima, Senior-Löken and COACH syndromes: more than just variants of Joubert syndrome. Am J Med Genet 1999;86:459–469.
Knopp C, Rudnik-Schöneborn S, Eggermann T, et al. Syndromic ciliopathies: From single gene to multi gene analysis by SNP arrays and next generation sequencing. Mol Cell Probes 2015;29:299–307.
Acknowledgements
This work was supported in part by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health, Bethesda, Maryland, USA. D.A.D. was supported by R01NS064077; University of Washington Intellectual and Developmental Disabilities Research Center; U54HD083091 Genetics Core 6845 and sub-project 6849; and private donations from families of children with Joubert syndrome. We thank the JS patients and their families for participating in this study.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Figure S1
(TIFF 543 kb)
Supplementary Figure S2
(TIFF 390 kb)
Supplementary Figures S3
(TIFF 772 kb)
Supplementary Table S1 and S2
(DOCX 29 kb)
Supplementary Tables S3
(DOCX 344 kb)
Rights and permissions
About this article
Cite this article
Vilboux, T., Doherty, D., Glass, I. et al. Molecular genetic findings and clinical correlations in 100 patients with Joubert syndrome and related disorders prospectively evaluated at a single center. Genet Med 19, 875–882 (2017). https://doi.org/10.1038/gim.2016.204
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2016.204
Keywords
This article is cited by
-
Mutations in the NUP93, NUP107 and NUP160 genes cause steroid-resistant nephrotic syndrome in Chinese children
Italian Journal of Pediatrics (2024)
-
Ocular manifestations of renal ciliopathies
Pediatric Nephrology (2024)
-
The genetic spectrum of congenital ocular motor apraxia type Cogan: an observational study, continued
Orphanet Journal of Rare Diseases (2023)
-
Molecular investigation in individuals with orofacial clefts and microphthalmia-anophthalmia-coloboma spectrum
European Journal of Human Genetics (2023)
-
Biallelic CC2D2A variants, SNV and LINE-1 insertion simultaneously identified in siblings using long-read whole-genome sequencing and haplotype phasing
Journal of Human Genetics (2023)