Abstract
Aberrant activation of hepatocyte growth factor/scatter factor (HGF/SF) and its receptor, Met, is involved in the development and progression of many human cancers. In the cell-based screening assay, (-)epigallocatechin-3-gallate (EGCG) inhibited HGF/SF-Met signaling as indicated by its inhibitory activity on HGF/SF-induced cell scattering and uPA activation (IC50 = 15.8 µg/ml). Further analysis revealed that EGCG at low doses specifically inhibited HGF/SF-induced tyrosine phosphorylation of Met but not epidermal growth factor (EGF)-induced phosphorylation of EGF receptor (EGFR). On the other hand, high-dose EGCG decreased both Met and EGFR proteins. We also found that EGCG did not act on the intracellular portion of Met receptor tyrosine kinase, i.e., it inhibited InlB-dependent activation of Met but not NGF-induced activation of Trk-Met hybrid receptor. This inhibition decreased HGF-induced migration and invasion by parental or HGF/SF-transfected B16F10 melanoma cells in vitro in either a paracrine or autocrine manner. Furthermore, EGCG inhibited the invasion/metastasis of HGF/SF-transfected B16F10 melanoma cells in mice. Our data suggest the possible use of EGCG in human cancers associated with dysregulated paracrine or autocrine HGF/SF-Met signaling.
Similar content being viewed by others
Introduction
The c-met protooncogene encodes a transmembrane glycoprotein, Met tyrosine kinase receptor (Naldini et al., 1991; Park et al., 1999), and the ligand for Met is hepatocyte growth factor, also known as scatter factor (HGF/SF) (Bottaro et al., 1991). Both Met and HGF/SF are expressed in various tissues and signaling via this receptor-ligand pair affects a variety of biological activities, including cell growth (Nakamura et al., 1986), cellular motility (Stoker et al., 1987), angiogenesis (Bussolino et al., 1992), and morphogenesis (Tsarfaty et al., 1992).
In addition, aberrant signaling driven by inappropriate activation of Met is frequently observed in human cancers and has been suggested to play a critical role in human tumorigenesis and metastasis (Jeffers et al., 1996). Most cases of Met activation in cancer have been reported to occur through ligand-dependent autocrine or paracrine mechanisms. For instance, osteosarcomas and glioblastoma multiforme express both Met and HGF/SF, which results in Met activation in an autocrine manner. In many types of carcinoma, such as breast, gastric and colorectal cancers, overexpression of Met or HGF/SF predominates, resulting in the activation of HGF/SF-Met signaling in a paracrine manner (Jeffers et al., 1996; Birchmeier et al., 1997). Recently, the finding of activating mutants of Met in several human cancers such as renal papillary cancer (Schmidt et al., 1997), early-onset hepatoma (Park et al., 1999) and gastric adenocarcinoma (Lee et al., 2000) provides clear evidence implicating a causative role for Met in human carcinogenesis. Furthermore, HGF/SF-Met signaling has been reported to participate in tumor progression (Jiang et al., 2005).
Therefore, molecules that inhibit Met and/or HGF/SF may interfere with molecular causes of cancer formation and/or progression (Michieli et al., 2004). In this regard, many efforts have been directed toward the development of inhibitors of HGF/SF and Met (Michieli et al., 2004). Herbal extracts are promising starting materials in the search for effective molecules. For example, polyphenols derived from green tea are effective chemopreventive agents. (-)-Epigallocatechin-3-gallate (EGCG) is the major bioactive polyphenol in green tea. It possesses anti-oxidant, anti-mutagenic, anti-proteolytic, and anti-proliferative activity (Sah et al., 2004). Interestingly, EGCG has been reported to inhibit EGF-dependent signaling (Sah et al., 2004) and platelet-derived growth factor signaling (Chen et al., 2003; Sakata et al., 2004; Weber et al., 2004), as well as VEGF-dependent signaling (Lamy et al., 2002; Lee et al., 2004).
In the present study, we demonstrate that EGCG inhibits HGF/SF-Met signaling by decreasing the amount of tyrosine phosphorylation, probably by acting on the extracellular and/or transmembrane portions of Met receptor tyrosine kinase. This inhibition decreases HGF-induced migration and invasion both in vitro and in vivo, suggesting the possible use of EGCG in human cancers with dysregulated HGF/SF-Met signaling.
Results
EGCG inhibdite the HGF/SF-Met-uPA-Plasmin proteolytic network and HGF/SF-induced cell scattering
While searching an herbal extract library obtained from Plant Extract Bank (Daejon, Korea) for a small molecule inhibitor of HGF/SF-Met signaling, we observed that the water extract of green tea efficiently blocked the HGF/SF-induced activation of uPA (Figure 1A, left panel). Since EGCG is the major known bioactive polyphenol in green tea, we investigated whether EGCG inhibited HGF/Met signaling. Indeed, EGCG inhibited HGF/SF-dependent plasmin activation in a dose-dependent manner, whereas it displayed only minimal cytotoxicity at concentrations at which significant inhibition of HGF-mediated plasmin activation was apparent (Figure 1A, right panel). The IC50 value for EGCG was 15.8 µg/ml (Figure 1B). During the plasmin assay, we clearly observed potent inhibitory activity by EGCG in HGF/SF-mediated MDCK2 cell scattering (Figure 1C). Since scattering of MDCK2 cells is not dependent on the uPA-plasmin, the inhibition of HGF/SF-mediated scattering by EGCG suggests that EGCG acts at the HGF/SF-Met level but not at the uPA-plasmin level of signaling.
EGCG inhibited the HGF/SF-Met-uPA-Plasmin network and HGF/SF-induced scattering. (A) Inhibition of HGF/SF-induced uPA activation. MDCK2 cells were used for a cell-based screening assay as described in Materials and Methods. Indicated concentrations of water extract of green tea (left panel) or EGCG (right panel) were applied to the system in triplicate for 24 h. uPA activity was measured by colorimetry, and the protein amount was measured using SRB assay. Values are either the absorbance at 405nm (for plasmin activity) or the percent of vehicle control (for SRB assay). *denotes statistical significance (P < 0.05) compared to vehicle control. (B) The IC50 value for EGCG was 15.8 µg/ml. Plasmin assay was performed and the data were normalized to the SRB assay. The percent of vehicle control was plotted, and the IC50 value was calculated. (C). EGCG inhibited HGF-induced cell scattering. The cells in the plasmin assay were observed under the phase-contrast microscope. Note the inhibitory activity of EGCG against HGF-mediated MDCK2 cell scattering.
Inhibition by EGCG stemmed from its action on Met phosphorylation and Met expression
We used human Chang liver cells to investigate whether EGCG influences the tyrosine phosphorylation of Met protein because canine Met protein in MDCK2 cells was not clearly detected with available antibodies. The phosphorylation of tyrosine residues in Met by HGF/SF was inhibited by EGCG at concentration as low as 1 µg/ml, which was quite evident at a concentration of 5 µg/ml (Figure 2A). In contrast, the level of EGF-induced tyrosine phosphorylation of EGFR remained relatively unchanged by EGCG administration up to 5 µg/ml (Figure 2C), suggesting the decreased tyrosine phosphorylation with EGCG was specific for HGF/SF-Met signaling. Notably, the amount of both Met protein and EGFR (Figure 2A, C) decreased with 25 µg/ml EGCG but not at lower concentrations as shown by both immunoprecipitation-western analysis (Figure 2A) and simple western analysis (Figure 2B). Thus dual mechanisms seem to be involved in EGCG inhibition of HGF/SF-Met signaling, i.e., Met-specific inhibition of tyrosine phosphorylation at low dose and non-specific inhibition of protein expression at high dose.
Inhibition by EGCG stemmed from its action on Met phosphorylation and Met expression. (A) HGF/SF-induced Met phosphorylation was inhibited by EGCG. Human Chang liver cells were seeded at a density of 1 × 106 cells/100 mm plate in complete medium for 18 h, and then incubated in DMEM containing 0.5% FBS for 24 h. EGCG was added to the media 2 h before the addition of HGF/SF (100 units/ml). Eight minutes after the treatment, cells were harvested, and the lysates were subjected to immunoprecipitation by anti-Met antibody followed by western blotting using anti-phosphotyrosine antibody (upper panel) and anti-Met antibody (lower panel). (B) The amount of Met protein decreased with high-dose EGCG. Cell lysates obtained as in (A) were subjected to SDS-PAGE, followed by western blotting using anti-Met antibody (upper panel). Actin was measured as a loading control. (C) Effect of EGCG on EGFR signaling. Cell lysates obtained as in (A) after treatment with EGF were subjected to immunoprecipitation by anti-EGFR antibody followed by western blotting using anti-phosphotyrosine antibody (upper panel) and anti-EGFR antibody (lower panel).
EGCG did not act on the intracellular part of Met
To more precisely understand the mode of action of EGCG on HGF/SF-Met signaling, we used InlB, the only known ligand of Met other than HGF/SF (Shen et al., 2000). We checked whether EGCG could inhibit InlB-induced Met activation. As shown in Figure 3A, EGCG clearly inhibited InlB-induced tyrosine phosphorylation of Met. Since HGF/SF and InlB bind to different portions of Met (Shen et al., 2000), these results suggest that EGCG acts on Met receptor itself rather than on the binding of HGF/SF and Met.
EGCG did not act on the intracellular part of Met. (A) EGCG inhibited InlB-induced Met activation and its down-stream signaling. Human Chang liver cells were treated and subjected to immunoprecipitation-western blotting as described in Figure 2a except that recombinant InlB (160 ng/ml) was used instead of HGF/SF. (B) EGCG could not inhibit NGF-induced Trk-Met signaling. NIH3T3 cells expressing Trk-Met hybrid receptor were pre-treated with EGCG and then treated with NGF (100 ng/ml).
Trk-Met is a hybrid receptor that consists of the extracellular part of Trk, the NGF receptor, and the intracellular part of Met (Sachs et al., 1996). Trk-Met receptor is activated by NGF, but not by HGF/SF, and its signaling resembles that of Met receptor kinase, but not of Trk. To determine whether the intracellular or extracellular part of Met is the target of EGCG, we investigated whether EGCG could inhibit NGF-induced Trk-Met activation. Since we failed to immunoprecipitate Trk-Met protein due to the unavailability of suitable antibody, we examined downstream of Trk-Met signaling, the Erk phosphorylation. As shown in Figure 3B, EGCG did not abolish the downstream ERK phosphorylation at the dose (5 µg/ml) that effectively blocked the activities of both HGF/SF and InlB. However, at higher doses, a non-specific decrease in protein expression was observed (data not shown). This observation, along with the ineffectiveness of EGCG against endogenous NGF receptor signaling (data not shown), strongly suggests that EGCG does not act on the intracellular part of Trk-Met, i.e., the intracellular part of Met.
EGCG inhibited HGF/SF-mediated in vitro cell motility and invasion.
Since dysregulated HGF/SF-Met signaling is one of the principal changes not only in tumorigenesis but also in tumor progression, we tested the ability of EGCG to inhibit HGF/SF-mediated motility and invasion in vitro. In order to take advantage of the syngeneic property of the tumor cells for later in vivo assays, we performed each assay with C57BL/6 mouse-derived B16F10 melanoma cells. The HGF/SF-Met signaling in B16F10 melanoma cells was also inhibited by EGCG (Supplementary Figure S1). As shown in Figure 4A, HGF/SF-induced migration of the cells in the "scratch wound assay" was clearly abolished by EGCG in a dose-dependent manner. We used HGF/SF at a concentration of 50 units/ml, which was much higher than that used in the uPA assay, and found that EGCG still effectively inhibited HGF/SF activity. The effect of EGCG on cell proliferation was negligible both with and without HGF/SF (Supplementary Figure S2A). We also tested the ability of EGCG to inhibit HGF/SF-mediated invasion of B16F10 melanoma cells across Matrigel-coated 8-µm pore filters (Fig. 4B). EGCG inhibited HGF/SF-mediated invasion of B16F10 cells at concentrations as low as 1 µg/ml in a dose-dependent manner. Although EGCG inhibited the proliferation of B16F10 melanoma cells irrespective of the presence of HGF under serum-free experimental conditions (Supplementary Figure S2B), when the invading cell number was corrected for the cell proliferation rate as shown in Figure 4B, the inhibitory activity of EGCG was still evident. These data demonstrate that EGCG is a potent inhibitor of HGF/SF-mediated cell motility and invasion in vitro.
EGCG inhibited HGF/SF-mediated cell migration and invasion. (A) Inhibition of HGF/SF-induced cell migration. B16F10 murine melanoma cells were seeded at a density of 20,000 cells/well in 24-well plates and cultured for 48 h. Confluent cells were scratched with a 1-ml micropipette tip, and fresh media containing the indicated concentrations of EGCG were added 2 h before the treatment with or without HGF (50 units/ml). After 28 h, cells were photographed under a phase-contrast microscope. (B) Inhibition of HGF/SF-mediated invasion. Transwell filters were coated with Matrigel (20 µg/filter) before the application of cells at a density of 20,000 cells/filter. EGCG was added at the indicated concentrations in both the upper and lower chambers 2 h before the addition of HGF (50 units/ml) to both chambers. After 48 h, filters were processed as described in Materials and Methods. Invading cells were counted under light microscope. Cell proliferation rate under the same conditions was measured and used to correct the invading cell number as follows: corrected cell number = number of cells counted/relative ratio of cell population compared to that without EGCG.
HGF/SF-secreting B16F10 cells were highly metastatic
To obtain constitutive stimulation by HGF/SF for a long-term in vivo assay, B16F10 cells were transfected with HGF cDNA and a stable clone with HGF/SF-Met autocrine signaling (C2 cells hereafter) was established. HGF/SF mRNA was detected in C2 cells but not in parental B16F10 cells (Figure 5B). As expected, the conditioned medium of C2 cells induced more MDCK cell scattering than HGF/SF (2.5 units/ml), whereas the conditioned medium of parental B16F10 cells induced negligible scattering as shown in Figure 5A. As shown in Figure 5B, C2 cells showed higher invasion through Matrigel-coated filter than HGF-treated parental B16F10 cells, indicative of their highly invasive and metastatic properties. Indeed, C2 cells revealed higher metastatic ability than parental B16F10 cells in tail vein metastasis assays performed in syngeneic C57BL6 mice (Supplementary Table 1).
C2 cells secreted functional HGF/SF and showed high invasive capacity. To obtain continuous stimulation by HGF/SF in vivo, B16F10 cells transfected with HGF cDNA (C2 cells) were established and characterized. (A) Secretion of functional HGF/SF from C2 cells. MDCK2 cells were grown to 1/3 confluence. Culture media were replaced by new media as indicated. After 24 h, the cells were observed under the phase-contrast microscope. Note the higher scattering activity of conditioned medium from C2 cells than that of HGF/SF at a concentration of 2.5 U/ml. (B) Transwell filters were coated with Matrigel (20 µg/filter) before the application of cells at a density of 20,000 cells/filter. HGF/SF (50 units/ml) was applied to B16F10 cells in both the upper and lower chambers. After 48 h, invading cells were counted under light microscope. Cell proliferation rate under the same conditions was measured and used to correct the invading cell number as follows: corrected cell number = number of invading cells/relative ratio of cell population compared to that without HGF/SF. Note the higher invasion of C2 cells compared to B16F10 cells with HGF/SF treatment. Inset figure shows the expression of HGF/SF mRNA by RT-PCR. RV HGF means HGF cDNA in retroviral vector, which was used as a positive control.
EGCG inhibited metastasis of autocrine C2 cells in vivo
To assess whether autocrine HGF/SF-Met signaling was also abolished by EGCG, in vitro migration and invasion assays were performed using C2 cells and different concentrations of EGCG. As shown in Figure 6A, migration of C2 cells in a "scratch wound" assay was inhibited by EGCG in a dose-dependent manner. Similarly, invasion of C2 cells through Matrigel-coated membrane was also dose-dependently inhibited by EGCG after correcting for cell number (Figure 6B), showing that EGCG also works in cells with Met signaling activated in autocrine manner.
EGCG inhibited migration and invasion of cells with autocrine HGF/SF-stimulation. (A) C2 cells with autocrine HGF/SF-Met signaling were seeded at a density of 20,000 cells/well in 24-well plates and cultured for 48 h. Confluent cells were scratched with a 1-ml micropipette tip, and fresh media containing the indicated concentrations of EGCG were added. After 28h, cells were photographed under a phase-contrast microscope. (B) Transwell filters were coated with Matrigel (20 µg/filter) before the application of C2 cells at a density of 20,000 cells/filter. EGCG was added at the indicated concentrations to both upper and lower chambers. After 48h, invading cells were counted under light microscope. Cell proliferation rate under the same conditions was measured and used to correct the invading cell number as follows: corrected cell number = number of cells counted/relative ratio of cell population compared to that without EGCG.
Syngeneic C5BL6 mice were used for in vivo tumorigenesis and spontaneous metastasis assays. Interestingly, as shown in Table 1, EGCG significantly blocked invasion or metastasis while it blocked tumor formation considerably but not statistically significantly in the subcutaneous inoculation model. These in vivo data were consistent with the in vitro data that the anti-migration/anti-invasive activity of EGCG was relatively stronger than its anti-proliferative activity. In addition, it is possible that the observed anti-metastatic activity of EGCG partly stemmed from its anti-proliferative effect in vivo. These data demonstrate that EGCG is a potent inhibitor of invasion and metastasis of cells with constitutively activated HGF/SF-Met signaling in an autocrine manner; such cells are frequently encountered in clinical situations such as osteosarcoma and glioblastoma multiforme.
Taken together, our data demonstrate that EGCG inhibits HGF/SF-Met signaling through its effect on either the extracellular or transmembrane portion of Met and that this inhibition is applicable to both autocrine and paracrine activation of HGF/SF-Met signaling, which leads to inhibition of HGF/SF-induced cancer cell migration and invasion both in vitro and in vivo.
Discussion
Activation of HGF/SF-Met signaling has been observed in a variety of human cancers. Various approaches to inhibit HGF/SF-Met signaling in experimental systems have included neutralizing anti-HGF/SF monoclonal antibodies (Cao et al., 2001), ribozyme against HGF/SF or Met (Abounader et al., 1999, 2002), and HGF/SF variants that inhibit the binding of HGF/SF to Met (Guerin et al., 2000; Brockmann et al., 2003). In addition, there have been attempts to inhibit the tyrosine kinase activity of Met with small molecule inhibitors selected from chemical libraries (Christensen et al., 2003; Sattler et al., 2003; Wang et al., 2004). However, small molecule inhibitors from chemical libraries have their own limitations in that there are possible unpredictable toxicity problems (Michieli et al., 2004). As one of the possible ways to by-pass the toxicity problems, we focused on extracts from edible plants and the known small molecules found in them. Through the use of uPA-plasmin assay, we found that EGCG, a well-known major bioactive polyphenol in green tea, had a significant inhibitory effect on HGF/SF-Met signaling. EGCG has been well documented for its potential use in treating human diseases, and many pre-clinical and some clinical studies have already been performed. Moyers and Kumar have reviewed those trials and concluded that the preclinical research was promising and EGCG should be further studied in phase II and III trials (Moyers and Kumar, 2004). Thus, EGCG may be readily applicable to phase II clinical trial once its new activity like the one described here is confirmed.
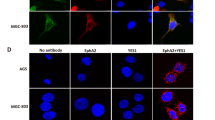
There are basically three known modes of activation of HGF/SF-Met signaling in human cancer (Liu et al., 2008). Autocrine activation is frequently observed in sarcomas, paracrine activation is usually observed in carcinomas, and the constitutively activating mutation of Met is found in a small number of carcinomas such as renal papillary cancer and early-onset hepatocellular carcinoma. Since EGCG inhibits both autocrine and paracrine activation of HGF/SF-Met signaling, we further addressed whether it was effective against the activating Met mutant in the absence of ligand. In the case of the activating mutant of Met, decreased protein levels at high concentrations of EGCG, but not decreased phosphotyrosine levels at low concentrations of EGCG, were observed (data not shown). Therefore, EGCG seems to be effective against two of the three modes of HGF/SF-Met activation, strongly suggesting its broad applicability for human cancers showing activation of HGF/SF-Met signaling. The inability of EGCG to inhibit the activating mutant of Met in the absence of HGF/SF is consistent with our observation that EGCG does not act on the cytoplasmic portion of Met (Figure 3B).
EGCG reportedly inhibits the activity of some growth factor receptors, including EGF receptor and its downstream kinases, AKT and ERK (Sah et al., 2004), as well as bFGF receptor (Sartippour et al., 2002) and VEGF receptor (Rodriguez et al., 2006). Sah et al. also found that EGCG directly inhibits the kinase activity of AKT and ERK in a cell-free system after EGF stimulation and suggested that EGCG could function at multiple sites to block signaling pathways (Sah et al., 2004). Also, EGCG is reported to inhibit VEGF receptor signaling by disrupting the formation of a receptor complex (Rodriguez et al., 2006). The underlying mechanism for the inhibitory activity of EGCG on HGF/SF-Met signaling is not clear yet. However, EGCG appears to have a 'dual' inhibitory mechanism, i.e., HGF/SF-Met-specific down-regulation of tyrosine phosphorylation at lower doses and nonspecific protein down-regulation at higher doses (Figure 2). As for the decrease in the amount of receptors in the presence of EGCG, EGCG has been reported to highly associate with lipid rafts on the plasma membrane, leading to down-regulation of IgE receptor in human basophilic KU812 cells (Fujimura et al., 2004). Whether the decrease in the amount of both EGFR and Met proteins in our system stems from the association of EGCG with lipid rafts or not remains to be clarified.
We took advantage of InlB-induced Met phosphorylation and NGF-induced Trk-Met phosphorylation to dissect the action of EGCG on HGF/SF-Met signaling. Interestingly, EGCG acts on the extracellular and/or transmembrane portion of Met receptor. We do not know the precise mode of action of EGCG: whether it inhibits ligand-receptor binding or induces a conformational change of the receptor after ligand binding. Since InlB binds to a different part of Met than HGF/SF (Shen et al., 2000), our data showing that EGCG effectively inhibits both HGF/SF- and InlB-induced Met activation suggests the latter possibility.
In this report, EGCG blocked invasion and metastasis clearer than tumor formation in the subcutaneous inoculation model (Table 1). HGF/SF-Met signaling appears to be involved in the early stages of cancer development, including the initiation phase of carcinogenesis. However, some studies imply that HGF/SF is more involved in the later stage of cancer, i.e., its spread and progression, by directly and/or indirectly stimulating invasion and metastasis processes as well as angiogenesis (Jiang et al., 2005). In line with the above implication, as shown in Figure 4, the effect of HGF/SF on the extent of B16F10 cell invasion was quite prominent, whereas its effect on cell proliferation was minimal. These in vitro data might explain why treatment with EGCG effectively blocked tumor invasion and metastasis but not tumorigenesis itself in nude mouse.
Bigelow et al., also addressed whether EGCG affects HGF/SF-Met signaling. Using breast cancer cells, the authors showed the inhibitory activity of EGCG against HGF/SF-induced activation of Met as well as its downstream signals (Bigelow et al., 2006). They also showed inhibitory activity of EGCG against HGF/SF-induced in vitro cell migration and invasion. The authors' data corroborate well with ours. Here, we additionally showed the effect of EGCG on HGF/SF-induced tumorigenesis and tumor progression in vivo. Furthermore, the effect of EGCG on different modes of activation of HGF/SF-Met signaling, as well as the mechanistic insight that EGCG works on either an extracellular or transmembrane part of Met, were addressed here. Our data strengthen the possibility of using EGCG to treat human cancers associated with dysregulated HGF/SF-Met signaling in either a paracrine or an autocrine manner.
Methods
Cell lines
MDCK2, Chang liver, B16F10 murine melanoma cells were obtained from the American Type Culture Collection (ATCC) and cultured in DMEM (Gibco-BRL, Rockville, MD) supplemented with 10% (V/V) fetal bovine serum (FBS) (Gibco-BRL). None of these cells appeared to produce HGF when tested by scattering assay (data not shown).
Reagents, antibodies, and constructs
All reagents used were obtained from Sigma (Saint Louis, MO). Rabbit anti-human Met antibody (C28) and mouse anti-murine Met antibody (B2) were purchased from Santa Cruz (Santa Cruz, CA). Mouse anti-phosphotyrosine antibody (PY20) was purchased from Invitrogen (Carlsbad, CA). Mouse anti-EGFR antibody was from BD Sciences (San Jose, CA); rabbit anti-p44/42 MAPK antibody and anti-phospho p44/42 MAPK antibody were from Cell Signaling (Danver, MA). Recombinant human EGF was obtained from BD biosciences (San Jose, CA). Recombinant human HGF and neutralizing antibody for HGF were purchased from R&D systems (Minneapolis, MN). Recombinant InlB protein was purified as described (Shen et al., 2000) from E.coli transformed with InlB cDNA (kindly provided by Dr. Ireton, University of Toronto, Canada). Purity of the recombinant protein was checked by protein staining of SDS-PAGE gel, and revealed to be > 90% (data not shown). Both Trk-Met vector (Sachs et al., 1996) and HGF expression vector which contains the human HGF cDNA in pMex vector were generous gifts from Dr. Vande Woude (Van Andel Institute, Grand Rapids, MI).
Transfection and screening
Transfection of HGF or Trk-Met construct and screening was performed as described previously (Baek et al., 2004) by using lipofectamine (Gibco-BRL). The transfected cells were cultured in DMEM/10% FBS supplemented with 800 µg/ml G-418 (Gibco-BRL) for two weeks. Expression of transfected cDNAs were verified by RT-PCR, and in case of HGF, by MDCK2 scattering assay.
Immunoprecipitation
Monolayers of cells were washed twice with ice-cold PBS, lysed in ice-cold RIPA buffer [10 mM sodium phosphate (pH7.2), 150 mM NaCl, 1% (V/V) Nonidet P-40, 0.1% (W/V) SDS supplemented with 10mM sodium fluoride, 5 mM sodium orthovanadate] with complete protease inhibitor cocktail (Boehringer Mannheim, Germany), and centrifuged (15 min, 4℃, 14,000 g). After quantitation by using BCA protein assay reagent (Pierce, Rockford, IL), 400 µg of each lysate was pre-cleared with protein A/G-Sepharose and then incubated with anti-Met antibody (C28 or B2) and protein A/G-Sepharose for overnight at 4℃ with rotation. The samples were then washed three times with ice-cold RIPA buffer. SDS gel-loading buffer (containing reducing agent) was added to each sample. After boiling and centrifugation, the resulting supernatants were resolved by SDS/PAGE and examined by Western blotting.
Cell proliferation
Cells were plated at low density and cultivated in normal growth medium in the presence or absence of EGCG at different concentrations. Cell proliferation was evaluated at indicated times by cell counting.
Colorimetric assay for uPA activity
uPA activity was measured as described (Webb et al., 2000) with slight modifications. Briefly, MDCK-2 cells were seeded at a density of 1500 cells/well of a 96-well microtiter plate and grown overnight in DMEM/10% FBS. Duplicate plates were made for the determination of plasmin activation and cell growth. Different concentrations of EGCG in DMEM/10% FBS media were added to the wells. Two h after EGCG administration, HGF (2.5 units/ml) was added to all wells (with the exception of wells used to calculate basal growth and plasmin activation). Twenty-four h after HGF addition, one of two duplicate plates was processed for the determination of plasmin activity by incubating at 37℃, 5% CO2 for 3 h in 200 µl of reaction buffer [50% (v/v) 0.05 units/ml plasminogen (Roche, Germany) in DMEM (without phenol red), 40% (v/v) 50 mM Tris buffer (pH 8.2), and 10% (v/v) 3 mM Chromozyme PL (Roche, Germany) in 100 mM glycine solution] at each well. The absorbances were read on an automated spectrophotometric plate reader at a single wavelength of 405 nm. The determination of cell growth on a duplicate plate was performed by measuring SRB staining of cellular proteins as described (Webb et al., 2000). Plasmin activation (A405 nm) was normalized for the amount of protein in each well.
Cell scattering assay
During the colorimetric assay for uPA activity, inhibition of the scattering induced by HGF/SF was assessed by microscopic observation. The degree of cell scattering inhibition was semiquantitatively scored by two independent researchers.
Scratch assay
B16F10 murine melanoma cells were seeded in a 24-well plate in normal growth medium. After 48 h, cells were scratched using a micropipette tip and EGCG was added at the indicated wells. Two hours later, HGF was treated to indicated wells. After additional incubation for 28 h, wells were observed under the light microscope.
Invasion assay
Cell invasion assays were performed using 24-well transwell units with 8-mm polycarbonate filters (Costar). Briefly, 2 × 104 cells (in 100 ml DMEM+1% BSA with or without EGCG) were plated onto the upper surface of the filter previously coated with Matrigel at a concentration of 20 mg/filter (BD Biosciences). The filter was then lowered into the lower compartment containing DMEM+1% BSA with or without recombinant human HGF/SF (50 units/ml) with the indicated concentration of EGCG. After 48 h of incubation at 37℃/5% CO2, cells were fixed in methanol and stained with Diff-Quick staining solution (Dade, Aguada, Puerto Rico). Non-migratory cells on the upper filter surface were removed using a cotton swab, and the total number of cells on each filter was counted at × 200 magnification using a phase-contrast microscope accommodated with an ocular grid. Cell proliferation at the same condition was monitored to compensate the effect of the difference in cell proliferation during the assay.
In vivo tumorigenesis and metastasis assay
B16F10 melanoma cells were used in this assay since it was originated from C57BL/6 mice. B16F10 melanoma cells expressing HGF (C2 cells) were generated as described above. Two hundred and fifty thousand cells were inoculated subcutaneously into 8-week-old female syngenic C57BL/6 mice. The mice were divided into two groups and injected intraperitoneally 6 times a week for 2 weeks with EGCG (1 mg/head) or saline, respectively. The size of the tumor nodules was measured twice weekly. Two weeks after inoculation, mice were sacrificed, and the tumor was excised and measured by weight. At the same time, metastasis into different organs was assessed by simple observation, which is possible due to the production of melanin pigment by the cells.
Abbreviations
- EGCG:
-
(-)-epigallocatechin-3-gallate
- HGF/SF:
-
hepatocyte growth factor/scatter factor
- uPA:
-
urokinase plasminogen activator
- InlB:
-
internalin B
References
Abounader R, Ranganathan S, Lal B, Fielding K, Book A, Dietz H, Burger P, Laterra J . Reversion of human glioblastoma malignancy by U1 small nuclear RNA/ribozyme targeting of scatter factor/hepatocyte growth factor and c-met expression . J Natl Cancer Inst 1999 ; 91 : 1548 - 1556
Abounader R, Lal B, Luddy C, Koe G, Davidson B, Rosen EM, Laterra J . In vivo targeting of SF/HGF and c-met expression via U1snRNA/ribozymes inhibits glioma growth and angiogenesis and promotes apoptosis . FASEB J 2002 ; 16 : 108 - 110
Baek CM, Jeon SH, Jang JJ, Lee BS, Lee JH . Transforming variant of Met receptor confers serum independence and anti-apoptotic property and could be involved in the mouse thymic lymphomagenesis . Exp Mol Med 2004 ; 36 : 283 - 291
Bigelow RL, Cardelli JA . The green tea catechins, (-)-Epigallocatechin-3-gallate (EGCG) and (-)-Epicatechin-3-gallate (ECG), inhibit HGF/Met signaling in immortalized and tumorigenic breast epithelial cells . Oncogene 2006 ; 25 : 1922 - 1930
Birchmeier W, Brinkmann V, Niemann C, Meiners S, DiCesare S, Naundorf H, Sachs M . Role of HGF/SF and c-Met in morphogenesis and metastasis of epithelial cells . Ciba Found Symp 1997 ; 212 : 230 - 240
Bottaro DP, Rubin JS, Faletto DL, Chan AM, Kmiecik TE, Vande Woude GF, Aaronson SA . Identification of the hepatocyte growth factor receptor as the c-met proto-oncogene product . Science 1991 ; 251 : 802 - 804
Brockmann MA, Papadimitriou A, Brandt M, Fillbrandt R, Westphal M, Lamszus K . Inhibition of intracerebral glioblastoma growth by local treatment with the scatter factor/hepatocyte growth factor-antagonist NK4 . Clin Cancer Res 2003 ; 9 : 4578 - 4585
Bussolino F, Di Renzo MF, Ziche M, Bocchietto E, Olivero M, Naldini L, Gaudino G, Tamagnone L, Coffer A, Comoglio PM . Hepatocyte growth factor is a potent angiogenic factor which stimulates endothelial cell motility and growth . J Cell Biol 1992 ; 119 : 629 - 641
Cao B, Su Y, Oskarsson M, Zhao P, Kort EJ, Fisher RJ, Wang LM, Vande Woude GF . Neutralizing monoclonal antibodies to hepatocyte growth factor/scatter factor (HGF/SF) display antitumor activity in animal models . Proc Natl Acad Sci USA 2001 ; 98 : 7443 - 7448
Chen A, Zhang L . The antioxidant (-)-epigallocatechin-3-gallate inhibits rat hepatic stellate cell proliferation in vitro by blocking the tyrosine phosphorylation and reducing the gene expression of platelet-derived growth factor-beta receptor . J Biol Chem 2003 ; 278 : 23381 - 23389
Christensen JG, Schreck R, Burrows J, Kuruganti P, Chan E, Le P, Chen J, Wang X, Ruslim L, Blake R, Lipson KE, Ramphal J . A selective small molecule inhibitor of c-Met kinase inhibits c-Met-dependent phenotypes in vitro and exhibits cytoreductive antitumor activity in vivo . Cancer Res 2003 ; 63 : 7345 - 7355
Fujimura Y, Tachibana H, Yamada K . Lipid raft-associated catechin suppresses the FcepsilonRI expression by inhibiting phosphorylation of the extracellular signal-regulated kinase1/2 . FEBS Lett 2004 ; 556 : 204 - 210
Guerin C, Luddy C, Abounader R, Lal B, Laterra J . Glioma inhibition by HGF/NK2, an antagonist of scatter factor/hepatocyte growth factor . Biochem Biophys Res Commun 2000 ; 273 : 287 - 293
Jeffers M, Rong S, Woude GF . Hepatocyte growth factor/scatter factor-Met signaling in tumorigenicity and invasion/metastasis . J Mol Med 1996 ; 74 : 505 - 513
Jiang WG, Martin TA, Parr C, Davies G, Matsumoto K, Nakamura T . Hepatocyte growth factor, its receptor, and their potential value in cancer therapies . Crit Rev Oncol Hematol 2005 ; 53 : 35 - 69
Lamy S, Gingras D, Beliveau R . Green tea catechins inhibit vascular endothelial growth factor receptor phosphorylation . Cancer Res 2002 ; 62 : 381 - 385
Lee JH, Han SU, Cho H, Jennings B, Gerrard B, Dean M, Schmidt L, Zbar B, Vande Woude GF . A novel germ line juxtamembrane Met mutation in human gastric cancer . Oncogene 2000 ; 19 : 4947 - 4953
Lee YK, Bone ND, Strege AK, Shanafelt TD, Jelinek DF, Kay NE . VEGF receptor phosphorylation status and apoptosis ismodulated by a green tea component, epigallocatechin-3-gallate (EGCG), in B-cell chronic lymphocytic leukemia . Blood 2004 ; 104 : 788 - 794
Liu X, Yao W, Newton RC, Scherle PA . Targeting the c-MET signaling pathway for cancer therapy . Expert Opin Investig Drugs 2008 ; 17 : 997 - 1011
Michieli P, Mazzone M, Basilico C, Cavassa S, Sottile A, Naldini L, Comoglio PM . Targeting the tumor and its microenvironment by a dual-function decoy Met receptor . Cancer Cell 2004 ; 6 : 61 - 73
Moyers SB, Kumar NB . Green tea polyphenols and cancer chemoprevention: multiple mechanisms and endpoints for phase II trials . Nutr Rev 2004 ; 62 : 204 - 211
Nakamura T, Teramoto H, Ichihara A . Purification and characterization of a growth factor from rat platelets for mature parenchymal hepatocytes in primary cultures . Proc Natl Acad Sci USA 1986 ; 83 : 6489 - 6493
Naldini L, Vigna E, Ferracini R, Longati P, Gandino L, Prat M, Comoglio PM . The tyrosine kinase encoded by the MET proto-oncogene is activated by autophosphorylation . Mol Cell Biol 1991 ; 11 : 1793 - 1803
Park WS, Dong SM, Kim SY, Na EY, Shin MS, Pi JH, Kim BJ, Bae JH, Hong YK, Lee KS, Lee SH, Yoo NJ . Somatic mutations in the kinase domain of the Met/hepatocyte growth factor receptor gene in childhood hepatocellular carcinomas . Cancer Res 1999 ; 59 : 307 - 310
Rodriguez SK, Guo W, Liu L, Band MA, Paulson EK, Meydani M . Green tea catechin, epigallocatechin-3-gallate, inhibits vascular endothelial growth factor angiogenic signaling by disrupting the formation of a receptor complex . Int J Cancer 2006 ; 118 : 1635 - 1644
Sachs M, Weidner KM, Brinkmann V, Walther I, Obermeier A, Ullrich A, Birchmeier W . Motogenic and morphogenic activity of epithelial receptor tyrosine kinases . J Cell Biol 1996 ; 133 : 1095 - 1107
Sah JF, Balasubramanian S, Eckert RL, Rorke EA . Epigallocatechin-3-gallate inhibits epidermal growth factor receptor signaling pathway. Evidence for direct inhibition of ERK1/2 and AKT kinases . J Biol Chem 2004 ; 279 : 12755 - 12762
Sakata R, Ueno T, Nakamura T, Sakamoto M, Torimura T, Sata M . Green tea polyphenol epigallocatechin-3-gallate inhibits platelet-derived growth factor-induced proliferation of human hepatic stellate cell line LI90 . J Hepatol 2004 ; 40 : 52 - 59
Sartippour MR, Heber D, Zhang L, Beatty P, Elashoff D, Elashoff R, Go VL, Brooks MN . Inhibition of fibroblast growth factors by green tea . Int J Oncol 2002 ; 21 : 487 - 491
Sattler M, Pride YB, Ma P, Gramlich JL, Chu SC, Quinnan LA, Shirazian S, Liang C, Podar K, Christensen JG, Salgia R . A novel small molecule met inhibitor induces apoptosis in cells transformed by the oncogenic TPR-MET tyrosine kinase . Cancer Res 2003 ; 63 : 5462 - 5469
Schmidt L, Duh FM, Chen F, Kishida T, Glenn G, Choyke P, Scherer SW, Zhuang Z, Lubensky I, Dean M, Allikmets R, Chidambaram A . Germline and somatic mutations in the tyrosine kinase domain of the MET proto-oncogene in papillary renal carcinomas . Nat Genet 1997 ; 16 : 68 - 73
Shen Y, Naujokas M, Park M, Ireton K . InIB-dependent internalization of Listeria is mediated by the Met receptor tyrosine kinase . Cell 2000 ; 103 : 501 - 510
Stoker M, Gherardi E, Perryman M, Gray J . Scatter factor is a fibroblast-derived modulator of epithelial cell mobility . Nature 1987 ; 327 : 239 - 242
Tsarfaty I, Resau JH, Rulong S, Keydar I, Faletto DL, Vande Woude GF . The met proto-oncogene receptor and lumen formation . Science 1992 ; 257 : 1258 - 1261
Wang SY, Chen B, Zhan YQ, Xu WX, Li CY, Yang RF, Zheng H, Yue PB, Larsen SH, Sun HB, Yang X . SU5416 is a potent inhibitor of hepatocyte growth factor receptor (c-Met) and blocks HGF-induced invasiveness of human HepG2 hepatoma cells . J Hepatol 2004 ; 41 : 267 - 273
Webb CP, Hose CD, Koochekpour S, Jeffers M, Oskarsson M, Sausville E, Monks A, Vande Woude GF . The geldanamycins are potent inhibitors of the hepatocyte growth factor/scatter factor-met-urokinase plasminogen activator-plasmin proteolytic network . Cancer Res 2000 ; 60 : 342 - 349
Weber AA, Neuhaus T, Skach RA, Hescheler J, Ahn HY, Schror K, Ko Y, Sachinidis A . Mechanisms of the inhibitory effects of epigallocatechin-3 gallate on platelet-derived growth factor-BB-induced cell signaling and mitogenesis . FASEB J 2004 ; 18 : 128 - 130
Acknowledgements
This work was supported by 2003 Research Grant from Department of Medical Sciences, the Graduate School, Ajou University (to YH Shin and KS Pai). Also this work was partly supported by Korea Science & Engineering Foundation through Chronic Inflammatory Disease Research Center (Grant No. R13-2003-019).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Supplementary Information accompanies the paper on the Experimental & Molecular Medicine website
Supplementary information
Rights and permissions
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kwak, Ih., Shin, YH., Kim, M. et al. Epigallocatechin-3-gallate inhibits paracrine and autocrine hepatocyte growth factor/scatter factor-induced tumor cell migration and invasion. Exp Mol Med 43, 111–120 (2011). https://doi.org/10.3858/emm.2011.43.2.013
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.3858/emm.2011.43.2.013
Keywords
This article is cited by
-
Quantitative comparison of cancer and normal cell adhesion using organosilane monolayer templates: an experimental study on the anti-adhesion effect of green-tea catechins
In Vitro Cellular & Developmental Biology - Animal (2016)
-
Dietary phytochemicals alter epigenetic events and signaling pathways for inhibition of metastasis cascade
Cancer and Metastasis Reviews (2014)
-
Flavonoids, a ubiquitous dietary phenolic subclass, exert extensive in vitro anti-invasive and in vivo anti-metastatic activities
Cancer and Metastasis Reviews (2012)