Abstract
Background:
MYB encodes for a transcription factor regulating the expression of a wide array of genes involved in cellular functions. It is reported to be amplified in a sub-set of pancreatic cancer (PC) cases; however, its pathobiological association has remained unclear thus far.
Methods:
Expression of MYB and other cellular proteins was analysed by immunoblot or qRT-PCR analyses. MYB was stably overexpressed in non-expressing (BxPC3) and silenced in highly expressing (MiaPaCa and Panc1) PC cells. Effect on growth was analysed by automated cell counting at 24-h interval. Cell-cycle progression and apoptotic indices of PC cells with altered MYB expression were measured through flow cytometry upon staining with respective biomarkers. Cell motility/invasion was examined in a Boyden’s chamber assay using non-coated or Matrigel-coated membranes. Effect on tumorigenicity and metastatic potential was examined by non-invasive imaging and through end-point measurements of luciferase-tagged MYB-altered PC implanted in the pancreas of nude mice.
Results:
MYB was aberrantly expressed in all malignant cases of pancreas, whereas remained undetectable in normal pancreas. All the tested established PC cell lines except BxPC3 also exhibited MYB expression. Forced expression of MYB in BxPC3 cells promoted their growth, cell-cycle progression, survival and malignant behaviour, whereas its silencing in MiaPaCa and Panc1 cells produced converse effects. More importantly, ectopic MYB expression was sufficient to confer tumorigenic and metastatic capabilities to non-tumorigenic BxPC3 cells, while its silencing resulted in significant loss of the same in MYB-overexpressing cells as demonstrated in orthotopic mouse model. We also identified several MYB-regulated genes in PC cells that might potentially mediate its effect on tumour growth and metastasis.
Conclusions:
MYB is aberrantly overexpressed in PC cells and acts as a key determinant of pancreatic tumour growth and metastasis.
Similar content being viewed by others
Main
Pancreatic cancer (PC) is the fourth leading cause of cancer-related death in the United States and is expected to become the second on the list by the year 2030 (Rahib et al, 2014). As per the estimate of American Cancer Society, nearly 48 960 patients will be diagnosed with PC by this year end and 40 560 will succumb to its lethality (Siegel et al, 2015). Another upsetting fact is that the 5-year survival rate of PC patients has not improved over the past three decades and has remained very dismal (3–6%) (Siegel et al, 2014). Most PCs are diagnosed late at a stage when they are either locally advanced or have metastasised to distant organs (Vincent et al, 2011). In view of this grim scenario, it is extremely important that we identify novel targets involved in its aggressive and metastatic progression, which can help in devising targeted, mechanism-based, effective treatments for this devastating malignancy.
The MYB proto-oncogene was originally identified as the cellular counterpart of the v-Myb oncogenes carried by the chicken leukemia viruses (Ramsay and Gonda, 2008). In humans, MYB is located on the 6q22-24 chromosomal region and encodes a transcription factor protein (MYB/c-MYB) (Ramsay and Gonda, 2008). MYB acts as a transcriptional activator in the majority of cases and also cooperates with other transcription factors to synergistically induce gene expression (Ness, 2003). Over the years, several functions have been ascribed to MYB (Sakamoto et al, 2006; Ramsay and Gonda, 2008; George and Ness, 2014), and emerging data continue to add novel information on its biological functions. Abnormalities in the chromosomal region harbouring MYB were first reported in human acute myelogenous leukemia (Gonda and Metcalf, 1984), and later, its deregulated expression has been recorded in several other malignancies as well (Biroccio et al, 2001; Greco et al, 2001; Persson et al, 2009). MYB was identified as a candidate oncogene in PC owing to its gene amplification (Wallrapp et al, 1997); however, no study has yet attempted to characterise its functional involvement in PC pathobiology.
Here we present data demonstrating the functional significance of MYB in PC. MYB is aberrantly expressed in malignant cases of pancreas and established PC cell lines, whereas remaining undetectable in normal pancreas. Using both gain- and loss-of-function approaches, we demonstrate that MYB promotes the growth and clonogenicity of pancreatic tumour cells owing to increased cell-cycle progression and reduced apoptosis and also potentiate their aggressive malignant properties. Moreover, MYB expression is directly associated with tumorigenicity and metastasis of PC cells in an orthotopic mouse tumour xenograft model. In addition, MYB-overexpressing PC cells exhibit elicited expression of several genes associated with growth, survival and metastasis. Together, these findings establish MYB as a key driver of PC progression and metastasis.
Materials and methods
Cell lines and patient samples
All the PC cell lines used in this study were procured and maintained as previously described (Singh et al, 2010; Tyagi et al, 2014). All the cells were tested and determined to be free of mycoplasma every month and prior to beginning of any functional assay. Frozen pancreatic tissue samples (normal and malignant) were obtained through southern division of cooperative human tissue network under Institutional Review Board approved protocol.
Reagents, gene constructs and antibodies
The following reagents were used: a Roswell Park Memorial Institute medium (RPMI-1640); Dulbecco’s Modified Eagle Medium; fetal bovine serum (FBS) (Atlanta Biologicals, Lawrenceville, GA, USA); penicillin and streptomycin (Invitrogen, Carlsbad, CA, USA); four independent short hairpin RNA (shRNA) expression constructs for MYB (pGFP-V-RS-shMYB #1, #2, #3 and #4) and non-targeted scrambled control (pGFP-V-RS-NT-Scr) (Origene, Rockville, MD, USA); PGL4.5 Luciferase hygro plasmid and VivoGlo Luciferin (Promega, Madison, WI, USA); MycoSensorPCR assay kit (Stratagene, La Jolla, CA, USA); FuGENE transfection reagent (Roche, Indianapolis, IN, USA); Diff-Quick cell staining kit (Dade Behring, Inc., Newark, DE, USA); High Capacity Complementary DNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA, USA); and western blotting SuperSignal West Femto Maximum Sensitivity Substrate Kit (Thermo Scientific, Logan, UT, USA). Antibodies used were: MYB (1 : 1000; rabbit monoclonal; Epitomics, Burlingame, CA, USA), Bcl-2, Bax, Cyclin D1, Cyclin E1, p27, MMP7 (1 : 1000; rabbit monoclonal); p21 (1 : 1000; mouse monoclonal) (Cell Signaling Technology, Beverly, MA, USA), mouse biotinylated anti-β-actin (1 : 20 000; Sigma-Aldrich, St Louis, MO, USA), and horseradish peroxidase-labelled secondary antibodies (1 : 2000; Santa Cruz Biotechnology, Dallas, TX, USA).
Generation of stable transfectants
For ectopic MYB overexpression (in BxPC3) and knockdown (in Panc1 and MiaPaCa), cells were transfected with pCMV6-MYB and pGFP-V-RS-shMYB plasmid constructs, respectively, using FuGENE as a transfection reagent as per the manufacturer’s instructions. Empty vector (pCMV6-Neo) or non-targeted scrambled sequence expressing construct (pGFP-V-RS-NT-Scr) were also transfected to generate control derivative cell lines. Stable pooled population of transfected cells were selected in RPMI-media containing G418 (200 μg ml−1; for pCMV6-Neo and pCMV6-MYB) or Puromycin (2 μg ml−1; for pGFP-V-RS-NT-Scr and pGFP-V-RS-shMYB) and expanded. Forced MYB overexpression and silencing was confirmed through RT-PCR and immunoblotting intermittently. MYB-overexpressing and -silenced cells were also transfected with pGL4.50[luc2/CMV/Hygro] plasmid to stably express luciferase and selected in hygromycin (100 μg ml−1)-containing media.
Western blotting analysis
Western blotting was performed using standard procedures as described earlier (Deshmukh et al, 2015; Srivastava et al, 2015a). Briefly, cell lysates were resolved on 10% polyacrylamide gels and transferred to PVDF membranes. Blots were subjected to a standard immunodetection procedure using specific antibodies against various proteins and visualised using SuperSignal West Femto Maximum Sensitivity Substrate Kit with a LAS-3000 image analyser (Fuji Photo Film Co., Tokyo, Japan).
RNA isolation, cDNA synthesis and quantitative reverse transcription-PCR (qRT-PCR)
Total RNA was extracted using TRIzol reagent. Two microgram of total RNA was used for cDNA synthesis using the High Capacity Complementary DNA Reverse Transcription Kit following the manufacturer’s instructions. Subsequently, qRT-PCR was performed in 96-well plates using cDNA as a template and SYBR Green Master Mix on an iCycler system (Bio-Rad, Hercules, CA, USA) with specific primer pair sets. The thermal conditions for real-time PCR assays were as follows: cycle 1: 95 °C for 10 min, and cycle 2 (× 40): 95 °C for 10 s and 58 °C for 45 s (Khan et al, 2015).
Growth kinetics assay
Low or high MYB-expressing cells (1 × 104 per well) were seeded in six-well plates. Subsequently, cell growth was monitored by counting the number of viable cells using Countess automatic cell counter (Invitrogen), every day for 8 days.
Anchorage-dependent and -independent colony-formation assay
For plating efficiency, low or high MYB-expressing cells (1 × 103 cells per well) were seeded in six-well plate and allowed to form colonies for 2 weeks. Subsequently, colonies were fixed, stained with crystal violet (0.1% w/v), imaged and counted using the Image analysis software (Gene Tools, Syngene, Frederick, MD, USA). Anchorage-independent colony-formation assay was performed as previously described by us (Srivastava et al, 2012). Briefly cells (2 × 103cells ml−1) were suspended in regular media and mixed with equal volume of 0.6% agarose. Cell suspension–agar mix (2 ml) was seeded as top layer on premade 0.8% agarose layer (bottom layer) and 1 ml of complete media was added onto the top layer, which was replaced twice a week. Plates were incubated under normal culture conditions for 2 weeks for colony formation. Colonies were observed and photographed using Nikon Eclipse microscope (Nikon Instruments Inc. Lewisville, TX, USA) and counted (× 100 magnification).
Cell-cycle analysis
Cells (1 × 106 cells per well) were synchronised by growing them in serum-deprived culture media for 72 h. After synchronisation, cells were cultured in regular serum-containing medium for 24 h and processed for staining with propidium iodide using the PI/RNase Kit (BD Biosciences, San Jose, CA, USA) and analysis by flow cytometry on a BD-FACS Canto II (BD Biosciences, San Jose, CA, USA) as previously described by us (Bhardwaj et al, 2014).
Apoptosis assay
For apoptosis assay, cells (1 × 105 cells per well) were allowed to grow in serum-deprived culture media for 72 h. Subsequently, cells were stained with PE Annexin V and 7AAD (7-amino-actinomycin-D) by using the PE Annexin V apoptosis Detection Kit (BD Biosciences, San Diego, CA, USA) and analysed by flow cytometry as described earlier (Bhardwaj et al, 2014; Srivastava et al, 2015b).
Motility and invasion assays
MYB-overexpressing or -silenced cells were plated onto the top chamber of uncoated polyethylene teraphthalate membrane (5 × 105 cells per well; for migration) or Matrigel-coated (1 × 105 cells per well; for invasion) transwell chambers and the number of migrated/invaded cells were examined as described earlier (Srivastava et al, 2011).
Aggregation assay
MYB-overexpressing or -silenced cells along with their respective controls were placed as cell suspension drops (20 μl each containing 20 000 cells) onto the inner surface Petri dish lid. Subsequently, lid was placed on to the Petri dish with drops containing cells hanging from the lid to allow cell–cell interaction under the force of gravity. Following overnight incubation at 37 °C, the lid was inverted and photographed using Nikon Eclipse microscope (Nikon Instruments Inc.).
Assessment of tumorigenicity and metastatic potential in vivo
Studies involving the use of animals were approved by the IACUC. Luciferase-tagged paired MYB-knockdown and -overexpressing PC cell lines were injected into the pancreas of immunocompromised mice (Harlan Laboratories, Prattville, AL, USA) (10 mice/group). After 1 week of orthotopic injection, tumour growth was monitored every alternate day by palpation and weekly by bioluminescence imaging using Xenogen-IVIS-cooled CCD optical system (IVIS Spectrum) following intraperitoneal injection of D-Luciferin (150 mg kg−1 body weight). A final imaging was carried out at the end point (35 days after implantation), and all animals were killed. Primary tumours were resected, and mice were imaged for detection of near and distant metastases. In addition, liver, lung and spleen were excised and imaged separately.
Statistical analysis
All experiments were performed at least three times, and numerical data were expressed as mean±s.d. Wherever appropriate, the data were also subjected to unpaired two-tailed Student’s t-test, and P<0.05 was considered as significant.
Results
MYB is overexpressed in PC cells and associated with their growth and clonogenic properties
To examine the expression level of MYB in PC, total protein was isolated from a panel of established PC cell lines and frozen tissues of normal (n=7) and malignant (n=21) pancreas, and immunoblot analysis was performed. Aberrant MYB expression was observed in all PC cell lines except BxPC3 (Figure 1A). Moreover, when we examined its expression in normal pancreas and PC tissues, it was found to be undetectable in all the cases of normal pancreas (Figure 1B) but aberrantly expressed in all PC tissues (Figure 1C). To examine the functional significance, MYB was ectopically overexpressed in MYB non-expressing, poorly tumorigenic BxPC3 cell line (Delesque et al, 1997; Deer et al, 2010) by stable transfection (Figure 2A). Moreover, in a converse approach, we silenced MYB expression in two high MYB-expressing (MiaPaCa and Panc1) cell lines by RNA interference. Out of four independent MYB-targeting shRNA constructs, two (shMYB #2 and shMYB #4) were able to cause significant MYB silencing in both cell lines (Figure 2B and C). Therefore, we performed subsequent functional studies with their resulting transfectants and/or their pooled population (MiaPaCa-shMYB/Panc1-shMYB). A positive association of MYB expression with growth of PC cells was observed with 40.1% induction in BxPC3-MYB cells on the eighth day, whereas it was reduced by 34.8% (MiaPaCa-shMYB) and 32.8% (Panc1-shMYB) relative to their control sublines (Figure 2D, Supplementary Figure S1A). Next we examined the effect of MYB on the clonogenic potential of PC cells by performing plating efficiency and anchorage-independent clonogenicity assay. Our data demonstrate that, in comparison to controls, plating efficiency of BxPC3 cells was also significantly increased (∼8.6-fold, P<0.05) upon MYB overexpression, whereas MYB-silenced MiaPaCa and Panc1 formed lesser colonies (∼2.6- and 3.3-fold, respectively, P<0.05) (Figure 2E, Supplementary Figure S1B). Similarly, anchorage-independent clonogenicity of BxPC3-MYB cells was also greater (∼12-fold) than that of BxPC3-Neo, whereas it was decreased (∼3.4- and ∼3.7-fold, P<0.05) in MiaPaCa-shMYB and Panc1-shMYB cells relative to their controls (Figure 2F, Supplementary Figure S1C). Together, these findings support a growth-promoting role of MYB in pancreatic tumour cells.
MYB enhances growth and clonogenic potential of PC cells. Total protein was isolated from MYB (A) overexpressing (BxPC3-MYB) and (B and C) silenced MiaPaCa (B) and Panc1 (C) PC cells along with respective control cells, and the expression of MYB was examined by immunoblot assay. β-Actin served as an internal control. (D) Growth kinetics measurement of PC cell lines exhibiting forced expression (BxPC3-MYB) or silencing (MiaPaCa-shMYB and Panc-1-shMYB) of MYB relative to their respective controls (BxPC3-Neo, MiaPaCa-NT-Scr and Panc1-NT-Scr). (E) Plating efficiency of MYB-overexpressing and -silenced PC cells. Bars represent the mean of total number of colonies±s.d. (n=3), *P<0.05. (F) Soft agar colony-forming assay. Bars represent the total number of colonies in 10 random view fields (mean±s.d.; n=3), *P<0.05.
MYB-induced growth is associated with enhanced cell-cycle progression and apoptosis resistance
As tumour growth and clonogenic potential are associated with cell-cycle progression and apoptosis resistance, we examined these aspects in control and MYB-overexpressing/silenced PC cells. Our cell-cycle data demonstrate an enhanced cell-cycle progression in MYB-overexpressing cells, while it is decreased in MYB-silenced cells. A greater fraction (∼24.4, ∼20.9 and ∼28.8%) of MYB-overexpressing PC cells (BxPC3-MYB, MiaPaCa-NT-Scr and Panc1-NT-Scr cells, respectively) is detected in S-phase as compared with low MYB-expressing (BxPC3-Neo, ∼8.23%; MiaPaCa-shMYB, ∼10.9% and Panc1-shMYB, ∼11.8%) cells (Figure 3A). Additionally, the data from apoptosis assay indicate lower apoptotic index in cells exhibiting higher expression of MYB, that is, BxPC3-MYB (12.7%), MiaPaca-Scr (29.0%) and Panc1-Scr (33.0%) cells after 72 h of serum starvation; it was considerably increased in BxPC3-Neo (32.9%), MiaPaCa-shMYB (52.9%) and Panc1-shMyb (50.8%) cells. Altogether, these data suggest that MYB potentiates the growth and clonogenicity of PC cells by promoting cell-cycle progression and apoptosis resistance.
MYB promotes cell-cycle progression and imparts resistance to apoptosis in PC cells. (A) Synchronised cultures of MYB-overexpressing or -silenced PC cells along with their controls were grown in regular culture media for 24 h. Thereafter, cells were fixed, stained with propidium iodide and analysed using flow cytometry. (B) Cells were cultured under serum-free conditions for 72 h, and the extent of apoptotic cells were analysed by flow cytometry using PE Annexin V.
MYB promotes malignant properties of pancreatic tumour cells
To explore the effect of MYB expression on the aggressiveness of PC cells, we next examined the role of MYB in cell migration (by trans-well chamber assays) and invasion (migration through a Matrigel-coated porous membrane). A ∼3.6-fold increase in the motility of BxPC3-MYB was observed as compared with BxPC3-Neo cells, whereas it was significantly reduced (∼4.6- and ∼3.4-folds; P<0.05) in MiaPaCa-shMYB and Panc1-shMYB, respectively, relative to their controls (MiaPaCa- and Panc1-NT-Scr) (Figure 4A, Supplementary Figure S1D). Likewise, we also observed enhanced (∼4.2-fold) invasiveness in BxPC3-MYB cells in comparison to control, whereas it was decreased in MYB-silenced MiaPaCa (∼5.2-fold) and Panc1 (∼4.4-fold) cells (Figure 4B, Supplementary Figure S1E). Another aggressive malignant behavioural property of tumour cells is their decreased cell–cell interaction (homotypic), which is required for their dissemination (Srivastava et al, 2012). Thus we next examined the effect of MYB on the homotypic interaction of pancreatic tumour cells in a hanging drop assay. Considerable reduction in cell–cell interaction was observed in all the high MYB-expressing (BxPC3-MYB, MiaPaCa-NT-Scr and Panc1-NT-Scr) cells as compared with their low MYB-expressing (BxPC3-Neo, MiaPaCa-shMYB and Panc1-shMYB) counterparts (Figure 4C). Together, these findings demonstrate a role of MYB in growth and aggressive malignant properties of PC cells.
MYB promotes malignant potential of PC cells. (A and B) Control and MYB-overexpressing/silenced cells were seeded on non-coated (for motility assay) or Matrigel-coated (for invasion assay) membranes. Media containing 10% FBS in the lower chamber served as a chemoattractant. (A) Migrated and (B) invaded cells were counted and presented as the average number of cells/field±s.d., *P<0.05. Photographs are representative of three independent experiments performed in triplicate. (C) Hanging drop assay showing cell–cell interaction.
MYB promotes PC growth and metastasis in an orthotopic mouse model
To assess the effect of MYB on PC growth and metastasis, we injected two groups of luciferase-tagged (Supplementary Figure S2) paired cell lines (BxPC3-Neo/BxPC3-MYB and MiaPaCa-NT-Scr/MiaPaCa-shMYB) into the mouse pancreas. Tumour growth was monitored every alternate day by manual palpation and each week by in vivo luminescence imaging. All mice were killed on thirty-fifth day postinjection. End-point analyses confirmed no tumour formation in any of the mice injected with BxPC3-Neo cells (Figure 5A), whereas 100% tumour incidence (average tumour weight of 1.8±0.34 g and size of 1363.8±8 mm3) was observed in mice injected with BxPC3-MYB cells (Figure 5A–C). Similarly, we observed large tumours in all the mice injected with MYB-overexpressing (MiaPaCa-NT-Scr) cells, whereas mice of MiaPaCa-shMYB group had relatively smaller tumours (Figure 5A). Average weight (Figure 5B) and size (Figure 5C) of tumours developed from MiaPaCa-NT-Scr cells were 2.25±0.32 g and 2093.3±543 mm3, respectively, as compared with 0.389±0.16 g and 356.3±138.4 mm3 in the MiaPaCa-shMYB group. Silencing and overexpression of MYB in tumour xenografts was confirmed by immunohistochemical analysis (Supplementary Figure S3). To analyse the impact of MYB expression on metastatic dissemination, we imaged mice after resection of primary tumours. Strong signals were observed in various organs of MYB-overexpressing group indicating the metastasis of tumour cells, while no signal was detected in any of the mice implanted with low MYB-expressing cells (Figure 6A). These findings were further confirmed by ex vivo imaging of organs. Metastases were detected in the liver, lung and spleen of BxPC3-MYB and MiaPaCa-NT-Scr tumour-bearing mice, whereas it was absent in the mice of BxPC3-Neo and MiaPaCa-shMYB groups (Figure 6B).
MYB enhances tumour growth in nude mice. (A) Luciferase-tagged MYB-overexpressing (BxPC3-MYB) or -silenced (MiaPaCa-shMYB) cells along with their respective control sublines were implanted into the pancreas of athymic nude mice (n=10 per group). Mice were imaged using IVIS in vivo imaging system to measure luminescence once a week after intraperitoneal injection of D-luciferin. Representative images of mice are from the day they were killed. (B and C) Upon killing the animals, their tumours were resected and measured for their weights and volumes. Graphs reflect the distribution of (B) weights and (C) volumes of tumours derived from MYB-overexpressing BxPC3 and -silenced MiaPaCa cells along with those originated from their respective controls.
MYB promotes metastasis in orthotopic mouse model of PC. (A) Following tumour excision, mice from each group were imaged to visualise metastases to secondary organs. Images are representative of all the mice. (B) Livers, lungs and spleens were carefully removed from the mice and imaged for metastatic lesions. (C) Incidence of metastasis to different secondary organs. Red and blue colours represent positive and negative incidence.
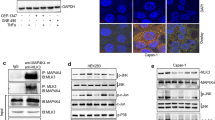
MYB modulates the expression of genes associated with proliferation, survival and metastasis
To gain insight into the underlying molecular mechanism of MYB-induced tumour-promoting and malignant phenotypes, we examined the expression of various genes associated with tumour progression and metastasis in high and low MYB-expressing PC cells by quantitative RT-PCR. We observed that, among the 85 analysed genes, 22 genes involved in the regulation of proliferation, survival, invasion and metastasis of cancer cells were significantly altered upon silencing of MYB (greater than or equal to two-fold difference; P⩽0.05) in comparison to high MYB-expressing control subline (MiaPaCa-NT-Scr) (Figure 7A). Expression of cell-cycle-associated genes, including CCND1, CCNE1 and PCNA, was decreased, whereas that of CDKN1B/p27 and CDKN1A/p21 was increased in MYB-silenced PC cells. Similarly, transcript levels of pro-apoptotic genes such as BAX were upregulated, whereas that of antiapoptotic genes, BCL2 and MCL1, lowered in MYB-silenced PC cells. Moreover, decreased expression of angiogenesis, migration, invasion and metastasis-related genes such as MMP7, ICAM1, VEGF, MYC, ADM and CXCR4 was also observed in low MYB-expressing PC cells. We further validated these findings at the protein level by conducting immunoblot analyses of select target proteins. As expected, reduced expression of cyclins (D1 and E1), antiapoptotic protein (Bcl2) and MMP7 was seen in low MYB-expressing PC cells (Figure 7B). In contrast, high expression of cyclin-dependent kinase inhibitors (p27 and p21) and pro-apoptotic protein (Bax) was detected in these cells as compared with high MYB-expressing PC cells (Figure 7B). Taken together, these findings suggest that the MYB promotes growth and metastatic potential of PC cells by modulating the expression of genes associated with proliferation, survival and metastasis.
MYB alters the expression of genes involved in the regulation of tumour-associated phenotypes. (A) Total RNA from MYB-silenced (MiaPaCa-shMYB) and control (MiaPaCa-NT-Scr) PC cells was isolated, cDNA was prepared and profiling of tumour-associated genes was performed using qRT-PCR. (B) Total protein was isolated and subjected to immunoblot analysis to the expression of various tumour-associated genes using specific antibody. β-Actin was used as a loading control.
Discussion
PC is a highly aggressive disease with no effective cure (Singh et al, 2010; Vincent et al, 2011). Over the years, we have developed an understanding of the common genetic aberrations involved in its aetiology and progression; however, this knowledge has not been translated into successful prevention and/or therapeutic strategies. Most pancreatic tumours are highly genetically advanced at the time of diagnosis and the disease is highly heterogeneous in nature (Vincent et al, 2011). This raises the possibility that multiple molecular mechanisms are operative with unique and/or overlapping functional impact, and it would be imperative to identify select target genes that are critically involved in PC pathobiology. The data presented herein identify MYB as an important determinant of pancreatic tumour growth, aggressive behaviour and metastasis using pancreatic cancer cell lines of varying genetic make-up (Deer et al, 2010) and by utilising two different approaches (loss and gain of function). These presented findings are strongly supportive of important roles of MYB in PC pathogenesis.
Previous studies have demonstrated important roles of MYB in normal development, homeostasis and pathophysiology of benign and malignant diseases (Nakata et al, 2007; Ramsay and Gonda, 2008; Drabsch et al, 2010; George and Ness, 2014; Ye et al, 2014; Wang et al, 2015). In the present study, our data revealed the essential role of MYB in promoting the growth of PC cells under in vitro as well as in orthotopic tumour xenograft mouse model. Similar observations have also been made in other studies (Melani et al, 1991; Ye et al, 2014; Cheasley et al, 2015; Wang et al, 2015). Blocking the function of MYB by antisense oligonucleotides or its dominant-negative forms led to the suppression of proliferation and survival in acute myeloid leukemia and chronic myeloid leukemia (Jahagirdar et al, 2001; Pattabiraman and Gonda, 2013). Knockdown of MYB increased the sensitivity of myeloid leukemia cells to the histone deacetylase inhibitor in vitro and in vivo (Ye et al, 2014). Similarly, in our recently published study, we reported that overexpression of MYB promoted, whereas its knockdown inhibited, the growth of prostate cancer cells (Srivastava et al, 2012). More recently, Cheasley et al (2015) demonstrated that defective MYB function perturbs colorectal tumorigenesis in mouse model. Furthermore, an overexpression of MYB was also reported in nasopharyngeal carcinoma (NPC), which was associated with the growth of NPC cells (Wang et al, 2015).
Growth of tumour cells is associated with the increased cell-cycle progression and acquisition of apoptosis resistance. Accordingly, we also observed a role of MYB in facilitating cell-cycle progression and apoptosis resistance in PC cells. Significance of MYB in cell-cycle progression and apoptosis resistance has been documented by us and others as well (Nakata et al, 2007; Drabsch et al, 2010; Srivastava et al, 2012). In our earlier study, we reported that MYB rescued prostate cancer cells from androgen-depletion-induced cell-cycle arrest and apoptosis to support their androgen-deprivation-resistant growth (Srivastava et al, 2012). Another group suggested the involvement of MYB in the cell-cycle regulation of hematopoietic cells (Muller et al, 1999). In NPC, it was shown that MYB induces the growth of NPC cells through potentiating cell-cycle progression. Authors demonstrated that silencing of MYB in 5-8F and CNE2 NPC cells resulted in cell-cycle arrest (Wang et al, 2015). Besides its role in cell-cycle regulation, studies also suggest its role in apoptosis resistance. MYB is shown to promote colon tumorigenesis by inhibiting the apoptosis of tumour cells (Biroccio et al, 2001). Similarly, MYB is reported to promote survival of CD4+CD8+ double-positive thymocytes (Yuan et al, 2010).
Besides its effect on growth and clonogenicity of PC cells, MYB also potentiated variety of phenotypes associated with cancer aggressiveness, such as migration, invasion and cell–cell interaction. Moreover, we observed a direct association of MYB with metastatic potential of pancreatic tumour cells in a mouse model. These findings are consistent with several previous observations (Chen et al, 2010; Tanno et al, 2010; Knopfova et al, 2012; Srivastava et al, 2012). MYB promoted migration and invasion of hepatocellular carcinoma cells by increasing the expression of osteopontin (Chen et al, 2010). Similarly, role of MYB in potentiating the invasive behaviour of breast cancer cells has also been documented (Knopfova et al, 2012). Moreover, in another report, MYB was shown to stimulate malignant potential and homing of cancer cells of different origin by regulating the expression of Slug and other regulators of mesenchymal transition (Tanno et al, 2010). More recently, we also demonstrated the functional significance of MYB in growth, invasion, migration and EMT of prostate cancer cells (Srivastava et al, 2012). A clinical correlation of MYB with metastatic potential of gallbladder carcinoma has also been reported (Shu et al, 2013).
Based on the studies conducted so far, it has been suggested that MYB can regulate various genes responsible for tumorigenesis and metastasis in various cancer types (Lorenzo et al, 2011; Quintana et al, 2011; Costa et al, 2014; Li et al, 2014; Cheasley et al, 2015). Using PCR-based array, we identified several genes involved in growth promotion, differentiation and malignant behaviour of tumour cells. Some of these genes are also being reported to be known direct targets of MYB in other cancer cells, such as BCL2, MYC, CCND1 and CXCR4 (Drabsch et al, 2010; Quintana et al, 2011). However, we also observed several potential novel targets of MYB in PC cells, suggesting that it may act in a cell- and context-specific manner to confer its biological properties. Differential expression of surface receptors such as EGFR and CXCR4 in MYB-overexpressing PC cells suggest that MYB dysregulation may have a broader impact depending upon the tumour microenvironment and other active mechanisms within the tumour and its surrounding stromal cells. Similarly, regulation of other transcription factors by MYB, such as KLF-4 and JUN-D, indicates that MYB may employ both direct and indirect mechanisms for gene regulation and to confer its diverse pathobiological actions in PC (Quintana et al, 2011).
In summary, we have identified that MYB acts as a key driver of pancreatic tumour growth and metastasis by altering several cellular phenotypes via regulating gene expression. It will, however, be important to study the clinical relevance of MYB in a larger set of pancreatic tumour samples as well as to understand the mechanisms underlying its widespread overexpression in pancreatic tumours. It will also be important to investigate the mechanisms through which MYB might act as a sensor and/or effector of evolving tumour microenvironment to understand its broader impact on pancreatic tumour pathobiology.
Change history
22 December 2015
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bhardwaj A, Srivastava SK, Singh S, Arora S, Tyagi N, Andrews J, McClellan S, Carter JE, Singh AP (2014) CXCL12/CXCR4 signaling counteracts docetaxel-induced microtubule stabilization via p21-activated kinase 4-dependent activation of LIM domain kinase 1. Oncotarget 5 (22): 11490–11500.
Biroccio A, Benassi B, D'Agnano I, D'Angelo C, Buglioni S, Mottolese M, Ricciotti A, Citro G, Cosimelli M, Ramsay RG, Calabretta B, Zupi G (2001) c-Myb and Bcl-x overexpression predicts poor prognosis in colorectal cancer: clinical and experimental findings. Am J Pathol 158 (4): 1289–1299.
Cheasley D, Pereira L, Sampurno S, Sieber O, Jorissen R, Xu H, Germann M, Yuqian Y, Ramsay RG, Malaterre J (2015) Defective Myb function ablates cyclin E1 expression and perturbs intestinal carcinogenesis. Mol Cancer Res 13 (8): 1185–1196.
Chen RX, Xia YH, Xue TC, Ye SL (2010) Transcription factor c-Myb promotes the invasion of hepatocellular carcinoma cells via increasing osteopontin expression. J Exp Clin Cancer Res 29: 172.
Costa AF, Altemani A, Garcia-Inc, Fresno F, Suarez C, Llorente JL, Hermsen M (2014) Analysis of MYB oncogene in transformed adenoid cystic carcinomas reveals distinct pathways of tumor progression. Lab Invest 94 (6): 692–702.
Deer EL, Gonzalez-Hernandez J, Coursen JD, Shea JE, Ngatia J, Scaife CL, Firpo MA, Mulvihill SJ (2010) Phenotype and genotype of pancreatic cancer cell lines. Pancreas 39 (4): 425–435.
Delesque N, Buscail L, Esteve JP, Saint-Laurent N, Muller C, Weckbecker G, Bruns C, Vaysse N, Susini C (1997) sst2 somatostatin receptor expression reverses tumorigenicity of human pancreatic cancer cells. Cancer Res 57 (5): 956–962.
Deshmukh SK, Srivastava SK, Bhardwaj A, Singh AP, Tyagi N, Marimuthu S, Dyess DL, Dal ZV, Carter JE, Singh S (2015) Resistin and interleukin-6 exhibit racially-disparate expression in breast cancer patients, display molecular association and promote growth and aggressiveness of tumor cells through STAT3 activation. Oncotarget 6 (13): 11231–11241.
Drabsch Y, Robert RG, Gonda TJ (2010) MYB suppresses differentiation and apoptosis of human breast cancer cells. Breast Cancer Res 12 (4): R55.
George OL, Ness SA (2014) Situational awareness: regulation of the myb transcription factor in differentiation, the cell cycle and oncogenesis. Cancers (Basel) 6 (4): 2049–2071.
Gonda TJ, Metcalf D (1984) Expression of myb, myc and fos proto-oncogenes during the differentiation of a murine myeloid leukaemia. Nature 310 (5974): 249–251.
Greco C, Alvino S, Buglioni S, Assisi D, Lapenta R, Grassi A, Stigliano V, Mottolese M, Casale V (2001) Activation of c-MYC and c-MYB proto-oncogenes is associated with decreased apoptosis in tumor colon progression. Anticancer Res 21 (5): 3185–3192.
Jahagirdar BN, Miller JS, Shet A, Verfaillie CM (2001) Novel therapies for chronic myelogenous leukemia. Exp Hematol 29 (5): 543–556.
Khan MA, Srivastava SK, Bhardwaj A, Singh S, Arora S, Zubair H, Carter JE, Singh AP (2015) Gemcitabine triggers angiogenesis-promoting molecular signals in pancreatic cancer cells: therapeutic implications. Oncotarget e-pub ahead of print 23 April 2015.
Knopfova L, Benes P, Pekarcikova L, Hermanova M, Masarik M, Pernicova Z, Soucek K, Smarda J (2012) c-Myb regulates matrix metalloproteinases 1/9, and cathepsin D: implications for matrix-dependent breast cancer cell invasion and metastasis. Mol Cancer 11: 15.
Li L, Chang W, Yang G, Ren C, Park S, Karantanos T, Karanika S, Wang J, Yin J, Shah PK, Takahiro H, Dobashi M, Zhang W, Efstathiou E, Maity SN, Aparicio AM, Li Ning Tapia EM, Troncoso P, Broom B, Xiao L, Lee HS, Lee JS, Corn PG, Navone N, Thompson TC (2014) Targeting poly(ADP-ribose) polymerase and the c-Myb-regulated DNA damage response pathway in castration-resistant prostate cancer. Sci Signal 7 (326): ra47.
Lorenzo PI, Brendeford EM, Gilfillan S, Gavrilov AA, Leedsak M, Razin SV, Eskeland R, Saether T, Gabrielsen OS (2011) Identification of c-Myb target genes in K562 cells reveals a role for c-Myb as a master regulator. Genes Cancer 2 (8): 805–817.
Melani C, Rivoltini L, Parmiani G, Calabretta B, Colombo MP (1991) Inhibition of proliferation by c-myb antisense oligodeoxynucleotides in colon adenocarcinoma cell lines that express c-myb. Cancer Res 51 (11): 2897–2901.
Muller C, Yang R, Idos G, Tidow N, Diederichs S, Koch OM, Verbeek W, Bender TP, Koeffler HP (1999) c-myb transactivates the human cyclin A1 promoter and induces cyclin A1 gene expression. Blood 94 (12): 4255–4262.
Nakata Y, Shetzline S, Sakashita C, Kalota A, Rallapalli R, Rudnick SI, Zhang Y, Emerson SG, Gewirtz AM (2007) c-Myb contributes to G2/M cell cycle transition in human hematopoietic cells by direct regulation of cyclin B1 expression. Mol Cell Biol 27 (6): 2048–2058.
Ness SA (2003) Myb protein specificity: evidence of a context-specific transcription factor code. Blood Cells Mol Dis 31 (2): 192–200.
Pattabiraman DR, Gonda TJ (2013) Role and potential for therapeutic targeting of MYB in leukemia. Leukemia 27 (2): 269–277.
Persson M, Andren Y, Mark J, Horlings HM, Persson F, Stenman G (2009) Recurrent fusion of MYB and NFIB transcription factor genes in carcinomas of the breast and head and neck. Proc Natl Acad Sci USA 106 (44): 18740–18744.
Quintana AM, Liu F, O'Rourke JP, Ness SA (2011) Identification and regulation of c-Myb target genes in MCF-7 cells. BMC Cancer 11: 30.
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM (2014) Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 74 (11): 2913–2921.
Ramsay RG, Gonda TJ (2008) MYB function in normal and cancer cells. Nat Rev Cancer 8 (7): 523–534.
Sakamoto H, Dai G, Tsujino K, Hashimoto K, Huang X, Fujimoto T, Mucenski M, Frampton J, Ogawa M (2006) Proper levels of c-Myb are discretely defined at distinct steps of hematopoietic cell development. Blood 108 (3): 896–903.
Shu GS, Lv F, Yang ZL, Miao XY (2013) Immunohistochemical study of PUMA, c-Myb and p53 expression in the benign and malignant lesions of gallbladder and their clinicopathological significances. Int J Clin Oncol 18 (4): 641–650.
Siegel R, Ma J, Zou Z, Jemal A (2014) Cancer statistics, 2014. CA Cancer J Clin 64 (1): 9–29.
Siegel RL, Miller KD, Jemal A (2015) Cancer statistics, 2015. CA Cancer J Clin 65 (1): 5–29.
Singh S, Srivastava SK, Bhardwaj A, Owen LB, Singh AP (2010) CXCL12-CXCR4 signalling axis confers gemcitabine resistance to pancreatic cancer cells: a novel target for therapy. Br J Cancer 103 (11): 1671–1679.
Srivastava SK, Bhardwaj A, Arora S, Tyagi N, Singh AP, Carter JE, Scammell JG, Fodstad O, Singh S (2015a) Interleukin-8 is a key mediator of FKBP51-induced melanoma growth, angiogenesis and metastasis. Br J Cancer 112 (11): 1772–1781.
Srivastava SK, Bhardwaj A, Arora S, Tyagi N, Singh S, Andrews J, McClellan S, Wang B, Singh AP (2015b) MicroRNA-345 induces apoptosis in pancreatic cancer cells through potentiation of caspase-dependent and -independent pathways. Br J Cancer 113 (4): 660–668.
Srivastava SK, Bhardwaj A, Singh S, Arora S, McClellan S, Grizzle WE, Reed E, Singh AP (2012) Myb overexpression overrides androgen depletion-induced cell cycle arrest and apoptosis in prostate cancer cells, and confers aggressive malignant traits: potential role in castration resistance. Carcinogenesis 33 (6): 1149–1157.
Srivastava SK, Bhardwaj A, Singh S, Arora S, Wang B, Grizzle WE, Singh AP (2011) MicroRNA-150 directly targets MUC4 and suppresses growth and malignant behavior of pancreatic cancer cells. Carcinogenesis 32 (12): 1832–1839.
Tanno B, Sesti F, Cesi V, Bossi G, Ferrari-Amorotti G, Bussolari R, Tirindelli D, Calabretta B, Raschella G (2010) Expression of Slug is regulated by c-Myb and is required for invasion and bone marrow homing of cancer cells of different origin. J Biol Chem 285 (38): 29434–29445.
Tyagi N, Bhardwaj A, Singh AP, McClellan S, Carter JE, Singh S (2014) p-21 activated kinase 4 promotes proliferation and survival of pancreatic cancer cells through AKT- and ERK-dependent activation of NF-kappaB pathway. Oncotarget 5 (18): 8778–8789.
Vincent A, Herman J, Schulick R, Hruban RH, Goggins M (2011) Pancreatic cancer. Lancet 378 (9791): 607–620.
Wallrapp C, Muller-Pillasch F, Solinas-Toldo S, Lichter P, Friess H, Buchler M, Fink T, Adler G, Gress TM (1997) Characterization of a high copy number amplification at 6q24 in pancreatic cancer identifies c-myb as a candidate oncogene. Cancer Res 57 (15): 3135–3139.
Wang W, Wu S, Shi Y, Miao Y, Luo X, Ji M, Yao K, He J (2015) c-MYB regulates cell growth and DNA damage repair through modulating MiR-143. FEBS Lett 589 (5): 555–564.
Ye P, Zhao L, McGirr C, Gonda TJ (2014) MYB down-regulation enhances sensitivity of U937 myeloid leukemia cells to the histone deacetylase inhibitor LBH589 in vitro and in vivo. Cancer Lett 343 (1): 98–106.
Yuan J, Crittenden RB, Bender TP (2010) c-Myb promotes the survival of CD4+CD8+ double-positive thymocytes through upregulation of Bcl-xL. J Immunol 184 (6): 2793–2804.
Acknowledgements
This work was supported by funding from NIH/NCI (CA167137, CA175772, CA185490 (to APS) and CA169829 (to SS)) and USAMCI.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Srivastava, S., Bhardwaj, A., Arora, S. et al. MYB is a novel regulator of pancreatic tumour growth and metastasis. Br J Cancer 113, 1694–1703 (2015). https://doi.org/10.1038/bjc.2015.400
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2015.400
Keywords
This article is cited by
-
MYB interacts with androgen receptor, sustains its ligand-independent activation and promotes castration resistance in prostate cancer
British Journal of Cancer (2022)
-
MYB oncoproteins: emerging players and potential therapeutic targets in human cancer
Oncogenesis (2021)
-
Clinicopathologic significance and race-specific prognostic association of MYB overexpression in ovarian cancer
Scientific Reports (2021)
-
DHX9 contributes to the malignant phenotypes of colorectal cancer via activating NF-κB signaling pathway
Cellular and Molecular Life Sciences (2021)
-
Genome-wide mapping of DNA-binding sites identifies stemness-related genes as directly repressed targets of SNAIL1 in colorectal cancer cells
Oncogene (2019)