Abstract
Polyoxomolybdates (PMs) as discrete molybdenum-oxide cluster anions have been investigated in the course of study of their medical applications. Here, we show the significant antitumour potency of the polyoxomolybdate [Me3NH]6[H2MoV12O28(OH)12(MoVIO3)4]·2H2O (PM-17), which is a photo-reduced compound of [NH3Pri]6[Mo7O24]·3H2O. The effect of PM-17 on the growth of cancer cell lines and xenografts was assessed by a cell viability test and analysis of tumour expansion rate. Morphological analysis was carried out by Hoechst staining, flow-cytometric analysis of Annexin V staining, terminal deoxynucleotidyl transferase-mediated ‘nick-end’ labelling staining, and electron-microscopic analysis. Activation of autophagy was detected by western blotting and fluorescence-microscopic analysis of the localisation of GFP-LC3 in transfected tumour cells. PM-17 inhibited the growth of human pancreatic cancer (AsPC-1) xenografts in a nude mice model, and induced morphological alterations in tumour cells. Correspondingly, PM-17 repressed the proliferation of AsPC-1 cells and human gastric cancer cells (MKN45) depending on the dose in vitro. We observed apoptotic patterns as the formation of apoptotic small bodies and translocation of phosphatidylserine by Hoechst staining and flow-cytometric analysis following Annexin V staining, and in parallel, autophagic conformation by the formulation of autophagosomes and localisation of GFP-LC3 by electron- and fluorescence-microscopic analysis.
Similar content being viewed by others
Main
Pancreatic cancer is an aggressive form of cancer, and has one of the poorest outcomes of all cancers (Jemal et al, 2005; Tani et al, 2006). Less than 10% of newly diagnosed pancreatic cancer patients achieve 5-year survival (Fakih, 2006). Although the clinical investigation of several antitumour agents has been conducted with a principal focus on fluorouracil, no agent has been found to suppress tumour growth. Also, there is no obvious improvement in the results of treatment with multiple drug therapy (Kelsen et al, 1991; Topham et al, 1991; Rougier et al, 1993; Nose et al, 1999) or the biochemical modulation of fluorouracil (Pazdur et al, 1992; Louvet et al, 1993; Weinerman and MacCormick, 1994; Bernhard et al, 1995). Gemcitabine, a nucleoside analogue, is efficacious in relieving the symptoms such as algia or general state in the case of nonscaling down of tumours (Casper et al, 1994). Furthermore, since the gemcitabine group has a beneficial effect on survival rate compared with the fluorouracil group, gemcitabine is the drug of choice for progressive pancreatic cancer at present. However, in recent findings, there is a significant toxic effect of gemcitabine combined with radiation in the treatment of advanced pancreatic cancer (McGinn et al, 2001, 2002; Wolff et al, 2001; Crane et al, 2002). In addition, since existing antipancreatic cancer drugs have no eradicative potency, it is necessary to find medicines that have new mechanisms of antitumour activity.
Dramatic improvement has been made in the treatment of patients by modern chemotherapeutic protocols, which are based on the dose-dependent antitumour activity of cisplatin (CDDP). However, the excellent antitumour activity of CDDP is accompanied by strong toxic effects. From chemical analogy with CDDP, antitumour active organometallic compounds such as titanocene dichloride, copper (I), silver (I), and gold (I or III) tetrahedral diphosphine complexes, and organosilicone compounds such as trimethylsilylethylthioethylamine and its derivatives, have been found (Fujita et al, 1990). In the course of examination of the biological effects of polyoxometalates, inorganic polymers of metal oxide, significant antitumour effects of polyoxomolybdates were found against conventional murine tumours (Fujita et al, 1992). [NH3Pri]6[Mo7O24]·3H2O (PM-8) was found to exhibit potent antitumour activity against MX-1 human breast cancer, Meth-A sarcoma, and MM46 adenocarcinoma in vivo (Yamase et al, 1988). Recent work from our laboratory showed that the efficacy of PM-8 has been recognised also for both AsPC-1 human pancreatic cancer and MKN45 human gastric cancer, which results from activation of the apoptotic pathway (Ogata et al, 2005; Mitsui et al, 2006; Yanagie et al, 2006). It has been proposed that PM-8 could be preferentially taken into tumour cells and converted into an approximately 10-fold more toxic species, produced through biological reduction probably in the mitochondrial system. This would inhibit ATP generation, and such a significant difference in toxicity between PM-8 and its reduced species would lead to a tumour-selective inhibition. This is based on the enhanced metabolism in tumour cells, since the high molecular weight of the reduced species (as a condensed species) would result in a longer stay in the tumour cells (Yamase, 2005).
In this study, we show noticeable antitumour activity of PM-17 (=[Me3NH]6[H2MoV12O28(OH)12(MoVIO3)4]·2H2O), one of the reduced species of PM-8, in the treatment of AsPC-1 cells and (or) MKN45 cells in vitro and in vivo. Furthermore, we aimed to clarify the mechanism of the anticancer effects of these compounds.
Materials and methods
PM-8 and PM-17
PM-8 was synthesised according to the published procedure (Yamase and Ikawa, 1977). PM-17 was prepared as follows: an aqueous solution (20 ml) of PM-8 (0.3 g, 0.2 mmol) in a Pyrex tube was irradiated for 4 days using a 500-W superhigh-pressure mercury/xenon lamp. iPrNH2 was added dropwise to the dark brown-coloured photolyte to adjust the pH to 8.8, then added [Me3NH]Cl (1 g, 10.4 mmol), and followed by cooling at 4°C. Reddish-brown rod crystals of the photo-reduced product were precipitated after 1–2 weeks and isolated by filtration. Yield: 64.3 mg, 25.9% based on Mo. Calcd: N 3.03, C 7.78, H 2.83, Mo 55.3%; found: N 3.42, C 8.16, H 2.56, Mo 53.8%. Manganometric redox titration showed the presence of 11.6±0.1 MoV centres in PM-17. Together with the X-ray crystallographic results (Yamase and Ishikawa), the elemental analysis enabled us to formulate PM-17 as given.
Animals and cell lines
Female nude mice (BALB/c, nu/nu) were purchased from Japan SLC Inc. The experiments were performed with the permission of the Animal Ethics Committee of The University of Tokyo in accordance with the Declaration of Helsinki. At the start of the experiments, the mice were 7 weeks old and were kept under controlled, specific pathogen-free conditions (temperature 23±2°C, relative humidity 55±5% and 12 h/12 h light/dark cycle) in isolation. An AsPC-1 human pancreatic cancer cell line and a MKN45 human gastric cancer cell line were used in this study, and were maintained in RPMI 1640 medium (GIBCO, Carlsbad, CA, USA) supplemented with 10% FBS (CLONTECH Laboratories, Mountain View, CA, USA), 100 U ml−1 of penicillin G, and 100 U ml−1 streptomycin in a 5% CO2 humidified atmosphere at 37°C.
Tumour growth inhibition test
To estimate the antitumour effects of PM-17 on the proliferation of AsPC-1 cells in vivo, 2 × 106 cells were transplanted into the back of nude mice. After 10 days, intratumoral injections of PM-17 (125μg or 500 μg dissolved in 100 μl saline) were performed for 10 days with a 2-day intermission on day 6. The control mice were treated with 100 μl saline per day under the same conditions used for the animals treated with PM-17. The tumour volume was determined using the two principal perpendicular diameters as V=1/2 × length (mm) × (width (mm))2.
Antibodies and chemicals
Antibodies were obtained from the following commercial sources: anti-MAP LC3 (Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA); anti-β-actin antibody (SIGMA-Aldrich, Saint Louis, MO, USA). Horseradish peroxidase-conjugated Streptavidin was purchased from Amersham Biosciences (Buckinghamshire, UK). PM-17 was prepared by the chemical synthesis group in our laboratory.
Cell viability assay
To determine the effect of PM-17 on tumour cells, we assessed cell viability after treatment using the trypan blue dye exclusion assay (Takeuchi et al, 2005). AsPC-1 and MKN45 in exponential growth phase were harvested, seeded at 1.5 × 105 cells per 6 cm cell culture dish (5 ml), and incubated at 37°C in 5% CO2 in air overnight. The cells were then incubated for 24 h with or without PM-17 in graduated concentrations from 0 to 230 μg ml−1 (AsPC-1) and from 0 to 60 μg ml−1 (MKN45). After the cells were collected with a scraper and stained with trypan blue, the viable cells were counted using a haemocytometer. Considering the viability of untreated cells (the control) as 100%, we calculated survival fractions from the mean cell viability of the treated cells.
Quantification of apoptosis in situ
Analysis of DNA fragmentation of the lamellae of the tumour by terminal deoxynucleotidyl transferase-mediated ‘nick-end’ labelling (TUNEL) was done using a POD labelling in situ cell death detection kit (Roche, Basel, Switzerland). DNA fragmentation was detected by enzyme reaction of labelled POD with DAB substrate (Roche).
Detection of apoptotic small bodies
One million cells growing in 25 cm2 culture flasks were exposed to PM-17 at concentrations of 175 μg ml−1 (AsPC-1) and 40 μg ml−1 (MKN45) for 24 h. The cells were harvested and centrifuged at 200 g for 10 min before being washed and resuspended in PBS containing 1 mM Hoechst dye 33342 (SIGMA-Aldrich). The apoptotic cells were visualised by fluorescence microscopy (KEYENCE CORPORATION, Osaka, Japan).
Detection of DNA ladder
Cells growing in 10-cm diameter culture dishes were treated with PM-17 at concentrations of 0 or 175 μg ml−1 (AsPC-1) and 0 or 40 μg ml−1 (MKN45) for 24 h. Following centrifugation at 200 g, the harvested cells were lysed with DNA extraction buffer (10 mM Tris-HCl (pH 7.4), 10 mM EDTA, 0.5% Triton X-100) and incubated at 4°C for 10 min. After centrifugation at 16 000 g for 5 min, the cell lysate was treated with 500 μg ml−1 DNase-free RNase at 37°C for 1 h, followed by treatment with 500 μg ml−1 proteinase K at 50°C for 30 min. Electrophoresis in 1% agarose gels was then performed and DNA ladders were visualised by UV illumination after staining with ethidium bromide.
Quantification of disruption of cytoplasmic membrane
The translocation of phosphatidylserine from the inner part of the plasma membrane to the outer layer was detected with Annexin-V-FLUOS staining; the disruption of the cytoplasmic membrane was analysed by the formulation of PI–DNA complexes by flow cytometry with a FAC Sort FCM machine (Beckman Coulter, Fullerton, CA, USA). The experiments were performed with Annexin-V-FLUOS followed by staining with the Roche kit.
Measurement of caspase-3 activity
Activity of caspase-3 was measured by Caspase-Glo™ 3/7 Assay kit (Promega Corporation, Madison, WI, USA). The assay provides a proluminescent caspase-3/7 substrate, which contains the tetrapeptide sequence DEVD. Luminescence is proportional to the amount of caspase activity present. The experimental procedures followed the manufacturer's instructions. We measured the intensity of luminescence with a Mithras LB 940 microplate reader (Berthold Technologies, Bad Wildbad, Germany).
Western blot analysis
Two million cells were cultured in sterile 10 cm dishes in 10% FCS/RPMI 1640 culture medium overnight. Next day, the cells were exposed to experimental medium with or without PM-17 (MKN45, 40 μg ml−1; AsPC-1, 175 μg ml−1) for 24, 48, or 72 h. The cultured cells were centrifuged at 200 g for 5 min at 4°C and washed in ice-cold PBS.
After centrifugation, the supernatant was removed and the cell pellet was resuspended in 0.1 ml lysis buffer (PBS, 1% Triton X-100, 1% Nonidet P-40), and incubated at 4°C for 30 min. The cells suspended in the buffer were centrifuged at 10 000 g for 10 min at 4°C, and then the supernatant (containing the total protein fraction) was carefully transferred to a new tube. Each sample, containing equal amounts of protein (80 μg), was mixed 1 : 3 (v v−1) with sample buffer (Wako Pure Chemical Industries Ltd, Osaka, Japan) containing 20% 2-mercaptoethanol and boiled for 5 min. Samples containing identical quantities of protein were subjected to SDS–PAGE (4–20% gradient gel) together with biotinylated SDS–PAGE standards (Bio-Rad, Hercules, CA, USA). Electrophoresis was performed for almost 1 h at 40 mA. After electrophoresis, the separated proteins were electroblotted onto PVDF membranes (Millipore Corporation, Bellerica, MA, USA) for 60 min at 20 V. The membranes were blocked for 1 h with blocking solution (Dainippon Sumitomo Pharma, Osaka, Japan) dissolved in PBS-T (0.05% Tween 20 in PBS), then incubated with the primary antibodies diluted with blocking solution at 4°C. The dilution rates of the antibodies were as follows: anti-MAP LC3 antibody 1 : 200 and anti-β-actin antibody 1 : 3000. The following day, the membranes were rinsed three times for 10 min each in PBS-T at room temperature and incubated with HRP-labelled secondary antibodies (1 : 3000) and HRP-conjugated Streptavidin (1 : 3000) (GE Healthcare UK Ltd, Buckinghamshire, UK) diluted in blocking solution for 1 h at room temperature. The membranes were then washed three times for 10 min each in PBS-T and reacted with ECL Plus Western Blotting Detection System (GE Healthcare UK Ltd). Chemiluminescence was analysed by ChemiDoc XRS (Bio-Rad).
Transmission electron microscopy
Cells were fixed in a mixture of 2.5% glutaraldehyde in 0.1 M phosphate buffer, pH 7.4 for 2 h at 4°C, washed in 0.2 M sucrose/0.1 M phosphate buffer, pH 7.4, for 2 h, and postfixed with 1.5% osmium tetroxide in 0.1 M phosphate buffer for 1 h at room temperature. The material was dehydrated in an ethanol gradient (50, 70, 80, 90, and 100%) and propylene oxide, and embedded in Epon 812. The blocks were cut with a microtome and stained with 4% uranyl acetate and Reynolds solution. Samples were photographed in a JEOL JEM-1200 EX electron microscope at 80 kV.
Transfection and fluorescence microscopy
MKN45 cells and AsPC-1 cells were transfected using lipofectamine 2000 reagent (Invitrogen, Carlsbad, CA, USA) and pGFP-LC3. One day before transfection, 2 × 105 cells were spread in 24 well plates in 500 μl growth medium. Then the transfection solution was prepared as follows: in one tube, 0.8 μg of DNA was diluted in 50 μl of serum-free medium and mixed gently, in the second tube, 2 μl of lipofectamine 2000 reagent was diluted in 48 μl of serum-free medium and incubated at room temperature for 5 min. After 5 min incubation, both solutions were carefully combined, mixed gently, and incubated at room temperature for 20 min. The cells were washed, the transfection mixture (100 μl each) was added, and incubated at 37°C, under 5% CO2 humidified atmosphere for 6 h. Afterwards, the transfection mixture was replaced with growth medium. After 24 h, transfected cells were treated with or without PM-8 (MKN45, 900 μg ml−1; AsPC-1, 1.65 mg ml−1) or PM-17 (MKN45; 40 μg ml−1, AsPC-1; 175 μg ml−1) for 24 h. The cells were resuspended in PBS and transferred onto glass slides. The fluorescence of GFP-labelled LC3 protein was observed by fluorescence microscopy (Keyence Corporation).
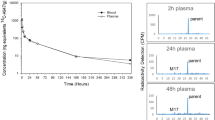
Haematological examination and blood chemistry assay
BALB/c nude mice were transplanted with 2 × 106 AsPC-1 cells into the back, and after 10 days, we carried out intratumoral injections of PM-17 (500 μg or 1 mg per 100 μl saline per day) for 10 days with a 2-day intermission on day 6. Control mice were treated with 100 μl of saline per day under the same conditions used for animals treated with PM-17. Negative control mice received neither tumour transplantation nor intratumoral injection. After 24 h from the last intratumoral injection, mice were anaesthetised and blood samples taken. Whole blood samples were used for haematological tests. Blood sera were assessed for BUN, creatinine, total bilirubin, total protein, AST, ALT, and ALP.
Statistical analysis
For the tumour cell inhibition assay in vivo, measurement of caspase-3 activity assay, haematological examination, and blood chemistry assay, statistical analysis was performed using t-test between control and samples treated with PM-17. P-values less than 0.05 indicate statistical significance.
Results
PM-17 interferes with the growth of a solid tumour of AsPC-1 in vivo
Timed measurements showed that PM-17 inhibited tumour growth at rates of 33.5 and 68.3% at doses of 125 μg and 500 μg per body per day (at 41 days after implantation of the tumour) compared with the controls (Figure 1A and B). In addition, there was no loss of body weight for mice injected with PM-17 in this experiment (Figure 1C). These results show that PM-17 inhibits the proliferation of AsPC-1 human pancreatic tumours in a dose-dependent manner in vivo.
PM-17 inhibits tumour growth depending on the dose in vivo. (A) Variance of tumour volume. After 10 days implantation of 2 × 106 AsPC-1 cells in BALB/c nude mice, these mice were treated with 0.9% NaCl solution (▪, n=5), PM-17 (125 μg per 100 μl) (•, n=5), and PM-17 (500 μg per 100 μl) (▴, n=5) intratumorally. The intratumoral injections were performed for 10 days with 2 days’ intermission on day 6. The tumour sizes were measured using a micrometre caliper. Points, mean of tumour volume of five mice per group; bars, s.d. *P<0.05 compared with control. (B) Tumours of 41 days after implantation (left, saline control; right, PM-17 500 μg per body treated). (C) Alteration of weight of tumour-bearing mice. Points, mean of percentage of body weight per group.
Inhibition of tumour cell growth with PM-17 in vitro
We examined the cytotoxic effects of PM-17 on the growth of AsPC-1 cells and MKN45 cells. These cells were suspended in RPMI 1640 culture medium containing a range of concentrations of PM-17. As shown in Figure 2, IC50 values of PM-17 against AsPC-1 cells and MKN45 cells were 175 and 40 μg ml−1, respectively.
The effect of PM-17 treatment on MKN45 cell and AsPC-1 cell survival in vitro. MKN45 cells were treated with PM-17 at the concentrations of 0–60 μg ml−1 for 24 h (A) and AsPC-1 cells were treated at the concentrations of 0–230 μg ml−1 for 24 h (B). Points, percentage of living cell in three independent experiments; bars, s.d.
Apoptotic changes of tumour cells treated with PM-17
To investigate the mechanism of cell inhibition by PM-17, morphological analysis by Hoechst staining was performed to detect the formation of apoptotic small bodies, as shown in Figure 3A. Sharp DNA laddering was observed after treatment with PM-17 by agarose gel electrophoresis of cell DNA extracts, which allowed us to confirm the induction of apoptosis by PM-17 (Figure 3B).
Apoptosis detection in tumour cells treated with PM-17. (A) Hoechst 33342 staining. The tumour cells treated with PM-17 at the IC50 concentrations (AsPC-1, 175 μg ml−1; MKN45, 40 μg ml−1) for 24 h were harvested and stained with Hoechst 33342. Arrows show apoptotic small bodies. (B) DNA ladder formation of AsPC-1 and MKN45 after 24 h treatment without or with IC50 of PM-17. DNA fragments derived from nontreated cells and treated cells were electrophoresed in agarose gel with 100 bp DNA ladder marker. (C) Flow-cytometric analysis by double-staining of Annexin-V-FLUOS and PI on AsPC-1 and MKN45 after 24 and 48 h treatment without or with IC50 of PM-17. (D) Activation of apoptosis signalling via caspase-3 activation in MKN45 cells and AsPC-1 cells treated with PM-17. The variation of caspase-3 activity with time was analysed by measurement of chemiluminescence of a proluminescent caspase-3/7 substrate. Columns, means of luminescence intensity response to activity of caspase-3 in three independent experiments; bars, s.d. *P<0.05 compared with control, n=3. (E) TUNEL staining of tumours injected with PM-8 (4 mg per 100 μl) or PM-17 (500 μg per 100 μl) or 100 μl of 0.9% NaCl solution as control once for all. The observations were made with a wide or narrow field of view as shown in panels.
Flow-cytometric analysis using Annexin V and PI staining was performed to determine the translocation of phosphatidylserine, disruption of cytoplasmic membranes, and produce quantitative results. Figure 3C shows that the ratio of apoptotic cells increased with the duration of PM-17 treatment: approximately 19.9% after 24 h and 77.8% after 48 h in MKN45 cells, and 16.2% after 24 h and 23.1% after 48 h in AsPC-1 cells.
The activation of caspase-3 was obtained in MKN45 cells and AsPC-1 cells treated with PM-17 as determined by Caspase-Glo™ 3/7 Assay. The substrate test used made it appear that caspase-3 was activated in both of the treated tumour cell lines (Figure 3D).
Moreover, TUNEL staining of thin sections of tumours after single injections of PM-8 or PM-17 showed the induction of cell degradation and DNA fragmentation (Figure 3E), and H&E staining showed that tumour cells treated with PM compounds led to hyalinisation by pathological observations. In the experiment, nude mice were injected with 2 × 106 of AsPC-1 cells. After 10 days, we gave single injections of PM-8 (4 mg per 100 μl saline) or PM-17 (500 μg per 100 μl saline) intratumorally. We then killed the mice after 24 h, eviscerated and fixed the tumours by freezing with O.C.T. Compound (Sakura Finetechnical Co. Ltd, Tokyo, Japan). Thin sections of tumours were stained with TUNEL stain. These results showed that PM-8 and PM-17 induced apoptosis of tumour cells in vivo.
Morphological analysis and detection of autophagic features
Electron-microscopic analysis shows that mitochondria had disrupted inner membranes in apoptotic MKN45 and AsPC-1 cells treated with PM-17 (Figure 4Aa, arrows). A number of vesicles, figurative autophagosomes, were formed (Figure 4Ab, arrows) in MKN45 and AsPC-1 cells treated with PM-8 and PM-17. Autophagic vacuoles contained cytosolic components and organelles.
Morphological analysis and detection of autophagic feature. MKN45 cells were treated with PM-8 (900 μg ml−1) or PM-17 (40 μg ml−1), and AsPC-1 cells were treated with PM-8 (1.65 mg ml−1) or PM-17 (175 μg ml−1). (A) Electron-microscopic analysis shows that mitochondria were disrupted. Inner constitution ((a), arrows) and appearance of quantity of autophagic vacuoles ((b), arrows) in MKN45 and AsPC-1 treated with IC50 of PM-8 or PM-17 for 24 h. (B) Subcellular localisation of GFP fusion LC3 protein in transfected MKN45 cells and AsPC-1 cells after treatment with or without IC50 of PM-8 or PM-17 for 24 h by fluorescent microscopy. (C) AsPC-1 cells treated with or without PM-17 (175 μg ml−1) for 24, 48, and 72 h. The cells were spun and lysed, and each 80 μg protein sample was loaded on SDS–PAGE gel and analysed by western blotting. Levels of LC3-I and -II expression were increased in cells treated with PM-17. Experiments were performed twice.
With a view to determine if an autophagic pathway or another cell death pathway had been activated in the tumour cells or not, we observed the localisation of LC3 after transient transfection (of MKN45 cells and AsPC-1 cells) of a plasmid encoding GFP-LC3 24 h after treatment with PM-8 or PM-17 (Figure 4B). LC3-II is a truncated form of LC-3, and is necessary to combine with the seclusion membrane for wrapping around cytoplasm components fundamentally at random in the primary stage of autophagy (Takeuchi et al, 2005). The GFP-LC3 was expressed and localised on subcellular components, which were considered to be autophagic vacuoles, upon treatment with PM-8 or PM-17 in fluorescence microscopic observations. We also examined the expression of LC3-II. Western blot analysis showed that the expression of LC3-II protein increased in AsPC-1 cells treated with PM-17 (Figure 4C). These results suggest that treatment with PM-17 induces activation of two types of cell death pathway, not only apoptosis but also autophagy.
Discussion
Some polyoxomolybates such as PM-8, PM-17, PM-26, and PM-32 were found to exhibit antitumour activities against Co-4 human colon tumour and Meth A sarcoma. In this research, we identified PM-17 as an antitumour compound effective against human pancreatic and gastric cancer cell lines, which induces apoptosis in parallel with autophagy in tumour cells. In addition, PM-17 has more potent antitumour activity than PM-8 in vivo (data not shown). It is thought that PM-17 is an active state of PM-8 at inside of the body or cells. PM-8 is reduced by electron transfer system in mitochondria, and becomes PM-17, which is a more cytotoxic agent (Yamase, 2005). Also we think that some of the antitumour activity of PM-8 is derived from reduced species such as PM-17.
From recent reports, the role of autophagy in the maintenance of cellular homoeostasis is becoming clearer. In normal cells, autophagy plays a role in the exclusion of excessive or abnormal proteins and organelles and in the recycling of cellular constituents (Boya et al, 2005). In addition, autophagic cell death, through the accumulation of autophagic vacuoles, affects degenerating neurones in some pathological states (Fletcher et al, 2000; Larsen et al, 2002), participates in retinal degeneration (Guimaraes et al, 2003), seals the fate of Salmonella-infected macrophages (Hernandez et al, 2003), and mediates chemotherapy-induced tumour cell death (Kanzawa et al, 2003, 2004; Opipari et al, 2004). However, there are few examples of the role of autophagy in physiological and pathological cell death because it is studied mainly based on morphological grounds (Tsujimoto and Shimizu, 2005).
Historically, three types of cell death have been distinguished in mammalian cells on morphological grounds; type 1 cell death better known as apoptosis, type 2 is autophagic cell death, and type 3 is also better known as necrosis. The molecular signalling systems of cell death have been elucidated progressively. In parallel, research has been focused on the connection of signalling between the different models of cell death. For example, in the model of immortalised baby-mouse kidney epithelial cells, which undergo cell death in response to hypoxia by knockdown of the pro-apoptotic proteins (Bax and Bak), however, the overexpression of the antiapoptotic protein Bcl-2 causes a shift from apoptosis to autophagic cell death (Golstein and Kroemer, 2007). In addition, in another model, human breast cancer MCF-7 cells exposed to camptothecin show rapidly induced apoptosis and much slower autophagy. Bid, BH3-only pro-death Bcl-2 family protein, knockout in MCF-7 cells results in suppression of camptothecin-induced apoptosis and a shift of cell death towards autophagy (Lamparska-Przybysz et al, 2005). These cases imply that there is a cross network pathway of apoptosis and autophagy in antitumoral cell death.
The results of our study show that PM-17 induces both apoptosis and autophagy in human pancreatic cancer AsPC-1 cells. We examined apoptosis-inductive signalling in tumour cell death, and neither activation of caspase-9 via the mitochondrial system nor activation of caspase-8 via the cytoplasmic system, known as representative apoptotic signalling systems, were confirmed (data not shown). We also verified the activation of caspase-3 and caspase-12 involved in ER stress signalling in preliminary experiments. On the other hand, there was no increase in PI3K(III) or Beclin-1, which were identified as regulatory factors of autophagy. In addition, in our study, AsPC-1 cells were pretreated with 3-MA (inhibitor of PI3K(III) in autophagy signalling) at increasing concentrations from 0 to 1 mM for 30 min before treatment with IC50 of PM-17 for 1–24 h, and estimated cell viability using the MTT assay. In this model, the inhibition of autophagy signalling by 3-MA had little effect on cell death induced by PM-17. It is possible that PM-17 activates autophagy through a different unknown route.
As another speculation, autophagy induced by PM-17 treatment does not function as the confrontive death system, but could be a reaction of the clearance system to the accumulation of dysfunctional organelles such as mitochondria or proteins denatured by chemotherapy. This mechanism could also be a rational way to reutilise the components of dying cells as nutrients for remaining cells. At present, we are proceeding to analyse the determination factor of the magnitude of apoptosis and autophagy.
Furthermore, we carried out a toxicity test for PM-17 in mice by haematological examination and serum chemistry (Table 1). In this investigation, blood sera were assessed for BUN, creatinine, total bilirubin, total protein, AST, ALT, and ALP. As a result, there was no significant difference between the control and PM-17 groups. The results showed that there was no impaired renal or hepatic function, nor haematocytes in our administration model of PM-17.
In conclusion, PM-17 may be useful as a novel effective reagent in treating pancreatic cancers, which generally have poor outcomes. We plan to investigate the induction mechanism of tumour cell death in detail, especially how PM-17 turns the cell death programme on, and continue research for in vivo models of antitumour therapy and the development of novel drug-delivery systems using PM-17 (Yanagie et al, 1997, 2004, 2006).
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bernhard H, Jager-Arand E, Bernhard G, Heike M, Klein O, Riemann JF, Meyer zum Buschenfelde KH, Dippold W, Knuth A (1995) Treatment of advanced pancreatic cancer with 5-fluorouracil, folinic acid and interferon alpha-2A: results of a phase II trial. Br J Cancer 71: 102–105
Boya P, Gonzalez-Polo RA, Casares N, Perfettini J, Dessen P, Larochette N, Métivier D, Meley D, Souquere S, Yoshimori T (2005) Inhibition of macroautophagy triggers apoptosis. Mol Cell Biol 25: 1025–1040
Casper ES, Green MR, Kelsen DP, Heelan RT, Brown TD, Flombaum CD, Trochanowski B, Tarassoff PG (1994) Phase II trial of gemcitabine (2,2′-difluorodeoxycytidine) in patients with adenocarcinoma of the pancreas. Invest New Drugs 12: 29–34
Crane CH, Abbruzzese JL, Evans DB, Wolff RA, Ballo MT, Delclos M, Milas L, Mason K, Charnsangavej C, Pisters PWT, Lee JE, Lenzi R, Vauthey JN, Wong ABS, Phan T, Nguyen Q, Janjan NA (2002) Is the therapeutic index better with gemcitabine-based chemoradiation than with 5-fluorouracil-based chemoradiation in locally advanced pancreatic cancer? Int J Radiat Oncol Biol Phys 52: 1293–1302
Fakih MG (2006) Gemcitabine-induced rectus abdominus radiation recall. JOP 7: 306–310
Fletcher GC, Xue L, Passingham KS, Tolkovsky MA (2000) Death commitment is advanced by axotomy in sympathetic neurons. J Cell Biol 150: 741–754
Fujita H, Fujita T, Sakurai T, Yamase T, Seto Y (1992) Antitumour activity of new antitumour substance, polyoxomolybdate, against several human cancers in athymic nude mice. Tohoku J Exp Med 168: 421–426
Fujita H, Fukushima K, Sakurai T (1990) Biological activity of organosilicone compounds – study on cancer chemotherapeutic activity. J Chem Industri Chem 5: 566–574
Golstein P, Kroemer G (2007) Cell death by necrosis: towards a molecular definition. Trends Biochem Sci 32: 37–43
Guimaraes CA, Benchimol M, Amarante-Mendes GP, Linden R (2003) Alternative programs of cell death in developing retinal tissue. J Biol Chem 278: 41938–41946
Hernandez LD, Pypaert M, Flavell RA, Galán JE (2003) A Salmonella protein causes macrophage cell death by inducing autophagy. J Cell Biol 163: 1123–1131
Jemal A, Murray T, Ward E, Samuels A, Tiwari RC, Ghafoor A, Feuer EJ, Thun MJ (2005) Cancer statistics, 2005. CA Cancer J Clin 55: 10–30
Kanzawa T, Germano MI, Komata T, Ito H, Kondo Y, Kondo S (2004) Role of autophagy in temozolomide-induced cytotoxicity for malignant glioma cells. Cell Death Differ 11: 448–457
Kanzawa T, Kondo Y, Ito H, Kondo S, Germano I (2003) Induction of autophagic cell death in malignant glioma cells by arsenic trioxide. Cancer Res 63: 2103–2108
Kelsen D, Hudis C, Niedzwiecki D, Dougherty J, Casper E, Botet J, Vinciguerra V, Rosenbluth R (1991) A phase III comparison trial of streptozotocin, mitomycin, and 5-fluorouracil with cisplatin, cytosine, arabinoside, and caffeine in patients with advanced pancreatic carcinoma. Cancer 68: 965–969
Lamparska-Przybysz M, Gajkowska B, Motyl T (2005) Cathepsins and BID are involved in the molecular switch between apoptosis and autophagy in breast cancer MCF-7 cells exposed to camptothecin. J Physiol Pharmacol 56: 159–179
Larsen KE, Fon AE, Hastings GT, Edwards HR, Sulzer D (2002) Methamphetamine-induced degeneration of dopaminergic neurons involves autophagy and upregulation of dopamine synthesis. J Neurosci 22: 8951–8960
Louvet C, Beerblock K, de Gramont A, Varette C, Demuynck B, Bennamoun M, Cady J, Delfau S, Maisani JE, Krulik M (1993) High-dose folinic acid, 5-fluorouracil bolus and infusion in advanced pancreatic adenocarcinoma: a pilot study. Eur J Cancer 29A: 1217
McGinn CJ, Lawrence TS, Zalupski MM (2002) On the development of gemcitabine-based chemoradiotherapy regimens in pancreatic cancer. Cancer 95: 933–940
McGinn CJ, Zalupski MM, Shureiqi I, Robertson JM, Eckhauser FE, Smith DC, Brown D, Heina G, Strawderman M, Normolle D, Lawrence TS (2001) Phase I trial of radiation dose escalation with concurrent weekly full-dose gemcitabine in patients with advanced pancreatic cancer. J Clin Oncol 19: 4202–4208
Mitsui S, Ogata A, Yanagie H, Kasano H, Hisa T, Yamase T, Eriguchi M (2006) Antitumour activity of polyoxomolybdate, [NH3Pri]6[Mo7O24].3H2O, against human gastric cancer model. Biomed Pharmacother 60: 353–358
Nose H, Okada S, Okusaka T, Furuse J, Yoshino M, Ogoshi K, Kato T, Miyaji M, Hoshino M, Ariyama J, Suyama M, Karasawa E, Yoshimori M (1999) 5-fluorouracil continuous infusion combined with cisplatin for advanced pancreatic cancer: a Japanese Cooperative Study. Hepato-Gastroenterol 46: 3244–3248
Ogata A, Mitsui S, Yanagie H, Kasano H, Hisa T, Yamase T, Eriguchi M (2005) A novel anti-tumour agent, polyoxomolybdate induces apoptotic cell death in AsPC-1 human pancreatic cancer cells. Biomed Pharmacother 59: 240–244
Opipari Jr AW, Tan L, Boitano AE, Sorenson DR, Aurora A, Liu JR (2004) Resveratrol-induced autophagocytosis in ovarian cancer cells. Cancer Res 64: 696–703
Pazdur R, Ajani JJ, Abbruzzese JL, Belt RJ, Dakhil SR, Dubovsky D, Graham S, Pilat S, Winn R, Levin B (1992) Phase II evaluation of fluorouracil and recombinant α-2a-interferon in previously untreated patients with pancreatic adenocarcinoma. Cancer 70: 2073–2076
Rougier P, Zarba JJ, Ducreux M, Basile M, Pignon JP, Mahjoubi M, Benahmed M, Droz JP, Cvitkovic E, Armand JP (1993) Phase II study of cisplatin and 120-h continuous infusion of 5-fluorouracil in patients with advanced pancreatic adenocarcinoma. Ann Oncol 4: 333–336
Takeuchi H, Kondo Y, Fujiwara K, Kanzawa T, Aoki H, Mills GB, Kondo S (2005) Synergistic augmentation of rapamycin-induced autophagy in malignant glioma cells by phosphatidylinositol 3-kinase/protein kinase B inhibitors. Cancer Res 65: 3336–3346
Tani M, Kawai M, Terasawa H, Ina S, Hirono S, Uchiyama K, Yamaue H (2006) Does postoperative chemotherapy have a survival benefit for patients with pancreatic cancer? J Surg Oncol 93: 485–490
Topham C, Glees J, Rawson NS, Woods EM, Coombes RC (1991) Randomised trial of epirubicin alone versus 5-fluorouracil, epirubicin and mitomycin C in locally advanced and metastatic carcinoma of the pancreas. Br J Cancer 64: 179–181
Tsujimoto Y, Shimizu S (2005) Another way to die: autophagic programmed cell death. Cell Death Differ 12: 1528–1534
Weinerman BH, MacCormick RE (1994) A phase II survival comparison of patients with adenocarcinoma of the pancreas treated with 5-fluorouracil and calcium leucovorin versus a matched tumour registry control population. Am J Clin Oncol 17: 467–469
Wolff RA, Evans DB, Gravel DM, Lenzi R, Psters PWT, Lee JE, Janjan NA, Charnsangavej C, Abbruzzese JL (2001) Phase I trial of gemcitabine combined with radiation for the treatment of locally advanced pancreatic adenocarcinoma. Clin Cancer Res 7: 2246–2253
Yamase T (2005) Anti-tumour, -viral, and -bacterial activities of polyoxometalates for realizing an inorganic drug. J Mater Chem 15: 4773–4782
Yamase T, Fujita H, Fukushima K (1988) Medical chemistry of polyoxometalates. Part 1. potent antitumor activity of polyoxomolybdates on animal transplantable tumors and human cancer xenograft. Inorg Chim Acta 151: 15–18
Yamase T, Ikawa T (1977) Photochemical study of the alkylammonium molybdates. III. Preparation and properties. Bull Chem Soc Jpn 50: 746–749
Yamase T, Ishikawa E manuscript for publication in preparation
Yanagie H, Maruyama K, Takizawa T, Ishida O, Ogura K, Matsumoto T, Sakurai Y, Kobayashi T, Shinohara A, Rant J, Skvarc J, Ilic R, Kuhne G, Chiba M, Furuya Y, Sugiyama H, Hisa T, Ono K, Kobayashi H, Eriguchi M (2006) Application of boron-entrapped stealth liposomes to inhibition of growth of tumour cells in the in vivo boron neutron-capture therapy model. Biomed Pharmacother 60: 43–50
Yanagie H, Ogata A, Mitsui S, Hisa T, Yamase T, Eriguchi M (2006) Anticancer activity of polyoxomolybdate. Biomed Pharmacother 60: 349–352
Yanagie H, Ogura K, Takagi K, Maruyama K, Matsumoto T, Sakurai Y, Skvarc J, Illic R, Kuhne G, Hisa T, Yoshizaki I, Kono K, Furuya Y, Sugiyama H, Kobayashi H, Ono K, Nakagawa K, Eriguchi M (2004) Accumulation of boron compounds to tumor with polyethylene-glycol binding liposome by using neutron capture autoradiography. Appl Radiat Isot 61: 639–649
Yanagie H, Tomita T, Kobayashi H, Fujii Y, Yonaka Y, Saegusa Y, Hasumi K, Eriguchi M, Kobayashi T, Ono K (1997) Inhibition of human pancreatic cancer growth in nude mice by boron neutron capture therapy. Br J Cancer 75: 660–665
Acknowledgements
Part of this study was supported by Grants-in-Aid for Scientific Research from the Ministry of Education, Science, Sport, and Culture of Japan (no. 17659402 to Hironobu Yanagie) (no. 18390360 to Hironobu Yanagie and Masazumi Eriguchi), and a grant from the ‘Creation of bio-devices with chemical and biological molecules for medical use’ (CREST) from the Japan Science and Technology agency (JST) (to Toshihiro Yamase). We thank Yuriko Sakurai and Kikue Mouri for technical support. Finally, we also gratefully acknowledge and pay respect to professor Alistair Renwick for great help and leading.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Ogata, A., Yanagie, H., Ishikawa, E. et al. Antitumour effect of polyoxomolybdates: induction of apoptotic cell death and autophagy in in vitro and in vivo models. Br J Cancer 98, 399–409 (2008). https://doi.org/10.1038/sj.bjc.6604133
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604133
Keywords
This article is cited by
-
Syntheses, Characterizations and Properties of [Mo2O2S2]-Based Oxothiomolybdenum Rings Incorporating Carboxylate Ligands
Journal of Cluster Science (2023)
-
Poly (N-vinylpyrrolidone) modification mitigates plasma protein corona formation on phosphomolybdate-based nanoparticles
Journal of Nanobiotechnology (2021)
-
Selected polyoxopalladates as promising and selective antitumor drug candidates
JBIC Journal of Biological Inorganic Chemistry (2021)
-
Synthesis, structures and applications of electron-rich polyoxometalates
Nature Reviews Chemistry (2018)
-
Gadolinium polytungstate nanoclusters: a new theranostic with ultrasmall size and versatile properties for dual-modal MR/CT imaging and photothermal therapy/radiotherapy of cancer
NPG Asia Materials (2016)