Abstract
We describe a novel technique to perform whole-body perfusion fixation in mice with specific relevance to micro-imaging. With the guidance of high-frequency ultrasound imaging, we were able to perfuse fixative and contrast agents via a catheter inserted into the left ventricle, and therefore preserved the integrity of the chest and abdominal cavity. In this preliminary study, our success rate over 15 animals was 73%. We demonstrate applications of this technique for magnetic resonance imaging and micro-CT, but we expect that this method can be generally applied to whole-body perfusions of other small animals in which the intact body is necessary.
Similar content being viewed by others
Main
Genetically manipulated mice have become widely applied animal models for exploring the molecular mechanisms of human diseases,1 but morphological phenotyping is one of the rate-limiting steps in fully characterizing new mouse mutants.2 In particular, whole-body anatomic pathology on all new mouse models is virtually impossible given the enormous number of mutant strains being created. Recently, a wide range of nondestructive imaging tools, such as magnetic resonance imaging (MRI), micro-CT and ultrasound biomicroscopy (UBM), are being developed to facilitate morphological phenotyping.3, 4, 5, 6, 7 These imaging techniques are advantageous compared with conventional gross pathology procedures, which require physically sectioning the animal and organs. For MRI and micro-CT, the highest imaging resolutions can be achieved in mouse cadavers because there are no physiological motions during the lengthy imaging process. On the other hand, contrast agents can be applied to improve the image contrast and reduce the scanning time.8 Therefore, mice need to be perfused with certain contrast agents, then fixed for imaging the whole body or the individual organs of interest.
For a comprehensive gross morphology study, it is very important to minimize damage of the mouse body during perfusions and fixation. Traditionally, perfusion–fixation of laboratory animal is accomplished by cannulating the left ventricle and draining from the right atrium in an open-chest procedure.9 However, in this procedure, physiologic pressure within the chest cavity is disrupted, leading to dramatic changes in the natural shape and spatial relation of the organs within the chest. To circumvent opening the chest cavity, Johnson et al6 used a multiple-perfusion method that fixes the whole mouse with cannulations into both the carotid artery and jugular vein and drainages through various points in the body. This procedure, although successful, is both labor intensive and time consuming, especially for small mice.
In this paper, we propose a method that reverts back to using the heart as the approach for the perfusion of contrast agent and fixation of the whole mouse, but utilizes a newly developed UBM to guide a catheter injection into the left ventricle without opening the chest. We apply this technique to the two imaging applications of MRI and micro-CT as described in protocols I and II below.
Materials and methods
All animal protocols were approved by the Hospital for Sick Children Animal Care Committee.
Protocol I
A total of 14 wild-type C57/BL6 mice (three males and 11 females, body weight: 23±6 g) (The Jackson Laboratory, Bar Harbor, Maine and Charles River Laboratories, Wilmington, MA, USA) were perfused with paramagnetic contrast agent and fixed for whole-body MRI. Each mouse was anesthetized using a mixture of Ketalean® at 100 mg/kg (Bimeda-MTC, Cambridge, Ont., Canada) and Rompun® (xylazine) at 20 mg/kg (Bayer Inc., Toronto). When adequately anesthetized, the mouse was secured with tape in the supine position in a custom-built mold designed to maintain the mouse's natural body shape after fixation. The hair on the chest wall was removed with a chemical hair remover. Ultrasound gel was spread over the precordial region and the UBM (Vevo 660, VisualSonics Inc., Toronto) with a 30-MHz transducer was used to visualize the left ventricle (Figure 1a). When the cross-section with the largest left-ventricular chamber dimension was located, an IV catheter (0.62 mm in outer diameter) with needle (BD Insyte, 24 GA, 0.75 IN, Becton Dickinson, Utah) was placed at the precordial area on the chest wall, with the longitudinal axis of the needle in the ultrasound imaging plane (Figure 1b). Under real-time image guidance, the needle was punctured into the left ventricle (Figure 1c). The needle was then removed, and the catheter was secured in place by tape (Figure 1d) and connected to a peristaltic pump (LKB Pump P-1, Pharmacia, Sweden) via a plastic tube.
Ultrasound-guided left-ventricular catheterization of an anesthetized mouse. (a) Sketch showing the spatial relation among the mouse chest, ultrasound transducer and the IV catheter with needle. (b) Two-dimensional ultrasound image showing the left ventricle (LV), and the tip of the needle on the surface of the chest. (c) Ultrasound image showing the needle punctured through the chest into the LV chamber. (d) Ultrasound image showing the catheter in the LV chamber after the needle was pulled out.
We then perfused with a mixture of saline, heparin (10 units/ml) and 10 mM gadopentetate dimeglumine (Magnevist®, Berlex Canada Inc., Qué., Canada) at a flow rate of 0.125 ml/min. This slow infusion with a high concentration of the contrast agent was performed for about 5 min, in an attempt to avoid rapid build-up of blood volume, which could result in heart failure, and to ensure that the whole mouse was thoroughly perfused with contrast agent while the heart was beating and circulation was intact. Then the jugular and femoral veins were cut for draining the blood and perfusate, and the mouse was flushed with a mixture of saline, heparin (10 units/ml), Magnevist® (1 mM) and blue dye (to monitor the progress of the perfusion) at a flow rate of 1.25 ml/min. Typically, the heart stopped beating after 2–3 min with this faster perfusion procedure. When the drained fluid ran clear, a mixture of 10% buffered formalin phosphate (Fisher Scientific, Nepean, Ont., Canada), Magnevist (1 mM) and blue dye was pumped through at a flow rate of 1.25 ml/min for ∼15 min to fix the whole mouse. The perfusion and fixation procedure from puncturing the left ventricle to the end of fixation took less than 30 min. During the perfusion, the proximal and distant ends of the right jugular vein and the right femoral vein were closed alternatively by hemostat to force the perfusate through the head, thorax and abdomen. In this way, 10 mice were successfully perfused and fixed, and four died because of repeated punctures on the left ventricle.
MR images were obtained with a 40-cm bore, 7-T magnet (Magnex Scientific, Oxford, UK) controlled by a UnityInova console (Varian NMR Instruments, Palo Alto, CA). The fixed whole mouse was placed in a 30-mm-diameter radiofrequency millipede coil10 (Varian NMR Instruments). We used a conventional spin echo acquisition with the following imaging parameters: 200 ms repetition time, 10 ms echo time, (28 × 28 × 120) mm3 Field-of-View and 420 × 420 × 1800 imaging matrix for a total imaging time of 9.8 h. The spin echo has the advantage of minimizing susceptibility artifacts that become pronounced at high field. After the reconstruction of the raw data, the three-dimensional (3D) data volume was visualized and processed using Amira software (TGS Inc., San Diego, CA, USA).
Protocol II
One wild-type C57/BL6 mouse (body weight: 35 g; female) was perfused with an X-ray contrast medium and then individual organs were harvested and fixed for micro-CT imaging. The anesthesia and left-ventricular catheterization procedures were the same as in protocol I. Following a 500-unit subcutaneous injection of heparin, a solution (∼100 ml) of heparinized-saline (1 unit/ml) at 37°C was infused to wash the blood in the cardiovascular system. The mouse's heart stopped within 1–2 min of the start of this infusion. Then the mouse was perfused with Microfil, a polymerizing silicone rubber contrast agent carrying a yellow lead oxide pigment to allow visibility and to increase the X-ray attenuation (Flow Tech Inc., Carver, MA, USA). The initial viscosity of the Microfil is comparable to blood but begins to harden 20 min after initiation. All fluids were infused at a constant pressure of 160 mmHg (21.3 kPa). The jugular vein was cut for drainage of blood and perfusate. After about 90 min, the brain, lungs, liver, spleen and kidneys were excised and stored in a solution of 10% formalin for fixation at 4°C for 24 h. After fixation, the organs were mounted in 10% gelatin for micro-CT imaging.
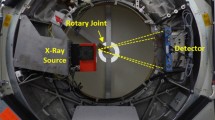
3D CT data sets were acquired for the individual organs using a micro-CT scanner (MS-8, GE Medical Systems, London, Ont., Canada). With the X-ray source at 80 kVp and 90 μA, the data were acquired in 2.5 h with 905 views at 35 μm resolution and a 3D data volume was reconstructed using the Feldkamp algorithm for cone beam CT geometry.11 3D surface rendering of the vasculature of individual organs was accomplished using Display software (Montréal Neurological Institute, McGill, Montréal, Qué., Canada).
Results and discussion
Figure 2 demonstrates a typical 3D data volume of a whole mouse MRI (Figure 2a), and 2D cross-sections showing specific organs (Figure 2b–f). The integrity of the thorax, the natural shape and spatial relation of the organs in the chest are well preserved (Figure 2b–d), except for a small hole through the chest and the left-ventricular wall due to the catheterization (Figure 2b). The entire cardiovascular system is significantly enhanced with respect to the surrounding soft tissues (Figure 2b–d). There is good contrast among the individual organs such as the parenchymal organs, muscle and fat (Figure 2e) and among different tissues within organs such as the spleen (Figure 2e). The nonvascular lumen such as the gallbladder (Figure 2c), stomach (Figure 2e), renal pelvis (Figure 2e), intestine (Figure 2f), urinary tract and bladder (not shown) and uterus (Figure 2f) were also clearly visualized, and the detailed wall structures were delineated due to the strong contrast between the lumen and the wall.
Typical MR images of a mouse perfused with gadopentetate dimeglumine. (a) The 3D data volume of the whole-body MR imaging. (b) An oblique cross-section showing the left atrium (LA) and left ventricle (LV), and the hole (arrow) through the ventricular and the chest walls caused by the catheterization. (c) A coronal cross-section showing the cardiac structures such as the LA, LV, ascending aorta (AA), right atrium (RA), right ventricle (RV) and main pulmonary artery (MPA) in the thoracic cavity and the liver (Li) with gallbladder (GB). (d) A coronal cross-section showing the right lung (RLu) and left lung (LLu) and the pulmonary vasculature. (e) A coronal cross-section showing the right kidney (RK) and left kidney (LK), spleen (Sp), stomach (St), cecum (Ce), fat (Fa) and psoas (Ps) in the abdomen. (f) A slightly oblique coronal cross-section showing small and large intestines (In) and one horn of uterus (Ut).
In the perfusion protocol II for micro-CT, the organs were well perfused as illustrated in Figure 3a. Figure 3b shows the 3D surface rendering of the pulmonary vasculature of the perfused lungs. Figure 3c shows the 3D surface rendering of the hepatic vasculature of the perfused liver, along with the inferior vena cava. Note that, we only see the vessels as the X-ray contrast agent is confined in those vascular lumens.
Three-dimensional surface rendering of the vasculatures based on the 3D data volume of micro-CT imaging on the mouse organs perfused with Microfil. (a) The perfused spleen and kidney. (b) The 3D pulmonary vasculature along with MPA and pulmonary vein (PV), viewed from back side. (c) The 3D hepatic vasculature along with inferior vena cava (IVC), viewed from the right side.
In summary, we have demonstrated a novel method of whole mouse perfusion and fixation for MRI of entire mouse and for micro-CT imaging of individual organs. This method minimizes anatomical damage and preserves the integrity of the chest cavity compared to the typical open-chest procedure. This method is also relatively simple compared to carotid cannulation. The success rate of our technique is slightly more than 70% in our present preliminary study and will further improve with experience. The initial puncturing of left ventricle is the most crucial step for the success, as repeated punctures after an initial failure may result in air entering or bleeding into the epicardial space, which can cause acoustical shadowing in the UBM imaging and eventual animal death. While we have shown this method in two specific applications in adult mice, it should be readily adaptable to young mice or other small animals in which other methods like carotid cannulation are very difficult due to the small body size. Although our applications have been for imaging, we believe that this technique can be generally used as an all-purpose perfusion–fixation method.
References
Rossant J, McKerlie C . Mouse-based phenogenomics for modeling human disease. Trends Mol Med 2001;7:502–507.
Brayton C, Justice M, Montgomery CA . Evaluating mutant mice: anatomic pathology. Vet Pathol 2001;38:1–19.
Kennel SJ, Davis IA, Branning J, et al. High resolution computed tomography and MRI for monitoring lung tumor growth in mice undergoing radioimmunotherapy: correlation with histology. Med Phys 2000;27:1101–1107.
Foster FS, Pavlin CJ, Harasiewicz KA, et al. Advances in ultrasound biomicroscopy. Ultrasound Med Biol 2000;26:1–27.
Balaban RS, Hampshire VA . Challenges in small animal noninvasive imaging. ILAR J 2001;42:248–262.
Johnson GA, Cofer GP, Fubara B, et al. Magnetic resonance histology for morphologic phenotyping. J Magn Reson Imaging 2002;16:423–429.
Zhou YQ, Foster FS, Qu DW, et al. Applications for multifrequency ultrasound biomicroscopy in mice from implantation to adulthood. Physiol Genomics 2002;10:113–126. Epub 2002 June 18.
Runge VM, Clanton JA, Herzer WA, et al. Intravascular contrast agents suitable for magnetic resonance imaging. Radiology 1984;153:171–176.
Stickrod G, Stansifer M . Perfusion of small animals using a mini-peristaltic pump. Physiol Behav 1981;27:1127–1128.
Wong WH, Sukumar S . “Millipede” imaging coil design for high field micro imaging applications [abstract], Proceedings of the ISMRM Eighth Annual Meeting. April 1–7, 2000. Denver, p. 1399.
Marxen M, Thornton MM, Chiarot CB, et al. Micro CT scanner performance and consideration for vascular specimen imaging. Med Phys 2004, (in press).
Acknowledgements
We thank Jun Dazai, Dr Natasa Kovacevic, Dr John G. Sled and Leila Baghdadi for their technical support, and Dr Laurence Hedlund for helpful discussion. This research was supported by Canada Foundation for Innovation, Ontario Innovation Trust, Ontario Research and Development Challenge Fund and the Canadian Institute of Health Research. There is a potential duality of interest. FSF has a financial interest in VisualSonics and serves on their board of directors. YQZ is a consultant to VisualSonics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhou, YQ., Davidson, L., Henkelman, R. et al. Ultrasound-guided left-ventricular catheterization: a novel method of whole mouse perfusion for microimaging. Lab Invest 84, 385–389 (2004). https://doi.org/10.1038/labinvest.3700038
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3700038
Keywords
This article is cited by
-
Microfocus computed tomography for fetal postmortem imaging: an overview
Pediatric Radiology (2022)
-
Articulated Whole-Body Atlases for Small Animal Image Analysis: Construction and Applications
Molecular Imaging and Biology (2011)
-
Correlation Between Local Hemodynamics and Lesion Distribution in a Novel Aortic Regurgitation Murine Model of Atherosclerosis
Annals of Biomedical Engineering (2011)
-
High-resolution ex vivo magnetic resonance angiography: a feasibility study on biological and medical tissues
BMC Physiology (2010)