Abstract
Study design:
Retrospective cohort study.
Objective:
Data on patient outcomes after surgery for spinal cord tumors have been derived from single-institution series. The objective of this study is to report inpatient complications, mortality and outcomes on a national level.
Setting:
United States, national inpatient care database.
Methods:
The National Inpatient Sample (NIS) was used to identify 19 017 admissions for resection of a spinal cord tumor in the United States from 1993 to 2002. The effects of patient and hospital characteristics on inpatient outcomes were analyzed using logistic regression.
Results:
The in-hospital mortality rate and the complication rate were 0.55 and 17.5%, respectively. Urinary and renal complications (3.7%), postoperative hemorrhages or hematomas (2.5%) and pulmonary complications (2.4%) were the most common complications reported. A single postoperative complication increased the length of stay by 4 days, increased the mortality rate by sixfold and added over $10 000 to hospital charges. Multivariate analysis showed that complications were more likely in African Americans and patients with multiple comorbidities. The odds of an adverse outcome increased significantly with age greater than 64, multiple comorbidities and postoperative complications.
Conclusion:
A national perspective on inpatient outcomes after resection of spinal cord tumors has been provided. The significant negative impact of postoperative complications on mortality and resource utilization has been demonstrated. We have identified advanced age and multiple comorbidities as risk factors that predict adverse outcome. Furthermore, this study highlights the importance of avoidance, recognition and prompt management of nonneurologic complications.
Similar content being viewed by others
Introduction
Intramedullary spinal cord tumors are rare and account for only 5–10% of spinal tumors. Spinal cord tumors are much less frequent than intracranial tumors with the overall prevalence of about one spinal cord tumor for every four intracranial tumors.1 The most common intramedullary spinal cord tumors include astrocytomas, ependymomas and hemangioblastomas. Complete resection of ependymomas and hemangioblastomas can often be achieved because of a favorable tissue plane between the tumor and the spinal cord. In contrast, about one-third of astrocytomas are diffusely infiltrative and are treated with biopsy and postoperative radiation.2
Evaluation of postoperative mortality, morbidity and outcomes after resection of spinal cord tumors is critical to the practice of evidence-based medicine. Medical decisions regarding treatment alternatives are guided by such evaluations. Hence, it is important to carefully examine surgical outcomes at an institutional as well as national level.
Given the relatively low incidence of spinal cord tumors, most information about patient characteristics, morbidity and mortality after surgery for spinal cord tumors has been derived from single-institution series. The objective of the current study was to define the rate of inpatient adverse outcomes, mortality rate, complication rate and the nature of complications following surgery for spinal cord tumors on a national level. We also analyze the effects of patient and hospital characteristics on outcomes such as complication rate, discharge disposition and length of stay (LOS).
Materials and methods
Data source
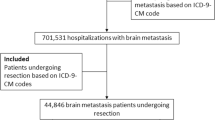
The National Inpatient Sample (NIS), the largest all-payer inpatient care database in the United States was utilized. This database is maintained by the Agency for Healthcare Research and Quality (AHRQ).3 It contains data from approximately 8 million annual discharges from 1004 hospitals in 37 states. It represents a 20% stratified sample of non-federal community hospitals, representing about 85% of all hospital discharges in the United States.
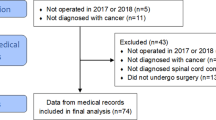
Inclusion criteria
All patients from 1993 to 2002 who had a primary diagnosis of neoplasm of uncertain behavior, malignant neoplasm or benign neoplasm of the spinal cord (ICD-9 diagnosis codes 192.2, 225.3, 237.5) who also underwent spine surgery (ICD-9 primary procedure codes 03.0, 03.4, 03.09, 81.0, 81.00–81.08) were included in this study. Patients with intradural extramedullary tumors such as spinal meningiomas (ICD-9 code 225.4) and nerve sheath tumors (ICD-9 code 215) were excluded from the analysis.
Patient and hospital characteristics
Variables such as patient age, gender, race, comorbidities, hospital size and year of treatment were abstracted from the NIS. Age was categorized into the following four groups: 0–17, 18–44, 45–64 and >64 years. Race was re-categorized into white, black and other. Year of treatment was categorized into two groups: 1993–1997 and 1998–2002. The frequency of a set of medical comorbidities as described by Elixhauser et al.,4 and previously listed in detail,5 was calculated using the AHRQ software (URL: www.ahcpr.gov/data/hcup/comorbid.htm).6 A single comorbidity score was then derived and used in the analysis.
The unique hospital identifier for each institution was used to determine the annual number of spinal cord tumor resections at each hospital. Annual hospital volume was then divided into quintiles representing very low, low, medium, high and very high volumes. The numeric thresholds for volume were 4 cases per year (very low), 8 cases per year (low), 17 cases per year (medium), 29 cases per year (high) and more than 29 cases per year (very high).
Outcome variables
The primary outcomes were ‘adverse outcome’ and complication rate. Adverse outcome was defined as death or discharge to institution other than home. Complications were obtained using the following ICD-9 codes: neurologic complications (997.00–997.09), pulmonary complications (518.81–518.85, 997.3), thromboembolic complications including deep venous thrombosis (DVT) and pulmonary embolism (415, 387, 415.11–415.19, 4510–4519, 4530–4539), cardiac complications (997.1, 410), urinary and renal complications (584, 997.5), hemorrhage or hematoma complicating a procedure (998.1–998.13). Mortality, LOS and hospital charges were also abstracted from the NIS dataset.
Statistical analysis
Descriptive statistics for demographic variables were tabulated. Outcomes were compared with χ2 analysis for categorical variables. A P-value of less than 0.05 was accepted as significant. A multivariate logistic regression model was constructed for the multivariate analysis, and only those variables that satisfied the screening cutoff of P<0.1 with the univariate analysis were incorporated into the multivariate analysis.5 The multivariate odds ratios (OR) are reported with the 95% confidence intervals (CI). For the purpose of multivariate analysis, LOS was categorized into normal LOS (less than or equal to median LOS) and prolonged LOS (greater than median LOS). Multivariate analysis was performed for the following binary outcome variables: mortality, complications, adverse outcome and LOS. Extrapolations to the entire United States population were performed using the SAS Proc Survey methodology.7 All data analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, NC, USA) running on Windows XP_Pro.
Results
Utilizing the NIS from 1993 to 2002, a total of 19 017 admissions for surgically treated spinal cord tumors were identified in the United States. Table 1 depicts the patient and hospital characteristics and their association with morbidity. Of them, 9% of the patients treated were less than 18 years of age and 38% were in the 18–44 years age group. A total of 84% of patients were Caucasian and 53% were women. Altogether, 54% of patients had no comorbidities and 6% had three or more comorbidities. Most patients (73%) were treated at large hospitals. Total in-hospital complication rate was 17.5% and the in-hospital mortality rate for the entire cohort was 0.55% (Table 2). The mean LOS was 7.2 days, and the median LOS was 5.0 days. The percent of patients discharged home was 79 and the mean hospital charges were 27 223 dollars.
Table 3 catalogs the complications by pulmonary, postoperative hemorrhage/hematoma, thromboembolic, renal/urinary, cardiac, infectious and neurologic. Renal/urinary complications were most frequent (3.7%), followed by postoperative hematoma or hemorrhage (2.5%) and pulmonary complications (2.4%). Postoperative neurologic deficit was reported in 1.7% of patients. The NIS dataset does not code preoperative neurologic deficits or the severity of postoperative complications, including neurologic complications. Due to this limitation of the NIS, these important parameters could not be assessed further.
The negative effects of complications on LOS, mortality, discharge disposition and hospital charges are demonstrated in Table 4. With just one postoperative complication, the mean LOS increased by 4 days, the mortality rate increased sixfold (from 0.3 to 1.8%), the likelihood of discharge to institution other than home almost doubled and hospital charges increased by over 10 000 dollars.
Age, race, comorbidities, hospital size and hospital volume were identified as potential predictors of morbidity by the univariate analysis (Table 1). Multivariate analysis for complications showed that morbidity was significantly higher for African American patients and for patients with comorbidities (Table 5). African American patients had 1.9 times higher odds of developing a postoperative complication compared to Caucasians. Also, patients with one or more comorbidities were 1.4–1.6 times more likely to have a complication. The odds of a complication were 1.6 times higher at large-size hospitals compared to small-size hospitals. However, when volume effects were calculated specifically for tumor resections, high-volume hospitals had similar complication rates as low-volume hospitals.
Multivariate analysis revealed age, three or more comorbidities and complications as significant factors affecting adverse outcome (Table 6). The odds of an adverse outcome in patients 65–84 years of age were 2.8 times that of patients 18–45 years of age. Patients with three or more comorbidities were 1.6 times more likely to have an adverse outcome compared to patients with no comorbidities. Having a single postoperative complication doubled the odds of an adverse outcome (OR=2.2).
The effects of age, gender, comorbidities and hospital volume on mortality were not statistically significant (Table 7). Multivariate analysis showed a very strong negative effect of postoperative complications on mortality. The odds of in-hospital death for patients with one postoperative complication were six times that of patients with no complications. Multivariate analysis for LOS showed increased LOS for pediatric patients (OR=2.1), African Americans (OR=1.6), patients who were operated in the earlier year group of 1993–1997 (OR=2.0) and who had three or more comorbidities (OR=1.6) or postoperative complications (OR=4.8).
Discussion
Postoperative outcomes of patients who underwent spine surgery for spinal cord tumors from 1993 to 2002 in the United States have been reported. Approximately 19 000 admissions from a nationally representative sample of hospitals were included in the current analysis. Previous single-institution series have reported postoperative complication rates of 11–64% with generally higher complication rates after resection of astrocytomas compared to ependymomas.8, 9, 10, 11, 12, 13, 14 The NIS data do not afford distinction between the different pathologic types of spinal cord tumors and hence, we cannot comment on the complication rates after resection of astrocytomas versus ependymomas. Furthermore, the 17.5% complication rate we report in our study is likely an underestimate of the true complication rate because only select complications were examined. In addition, the NIS database contains only inpatient complications for that particular admission and complications that arise after discharge are not included in the NIS database.
Age, gender, ethnicity, comorbidities, hospital volume and complications are potential predictors of outcome and were evaluated in this study. Due to the limitation of the NIS dataset, other previously reported factors such as tumor pathology, grade, preoperative neurologic status and extent of tumor resection that predict outcome could not be evaluated in this analysis.2, 9, 10, 12 Also, this analysis contains only inpatient outcomes and cannot comment on long-term outcomes or recurrences. Nonetheless, this is the first study to report morbidity, mortality and the effect of postoperative complications on resource utilization on a national level for surgically treated spinal cord tumors.
It is intuitive that postoperative complications would lead to a worse outcome and increased resource utilization. However, this has not been previously quantified. After controlling for factors such as age, gender and comorbidities in the multivariate analysis, postoperative complications were found to increase adverse outcome and mortality significantly. Compared to patients with no complications, patients with a single complication were four times more likely to die and almost two times more likely to be discharged to an institution other than home. Furthermore, complications dramatically increased resource utilization as demonstrated by the increase in LOS and hospital charges. Renal/urinary complications, postoperative hemorrhage/hematoma and pulmonary complications were the most commonly reported morbidities. Neurologic complications were likely underreported and recorded in only 1.7% of the cases. In our judgment, the common sensory impairments and minor neurologic deficits were likely not reported in the NIS and only major neurologic deficits were recorded. Previous single-institution series have almost exclusively focused on the description, prevention and management of neurologic complications.8, 9, 10, 11, 12, 13, 14 Our study demonstrates the significant negative impact of mostly nonneurologic complications on patient outcomes. Therefore, avoidance, recognition and prompt management of neurologic as well as nonneurologic postoperative complications is extremely important in the successful surgical management of patients with spinal tumors.
Multivariate analysis found that odds of a complication increased with African American ethnicity and with the presence of preoperative comorbidities. Odds of death or discharge to an institution other than home increased with advanced age, multiple comorbidities and postoperative complications. Our previous analysis of patients undergoing surgery for spinal metastasis in the United States showed that the majority of patients with spinal metastasis had at least one preoperative comorbidity.5 We also demonstrated a strong negative impact of comorbidities on adverse outcome in patients after surgical resection of spinal metastasis. In contrast, over 80% of patients undergoing resection of spinal cord tumor had no or one comorbidity. Hence, in general, patients undergoing surgery for spinal cord tumors are healthier than patients undergoing surgery for spinal metastasis. In contrast to the significant negative influence of comorbidities seen in spinal metastasis patients, the current analysis shows only a modest impact of multiple comorbidities on adverse outcome.
In summary, a national perspective on inpatient complications and outcomes after surgery for spinal cord tumors in the United States has been provided. The significant negative effects of postoperative complications on discharge disposition, LOS, mortality and resource utilization have been demonstrated and quantified. We have shown that advanced age and multiple comorbidities are risk factors that predict adverse outcome. Furthermore, this study highlights the importance of avoidance, recognition and prompt management of nonneurologic complications such as renal failure, cardiopulmonary dysfunction and postoperative hemorrhage.
References
Tihan T, Chi JH, McCormick PC, Ames CP, Parsa AT . Pathologic and epidemiologic findings of intramedullary spinal cord tumors. Neurosurg Clin N Am 2006; 17: 7–11.
Parsa AT, Lee J, Parney IF, Weinstein P, McCormick PC, Ames C . Spinal cord and intradural-extraparenchymal spinal tumors: current best care practices and strategies. J Neurooncol 2004; 69: 291–318.
Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality: Rockville, MD, 2004.
Elixhauser A, Steiner C, Harris DR, Coffey RM . Comorbidity measures for use with administrative data. Med Care 1998; 36: 8–27.
Patil CG, Lad SP, Santarelli J, Boakye M . National inpatient complications and outcomes after surgery for spinal metastasis from 1993–2002. Cancer 2007; 110: 625–630.
Barker II FG . Craniotomy for the resection of metastatic brain tumors in the US, 1988–2000: decreasing mortality and the effect of provider caseload. Cancer 2004; 100: 999–1007.
Agency for Healthcare Research and Quality. Calculating Nationwide Inpatient Sample Variances. Agency for Healthcare Research and Quality: Rockville, MD, 2002.
Chang UK, Choe WJ, Chung SK, Chung CK, Kim HJ . Surgical outcome and prognostic factors of spinal intramedullary ependymomas in adults. J Neurooncol 2002; 57: 133–139.
Epstein FJ, Farmer JP, Freed D . Adult intramedullary spinal cord ependymomas: the result of surgery in 38 patients. J Neurosurg 1993; 79: 204–209.
Hanbali F, Fourney DR, Marmor E, Suki D, Rhines LD, Weinberg JS et al. Spinal cord ependymoma: radical surgical resection and outcome. Neurosurgery 2002; 51: 1162–1172, discussion 1172–1174.
Lee HK, Chang EL, Fuller GN, Aldape KD, Atkinson GJ, Levy LB et al. The prognostic value of neurologic function in astrocytic spinal cord glioma. Neuro Oncol 2003; 5: 208–213.
McCormick PC, Stein BM . Intramedullary tumors in adults. Neurosurg Clin N Am 1990; 1: 609–630.
Samii M, Klekamp J . Surgical results of 100 intramedullary tumors in relation to accompanying syringomyelia. Neurosurgery 1994; 35: 865–873 discussion 873.
Shirato H, Kamada T, Hida K, Koyanagi I, Iwasaki Y, Miyasaka K et al. The role of radiotherapy in the management of spinal cord glioma. Int J Radiat Oncol Biol Phys 1995; 33: 323–328.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Patil, C., Patil, T., Lad, S. et al. Complications and outcomes after spinal cord tumor resection in the United States from 1993 to 2002. Spinal Cord 46, 375–379 (2008). https://doi.org/10.1038/sj.sc.3102155
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102155
Keywords
This article is cited by
-
Effect of race, sex, and socioeconomic factors on overall survival following the resection of intramedullary spinal cord tumors
Journal of Neuro-Oncology (2023)
-
Efficacy analysis of two surgical treatments for thoracic and lumbar intraspinal tumours
BMC Surgery (2019)
-
Management and outcome in adult intramedullary spinal cord tumours: a 20-year single institution experience
BMC Research Notes (2014)