Abstract
Study Design:
Retrospective chart review.
Objectives:
We investigated the morbidity associated with Proteus bacteriuria in a spinal cord injured (SCI) population.
Setting:
Michael E DeBakey Veterans Affairs Medical Center in Houston, Texas, USA.
Methods:
We reviewed the medical records of all veterans with SCI who received care in our medical center during the past 3 years. Proteus bacteriuria was defined as the growth of Proteus species in any urine culture during the study period. Urinary stones were defined as either renal or bladder calculi.
Results:
During the study period, 71 of the 501 subjects (14%) had Proteus and 90 (18%) had urinary stones. Twenty-seven percent of the subjects with Proteus had stones, and the association of Proteus with stones was significant (P<0.05). Proteus bacteriuria was likewise associated with complete injury, hospitalization, decubitus ulcers, and history of stones (P<0.001). Subjects using indwelling catheters, either transurethral or suprapubic, were significantly more likely to have Proteus, whereas subjects practising spontaneous voiding and clean intermittent catheterization were significantly less likely to have Proteus. In the 90 patients with stones, Proteus was associated with requiring treatment for stones and having multiple stones (P<0.01). Twenty-five of the 90 patients with stones (28%) required treatment, most often with lithotripsy, and 6 (7%) developed urosepsis.
Conclusions:
In persons with SCI, Proteus was found in subjects with a greater degree of impairment who were more likely to be hospitalized, to have decubiti, and to use indwelling catheters. Bacteriuria with Proteus predicted urologic complications in persons with SCI.
Statement of Ethics:
All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Sponsorship:
This work was supported by USPHS grant HD42014.
Similar content being viewed by others
Introduction
Patients with spinal cord injury (SCI) and neurogenic bladders are at high risk for recurrent urinary tract infections. Predisposing factors include impaired bladder emptying, repeated instrumentation, vesiculoureteral reflux, and indwelling urinary catheters.1 Patients with SCI are also prone to the development of bladder and renal stones.2, 3 One link between chronic bacteriuria and the formation of stones is infection of the urinary tract with urease-producing organisms.4 Urease splits the urea present in urine to form ammonia and carbon dioxide, thus raising urinary pH and causing normally soluble ions to precipitate and form stones.5 Several bacterial species that commonly infect neurogenic bladders can split urease, including Klebsiella, Providencia, Morganella, Pseudomonas, and Proteus. As the Proteus urease has the fastest rate of urea hydrolysis,4, 6 Proteus is the organism most commonly implicated in catheter encrustation, catheter blockage, and stone formation in the urinary tracts of individuals with indwelling catheters. Antimicrobial therapy often fails to eradicate Proteus and other organisms embedded in the crevices of stones.7
Infectious complications of Proteus bacteriuria have been well documented in the general population of persons with indwelling catheters or abnormal urinary tracts.7 However, the outcomes of Proteus bacteriuria specifically in persons with SCI have not been described. Accordingly, we sought to define the relationship in the SCI population between Proteus bacteriuria and the presence of urinary complications, including stones.
Methods
Study design
A retrospective chart review of the electronic medical record was performed on all veterans with SCI who had received care at the Michael E DeBakey Veterans Affairs Medical Center over the 3 previous years, from 1 January 2003 to 2 January 2006. Patients who had undergone urinary diversion/ileostomy were excluded. Demographic information collected included age, time since injury, ethnicity, level of SCI, complete versus incomplete injury, substance abuse (alcohol, illicit drugs, and tobacco), and type of bladder management. In subjects who had more than one type of bladder management during the study period, all methods used were recorded. Thus, each subject could have several types of bladder management. Medical information collected included whether the subject was hospitalized, treated for a decubitus ulcer, treated for diabetes, developed urosepsis, had a prior history of stones, or required treatment for stones during the study period.
Microbiology
All urine cultures collected from subjects during the study period were reviewed. Any organism identified to the genus level was recorded. Proteus bacteriuria was defined as the growth of Proteus species in any urine culture during the study period. Urinalysis data were collected from all urine specimens corresponding to a documented episode of Proteus bacteriuria.
Definitions of stones
Stones were defined as either renal or bladder calculi during the 3-year time frame of the study. Multiple stones was defined as the presence of >1 stone during the time period, regardless of whether the multiple stones were present at the same time or separated in time. Treatments for stones included nephrostomy tube placement, lithotripsy, and surgical removal.
Statistical analysis
Data were compared using SAS (Release 8.2). The Fisher exact test was used for all pairwise comparisons, and logistic regression was used for multivariate analysis.
Results
Demographics
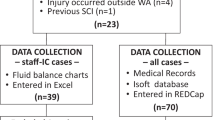
Our medical center currently serves 596 veterans with SCI. We excluded a total of 95 patients for not being seen at our medical center during the study period (71 patients) or for having had urinary diversion (24 patients). Demographic information on the remaining 501 subjects is shown in Table 1. The median age was 57.5 years (interquartile range 50–63 years) and the median time since injury was 15 years (interquartile range 5–26 years). Only 4 subjects had bladder stones, and 1 of these 4 had both bladder and renal stones. The type of bladder management from the most common to the least common was clean intermittent catheterization (N=230), spontaneous voiding (N=136), indwelling Foley catheter (N=99), external condom catheter (N=98), and suprapubic tube (N=56).
Medical conditions
The following conditions were associated with having Proteus bacteriuria: complete injury, hospitalization, decubitus ulcer, and a history of stones (Table 2). Veterans with tobacco abuse were less likely to have Proteus in the urine. Complete injury, hospitalization, decubitus ulcer, and tobacco abuse remained significant predictors in multivariate analysis (P<0.02). Only hospitalization, decubitus ulcer, and a history of stones were associated with having stones (Table 2), and in the multivariate analysis only decubitus ulcer and a history of stones remained significant predictors of stones (P<0.03). Not surprisingly, hospitalization was significantly associated with decubitus ulcer (P<0.0001). Time since SCI did not prove to be significantly related to Proteus bacteriuria, decubitus ulcer, stones, or type of bladder management.
Microbiology
Many of the bacterial species cultured from subjects' urine were strongly associated with having Proteus bacteriuria during the study period. These organisms included Staphylococcus aureus, Enterococcus, Escherichia coli, Pseudomonas, Morganella, group B Streptococcus, Providencia, and Candida (P<0.001). Serratia was also significantly associated with Proteus bacteriuria (P<0.04). A statistically insignificant trend was noted between Acinetobacter and Proteus bacteriuria (P=0.06). Organisms not significantly associated with Proteus bacteriuria included Enterobacter, Klebsiella, Citrobacter, and Alcaligenes. Of the 71 subjects diagnosed with Proteus in their urine at some point during the study period, 19 (27%) were also diagnosed with stones (P=0.045). Other organisms associated with the presence of stones included Enterococcus, Klebsiella, Pseudomonas, Morganella, and Providencia (P<0.05).
Bladder management
Subjects using indwelling catheters, either transurethral or suprapubic, were significantly more likely to have Proteus bacteriuria (P<0.001), whereas subjects practising spontaneous voiding and clean intermittent catheterization were significantly less likely to have Proteus bacteriuria (P<0.01) (Table 3). The association between external catheter use and Proteus was not significant in either direction. Of these types of bladder management, only suprapubic catheters were significantly associated with stones (P=0.04). The association of indwelling catheters with stones nearly reached significance (P=0.08), and spontaneous voiding was nearly significantly protective against having stones (P=0.07). Indwelling Foley catheters, external catheters, and suprapubic catheters were also significantly associated with having decubitus ulcer (P<0.02).
Analysis of subjects with stones
During the study period, 90 SCI patients were diagnosed with either bladder or renal stones. In these subjects, having Proteus bacteriuria was associated with requiring treatment for stones and having multiple stones (P<0.01). Of the 90 patients with stones, 25 (28%) required treatment, most often with lithotripsy (22/25, 88%). Six of the 90 (7%) patients with stones developed urosepsis.
Urinalysis data
When available, urinalysis data were recorded during each episode of Proteus bacteriuria. These results appear in Table 4. Means differ considerably from medians owing to the presence of outliers in each category. For example, one urine sample had 15 429 wbc/hpf, whereas another urine sample had 5100 rbc/hpf. Of note, the urinary pH was slightly basic, as expected. Also, 66% of such urines had large leukocyte esterase and 43% had a positive nitrite test.
Conclusions
Our study confirms that bacteriuria with Proteus predicts urologic complications in persons with SCI. Proteus bacteriuria was more common in persons who had a greater degree of spinal cord impairment, were hospitalized, had decubitus ulcers, and used indwelling catheters. Proteus bacteriuria was associated with having stones, and subjects with both Proteus and stones were more likely to require treatment for stones or have multiple stones. Thus, the presence of Proteus in the bladder is not a benign condition and may be a marker for poor urinary tract health overall.
The association between Proteus bacteriuria and other nosocomial urinary pathogens was not surprising. Several of the less common nosocomial pathogens were not significantly associated with Proteus, such as Alcaligenes, but the very few infections caused by these organisms during our study were unlikely to achieve statistical significance. The lack of association of Enterobacter, Klebsiella, and Citrobacter with Proteus cannot be attributed to low numbers of infections, as these organisms are relatively common. Perhaps these organisms, unlike Proteus, have an equal propensity to infect healthy and diseased urinary tracts. Of the organisms found to be associated with stones, one of these, Enterococcus, does not make urease. We suspect that the strong association of this nosocomial pathogen with Proteus bacteriuria accounts for its association with stones.
Proteus has previously been reported as a common cause of bacteriuria in chronically catheterized residents of long-term care facilities.8 Furthermore, the relationship between Proteus bacteriuria and urinary catheter encrustation and blockage is well documented.9, 10 Proteus bacteriuria has likewise been documented in persons with SCI,1, 11, 12 but not specifically in association with stones. Two retrospective reports published two decades ago of almost 6000 patients with SCI found that bladder calculi were associated with the complete injuries and with Klebsiella bacteriuria.2, 3 In these studies, Proteus bacteriuria was nearly significantly associated with development of bladder stones within 2 years of hospital discharge for initial injury (P=0.06). Renal stones were likewise associated with neurologically complete lesions, and having an indwelling catheter showed a trend toward an association with stones. Thus, our results confirm and expand upon these earlier studies. Our Veterans Affairs Medical Center serves a large and diverse population of SCI patients, so we suspect that our results would also be applicable to other predominantly male SCI populations. As only 2% of our SCI subjects were female, we cannot presume that our results can be generalized to women with SCI.
Our study has several limitations. Like all retrospective studies, we relied on data reported in the medical record. We looked at all urine culture results on SCI subjects during the study period, but we do not know the reason why urine was cultured at a given time. The computerized medical record did not adequately capture data about catheter blockage; hence we were unable to study that outcome. Dates at which catheter management strategies changed were likewise not recorded; therefore, we cannot report a temporal relationship between bladder management strategies and Proteus bacteriuria or stones. We also suspect that the data on substance abuse were unreliable, both because physicians may not always record this information and because patients may not disclose the extent of their substance use. The apparent protective effect of tobacco use on Proteus bladder infection could be attributed to the fact that subjects with lesser degrees of neurological impairment, and thus less likely to have Proteus bacteriuria, had greater opportunities to acquire and smoke cigarettes. As with all observational studies, we can demonstrate associations of various outcomes with Proteus bacteriuria, but we cannot prove causality.
Proteus is extremely difficult to eradicate from the catheterized urinary tract. In a study that investigated the molecular epidemiology of catheter-associated bladder infections with Proteus, the same strain of Proteus persisted in one patient over 121 days despite eight catheter changes, a 20-day period without catheterization, and an 8-day course of antibiotics.9 In our own study of bladder colonization with benign E. coli in patients with SCI and indwelling urinary catheters, we were unable to eradicate Proteus bacteriuria in four of four subjects despite a week of targeted antibiotics accompanied by catheter change during the course of antibiotics.13 Two of these subjects developed catheter encrustation and blockage within <3 weeks. As we have confirmed that the same SCI patients who are infected with Proteus are likely to experience complications such as stones and catheter encrustation, a more effective approach to clearing this organism from the urinary tract is needed. Urinary catheters inflated with triclosan prevented catheter colonization and biofilm formation by Proteus in vitro.14 Microbicins, or natural antibiotics produced by bacteria, may offer another defensive strategy against Proteus, but as yet we have only used microbicins against E. coli in vitro.15 The data that we have collected on the conditions associated with Proteus bacteriuria in SCI patients indicate that bladder colonization with Proteus is harmful, and we anticipate using this information to design future clinical studies targeting this pathogen.
References
Stover S, Lloyd K, Waites K, Jackson A . Urinary tract infection in spinal cord injury. Arch Phys Med Rehabil 1989; 70: 47–54.
DeVivo MJ, Fine PR, Cutter GR, Maetz HM . The risk of renal calculi in spinal cord injury patients. J Urol 1984; 131: 857–860.
DeVivo MJ, Fine PR, Cutter GR, Maetz HM . The risk of bladder calculi in patients with spinal cord injuries. Arch Intern Med 1985; 145: 428–430.
Rodman JS . Struvite stones. Nephron 1999; 81: 9–50.
Li X, Zhao H, Lockatell CV, Drachenberg CB, Johnson DE, Mobley HL . Visualization of Proteus mirabilis within the matrix of urease-induced bladder stones during experimental urinary tract infection. Infect Immun 2002; 70: 389–394.
Jones BD, Mobley HL . Genetic and biochemical diversity of ureases of Proteus, Providencia, and Morganella species isolated from urinary tract infection. Infect Immun 1987; 55: 2198–2203.
Mobley HL, Belas R . Swarming and pathogenicity of Proteus mirabilis in the urinary tract. Trends Microbiol 1995; 3: 280–284.
Warren J, Tenney J, Hoopes J, Muncle H, Anthony W . A prospective microbiologic study of bacteriuria in patients with chronic indwelling urethral catheters. J Infect Dis 1982; 146: 719–723.
Sabbuba N, Mahenthiralingam E, Stickler D . Molecular epidemiology of Proteus mirabilis infections of the catheterized urinary tract. J Clin Micro 2003; 41: 4961–4965.
Stickler D, Ganderton L, King J, Nettleton J, Winters C . Proteus mirabilis biofilms and the encrustation of urethral catheters. Urol Res 1993; 21: 407–411.
Biering-Sorensen F, Bagi P, Hoiby N . Urinary tract infections in patients with spinal cord lesions: treatment and prevention. Drugs 2001; 61: 1275–1287.
Waites KB, Canupp KC, DeVivo MJ . Epidemiology and risk factors for urinary tract infection following spinal cord injury. Arch Phys Med Rehabil 1993; 74: 691–695.
Trautner BW, Hull RA, Thornby JI, Darouiche RO . Coating urinary catheters with an avirulent strain of Escherichia coli as a means to establish asymptomatic colonization. Infect Control Hosp Epidemiol (in press).
Jones GL, Muller CT, O'Reilly M, Stickler DJ . Effect of triclosan on the development of bacterial biofilms by urinary tract pathogens on urinary catheters. J Antimicrob Chemother 2006; 57: 266–272.
Trautner BW, Hull RA, Darouiche RO . Colicins prevent colonization of urinary catheters. Journal of Antimicrobial Chemotherapy 2005; 56: 413–415.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Hung, E., Darouiche, R. & Trautner, B. Proteus bacteriuria is associated with significant morbidity in spinal cord injury. Spinal Cord 45, 616–620 (2007). https://doi.org/10.1038/sj.sc.3102004
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3102004
Keywords
This article is cited by
-
Current insights into the mechanisms and management of infection stones
Nature Reviews Urology (2019)
-
Quality of Life and Bladder Management post Spinal Cord Injury: A Systematic Review
Applied Research in Quality of Life (2014)
-
The encrustation and blockage of long-term indwelling bladder catheters: a way forward in prevention and control
Spinal Cord (2010)
-
US Experience With Bladder Management Following Spinal Cord Injury
Current Bladder Dysfunction Reports (2010)
-
Infarction of middle third posterior cortex of kidney: a complication of extended pyelolithotomy, intra-operative electrohydraulic lithotripsy and extraction of calyceal stones under vision using stone basket and flexible cystoscope in a spinal cord injury patient – a case report
Cases Journal (2009)