Abstract
Study design:
Transversal.
Objectives:
The few studies concerning maximal static mouth respiratory pressures in patients with spinal cord lesions suggest a marked reduction. We studied the correlation of these parameters with the motor level of injury.
Setting:
Rehabilitation Center, Brasília/DF, Brazil.
Methods:
One hundred and thirty-one patients with traumatic spinal cord injury (C4–L3) were recruited. The participants were assessed by standard spirometry and maximal static mouth respiratory pressure.
Results:
Forced vital capacity was most reduced in tetraplegics (subgroup C4–C5, 49%±25 predicted) and increase successively for each descending subgroup (C6–C8, 61%±22 predicted; T1–T6, 70%±15 predicted), becoming normal in low paraplegia (T7–L3, 84%±15 predicted). There is no evidence of an obstructive disturbance throughout all groups. The lowest average percent predicted of maximal static inspiratory pressure (MIP) was in the subgroup C4–C5 (50%±23). The average percent predicted of maximal static expiratory pressure (MEP) improved from 19%±14 in the C4–C5 subgroup to 51%±19 for T7–L3 subgroup. The average percent predicted of all participants for MIP was 74%±30 and for MEP was 37%±21. In patients with complete motor lesion, the correlation with the level of injury was stronger for MEP (r=0.81, P<0.0001; r2=0.65) than for MIP (r=0.62, P=0.004; r2=0.38). No correlation was found among incomplete motor lesion patients.
Conclusions:
The linear regression equations for the relationship of percent predicted MIP or MEP to level of injury are applicable only to complete motor lesions and may be useful to establish normative association between them.
Similar content being viewed by others
Introduction
The high frequency of respiratory complications in patients with spinal cord lesions, especially those with tetraplegia,1 clearly contributes to their morbidity and mortality rates.2, 3 The most important pulmonary function change is a nonparenchymatous pulmonary restriction,4, 5 owing to weakness or paralysis of respiratory muscles.6, 7
Maximal static mouth respiratory pressures are used in the evaluation of respiratory muscle strength.8 Studies in patients with spinal cord lesions are infrequent, but point to a reduction over wide range in these parameters. These reports, however, have not attempted to correlate the reduction in pressures with the motor level of the spinal cord lesion.6, 9, 10, 11 The aim of this study is to measure the maximal static respiratory pressures, expressed as percentage of predicted, in patients with spinal cord injury, correlated with the motor level of the injury. We hope, thereby, to improve interpretation of the pulmonary dysfunction in these patients.
Materials and methods
Subjects
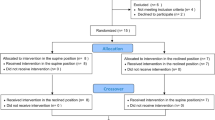
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. The hospital's ethics committee reviewed and approved the study. The investigation was fully explained to and formal written consent obtained from each participant. All patients were drawn from the spinal cord injury rehabilitation program of Hospital Sarah, Brasilia. From August 2003 to February 2005, 131 otherwise healthy patients with traumatic spinal cord injury were recruited for study.
All study subjects were clinically stable and without prior history of pulmonary or other neurological disease. None of the selected participants required the use of a cervical orthosis or body jacket for postural stability at the time of testing.
The level and severity of the lesion was defined by physical examination in accordance with the criteria of the American Spinal Injury Association (ASIA).12 The patients showed lesions from C4 to L3. The 52 patients with tetraplegia (39.7%) were divided into two subgroups by the level of the motor lesion, upper (30 patients, C4–C5) and lower (22 patients, C6–C8). The 79 patients with paraplegia (60.3%) were similarly divided into two subgroups, upper (32 patients, T1–T6) and lower (47 patients, T7–L3) thoracolumbar spinal cord injury.
Prevalence of current or former smokers was 32.1% (CI95%, 24.2–40.8) without difference between groups and subgroups. Gender, ASIA, age, weight, height, and time since injury, also showed no differences between the groups and subgroups (Table 1).
Procedures
A single investigator (SRMM) conducted all spirometry and maximal static respiratory pressure tests, in that sequence, during the afternoon, in the respiratory function laboratory of the institution. All participants were tested seated in their own wheelchairs and, if the case, without abdominal binder. A standard nose clip was used for the examinations.
The forced spirometry (Master Screen, Erich Jaeger GmbH, Hoechberg, Germany) was obtained observing the criteria of American Thoracic Society (ATS).13 Crapo's14 equation was adopted for predicted values. In some individuals, reproducible efforts were deemed acceptable despite back-extrapolated volumes in excess of standard limits and/or despite forced expiratory times lasting less than 6 s, as has been previously validated for subjects with cervical spinal cord injury.15 Immediately following spirometry, the participants were instructed in the procedures and were acquainted with the equipment (DataSpir 120D, Sibelmed, Barcelona, Spain) for maximal static mouth respiratory pressures measurement. Because of possible learning effect, a set of at least four successive measurements for each technique, maximal static inspiratory pressure (MIP) and maximal static expiratory pressure (MEP), were obtained from subjects in a random sequence of the set. The highest value of each maneuver was used. The patient effort and occlusion time of the system, during the measurement, was a minimum of 2 s. For quality control and assurance, we applied Ringqvist's criteria.16 The patients could not see their efforts on the screen of the computer and therefore did not get visual feedback. However, they received verbal encouragement. The physical limitations of the patient were always respected allowing variable rest times between measurements as required.
All pressure measurements were conducted using a rigid tube style mouth piece (Figure 1A). This mouth piece was firmly connected to a nonflexible 17 cm long tube (Figure 1B). At the other end of this tube, there are three fittings: a 2 mm diameter by 40 mm long pressure relief port that avoids the closure of the glottis (Figure 1C); a flexible connector to the pressure transducer (Figure 1D; range 0–300 cmH2O; resolution 1 cmH2O; accuracy 3%; sample rate 100 Hz); and a sliding shutter valve (Figure 1E). Rigid adherence to the operational technical details was maintained throughout the study to insure comparable results. The sliding shutter valve must be closed during the apnea phase in the moment just before each forced inspiratory or expiratory command (Figure 1F) and the mouthpiece must be firmly sealed against the lips by the operator (Figure 1G).
Details of the method for measurement of the maximum static respiratory pressures. The rigid mouth piece (A) is connected to a rigid 17 cm long transparent tube (B). At the distal end of B there is an orifice (C) 2 mm diameter by 4.0 mm long permitting air to escape. A flexible plastic tube is connected to a metal fitting on the side of the tube for the measurement of pressure (D). A 1.5-cm orifice that can be occluded by the sliding valve (E) is controlled by the technician (F). The technician is also responsible for maintaining the seal between the mouth piece and the lips and cheeks (G)
Pressure was registered with the system occluded at total pulmonary capacity for MEP and at residual volume for MIP. The record of the peak pressure obtained after the first second following initiation of the forced maneuver and sustained for at least 1 s, was used for analysis. This single point was chosen by the computer software program (Figure 2). We adopted the estimates of Black and Hyatt17 for the predicted values of respiratory pressures (Appendix) because of their wide acceptance and similarity to our methodology. The spirometry equipment was calibrated at the beginning of each session using a three-litre syringe and the respiratory pressure apparatus using a water column, exactly following the manufacturer's recommendations. Spirometry and static maximal pressures signals were recorded by the computer.
Statistical analysis
A comparative analysis was performed on paraplegics and tetraplegic groups and respective subgroups. Following the lead of other authors,4, 5 relationships between MIP and MEP and injury level were assessed using simple regression analysis by assigning a corresponding numerical value between 1 and 23 to neurological levels C1 through L3. If the motor level of injury varied between sides, the highest one was considered for the analysis. Independent of ASIA classification, the number of participants at each motor level varied from 1 to 17. Average values were calculated for each level. This method was used to minimize bias related to the discrepancy in the number of observations at each level. Thus, the correlative analysis consisted of different points representing the motor levels available for evaluation of MIP and MEP, analyzed also by completeness of the lesion (ASIA A/B and C/D).
Continuous variables were expressed as the average and standard deviation and analyzed by the Student's t-test and analysis of variance, complemented with Bonferroni correction (post hoc). For proportions comparisons, we utilized χ2 test. The occurrence of a type I error was estimated by a P-value <0.05. All statistical analysis was conducted using SPSS (version 13).
Results
The percent predicted forced vital capacity (FVC) and forced expiratory volume in 1 s (FEV1) differed among subgroups. The restrictive pulmonary pattern was most marked in high tetraplegia (C4–C5, FVC 49%±25 predicted) and lessened successively for each descending subgroup (C6–C8, 61%±22 predicted; T1–T6, 70%±15 predicted), becoming normal in low paraplegia (T7–L3, 84%±15 predicted) (Figure 3). The ratio FEV1/FVC × 100 was normal (> 80%) and similar throughout all groups, showing no evidence of an obstructive disturbance (Table 2).
The lowest average percent predicted MIP was in the subgroup C4–C5 (50%±23 predicted). In the other three subgroups, the average MIP was similar and greater than 69% predicted. The percent predicted MEP differed between subgroups (P<0.001), improving from 19%±14 in the C4–C5 subgroup to 51%±19 for T7–L3 subgroup (Figure 3). The average of the percent predicted of all participants for MIP was 74%±30 and for MEP was 37%±21 (Table 2).
Significant correlation was found only for complete motor lesion levels (ASIA A and B) and the average percent predicted of the maximal static respiratory pressures (99 patients, 19 points). The correlation for MEP (r=0.81, P<0.0001; r2=0.65) was stronger than for MIP (r=0.62, P=0.004; r2=0.38). Figure 4 presents these analyses with their respective equations. No correlation was found for MIP and MEP in incomplete motor lesion patients (32 participants).
Simple linear regression, correlation coefficients (r), and the equations for the percent predicted of MIP (top) and MEP (bottom) and level of complete motor lesion. Vertical bars and numbers represent the range of values at each level and the number of subjects in both measurements. Broken line represents the 95% confidence interval limits
Discussion
A group of selected traumatic spinal cord injured patients showed a clear range of restrictive ventilatory disturbance that varied dependent on the 21 different motor levels studied. The FVC change varied from a maximal impairment in the high cervical lesions (C4–C5) to complete normality in the low thoracolumbar lesions (T7–L3). Similarly, the average percent predicted of maximal static mouth respiratory pressures improved from higher to lower levels of injury. The main difference between these pressure measurements was that MEP was more severely impaired than MIP. Thus, the highest mean percent predicted value for MEP was equal to the lowest one achieved for MIP. The maximal static mouth expiratory pressure was impaired in all spinal cord injured patients. The maximal static mouth pressure correlates with level of injury only for complete motor injured patients. This correlation was better for MEP than MIP.
Spirometry has been the most frequently used measurement of respiratory muscle function in spinal cord lesion patients.4, 5 Although theoretically important, maximal static respiratory pressures have not played as great a clinical role in the evaluation of the respiratory muscles. Thirty-three articles were found that measured maximal static respiratory pressures in patients with spinal cord injury (March 2006, Medline, Embase, Cinahl, Pedro, and Lilacs) (Supplementary Information on the journal's web site). Lack of standard equations for predicted values, differences in equipment, and methodology add difficulty to the analysis of the research on this topic. Of these 33 articles, only eight describe the type of mouth piece, 11 describe the presence and size of a pressure relief port, varying from 0.5 to 1.8 mm, and 11 report the minimum time of respiratory effort. Eight of 33 applied predictive equations to the analysis, five used Black and Hyatt,17 two Wilson et al,18 and one Rochester,19 with the rest considering only the absolute values.
In view of the variability and diversity of available equipment and methodology, it seems important to describe the laboratory procedure in detail. Our protocol was chosen based on criteria of easy applicability and reproducibility in obtaining maximal static mouth respiratory pressures. The equation of Black and Hyatt17 for prediction of maximal static mouth respiratory pressures was chosen considering the similarity of their methodology to our protocol, although we detail some small differences. This method is the current routine for all our patients with spinal cord injury. Standardized methodology provides a better basis from which to analyze the data in patients with lesions from C4 to L3.
The rigid tube style mouth piece was chosen as it is the most appropriate in the general population,20 as well as patients with spinal cord lesions.6 A pressure relief escape of 2 mm diameter by 40 mm length has been shown to be the most effective in avoidance of closure of the glottis.8 It also minimizes the undesirable effects of pressures generated by face muscles during the respiratory force measurement.16, 21 The total pulmonary capacity was adopted as the point from which to measure MEP and residual volume from which to measure MIP. They represent reliably recognized and reproducible points in the respiratory cycle.19 The peak pressure sustained for 1 s just after the first second following initiation of the respiratory effort was chosen because it is reproducible8 and minimizes interference from potential spasticity generated in response to the forced maneuver in some patients with tetraplegia.22 A minimum of four tests of MIP and MEP was conducted avoiding fatigue effects. We accept that there may be difficulty in comparing our results to other published literature. At a minimum, we would encourage others to meticulously detail their methodology.
The current difficulty in comparing the results of studies is exemplified in two small methodological differences between our adopted technique and that of Black and Hyatt.17 Differences in pressure measurements stem from the way a mouthpiece is used rather than the mouthpiece per se.20 Black and Hyatt17 subjects held the mouthpiece, whereas in our protocol it was by the operator. Subject held mouthpieces may favor lower values owing to less secure mouth sealing around the apparatus. Secondly, maximum sustained pressures for 1 s may not be as high as the obtained peak pressure but is believed to be more reproducible.8 In Black and Hyatt17 study, the measured peak pressure was recorded during the first second, whereas we considered the peak pressure just after the first second, favoring higher values in the former. The differences in these two aspects of the both studies are based on differing applicability in patients with spinal cord lesions. Thus, we do not know if these differences affect equivalency and comparability of the results. Moreover, other currently unappreciated methodological aspects may affect the applicability of the Black and Hyatt17 equations to spinal cord lesion patients. As there is currently a lack of specific predictive equation for patients with spinal cord injury, we feel that our data may help the interpretation of MIP and MEP measurements in these patients.
The greater negative impact of spinal cord injury on MEP than MIP has already been well established in the literature.12 However, the strong correlation observed with the exact complete motor level has not been reported previously. This result reinforces the thought that MEP and MIP impairment may have a common origin, related to the segmental nature of the motor neural control of the respiratory muscles, and synergism between inspiration and expiration activity. The diaphragm is the main muscle of inspiration innervated by roots C3–C5 and the reason why MIP is normal in the group patients with lesion below T1 level. The main muscles of expiration are abdominal whose innervations are from T6–T11, although numerous other muscles above and below this level can indirectly participate in forced expiration.23 This peculiarity may explain why all subgroups exhibited average percent predicted MEP below 80% and the better correlation with the level of spinal cord lesion. The mechanical efficiency of the diaphragm depends on its position and the stability of the chest wall, provided mainly by the intercostals and abdominal muscles.23
Then remains the question of how our patients with C4 injury, with phrenic nerve diaphragm innervation impaired, could generate measurable inspiratory pressure. Additionally, how do those with injury above T6, and therefore without abdominal muscle innervation, generate measurable expiratory pressure? In the case of C4 injury, patients may be capable of generating negative inspiratory pressure, through the action of accessory inspiratory muscles, innervated by the cervical plexus, such as stenocleidomastoid and residual diaphragm motor unit recruitment.23 Patients with lesions above T6, may generate expiratory pressure by the action of the clavicular portion of the major pectoral muscle.24, 25
For practical reasons, we attributed an arbitrary unit value for each level of lesion in the correlative analysis. This number may not fully reflect actual difference from one level to another. It may serve only as a gross estimation because the real contribution of each level must be different owing to the varying importance of segmental innervation of the participating muscle groups. As more segmental muscles participate in expiration than in inspiration the discrepancy between levels appears more gradual for MEP than MIP. Other unmeasured factors may be contributing to these results, especially the dependence of pulmonary volumes on the viscoelastic properties of the respiratory system.8
Linear regression equations for the relationship of percent predicted MIP or MEP to complete motor level of injury may be useful to establish normative association between them. The equations are already adjusted for gender and age differences.17 This could be used in detecting associated disorders as distinct from anticipated neurological effects based on spinal cord injury level per se. A discrepancy between the percentages predicted maximal static pressure and the actual measurement might stimulate a search for other related injuries such as phrenic nerve injury or syringomyelia, resultant from the primary traumatic event. We feel that these relationships should be considered in the pulmonary evaluation of patients with spinal cord injury.
References
Mansel JK, Norman JR . Respiratory complications and management of spinal cord injuries. Chest 1990; 97: 1446–1452.
DeVivo MJ et al. Cause of death for patients with spinal cord injuries. Arch Intern Med 1989; 149: 1761–1766.
DeVivo MJ, Black KJ, Stover SL . Causes of death during the first 12 years after spinal cord injury. Arch Phys Med Rehabil 1993; 74: 248–254.
Baydur A, Adkins RH, Milic-Emili J . Lung mechanics in individuals with spinal cord injury: effects of injury level and posture. J Appl Physiol 2001; 90: 405–411.
Linn WS et al. Forced vital capacity in two large outpatient populations with chronic spinal cord injury. Spinal Cord 2001; 39: 263–268.
Tully K et al. Maximal expiratory pressures in spinal cord injury using two mouthpieces. Chest 1997; 112: 113–116.
Uijl SG et al. Training of the respiratory muscles in individuals with tetraplegia. Spinal Cord 1999; 37: 575–579.
Anonymous. ATS/ERS Statement on Respiratory Muscle Testing. Am J Respir Crit Care Med 2002; 166: 518–624.
Gounden P . Static respiratory pressures in patients with post-traumatic tetraplegia. Spinal Cord 1997; 35: 43–47.
Fujiwara T, Hara Y, Chino N . Expiratory function in complete tetraplegics: study of spirometry, maximal expiratory pressure, and muscle activity of pectoralis major and latissimus dorsi muscles. Am J Phys Med Rehabil 1999; 78: 464–469.
Boaventura CM et al. Effect of an abdominal binder on the efficacy of respiratory muscles in seated and supine tetraplegic patients. Physiotherapy 2003; 89: 290–295.
Maynard Jr FM et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord 1997; 35: 266–274.
American Thoracic Society. Standardization of Spirometry, 1994 Update. Am J Respir Crit Care Med 1995; 152: 1107–1136.
Crapo RO, Morris AH, Gardner RM . Reference spirometric values using techniques and equipment that meet ATS recommendations. Am Rev Respir Dis 1981; 123: 659–664.
Ashba J et al. Spirometry-acceptability and reproducibility in spinal cord injured subjects. J Am Paraplegia Soc 1993; 16: 197–203.
Ringqvist T . The ventilatory capacity in healthy subjects. An analysis of causal factors with special reference to the respiratory forces. Scand J Clin Lab Invest Suppl 1966; 88: 5–179.
Black LF, Hyatt RE . Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis 1969; 99: 696–702.
Wilson SH et al. Predicted normal values for maximal respiratory pressures in Caucasian adults and children. Thorax 1984; 39: 535–538.
Rochester DF . Tests of respiratory muscle function. Clin Chest Med 1988; 9: 249–261.
Koulouris N et al. Comparison of two different mouthpieces for the measurement of Pimax and Pemax in normal and weak subjects. Eur Respir J 1988; 1: 863–867.
Mayos M et al. Measurement of maximal static respiratory pressures at the mouth with different air leaks. Chest 1991; 100: 364–366.
De Troyer A, Heilporn A . Respiratory mechanics in quadriplegia. The respiratory function of the intercostal muscles. Am Rev Respir Dis 1980; 122: 591–600.
De Troyer A, Estenne M . Functional anatomy of the respiratory muscles. Clin Chest Med 1988; 9: 175–193.
De Troyer A, Estenne M, Heilporn A . Mechanism of active expiration in tetraplegic subjects. N Engl J Med 1986; 314: 740–744.
Estenne M et al. The effect of pectoralis muscle training in tetraplegic subjects. Am Rev Respir Dis 1989; 139: 1218–1222.
Author information
Authors and Affiliations
Additional information
All work was performed at Centro Sarah de Formação e Pesquisa, Rede Sarah de Hospitais de Reabilitação – SARAH BRASÍLIA, SMHS Qd 301 Bloco B N 45 2a andar, CEP 70335-901, Brasilia, DF, Brazil
Supplementary Information accompanies the paper on the Spinal Cord website (http://www.nature.com/sc).
Supplementary information
Rights and permissions
About this article
Cite this article
Mateus, S., Beraldo, P. & Horan, T. Maximal static mouth respiratory pressure in spinal cord injured patients: correlation with motor level. Spinal Cord 45, 569–575 (2007). https://doi.org/10.1038/sj.sc.3101998
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101998
Keywords
This article is cited by
-
Locomotor-respiratory coupling in ambulatory adults with incomplete spinal cord injury
Spinal Cord Series and Cases (2022)
-
Diaphragm ultrasonography and pulmonary function tests in patients with spinal cord injury
Spinal Cord (2019)
-
Respiratory Motor Control Disrupted by Spinal Cord Injury: Mechanisms, Evaluation, and Restoration
Translational Stroke Research (2011)