Abstract
Study Design:
Pre-test, post-test study of the relationship between exercise-related changes in feeling states and pain among persons with chronic incomplete spinal cord injury (SCI) who performed three separate exercise sessions consisting of body-weight supported treadmill training (BWSTT).
Objectives:
To determine whether exercise-related changes in feeling states are related to exercise-related changes in pain and in-task pain.
Setting:
Hamilton, Ontario, Canada.
Methods:
A total of 14 men and women with chronic, incomplete SCI (ASIA B and C) performed three exercise sessions of BWSTT. Measures of pain and feeling states were administered before and after each session along with a measure of pain experienced while exercising.
Results:
Participants who experienced greater decreases in pain from pre- to post-exercise also experienced greater improvements in feeling states. Pain experienced during exercise was unrelated to changes in feeling states.
Conclusion:
Among persons with SCI, exercise-related changes in pain can influence the effects of individual exercise bouts on feeling states.
Similar content being viewed by others
Introduction
It is well documented that physical activity plays an important role in the maintenance and promotion of psychological well-being. Indeed, numerous studies involving nondisabled populations have shown that single, acute bouts of physical activity can improve people's feeling states. For instance, in one study, women's feeling states were more positive on days when they had exercised than on days when they had not.1 In another study, men and women who went for a short, 10–15 min walk reported significant improvements in their feeling states relative to study participants who simply sat and read a book.2 Yet, while these findings speak to the psychological benefits of acute activity bouts for the general population, little is known about the psychological effects of acute exercise on people with physical disabilities such as spinal cord injury (SCI).
The dearth of research on this topic is somewhat surprising given that psychological responses to acute exercise bouts could have important health implications for people with disabilities. For example, over time, the accumulation of mood-enhancing exercise bouts could help alleviate more enduring types of mood disturbances, such as clinical depression and anxiety. Furthermore, positive responses to exercise could influence subsequent exercise motivation and adherence; people may be more motivated to adhere to an exercise regimen if they experience post-exercise mood improvements.3 For these reasons, the study of exercise-induced changes in feeling states represents an important avenue for investigation.
Only a handful of studies have examined the acute psychological effects of exercise on people with a disability. One such study was an investigation of patients with knee osteoarthritis (OA). Interestingly, unlike the results typically seen in healthy adults who engage in an acute exercise bout,4 the knee OA patients did not experience a post-exercise improvement in feeling states. Furthermore, those patients who reported the most pain during exercise also reported the most negative post-exercise feeling states. Based on these findings, the study authors suggested that OA patients might not derive feeling state benefits from exercise because exercise can exacerbate the chronic knee pain associated with OA. Increases in pain could, in turn, have a negative effect on their feeling states.
The present experiment examined the relationship between pain and exercise-related changes in feeling states among people with SCI. Given that pain is a common secondary complication of SCI,5 there is value in determining whether pain attenuates the exercise-feeling state relationship. We addressed our research question by examining the effects of exercise – consisting of body-weight supported treadmill training (BWSTT) – on pain and feeling states in people with SCI. It was hypothesized that individuals who experienced more pain during exercise and more pain exacerbation from pre- to post-exercise would report smaller feeling state improvements.
Methods
Participants
Participants were three female and 11 male (Mage=28.8±8.1) volunteers for a 12-month study of BWSTT.6 All had experienced a traumatic, incomplete SCI (ASIA B or C) at least 12 months earlier (Myears post-injury=7.4±6.9). Exclusion criteria were as follows: cardiac pacemaker, unstable angina or documented heart disease, uncontrolled cardiac dysrhythmia, chronic obstructive lung disease, uncontrolled autonomic dysreflexia, recent nontraumatic fracture, tracheostomy, bilateral hip and knee flexion contractures greater than 20°, drug addiction, severe muscle shortening or severe skin ulcerations, age greater than 60 years, or persons greater than 40 years who failed phase 1 of a progressive incremental exercise tolerance test. Four participants had engaged in some form of exercise training within the previous year, but none had engaged in BWSTT. A complete description of the participants is presented in Hicks et al.6
Procedure
The study protocol was approved by the McMaster University Research Ethics Board. All participants provided informed consent. Data for the present investigation were collected during the first three sessions of a larger 144 session (12-month) study of the effects of BWSTT on functional walking ability and subjective well-being.6
Immediately prior to their very first BWSTT session, participants completed the 65-item Profile of Mood States (POMS),7 indicating how they felt at that moment. Total mood disturbance was calculated by subtracting the Vigor subscale score from the sum of the Tension, Depression, Anger, Fatigue and Confusion subscale scores.7 For ease of interpretation, this score was reversed so that higher scores indicated more positive feelings. Participants also completed the single-item Feeling Scale (FS),8 an index of affective response to an exercise bout whereby respondents indicate how they feel ‘right now.’ Participants then rated their current pain by responding to the item ‘how much pain do you have right now’ from the Brief Pain Inventory.9
All training took place on Woodway Loco-system (Woodway USA Inc., Foster, CT, USA) treadmills, which provide body-weight support (BWS) via an overhead pulley system with weight counterbalances. A level of BWS was chosen for the participant that enabled maintenance of an upright trunk without the knees buckling. Treadmill speed was chosen based on participant comfort and safety. Most participants began training with 60% BWS or greater and walked at treadmill speeds ⩽0.6 km/h.6 Each exercise session consisted of three separate bouts of BWSTT. Depending on the participant's tolerance, each bout lasted from 5 to 15 min with a 10 min rest between bouts.
Upon completion of the exercise session (ie, all three bouts), the POMS, FS, and pain scales were readministered along with a single item assessing pain experienced during exercise (ie, in-task pain). Consistent with Focht et al's4 study of knee OA patients, in-task pain was measured at the end of the session in order to get an assessment of pain experienced across the duration of the session. To determine the reliability of any effects, this entire protocol was repeated at the participants' second and third BWSTT sessions, which took place on separate days, later that same week.
Analyses
A general linear model (GLM) repeated measures analysis of variance (ANOVA) was used to assess change in pain at each session. GLM repeated measures ANCOVAs assessed change in the POMS and FS scores at each session, with change in pain treated as a covariate. Simple change scores (Δ) were calculated for each of the study measures, such that positive scores indicated improvements. One-tailed Pearson correlation coefficients were then computed to examine the relationship between changes in mood and pain. For all analyses, α was set at P<0.05.
Results and discussion
There were nonsignificant small- to medium-sized decreases in pain in Sessions 1 (ES (Cohen's d)=0.23) and 2 (ES=0.39), Ps>0.23. No change in pain occurred at Session 3 (ES=0.00). As shown in Table 1, at each session, some participants reported an increase in pain from pre- to post-exercise while others reported a decrease.
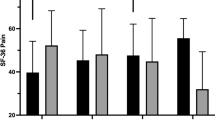
Repeated measures ANCOVAs on the POMS and FS did not reveal any main effects for time (all Ps>0.17). Effect sizes for pre- to post-exercise changes in POMS scores were 0.21, −0.09, and −0.18 for Sessions 1, 2, and 3, respectively. For the FS, effect sizes were 0.31, 0.12, and 0.13 for Sessions 1, 2, and 3, respectively. These values indicate small- to medium-sized changes from pre- to post-exercise. Although the negative POMS effect sizes may be interpreted as a worsening of moods, in exercise studies, negative changes in POMS are typically due to exercise-related increases in somatic symptoms measured by the Fatigue (eg, fatigued, exhausted) and Tension (eg, tense, shaky) subscales.3 When performing bouts of exercise, increases along these somatic dimensions do not necessarily translate into mood decrements. In contrast to the POMS, the FS was designed specifically to measure affective responses to exercise, so its scores are not confounded by exercise-induced changes in somatic symptoms of fatigue and muscular tension. As such, the consistently positive effects detected by the FS may provide a truer picture of people's psychological responses to BWSTT than the POMS scores.
Although there were no main effects for time in the analyses of the POMS and FS scores, time interacted significantly with the covariate of Δ pain in most of the analyses. For the POMS, a significant time × Δ pain interaction emerged at Sessions 1 and 3 (Ps<0.05), and the interaction approached significance at Session 2 (P=0.09). For the FS, significant time × Δ pain interactions emerged at Sessions 2 and 3 (P<0.01). These interactions indicate that the magnitude of mood change depended on the magnitude of pain change.
Indeed, as hypothesized, correlational analyses revealed that changes in pain were significantly, negatively correlated with changes in feeling states. The participants who experienced the greatest decreases in pain also experienced the greatest improvements on the POMS and FS. This was a robust finding; Δ pain significantly correlated with ΔPOMS at 3/3 exercise sessions and ΔFS at 2/3 sessions. Although the correlational design of this study precludes assumptions of causality, our findings suggest that pain reductions experienced in conjunction with BWSTT may contribute to improvements in feeling states following BWSTT.
With regard to in-task pain, participants reported moderate pain during each exercise session. However, contrary to hypothesis, in-task pain was unrelated to feeling state changes – a finding in opposition to Focht et al's4 study of OA patients. Perhaps in-task pain is overridden by other positive thoughts and feelings that can occur during BWSTT (eg, a sense of accomplishment, excitement about standing upright, tingling sensations in the legs),10 which, in turn, may have a greater impact on post-exercise feelings. Another possibility is that in-task pain simply has less impact on post-exercise feeling states than post-exercise pain.
It should also be noted that a different in-task pain measurement protocol could yield different results. We used the same measurement protocol as Focht et al, and assessed in-task pain as a summative, retrospective evaluation at the end of the day's exercise session. With such an approach, it is unclear whether participants are truly reporting the average amount of pain they experienced while exercising. For instance, their recall may be biased by the most intense pain experienced during the session, even if it only lasted for a couple of minutes. Because this experiment was conducted during participants' very first experiences with BWSTT, an experience that could be quite physically, cognitively, and emotionally taxing, we did not want to burden them with multiple measures of pain while they were on the treadmill. Nevertheless, had we measured pain during the three bouts at each exercise session, it is possible that these truly in-task measures of pain would have been significantly correlated with changes in the POMS and FS. As such, our measure of in-task pain is a limitation of this study.
Another limitation is the study's sample size. Sample sizes are notoriously small in exercise training studies involving people with SCI,11 and our investigation was no exception. A greater number of participants would have afforded greater statistical power for detecting significant changes in the feeling state and pain measures. Also, the generalizability of our findings are limited to people with the narrowly defined range of injuries included in this study.
In summary, the present data indicate that BWSTT-induced changes in pain are associated with BWSTT-induced changes in feeling states. Decreased pain has been identified as a mechanism by which long-term exercise training enhances relatively enduring aspects of psychological well-being (eg, depression, stress) in people with SCI.12, 13, 14 The present findings highlight the utility of conducting further investigations to determine if changes in pain mediate the acute psychological effects of BWSTT and other types of exercise. Such investigations would be valuable for determining the therapeutic benefits of exercise for improving psychological well-being among people with SCI.
References
Gauvin L, Rejeski WJ, Reboussin BA . Contributions of acute bouts of vigorous physical activity to explaining diurnal variations in feeling states in active, middle-aged women. Health Psychol 2000; 19: 365–375.
Ekkekakis P, Hall EE, VanLanduyt LM, Petruzzello SJ . Walking in (affective) circles: can short walks enhance affect? J Behav Med 2000; 23: 245–275.
Gauvin L, Spence JC . In: Duda JL (ed). Advances in Sport and Exercise Psychology Measurement. Fitness Information Technology: Morgantown, WV 1998, pp 325–336.
Focht BC, Gauvin L, Rejeski WJ . The contribution of daily experiences and acute exercise to fluctuations in daily feeling states among older, obese adults with knee osteoarthritis. J Behav Med 2004; 27: 101–121.
Jensen MP, Hoffman AJ, Cardenas DD . Chronic pain in individuals with spinal cord injury: a survey and longitudinal study. Spinal Cord 2005; 43: 704–712.
Hicks AL et al. Long-term body-weight-supported treadmill training and subsequent follow-up in persons with chronic SCI: effects on functional walking ability and measures of subjective well-being. Spinal Cord 2005; 43: 291–298.
McNair D, Lorr M, Droppleman LF . Manual for the Profile of Mood States. Educational and Industrial Testing Service: San Diego, CA 1971.
Hardy CJ, Rejeski WJ . Not what but how one feels: the measurement of affect furing exercise. J Sport Exercise Psychol 1989; 11: 304–317.
Cleeland CS . In: Osoba D (ed). Effect of Cancer on Quality of Life. CRC Press: Boca Raton, FL 1991, pp 293–305.
Semerjian TZ, Montague SM, Dominguez JF, Davidian AM, de Leon RD . Enhancement of quality of life and body satisfaction through the use of adapted exercise devices for individuals with spinal cord injuries. Topics Spinal Cord Injury Rehabil 2005; 11: 95–108.
Martin Ginis KA, Hicks AL . Exercise research issues in the spinal cord injured population. Exercise Sport Sci Rev 2005; 33: 49–53.
Martin Ginis KA et al. Using physical activity to enhance subjective well-being among people with spinal cord injury: the mediating influences of stress and pain. Rehabil Psychol 2003; 48: 157–164.
Latimer AE, Martin Ginis KA, Hicks AL, McCartney N . An examination of mechanisms of exercise-induced change in pain and physical and psychological well-being among people with spinal cord injury. J Rehabil Res Dev 2004; 41: 643–652.
Martin Ginis KA, Latimer AE, Francoeur C, Hanley H, Watson K . Sustaining exercise motivation and participation among people with spinal cord injuries: lessons learned from a 9-month intervention. Palaestra 2002; 18: 38–42.
Acknowledgements
This research was supported by a grant from the Ontario Neurotrauma Foundation. The manuscript preparation was supported by a Canadian Institutes of Health Research (CIHR) New Investigator Award, awarded to KA Martin Ginis.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Martin Ginis, K., Latimer, A. The effects of single bouts of body-weight supported treadmill training on the feeling states of people with spinal cord injury. Spinal Cord 45, 112–115 (2007). https://doi.org/10.1038/sj.sc.3101911
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101911
Keywords
This article is cited by
-
The effects of active upper-limb versus passive lower-limb exercise on quality of life among individuals with motor-complete spinal cord injury
Spinal Cord (2022)
-
Physical activity interventions, chronic pain, and subjective well-being among persons with spinal cord injury: a systematic scoping review
Spinal Cord (2021)
-
An examination of diurnal variations in neuropathic pain and affect, on exercise and non-exercise days, in adults with spinal cord injury
Spinal Cord Series and Cases (2018)
-
Strength training versus robot-assisted gait training after incomplete spinal cord injury: a randomized pilot study in patients depending on walking assistance
Journal of NeuroEngineering and Rehabilitation (2014)
-
Effectiveness of Non-pharmacological and Non-surgical Interventions to Support Pain Management after Spinal Cord Injury
HeilberufeScience (2010)