Abstract
The novel antipsychotic aripiprazole requires high (>90%) striatal D2 receptor occupancy (D2RO) to be clinically active, but despite its high D2RO it does not show extrapyramidal symptoms. While most antipsychotics are active at nearly 65% D2RO, they show motor side effects when D2RO exceeds 80%. We investigated this discrepancy between D2RO, 5HT2 receptor occupancy (5-HT2RO) and in vivo functional activity of aripiprazole in comparison to haloperidol (typical) and risperidone (atypical) in animal models. All three drugs showed dose-dependent D2RO. While risperidone clearly showed higher 5-HT2RO than D2RO, aripiprazole and haloperidol showed higher D2RO than 5-HT2RO at all doses. Haloperidol and risperidone induced catalepsy at doses producing >80% D2RO, while aripiprazole despite higher D2RO (>90%) induced no catalepsy. Haloperidol and risperidone's ED50 values for inhibition of conditioned avoidance response (CAR) and amphetamine-induced locomotor activity (AIL) corresponded to ∼60% D2RO. In contrast, aripiprazole showed a significant dissociation; while it blocked AIL at similar D2RO, a 23-fold higher dose (86% D2RO) was required to inhibit CAR. FOS expression in shell region of the nucleus accumbens was significant for all drugs at D2ROs that were effective in CAR. However, in the core region of the nucleus accumbens and dorsolateral striatum, aripiprazole differed from the others in that despite high D2RO it induced low FOS. Haloperidol and risperidone showed dose/occupancy-dependent prolactin elevations, while aripiprazole did not. Across models, haloperidol and risperidone show similar occupancy-functional antagonism of the D2 system, while aripiprazole shows a clear dissociation. Partial agonism of aripiprazole offers a good explanation for this dissociation and provides a framework for understanding occupancy-functional relationships of partial D2 agonist antipsychotics.
Similar content being viewed by others
INTRODUCTION
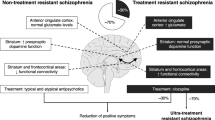
The clinical effect of many antipsychotics emerge when 60–70% of striatal dopamine D2 receptors are blocked, and motor side effects become prominent when the receptor blockade exceeds 80% (Farde et al, 1988; Kapur et al, 2000a). This pattern of relationship between striatal D2 receptor occupancy (D2RO) and clinical efficacy has also been shown in animal occupancy studies using conditioned avoidance response (CAR) as a surrogate for antipsychotic efficacy and catalepsy (CAT) as a surrogate for motor side effects (Wadenberg et al, 2000). Similar to human subjects, CAT was observed in animals receiving haloperidol, risperidone, and olanzapine at doses that exceed 80% D2RO while they were effective in inhibiting CAR at lower D2RO (Wadenberg et al, 2001b).
These relationships between D2RO and functional effects have been derived from antipsychotics that are antagonists at the dopamine D2 receptor. In this context, the introduction of aripiprazole is of interest because while clinically it has all the features of an atypical antipsychotic (antipsychotic effect with very low motor side effects) (Kane et al, 2002; Potkin et al, 2003), it differs from all other antipsychotics in that it is a partial D2 receptor agonist (Burris et al, 2002). Aripiprazole has been demonstrated to be a partial D2 agonist in vitro as it acts like an antagonist in the presence of dopamine, while in dopamine's absence it increases dopamine transmission in several cell lines expressing cloned human dopamine D2L receptors (Lawler et al, 1999; Burris et al, 2002; Shapiro et al, 2003). However, the degree of aripiprazole's partial agonism seems to be dependent upon the cell-line and assay conditions used and in certain assays it shows no intrinsic efficacy (Lawler et al, 1999). So while an absolute number of its intrinsic efficacy cannot be deduced based on in vitro assays, the inability of aripiprazole in vivo to increase locomotion in a hypodopaminergic condition (reserpinized rats) suggests weak partial agonism (Kikuchi et al, 1995). The functional effects of aripiprazole are further complicated by the fact that it shows preferential activity at the presynaptic dopamine autoreceptors (which would decrease dopamine levels), while showing partial agonism at the postsynaptic dopaminergic transmission (which could, in theory increase or decrease transmission depending upon the endogenous tone) (Kikuchi et al, 1995). Further, it has been suggested that the overall effect of aripiprazole's partial agonism is dependent upon the ‘receptor reserve’ within the system (Burris et al, 2002), although it remains unclear how much receptor reserve exists in the dopamine D2-relevant systems. These complexities make it impossible, based on in vitro considerations alone, to predict the net effect of aripiprazole's D2RO on functions dependent upon D2 transmission.
The clinical PET data on aripiprazole are intriguing. In a study of aripiprazole, healthy volunteers treated for 2 weeks with a dose of 2 mg/day showed D2RO between 70 and 80% of dopamine receptors in the putamen, while a dose of 30 mg/day showed an occupancy of nearly 95% with an incidence of extrapyramidal symptoms (EPS) no higher than with placebo (Yokoi et al, 2002). Two important facts emerge. First, unlike other antipsychotics, which lead to clinical efficacy at 60–65% D2RO, aripiprazole seems to be effective only at doses which occupy >90% receptors (doses of 15–30 mg/day). Second, despite >90% occupancy, the incidence of EPS in normal volunteers and patients does not exceed that of placebo (Kane et al, 2002; Potkin et al, 2003). Thus, there appears to be a dissociation between the degree to which receptors are blocked (occupancy) and expression of functional antagonism (antipsychotic effects and extrapyramidal side effects) when compared to existing antipsychotic agents.
Finally, aripiprazole has affinity not only to D2 receptors but also to the serotonin 5-HT2 receptors. With the exception of amisulpride, all widely used atypical antipsychotics show a higher affinity for 5-HT2 than D2 receptors, and this has been suggested to play a key role in their atypical antipsychotic action (Meltzer, 1999). Aripiprazole is unique in this regard as its D2 affinity exceeds its 5-HT2 affinity (Lawler et al, 1999). However its relative 5-HT2/D2 occupancies have not been investigated in vivo in animals or humans. At present, it is unknown if aripiprazole shows a high 5-HT2RO in vivo, or like amisulpride, it is an atypical antipsychotic with low 5-HT2RO.
To resolve some of these issues, the objective of the present study was to examine aripiprazole's relationship (and possible dissociation) between in vivo receptor occupancy (D2 as well as 5-HT2) and functional antagonism in a series of convergent animal models commonly used to asses and predict antipsychotic, motor, and neuroendocrine effects. We chose the following models/indices: (a) CAR, AIL, spontaneous motor activity, and FOS induction in the shell of the nucleus accumbens as markers/predictors of antipsychotic effect (Deutch et al, 1992; Arnt et al, 1997); (b) CAT and FOS expression in the core of the nucleus accumbens and dorsolateral striatum as markers/predictors of motor liability (Robertson et al, 1994; Hoffman and Donovan, 1995; Deutch et al, 1992); and (c) plasma prolactin levels as an endocrine marker. To put these findings in a comparative context, we compared aripiprazole to two widely used and clinically studied antipsychotics: haloperidol, a classical typical antipsychotic agent, and risperidone, one of the most widely used atypical agents (Miyamoto et al, 2005).
MATERIALS AND METHODS
Animals
Adult male Sprague–Dawley rats weighing 250–275 g were procured from Charles River Laboratories, Montreal, Canada. They were housed under reversed lighting conditions (12 h reverse light/dark cycle—lights off at 0800), with access to food and water ad libitum. The animals were allowed to acclimatize to the vivarium for a minimum of 5 days before being used for experimentation. All experiments were approved by the institute's animal care committee.
Drugs
Haloperidol (Sabex Inc., Boucherville, QC, Canada), risperidone (Sigma-Aldrich, St Louis, MO, USA), and aripiprazole (a gift from Eli Lilly, Indianapolis, IN, USA) were used in the study. Aripiprazole was dissolved in 30% dimethylformamide (in physiological saline), while the other drugs were dissolved in 1–2% glacial acetic acid and made up to volume with physiological saline. d-Amphetamine sulfate was obtained from US Pharmacopoeia and dissolved in physiological saline. All drugs were administered subcutaneously (s.c.) in a volume of 1 ml/kg of body weight. [3H]raclopride and [3H]ketanserin (Perkin Elmer Life Sciences, Boston, MA, USA), used as radiotracers in the occupancy studies, were administered intravenously.
D2/5-HT2 Occupancy Experiments
Haloperidol (0.025–5 mg/kg), risperidone (0.005–2 mg/kg), and aripiprazole (0.1–30 mg/kg) were administered to rats to obtain a dose response of D2/5-HT2 occupancy levels. Animals were randomly assigned (minimum of four) to each dose level of drug testing. Animals were killed by decapitation 1 h after injection. The animals received 7.5 μCi/rat of [3H]raclopride (D2RO) or [3H]ketanserin (5-HT2RO), diluted in saline in a constant volume of 0.4 ml, 30 or 45 min before being killed. The timing of the experiment was based on previous experiments where the striatal (for D2RO) or prefrontal (for 5-HT2RO) vs cerebellar uptake ratio for [3H]raclopride or [3H]ketanserin reached a state of equilibrium (Sumiyoshi et al, 1995; Wadenberg et al, 2000). Striatum or prefrontal cortex and cerebellum were rapidly dissected and dissolved overnight using 2 ml Solvable® (Canberra Packard, Canada) and counted using liquid scintillation spectrometry by addition of 5 ml of scintillation fluid (Aquasure® Canberra Packard, Canada) (Wadenberg et al, 2000). To obtain an index of the binding potential (BP) of dopamine D2 receptors, the ratio of striatum minus cerebellum (index of specific binding)/cerebellum (index of free and nonspecific binding) was used. In the case of 5-HT2RO, prefrontal cortex was used. This method is based on clinical occupancy experimentation and has been validated in experimental animals (Farde et al, 1988; Kapur et al, 1999; Wadenberg et al, 2000). The occupancy induced by the drug was calculated using the formula: %Occupancy=100 × (BPcontrols−BPdrug/BPcontrols); where BPcontrols is the pooled D2 or 5-HT2 binding potential of all the control animals and BPdrug is the D2 or 5-HT2 binding potential of a drug-treated animal. Occupancy curves and the ED50 values (dose at which 50% receptors are occupied) were determined using the nonlinear regression equation representing a rectangular hyperbola (y=ax/(b+x)) using Sigma Plot® software.
CAT
Animals used for the occupancy experiment were also used to measure CAT. At 10 min before being killed, animals were placed on an inclined grid (60°) and the time the animals remained immobile (excluding the first 30 s) was used as an index of CAT (on a scale 0–5 in which time was a square root transformation: 0=0–0.08, 1=0.09–0.35, 2=0.36–0.80, 3=0.81–1.42, 4=1.43–2.24, 5=>2.24 min) (Ahlenius and Hillegaart, 1986; Wadenberg et al, 2000). An animal was considered cataleptic with a score ⩾2. Raters were blind to drug treatment and the ED50 values were evaluated using probit analysis (Finney, 1971).
CAR
Rats were trained and tested in a two-way active avoidance (shuttle boxes) apparatus (Med Associates, Vermount, USA) set in a ventilated, sound and light attenuating, outer compartment. The shuttle boxes were enabled with a tilting grid floor and microswitch detection. Foot shocks were delivered to the grid floor by a current source set at 0.8 mA intensity. The boxes were divided into two compartments of equal size by a partition with an opening of 9 cm wide and 8 cm high. The opening was 6 cm above the grid floor. During the experimental sessions, two lights mounted in the top back corners of the outer compartment provided the illumination. A shielded house light also was set in the center at top right-hand corner of the shuttle box. A 80 dB white-noise served as a conditioned stimulus which was followed 10 s later by a 0.6 mA shock as the unconditioned stimulus in a computer-assisted two-way active avoidance task (shuttlebox). Animals that moved to the other side of the box within the period of the conditioned stimulus only (10 s) were noted as having made an ‘avoidance’ response. Those who escaped the shock in the next 10 s were termed as having ‘escaped’, and those not escaping within the total 20 s were termed as ‘escape failures’ (Wadenberg et al, 2001b). Rats were trained for 5 days before drug testing. While the training phase consisted of 40 trials each day (in one session), the testing phase consisted of 20 trials each session (one session at each of the time points). A performance criterion of greater than 80% avoidance after the 5-day training served as the basis for selecting rats that were used for drug testing. The entire protocol as well as recording of the animal's performance was administered by programs running on a computer. The ED50 for CAR was the dose required to produce 50% inhibition of avoidance, and was calculated using probit analysis at the 90 min time point after drug administration (Finney, 1971). Haloperidol was tested at 0.02, 0.05, and 0.15 mg/kg in eight subjects; risperidone was tested at doses of 0.1, 0.3, and 1 mg/kg in 10 subjects; while aripiprazole was tested at 3, 10, and 30 mg/kg in eight subjects. Animals of each drug group served as their own controls in a within-subject design. The sequence of drug administration was balanced as far as possible. Animals were tested at 0, 20, 90, 240 min, and 24 h after drug administration with an interval of at least 2 days between experiments.
Locomotor Activity
The locomotor activity boxes were clear plexiglas housing cages (27 × 48 × 20 cm) equipped with a row of six photocell beams placed 3 cm above the floor of the cage. A computer was used to detect and record the number of photobeam interruptions. For investigating the effects of haloperidol (0.01–0.5 mg/kg), risperidone (0.1–0.5 mg/kg), and aripriprazole (0.3–10 mg/kg) on AIL, rats were first injected with the appropriate antipsychotic or vehicle and placed in the locomotor activity boxes for a period of 30 min. Then, d-amphetamine (1.5 mg/kg/s.c.) was administered and locomotor activity was monitored for a period of 60 min. The ED50 value was the dose that was required to inhibit 50% of locomotor activity counts recorded over the period of 60 min with respect to vehicle-treated amphetamine-administered animals. Inhibition of spontaneous locomotor activity was evaluated by administering the drug and monitoring locomotor activity for a period of 1 h. Each group contained a minimum of six subjects at each dose level tested. The ED50 values were calculated using nonlinear regression using Sigma Plot® software.
FOS Immunohistochemistry
Haloperidol (0.01–1 mg/kg), risperidone (0.1–5 mg/kg), and aripiprazole (3–100 mg/kg) were evaluated for their ability to induce FOS in brain regions associated with antipsychotic action. The animals were deeply anaesthetized with sodium pentobarbital (100 mg/kg i.p.), 2 h after drug administration, and perfused transcardially with saline followed by 4% paraformaldehyde. The brains were removed, postfixed in 4% paraformaldehyde, transferred to sucrose solutions (10% for 2 h, 20% for 12 h, and 30% for 24 h) and then dried and stored at −80°C until processing. Immunostaining was performed on free-floating, 40 μm cryostat sections with a polyclonal primary antiserum raised in rabbit against the FOS peptide (4–17 amino acids of human FOS; Oncogene Research Products, Cambridge, Mass., USA), diluted 1 : 12 500 and incubated for 48 h at 4°C. The tissue sections were then exposed to biotinylated goat anti-rabbit secondary antibody (1 : 600, Vector Laboratories, Burlingame, California, USA), which was followed by incubation with horseradish peroxidase avidin–biotin complex (Vector Laboratories, Burlingame, California, USA) to visualize the FOS staining. FOS-immunoreactive nuclei were counted within a 400 × 400 μm grid at a magnification of × 100 in the nucleus accumbens (shell and core) and dorsolateral striatum (bregma 1.70–1.00) (Paxinos and Watson, 1986; Robertson et al, 1994) using an MCID M5 imaging and software system (Imaging Research, St Catherines, Ontario, Canada). Cell counts were obtained from at least three separate brain sections for each brain obtained from at least four subjects per group, by an observer who was blind to treatment conditions.
Plasma Prolactin Measurements
Prolactin levels were measured using plasma collected from rats killed for the occupancy experiment. Plasma samples were stored in −80°C until they were assayed. The prolactin levels (ng/ml) were measured using a rat prolactin enzyme immunoassay kit (ALPCO Diagnostics®, Windham, New Hampshire, USA). Increase in prolactin value (percentage from baseline) was calculated using nonlinear regression with Sigma Plot® software.
RESULTS
Occupancy and CAT
The results showed a dose-dependent D2RO for all the three antipsychotic agents (Figure 1, Table 1). Haloperidol in a dose range of 0.025–1 mg/kg showed a dose-dependent increase in striatal D2RO from 31 to 94% with an ED50 of 0.02 mg/kg (CI 95%: 0.012–0.028). Doses of haloperidol (⩾0.1 mg/kg, ie >5 times ED50) that exceeded ∼80% D2RO showed CAT. Risperidone on the other hand showed a D2RO of 26–91% in a dose range from 0.05 to 2 mg/kg with an ED50 of 0.14 mg/kg (CI 95%: 0.12–0.16). CAT was observed when occupancies exceeded ∼80% D2RO (⩾1 mg/kg, ie >5 times ED50). Aripiprazole showed a dose-dependent D2RO of 15–90% when tested at a dose range from 0.3 to 30 mg/kg with an ED50 of 0.7 mg/kg (CI 95%: 0.52–0.88). In the case of aripiprazole, CAT was not observed even at a dose of 30 mg/kg (ie >50 times ED50) that gave rise to occupancies of >85% (Figure 2).
Relationship between drug dose and receptor occupancy (D2 and 5-HT2) 1 h after single subcutaneous administration of haloperidol (n=5 for each dose), risperidone (n=4 for the D2RO and n=5 for the 5-HT2RO), and aripiprazole (n=5). The percentage occupancy values are expressed as Mean±SD. The curves were generated using nonlinear regression equation representing a rectangular hyperbola (y=ax/(b+x)) using Sigma Plot® software.
The figure shows percentage D2RO of individual animals 1 h after single subcutaneous administration of haloperidol (n=5 for each dose), risperidone (n=4), and aripiprazole (n=5). Animals showing CAT are represented as filled symbols. Also, percentage of animals showing CAT among those whose D2RO values exceeded 80% has been depicted.
In the case of 5-HT2 receptors, haloperidol and risperidone showed significant and dose-dependent in vivo receptor occupancy, while aripiprazole showed very low 5-HT2RO (Figure 1, Table 1). Haloperidol's ED50 was 0.96 mg/kg (CI 95%: 0.44–1.48) when tested in a dose range of 0.05–5 mg/kg. Risperidone's ED50 value was determined to be 0.01 mg/kg (CI 95%: 0.0002–0.012), when tested in a dose range of 0.005–0.5 mg/kg. Aripiprazole was tested over a dose range of 0.1–30 mg/kg and an ED50 could not be determined as 5-HT2 receptor occupancies did not exceed 50%.
CAR Inhibition
All of the antipsychotics inhibited CAR in a dose-dependent manner (Figure 3, Table 1). Haloperidol's ED50 at 90 min was 0.03 mg/kg (CI 95%: 0.01–0.05). Risperidone treatment resulted in an ED50 (90 min) of 0.7 mg/kg (CI 95%: 0.5–1). Aripiprazole's ED50 (90 min) was 12.6 mg/kg (CI 95%: 6–24). Haloperidol and risperidone were effective (ED50 values) at doses producing >60% D2RO, while aripiprazole on the other hand blocked CAR effectively only at doses that led to >85% D2RO. All drug-treated animals returned to their baseline 24 h after drug administration. There were no escape failures throughout the trials.
Effect of haloperidol (n=8), risperidone (n=10), and aripiprazole (n=8) (mg/kg) on the performance of conditioned avoidance response in rats 90 min after single subcutaneous administration. The animals served as their own controls using a within-subject design. Values of percentage inhibition of avoidance are expressed as Mean±SEM. The avoidance values were analyzed in an repeated measures analysis of variance with dose (vehicle, three drug doses) as a within-subjects factor for each drug separately. The sphericity assumption was met and the main effect of dose was significant for all the three drugs (haloperidol F (3, 21)=19.52, P<0.0005, ηP2 0.74; risperidone F (3, 27)=21.36, P<0.0005 ηP2 0.7; aripiprazole F (3, 21)=29.11, P<0.0005, ηP2 0.8). Post hoc comparisons were performed using the Bonferroni adjustment for multiple comparisons and the level of significance indicated in the figure is that with respect to vehicle treatment (**P<0.05) and all statistical analysis were carried out using SPSS® software.
Locomotor Activity
All three antipsychotic agents antagonized AIL (Figure 4, Table 1). The ED50 values for haloperidol and risperidone were 0.04 mg/kg (CI 95%: 0.02–0.06) and 0.38 mg/kg (CI 95%: 0.002–0.74), respectively. Haloperidol and risperidone were effective (ED50 values) at doses that produced ∼60% D2RO; the effective doses were in the same range as those that produced impaired CAR (ED50 values). In the case of aripiprazole, the ED50 obtained to inhibit AIL was 0.55 mg/kg (0.19–0.91) (slightly lower than 50% D2RO), which is several fold lower than that required to inhibit CAR. The ED50 values for inhibition of spontaneous locomotor activity was determined as 0.09 mg/kg (CI 95%: 0.03–0.15) for haloperidol, 0.26 mg/kg (CI 95%: 0.23–0.29) for risperidone, and 0.4 mg/kg (CI 95%: 0.38–0.42) for aripiprazole. The ED50 values for inhibiting spontaneous locomotor activity for haloperidol and risperidone were ∼70% D2RO, while it was lower than 50% D2RO for aripiprazole.
The effects of haloperidol (n=6), risperidone (n=6), and aripiprazole (n=6) (mg/kg) on locomotor activity measured for 1 h duration after amphetamine or saline administration and expressed as Mean±SEM. The drugs were administered by a single subcutaneous administration 30 min prior to amphetamine or saline administration. **P<0.001, *P<0.005 One-way ANOVA F(12, 69)=32.38; post hoc Dunnett (two-sided) with respect to amphetamine treatment using SPSS® software.
FOS Induction
Induction of FOS was measured over different doses along the D2RO curve in the nucleus accumbens (shell and core) as well as the dorsolateral striatum (Figure 5). The results clearly showed a dose-related increase in FOS induction in the shell of nucleus accumbens for all three antipsychotics. For haloperidol and risperidone, significant FOS induction in the nucleus accumbens shell emerged when occupancies exceeded 60% D2RO. The dose of aripiprazole 3 mg/kg, which gave rise to 72% D2RO occupancy, did not produce a discernable FOS signal in the nucleus accumbens shell. FOS expression for aripiprazole in the accumbens shell became observable only at occupancies exceeding 80% D2RO (Figure 5). Doses of risperidone (1 and 5 mg/kg) and haloperidol (0.5 and 1 mg/kg) that have the propensity for inducing CAT (D2RO>80%) clearly showed high levels of FOS induction in the core region of nucleus accumbens (greater than 40 counts in a 400 × 400 μm area) as well as in the dorsolateral striatum (greater than 30 counts). While there was a statistically significant increase in FOS expression in the nucleus accumbens core as well as dorsolateral striatum at higher doses of aripiprazole (D2RO>80%), the extent of FOS expression did not translate into motor side effects as evaluated by CAT (Figure 5). This suggests that FOS expression exceeding 40 counts in the nucleus accumbens core region as well as 30 counts (in a 400 × 400 μm area) in the dorsolateral striatum may be a molecular marker of a threshold for the induction of CAT under these conditions. Figure 6 shows the differential expression of FOS in the dorsolateral striatum for the three drugs.
The effect of (a) haloperidol (n=4 for each dose), (b) risperidone (n=4), and (c) aripiprazole (n=4) mg/kg on FOS expression in the nucleus accumbens (shell and core) and dorsolateral striatum in rats. Rats were killed 2 h after drug administration and FOS-immunoreactive nuclei counted within a 400 × 400 μm grid in the specific brain regions are expressed as Mean±SEM. *P<0.005 One-way ANOVA F(13, 50)=26.2; post hoc Dunnett (two-sided) with respect to the pooled vehicle control of nucleus accumbens (shell). #P<0.005 One-way ANOVA F(13, 50)=23.28; post hoc Dunnett (two-sided) with respect to the pooled vehicle control of nucleus accumbens (core). †P<0.05 One-way ANOVA F(13, 50)=15.08; post hoc Dunnett (two-sided) with respect to pooled vehicle treatment of dorsolateral striatum. All statistical analysis were performed using SPSS® software.
Prolactin Levels
Haloperidol and risperidone showed dose-related prolactin induction (Figure 7). In the haloperidol group, one rat in the 0.05 mg/kg treatment group was a significant outlier (prolactin value of 140 ng/ml; Grubbs test Z=1.71, P<0.05) and was excluded from the calculations and one sample in the 1 mg/kg group was lost due to contamination. In the case of aripiprazole, only at the dose of 10 mg/kg, a small increase was obtained and the increase was not present at a higher dose (30 mg/kg). In the case of risperidone, a dose of 0.05 mg/kg correlating to its central D2RO of 27%, induced significant prolactin levels.
Plasma prolactin levels (minimum of n=4 for each dose) for haloperidol, risperidone, and aripiprazole measured from plasma samples obtained from the occupancy experiments are expressed as Mean±SEM. **P<0.001, *P<0.01 One-way ANOVA F(12, 60)=15.41; post hoc Dunnett (two-sided) with respect to the pooled vehicle control using SPSS® software.
However, in the case of haloperidol, 27% D2RO correlated to a dose of 0.008 mg/kg and extrapolating for prolactin levels resulted in a value similar to the mean value of vehicle-treated animals, while a dose of 0.05 mg/kg (66% D2RO) resulted in significant prolactin elevation. Aripiprazole did not show prolactin elevation at D2RO exceeding 80% (30 mg/kg). The results clearly dissociate the relationship between central D2RO and prolactin elevation even within the D2 antagonist class of drugs (risperidone vs haloperidol), while aripiprazole does not have the expected antagonistic effect despite very high D2RO.
DISCUSSION
The clinical efficacy of aripiprazole, a partial agonist at the dopamine D2 receptor, has demonstrated that drugs other than neutral antagonists or inverse agonists can act as antipsychotics (Akam and Strange, 2004). With this clinical breakthrough comes the opportunity to re-examine many of the tenets associated with previous antipsychotics, a major one being the relationship between D2RO and different aspects of efficacy and side effects. The results of this study clearly demonstrate that aripiprazole shows a different relationship between D2RO and functional antagonism in animal models of CAR, AIL, spontaneous locomotion, CAT, and FOS induction as compared to typical and atypical D2 antagonist antipsychotics. We discuss the implications below.
It is commonly observed that motor side effects become prominent in patients when the dopamine D2 receptor blockade exceeds 80% (Farde et al, 1988; Kapur et al, 2000b). CAT is a valid model of these motor side effects and its expression is usually associated with >80% blockade of the dopamine D2 receptors (Wadenberg et al, 2001b). In the present study, both haloperidol and risperidone gave rise to CAT, while aripiprazole did not. In the animals tested with aripiprazole, D2RO exceeded 80% in 13 out of 25 animals and there was no evidence of CAT (Figure 2). These results concur with a study in normal volunteers where no functional impact of D2 blockade was observed on motor function despite occupancies exceeding 80% D2RO (Yokoi et al, 2002). Aripiprazole's characterization as a partial agonist could explain these findings. If one assumes its functional in vivo intrinsic efficacy as an agonist to be slightly greater than 20%, then 100% D2RO would lead to less than 80% functional antagonism of dopamine transmission. This could prevent the emergence of CAT despite a high level of D2RO (>80%).
Inhibition of CAR is another test that shows very high mechanistic, construct, and predictive validity for antipsychotic efficacy (Wadenberg and Hicks, 1999). Haloperidol and risperidone were effective at doses producing >60% D2RO, while aripiprazole was effective at doses that gave rise to occupancies of >85%. This finding replicates the dissociation observed in clinical studies; while haloperidol and risperidone are clinically active from ∼60% D2RO, aripiprazole is effective only at doses >85% D2RO (Farde et al, 1992; Kapur et al, 1995; Kapur et al, 1996; Kane et al, 2002; Yokoi et al, 2002; Marder et al, 2003). This finding can also be understood using the same assumption of functional in vivo intrinsic efficacy of aripiprazole as a partial agonist made earlier to explain lack of motor side effects. Data from haloperidol and risperidone suggest that one requires blockade of >60% dopamine transmission to obtain inhibition of CAR. Aripiprazole as a partial agonist, assuming >20% intrinsic efficacy as an agonist, would increase the threshold for CAR inhibition above 60 plus 20% occupancy of D2 receptors, and this seems to be the case.
The data from AIL and CAR models provide further evidence for a divergent relationship between occupancy and functional antagonism with aripiprazole. AIL activity represents a model for hyperdopaminergia and this model has been often used to predict antipsychotic efficacy (Arnt et al, 1997). Under the standard use of this paradigm, amphetamine releases dopamine and antipsychotics exert their effects in this model by competing for postsynaptic dopamine D2 receptors in the mesolimbic striatum (Pijnenburg et al, 1975). Both haloperidol and risperidone were effective in this model in reducing the effects of amphetamine (by 50%) at doses that gave rise to D2RO of ∼60%. Aripiprazole was equally effective at doses, if anything gave rise to a slightly lower level of D2 occupancy of ∼50%.
When seen from the perspective of its D2RO, aripiprazole shows antagonism of AIL at roughly equal levels of occupancy as that of haloperidol and risperidone, but requires a 23-fold higher dose (and occupancy) to block CAR (Table 1). An explanation for this dissociation could be attributed to the presence or absence of receptor reserves for dopamine-mediated actions in some behavioral/functional attributes that have been reporter earlier (Meller et al, 1989; Cox and Waszczak, 1990; Enz et al, 1990; Meller et al, 1991). It has been demonstrated in in vitro systems that agonistic efficacy of aripiprazole, relative to that of dopamine, varied from 25% in cells that lacked spare receptors for dopamine to 90% in cells with receptor reserve (Burris et al, 2002). So, in the presence of spare receptors, the agonist efficacy of a partial agonist increases relative to systems/behaviors having sparse spare receptors. So in the case of AIL, a pharmacological condition resulting from supranormal stimulation of dopamine D2 receptors, little or no receptor reserve may be present. Under these conditions, a partial agonist with weak intrinsic activity may look similar to a neutral antagonist. Whereas in CAR, unlike the AIL model, there is no supranormal stimulation. The existing receptor reserve would lead to aripiprazole expressing its agonist action and thereby necessitating a higher level of D2RO to block dopamine transmission.
To understand the emerging dissociation between occupancy and functional antagonism of aripiprazole at the molecular level, the ability of antipsychotics to induce FOS protein, a product of immediate-early genes in response to acute antipsychotic administration, was examined. It has been shown that all effective antipsychotics induce FOS in nucleus accumbens shell, while FOS induction in the core region of the nucleus accumbens as well as dorsolateral striatum is an indicator of EPS liability (Deutch et al, 1992; Dragunow et al, 1990; Oka et al, 2004; Robertson et al, 1994; Robertson and Fibiger, 1996). All three antipsychotics in our study induced FOS in the shell of the nucleus accumbens. Haloperidol and risperidone increased FOS expression (>20 counts in a 400 × 400 μm area) in the nucleus accumbens shell at doses that were in the CAR effective dose range (>60% D2RO). For aripiprazole, the doses needed to induce equivalent FOS increases (ie >20 counts) required D2RO in excess of 80%. With respect to the nucleus accumbens core (>40 counts) and the dorsolateral striatum (>30 counts), there seems to be a distinct threshold beyond which CAT is observed and it corresponds to doses of haloperidol and risperidone that result in >80% D2RO (Figure 5). Aripiprazole's FOS counts in the nucleus accumbens core and the dorsolateral striatum did not exceed these threshold levels even at doses that resulted in very high striatal D2RO. Since FOS induction is a functional marker of postsynaptic D2 antagonism, these findings confirm the dissociation between occupancy and antagonism at a postsynaptic level.
In the past, both motor side effects and prolactin elevation have been related to D2 receptor blockade, but the mechanism behind these functions differ significantly. While EPS is related to functional blockade of the striatal D2 receptors, prolactin secretion is understood to be related to D2 receptor antagonism mainly at the anterior pituitary, where dopamine exerts a tonically inhibitory effect. A 250% increase in prolactin levels from baseline for risperidone corresponds to 27% D2RO, while for haloperidol it corresponds to a D2RO of 80%. Aripiprazole showed no (with exception of one intermediate dose) propensity for prolactin elevation. The intermediate dose at which an elevation was observed could reflect the biphasic nature of aripiprazole in this system or just an aberration in measurement. Thus two dissociations emerge. First, risperidone gives rise to higher prolactin at lower D2ROs compared to haloperidol. The other dissociation is that aripiprazole does not give rise to prolactin elevation despite very high D2RO. The first one probably is an issue of drugs or their active metabolites poorly crossing the blood-brain barrier, such that there is a preferential occupancy of peripheral (pituitary) vs central D2 receptors (Kapur et al, 2002). In the case of aripiprazole, it is most likely its partial agonist effect (Inoue et al, 1996).
5-HT2 receptors have been implicated in the potentiation of antipsychotic effect in CAR (Wadenberg et al, 1998, 2001a) and could have influenced our findings with respect to aripiprazole. However, in the present study, aripiprazole did not seem to occupy 5-HT2 receptors in a significant manner to influence antipsychotic behavior. This was somewhat surprising given aripiprazole's 5-HT2 in vitro affinity (Shapiro et al, 2003). For haloperidol and risperidone, 5-HT2 receptor occupancy followed very orderly within-experiment dose-occupancy relationships and were consistent with previously reported values by others (Zhang and Bymaster, 1999). This makes its unlikely that our failure to observe 5-HT2 occupancy is a methodological or technical effect, and questions whether 5-HT2 receptors in this species makes a major contribution to the pharmacological effects of aripiprazole in CAR and CAT models on acute administration. Our findings with respect to aripiprazole's 5-HT2 receptor occupancy are also supported by the fact that in an in vivo model of 5-HT2 antagonism (MDMT-induced head twitches in mice), aripiprazole exhibited weak inhibition at comparable doses (Hirose et al, 2004). The divergence between in vitro vs in vivo D2/5-HT2 ratios could be often explained by the presence of active metabolites which in turn have different receptor affinity profiles. DM-1451, a major metabolite found in rodents as well as in humans, has comparable affinity to the D2 receptors as that of aripiprazole; however, its affinity at the 5-HT2 site is not known (Lawler et al, 1999). If it were the case that this, or some other metabolite, had a different profile of 5-HT2/D2 affinity than the parent compound, it could explain the results. Aripiprazole also has moderately high affinity for the 5-HT1A receptor (Jordan et al, 2002) and this could have influenced the induction of CAT or inhibition of CAR in rodents (Wadenberg et al, 1994; Andersen and Kilpatrick, 1996). However, in a recent study, pretreatment with the 5-HT1A selective antagonist WAY 100635 did not precipitate CAT in aripiprazole-treated rats (at comparable doses with the present study), unlike other D2 antagonists (ziprasidone) or partial agonists (SLV313, bifeprunox, and sarizotan) that also have 5-HT1A receptor affinity (Kleven et al, 2005). The role played by 5-HT2/5-HT1A receptors in aripiprazole's clinical actions will have to await data in humans for a final conclusion.
This study replicates two aspects of aripiprazole that are suggested by clinical data, a very high level of D2RO required for response (>80% vs the usual of >60%) and no EPS despite high occupancy. Our data and the clinical findings are consistent with aripiprazole's expression of partial D2 agonistic activity. This would explain the absence of CAT or FOS induction in the dorsolateral striatum for aripiprazole, despite high D2RO, as some D2 transmission is maintained. Also, partial agonism explains why relatively high D2RO is needed for suppression of CAR and expression of FOS in the nucleus accumbens. It also explains the need for very divergent doses between antagonizing AIL and CAR. Beyond illuminating the mechanism of aripiprazole, the study underscores how occupancy-function relationships obtained with antagonists would not translate to partial agonists. This is a particularly relevant finding as a number of new D2 partial agonists have clinically failed in the past (Tamminga, 2002) and a number of new ones are in development (Hertel et al, 2005). Thus while measuring occupancy is still going to be a very relevant construct, one cannot borrow the occupancy-function correlation of previously known antagonists. The present data allows us to hypothesize that the occupancy-functional antagonism relationship of partial D2 agonists will be a function of their degree of intrinsic efficacy—a hypothesis we are now in the process of testing.
References
Ahlenius S, Hillegaart V (1986). Involvement of extrapyramidal motor mechanisms in the suppression of locomotor activity by antipsychotic drugs: a comparison between the effects produced by pre- and post-synaptic inhibition of dopaminergic neurotransmission. Pharmacol Biochem Behav 24: 1409–1415.
Akam E, Strange PG (2004). Inverse agonist properties of atypical antipsychotic drugs. Biochem Pharmacol 67: 2039–2045.
Andersen HL, Kilpatrick IC (1996). Prevention by (+/−)-8-hydroxy-2-(di-n-propylamino)tetralin of both catalepsy and the rises in rat striatal dopamine metabolism caused by haloperidol. Br J Pharmacol 118: 421–427.
Arnt J, Skarsfeldt T, Hyttel J (1997). Differentiation of classical and novel antipsychotics using animal models. Int Clin Psychopharmacol 12 (Suppl 1): S9–S17.
Burris KD, Molski TF, Xu C, Ryan E, Tottori K, Kikuchi T et al (2002). Aripiprazole, a novel antipsychotic, is a high-affinity partial agonist at human dopamine D2 receptors. J Pharmacol Exp Ther 302: 381–389.
Cox RF, Waszczak BL (1990). Irreversible receptor inactivation reveals differences in dopamine receptor reserve between A9 and A10 dopamine systems: an electrophysiological analysis. Brain Res 534: 273–282.
Deutch AY, Lee MC, Iadarola MJ (1992). Regionally specific effects of atypical antipsychotic drugs on striatal Fos expression: the nucleus accumbens shell as a locus of antipsychotic action. Mol Cell Neurosci 3: 332–341.
Dragunow M, Robertson GS, Faull RL, Robertson HA, Jansen K (1990). D2 dopamine receptor antagonists induce fos and related proteins in rat striatal neurons. Neuroscience 37: 287–294.
Enz A, Goldstein M, Meller E (1990). Dopamine agonist-induced elevation of striatal acetylcholine: relationship between receptor occupancy and response in normal and denervated rat striatum. Mol Pharmacol 37: 560–565.
Farde L, Nordstrom AL, Wiesel FA, Pauli S, Halldin C, Sedvall G (1992). Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine. Relation to extrapyramidal side effects. Arch Gen Psychiatry 49: 538–544.
Farde L, Wiesel FA, Halldin C, Sedvall G (1988). Central D2-dopamine receptor occupancy in schizophrenic patients treated with antipsychotic drugs. Arch Gen Psychiatry 45: 71–76.
Finney DJ (1971). Probit Analysis. Cambridge University Press: London.
Hertel P, Olsen CK, Didriksen M, Arnt J, Marquis K, van der Heyden J et al (2005). Bifeprunox: a New and Different Antipsychotic. International Congress on Schizophrenia Research. Savannah Georgia, USA.
Hirose T, Uwahodo Y, Yamada S, Miwa T, Kikuchi T, Kitagawa H et al (2004). Mechanism of action of aripiprazole predicts clinical efficacy and a favourable side-effect profile. J Psychopharmacol 18: 375–383.
Hoffman DC, Donovan H (1995). Catalepsy as a rodent model for detecting antipsychotic drugs with extrapyramidal side effect liability. Psychopharmacology (Berl) 120: 128–133.
Inoue T, Domae M, Yamada K, Furukawa T (1996). Effects of the novel antipsychotic agent 7-(4-[4-(2,3-dichlorophenyl)-1-piperazinyl]butyloxy)-3,4-dihydro -2(1H)-quinolinone (OPC-14597) on prolactin release from the rat anterior pituitary gland. J Pharmacol Exp Ther 277: 137–143.
Jordan S, Koprivica V, Chen R, Tottori K, Kikuchi T, Altar CA (2002). The antipsychotic aripiprazole is a potent, partial agonist at the human 5-HT1A receptor. Eu J Pharmacol 441: 137–140.
Kane JM, Carson WH, Saha AR, McQuade RD, Ingenito GG, Zimbroff DL et al (2002). Efficacy and safety of aripiprazole and haloperidol versus placebo in patients with schizophrenia and schizoaffective disorder. J Clin Psychiatry 63: 763–771.
Kapur S, Langlois X, Vinken P, Megens AA, De Coster R, Andrews JS (2002). The differential effects of atypical antipsychotics on prolactin elevation are explained by their differential blood–brain disposition: a pharmacological analysis in rats. J Pharmacol Exp Ther 302: 1129–1134.
Kapur S, Remington G, Jones C, Wilson A, DaSilva J, Houle S et al (1996). High levels of dopamine D2 receptor occupancy with low-dose haloperidol treatment: a PET study. Am J Psychiatry 153: 948–950.
Kapur S, Remington G, Zipursky RB, Wilson AA, Houle S (1995). The D2 dopamine receptor occupancy of risperidone and its relationship to extrapyramidal symptoms: a PET study. Life Sci 57: PL103–PL107.
Kapur S, Zipursky R, Jones C, Remington G, Houle S (2000a). Relationship between dopamine D(2) occupancy, clinical response, and side effects: a double-blind PET study of first-episode schizophrenia. Am J Psychiatry 157: 514–520.
Kapur S, Zipursky R, Jones C, Shammi CS, Remington G, Seeman P (2000b). A positron emission tomography study of quetiapine in schizophrenia: a preliminary finding of an antipsychotic effect with only transiently high dopamine D2 receptor occupancy. Arch Gen Psychiatry 57: 553–559.
Kapur S, Zipursky RB, Remington G (1999). Clinical and theoretical implications of 5-HT2 and D2 receptor occupancy of clozapine, risperidone, and olanzapine in schizophrenia. Am J Psychiatry 156: 286–293.
Kikuchi T, Tottori K, Uwahodo Y, Hirose T, Miwa T, Oshiro Y et al (1995). 7-(4-[4-(2,3-Dichlorophenyl)-1-piperazinyl]butyloxy)-3,4-dihydro-2(1H)-qui nolinone (OPC-14597), a new putative antipsychotic drug with both presynaptic dopamine autoreceptor agonistic activity and postsynaptic D2 receptor antagonistic activity. J Pharmacol Exp Ther 274: 329–336.
Kleven MS, Barret-Grevoz C, Slot LB, Newman-Tancredi A (2005). Novel antipsychotic agents with 5-HT(1A) agonist properties: role of 5-HT(1A) receptor activation in attenuation of catalepsy induction in rats. Neuropharmacology 49: 135–143.
Lawler CP, Prioleau C, Lewis MM, Mak C, Jiang D, Schetz JA et al (1999). Interactions of the novel antipsychotic aripiprazole (OPC-14597) with dopamine and serotonin receptor subtypes. Neuropsychopharmacology 20: 612–627.
Marder SR, McQuade RD, Stock E, Kaplita S, Marcus R, Safferman AZ et al (2003). Aripiprazole in the treatment of schizophrenia: safety and tolerability in short-term, placebo-controlled trials. Schizophr Res 61: 123–136.
Meller E, Hizami R, Kreuter L (1989). Hypothermia in mice: D2 dopamine receptor mediation and absence of spare receptors. Pharmacol Biochem Behav 32: 141–145.
Meller E, Puza T, Miller JC, Friedhoff AJ, Schweitzer JW (1991). Receptor reserve for D2 dopaminergic inhibition of prolactin release in vivo and in vitro. J Pharmacol Exp Ther 257: 668–675.
Meltzer HY (1999). The role of serotonin in antipsychotic drug action. Neuropsychopharmacology 21 (Suppl 1): S106–S115.
Miyamoto S, Duncan GE, Marx CE, Lieberman JA (2005). Treatments for schizophrenia: a critical review of pharmacology and mechanisms of action of antipsychotic drugs. Mol Psychiatry 10: 79–104.
Oka T, Hamamura T, Lee Y, Miyata S, Habara T, Endo S et al (2004). Atypical properties of several classes of antipsychotic drugs on the basis of differential induction of Fos-like immunoreactivity in the rat brain. Life Sci 76: 225–237.
Paxinos G, Watson C (1986). The Rat Brain in Stereotaxic Coordinates. Academic press: New York.
Pijnenburg AJ, Honig WM, Van Rossum JM (1975). Inhibition of d-amphetamine-induced locomotor activity by injection of haloperidol into the nucleus accumbens of the rat. Psychopharmacologia 41: 87–95.
Potkin SG, Saha AR, Kujawa MJ, Carson WH, Ali M, Stock E et al (2003). Aripiprazole, an antipsychotic with a novel mechanism of action, and risperidone vs placebo in patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatry 60: 681–690.
Robertson GS, Fibiger HC (1996). Effects of olanzapine on regional C-Fos expression in ratforebrain. Neuropsychopharmacology 14: 105–110.
Robertson GS, Matsumura H, Fibiger HC (1994). Induction patterns of Fos-like immunoreactivity in the forebrain as predictors of atypical antipsychotic activity. J Pharmacol Exp Ther 271: 1058–1066.
Shapiro DA, Renock S, Arrington E, Chiodo LA, Liu LX, Sibley DR et al (2003). Aripiprazole, a novel atypical antipsychotic drug with a unique and robust pharmacology. Neuropsychopharmacology 28: 1400–1411.
Sumiyoshi T, Suzuki K, Sakamoto H, Yamaguchi N, Mori H, Shiba K et al (1995). Atypicality of several antipsychotics on the basis of in vivo dopamine-D2 and serotonin-5HT2 receptor occupancy. Neuropsychopharmacology 12: 57–64.
Tamminga CA (2002). Partial dopamine agonists in the treatment of psychosis. J Neural Transm 109: 411–420.
Wadenberg MG, Browning JL, Young KA, Hicks PB (2001a). Antagonism at 5-HT(2A) receptors potentiates the effect of haloperidol in a conditioned avoidance response task in rats. Pharmacol Biochem Behav 68: 363–370.
Wadenberg ML, Cortizo L, Ahlenius S (1994). Evidence for specific interactions between 5-HT1A and dopamine D2 receptor mechanisms in the mediation of extrapyramidal motor functions in the rat. Pharmacol Biochem Behav 47: 509–513.
Wadenberg ML, Hicks PB (1999). The conditioned avoidance response test re-evaluated: is it a sensitive test for the detection of potentially atypical antipsychotics? Neurosci Biobehav Rev 23: 851–862.
Wadenberg ML, Hicks PB, Richter JT, Young KA (1998). Enhancement of antipsychotic like properties of raclopride in rats using the selective serotonin2A receptor antagonist MDL 100,907. Biol Psychiatry 44: 508–515.
Wadenberg ML, Kapur S, Soliman A, Jones C, Vaccarino F (2000). Dopamine D2 receptor occupancy predicts catalepsy and the suppression of conditioned avoidance response behavior in rats. Psychopharmacology (Berl) 150: 422–429.
Wadenberg ML, Soliman A, VanderSpek SC, Kapur S (2001b). Dopamine D(2) receptor occupancy is a common mechanism underlying animal models of antipsychotics and their clinical effects. Neuropsychopharmacology 25: 633–641.
Yokoi F, Grunder G, Biziere K, Stephane M, Dogan AS, Dannals RF et al (2002). Dopamine D2 and D3 receptor occupancy in normal humans treated with the antipsychotic drug aripiprazole (OPC 14597): a study using positron emission tomography and [11C]raclopride. Neuropsychopharmacology 27: 248–259.
Zhang W, Bymaster FP (1999). The in vivo effects of olanzapine and other antipsychotic agents on receptor occupancy and antagonism of dopamine D1, D2, D3, 5HT2A and muscarinic receptors. Psychopharmacology (Berl) 141: 267–278.
Acknowledgements
This study was funded by a CIHR grant to Shitij Kapur. We thank Eli Lilly for the supply of aripiprazole. Suzi VanderSpeck, Doug Hussey, and Jun Parkes of the PET group and Karen Barlow of the Neuroimaging section of CAMH are acknowledged for their technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Natesan, S., Reckless, G., Nobrega, J. et al. Dissociation between In Vivo Occupancy and Functional Antagonism of Dopamine D2 Receptors: Comparing Aripiprazole to Other Antipsychotics in Animal Models. Neuropsychopharmacol 31, 1854–1863 (2006). https://doi.org/10.1038/sj.npp.1300983
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300983
Keywords
This article is cited by
-
Structure-based design of a novel third-generation antipsychotic drug lead with potential antidepressant properties
Nature Neuroscience (2022)
-
Spironolactone alleviates schizophrenia-related reversal learning in Tcf4 transgenic mice subjected to social defeat
Schizophrenia (2022)
-
Effect of 5-HT2A receptor antagonism on levels of D2/3 receptor occupancy and adverse behavioral side-effects induced by haloperidol: a SPECT imaging study in the rat
Translational Psychiatry (2021)
-
Modulation by chronic antipsychotic administration of PKA- and GSK3β-mediated pathways and the NMDA receptor in rat ventral midbrain
Psychopharmacology (2019)
-
The relationship between dopamine receptor blockade and cognitive performance in schizophrenia: a [11C]-raclopride PET study with aripiprazole
Translational Psychiatry (2018)