Abstract
The α2-adrenoceptor antagonist idazoxan may improve motor symptoms in Parkinson's disease and experimental Parkinsonism. We studied the effect of idazoxan on haloperidol-induced catalepsy in rats, an animal model of the drug-induced extrapyramidal side effects in man. Catalepsy was induced by a subcutaneous (s.c.) injection of haloperidol (1 mg/kg) and measured by the bar test for a maximum of 5 min. At 3 h after haloperidol, rats were given 0.16–5.0 mg/kg s.c. idazoxan, and descent latency was measured 1 h later. Idazoxan potently reversed haloperidol-induced catalepsy with an ED50 of 0.25 mg/kg. This effect was mimicked by the selective α2-adrenoceptor antagonist RS-15385-197 (0.3 and 1 mg/kg orally). We assessed how dopaminergic mechanisms were involved in the anticataleptic effect of idazoxan by studying its effect on dopamine (DA) release in the striatum, with the microdialysis technique in conscious rats. Idazoxan (0.3 and 2.5 mg/kg) had no effect on extracellular DA and did not modify the rise of extracellular DA induced by haloperidol, indicating that changes of striatal DA release were not involved in the reversal of catalepsy. The anticataleptic effect of 2.5 mg/kg idazoxan (haloperidol+vehicle 288±8 s, haloperidol+idazoxan 47±22 s) was attenuated in rats given an intraventricular injection of 150 μg of the serotonin (5-HT) neurotoxin 5,7-dihydroxytryptamine (haloperidol+vehicle 275±25 s, haloperidol+idazoxan 137±28 s). The 5-HT1A receptor antagonist WAY100 635 (0.1 mg/kg s.c.) did not affect the anticataleptic effect of idazoxan. The results suggest that idazoxan reversed haloperidol-induced catalepsy by a mechanism involving blockade of α2-adrenoceptors and, at least in part, 5-HT neurons.
Similar content being viewed by others
INTRODUCTION
Blockade of α2-adrenoceptors may alleviate the extrapyramidal effects of neuroleptic agents (Nutt, 1994; Kalkman et al, 1998). Particularly interesting is the finding that the α2-adrenoceptor antagonist idazoxan improves motor function in a severe form of motor disorder, progressive supranuclear palsy (Ghika et al, 1991). Pilot studies indicate that idazoxan also improves motor symptoms in Parkinson's disease (Peyro-Saint-Paul et al, 1995), l-DOPA-induced dyskinesias (Rascol et al, 2001; Grondin et al, 2000), and experimental Parkinsonism (Bezard et al, 1999; Henry et al, 1999).
Antagonists at α2-adrenoceptors facilitate dopamine (DA) transmission as shown by the fact that they enhance the effect of D-amphetamine on locomotor activity (Dickinson et al, 1988) and the ipsilateral rotation induced by D-amphetamine in unilateral substantia nigra-lesioned rats (Mavridis et al, 1991). Recently, various α2-adrenoceptor antagonists were found to inhibit the cataleptic response to loxapine (Kalkman et al, 1998) and yohimbine inhibited haloperidol-induced catalepsy as well (Al-Shabibi and Dogget, 1978; Kalkman et al, 1998). Surprisingly, the α2-adrenoceptor antagonist idazoxan (Doxey et al, 1983) did not antagonize raclopride-induced catalepsy (Hertel et al, 1999a).
There is considerable evidence that catalepsy induced by neuroleptics is because of blockade of nigrostriatal DA transmission (Sanberg, 1980; Calderon et al, 1988). DA D2 receptors are quite likely involved in this type of catalepsy, as D2 receptor-deficient mice display catalepsy (Baik et al, 1995) and D2 receptor occupancy predicts catalepsy in rats (Wadenberg et al, 2000) and extrapyramidal side effects in humans (Farde et al, 1992; Kapur et al, 1995, 2000). The mechanism by which α2-adrenoceptor blockade improves motor function may reflect increased release of DA in the nigrostriatal pathway (Nutt, 1993; Kalkman et al, 1998). A subcutaneous injection of 0.5 and 1.5 mg/kg idazoxan markedly increased extracellular DA in the medial prefrontal cortex, with no effect on DA output in the striatum and nucleus accumbens (Hertel et al, 1999b). However, local administration of idazoxan in the striatum significantly increased DA output in this region (Hertel et al, 1999b).
The present study was designed to examine whether idazoxan antagonized catalepsy induced by haloperidol and modified the effect of the neuroleptic on striatal extracellular DA, as measured by the in vivo microdialysis technique. To confirm that blockade of α2-adrenoceptors antagonized haloperidol-induced catalepsy, in one experiment we used a very potent and selective α2-adrenoceptor antagonist RS-15358-197 which, unlike idazoxan, has no affinity for the nonadrenoceptor imidazoline-binding sites (Brown et al, 1993).
Serotonin (5-HT) appears to have a complex role in neuroleptic-induced catalepsy. This catalepsy is reduced after stimulation of 5-HT1A and 5-HT2A receptors (Hicks, 1990; Wadenberg, 1996; Invernizzi et al, 1988; Neal-Beliveau, 1993), and blockade of 5-HT2C receptors (Reavill et al, 1999). Given that idazoxan enhances 5-HT release in the frontal cortex (Garrat et al, 1991; Matsumoto et al, 1998) and, at high doses, may stimulate 5-HT1A receptors (Kawai et al, 1994; Llado et al, 1996), the serotonergic system may play a significant role in the mechanism of action of idazoxan. Therefore, we investigated the anticataleptic effect of idazoxan in rats whose serotonergic neurons were selectively destroyed by neurotoxic lesions with 5,7-dihydroxytryptamine (5,7-DHT), or which were treated with the selective 5-HT1A receptor antagonist WAY100635 (Forster et al, 1995).
MATERIALS AND METHODS
Induction and Measurement of Catalepsy
Male CD-COBS rats (Charles River, Calco, Italy) were gently handled for 5 min/day for a week before the experiment. On the day of the experiment, 30–60 min before treatment with haloperidol, they were placed one per cage to adapt to the new environment. Rats were injected with 1 mg/kg haloperidol (0.3 mg/kg in one experiment) and catalepsy measured by gently placing their front limbs over a 10-cm high horizontal bar. The intensity of catalepsy was assessed by measuring the time the rats remained in this position, with the limbs completely immobile for a maximum of 5 min (Invernizzi et al, 1988).
In another experiment, we evaluated the effect of idazoxan on catalepsy induced by haloperidol (1 mg/kg), in the grid test (Ahlenius and Hillegaart, 1986). Rats were given haloperidol and 3 h later received idazoxan (1.5 and 2.5 mg/kg) or saline. At 1 h after idazoxan, rats were placed on a 60°-inclined grid and, after 30 s habituation, the time they remained in the same position was measured for a maximum of 3 min.
Dialysis Procedure
Dialysis experiments were conducted in freely moving rats. Rats were anesthetized with 3.5 ml/kg Equithesin (1.2 g pentobarbital, 5.3 g chloral hydrate, 2.7 g MgSO4, 49.5 ml propylene glycol, 12.5 ml ethanol, and 58 ml distilled water) and placed on a stereotaxic apparatus (David Kopf Instruments, Tujunga, CA). A hole was drilled in the skull and a small incision made in the dura with a bent needle tip. The probe was lowered slowly into the rat anterolateral striatum, while being perfused (2–5 μl/min) with artificial cerebrospinal fluid (aCSF), and fixed to the skull vertically using anchorage screws and acrylic cement. Stereotaxic coordinates for the probe tip were as follows: AP=+9.7, L=+3.4, and V=+3.4 from the interaural line according to the Paxinos and Watson (1982) atlas.
Vertical dialysis probes were prepared essentially as described by Robinson and Whishaw (1988), except that the dialysis membrane was made of polyacrylonitrile-sodium methallyl sulfonate (AN 69 Hospal S.p.A.; 310 μm outer diameter, 55 000 Da M.W. cutoff). The exposed membrane was 2 mm long.
Rats were allowed to recover from anesthesia, one per cage, with free access to food and water. About 24 h after surgery the inlet cannula was connected by polyethylene tubing to a 2.5 ml plastic syringe containing aCSF (composition in mM: 145 NaCl, 3 KCl, 1.26 CaCl2·2H2O, 1 MgCl2.6H2O in distilled water and buffered at pH 7.4 with 2 mM sodium phosphate buffer). Probes were perfused at a constant flow rate of 2 μl/min with a CMA/100 microinfusion pump (CMA/Microdialysis, Stockholm, Sweden). After a 30-min washout period, consecutive 20-min samples of perfusate containing DA were collected in minivials.
Analytical Procedure
DA in dialysate was assayed by high-performance liquid chromatography with electrochemical detection (HPLC-ED), as previously described (Invernizzi et al, 1990). The chromatograph consisted of a Gilson pump with titanium head mod. 307 (Gilson, France), a Rheodyne injection valve model 7125 (Rheodyne, Cotati, CA), an analytical column (Supelcosil LC-18DB, 3 μm, 4.6 × 150 mm, Supelchem, Italy), a guard column (4 × 30 mm, packed with Perisorb, 30–40 μm, Merck, Germany), and an electrochemical detector (Coulochem II; ESA, Bedford, MA) equipped with an analytical cell consisting of two in-series electrodes (model 5011). The first electrode was set at +300 mV and the second at −280 mV. DA was read as second electrode output signal. The mobile phase consisted of 0.1 M sodium acetate, 0.34 mM sodium octyl sulfate, 0.1 mM Na2EDTA, 60 ml/l CH3OH, pH 4.2 with acetic acid, pumped at a constant flow rate of 1 ml/min.
Histology
At the end of the dialysis experiment, rats were deeply anesthetized with chloral hydrate and killed by decapitation; their brains were immediately removed and frozen on dry ice. Probe tracks were examined on 40 μm coronal sections from the striatum of each rat. Only rats with probe positioned in the region between ±0.5 mm AP,±0.3 mm V, and ±0.3 mm L of the striatum were included in the results (see scheme in Figure 5).
Schematic drawing of probes placement in the striatum (adapted from Paxinos and Watson, 1982; vertical bars indicate the probes).
Drug Treatment
Rats were randomly assigned to the different experimental groups. Idazoxan (Institut de Recherche Pierre Fabre, Labège, France), WAY100 635 (Pharmacia, Nerviano, Italy), and RS-15385-197 (Roche Bioscience, Palo Alto, CA) were dissolved in sterile 0.9% NaCl solution (saline). Haloperidol (Lusofarmaco, Milan, Italy) was dissolved with a few drops of acetic acid and the solution was buffered to pH 5 with 5 M NaOH. Drugs were injected subcutaneously except for RS-15385-197, which was administered orally. Doses are referred to the free base.
Rats were given haloperidol (0.3 or 1 mg/kg) and, 3 h later, idazoxan (0.16, 0.31, 0.63, 1.25, 2.5, and 5.0 mg/kg), RS-15385-197 (0.1, 0.3, and 1 mg/kg), or saline. Idazoxan and RS-15385-197 were injected 3 h after haloperidol since at this time catalepsy was fully established and the response remained undiminished for the duration of the experiment. To assess the role of 5-HT1A receptors in the anticataleptic effect of idazoxan, rats were given the selective 5-HT1A receptor antagonist WAY100 635 (0.1 mg/kg s.c.), 30 min before idazoxan (2.5 mg/kg). Different sets of rats were used for each treatment group.
The neurochemical studies follow the same protocol as the behavioral experiments. Once the basal extracellular concentrations of DA was stable (at least three consecutive samples differing less than 15% of the mean basal value), rats were injected with haloperidol and 3 h later with idazoxan (0.3 and 2.5 mg/kg) or saline. Extracellular DA was measured for 2 h after idazoxan injection.
5,7-DHT Injection
5,7-DHT creatinine sulfate (150 μg of the free base) (ICN Biomedicals, Milan, Italy) was dissolved in 10 μL distilled water containing 1 mg/ml ascorbic acid. Rats were anesthetized with Equithesin and placed on a stereotaxic apparatus (David Kopf Instruments, Tujunga, CA). 5,7-DHT or ascorbic acid solutions were infused monolaterally into the lateral ventricle at a constant flow rate of 4 μl/min with a microinjection pump (CMA/Microdialysis, Sweden). The needle was left in place for 1 min before withdrawal. To protect noradrenergic neurons, the rats were given 25 mg/kg desipramine 30 min before 5,7-DHT (Breese and Cooper, 1975). Catalepsy experiments started 21 days after injection of the neurotoxin. To assess the efficacy and selectivity of the lesion with 5,7-DHT, 24 h after the experiment, vehicle- and 5,7-DHT-treated rats were killed by decapitation and the concentrations of 5-HT, DA, and NA were measured in the forebrain by HPLC-ED as previously described (Pozzi et al, 1999).
Statistics
The results of the experiments on haloperidol-induced catalepsy were examined by one- or two-way ANOVA (idazoxan plus WAY100 635 or 5,7-DHT), and post hoc comparison was carried out by Dunnett's and Tukey–Kramer's tests. The effect of idazoxan alone or in combination with haloperidol on extracellular DA was analyzed by ANOVA for repeated measures with time and treatment as within and between factors, respectively. The analysis was applied to the part of the curve from 20 min before to 120 min after idazoxan or saline.
RESULTS
Effect of Idazoxan and RS-15385-197 on Haloperidol-Induced Catalepsy
The time course of haloperidol-induced catalepsy is shown in Table 1. Maximum catalepsy occurred between 2 and 5 h after 1 mg/kg haloperidol when descent latency was longer than 200 s out of the 300-s test period. Typically, rats given vehicle remained immobile on the bar for 1–5 s. Although a few control rats remained on the bar longer, their descent latency never exceeded 22 s.
Figure 1 shows the effect of 0.16–5 mg/kg idazoxan on haloperidol-induced catalepsy. The effect of haloperidol was significantly and potently inhibited by idazoxan (F(6,57)=10.9, P<0.001). The effect of idazoxan was dose dependent with an estimated ED50 (dose reducing descent latency in rats given 1 mg/kg haloperidol by 50%) of 0.25 mg/kg (0.18–0.35 mg/kg, 95% confidence interval). The lowest dose of idazoxan that significantly reduced haloperidol-induced catalepsy was 0.31 mg/kg. Higher doses tended to have a larger anticataleptic effect although descent latencies were not significantly different from the rats given 0.31 mg/kg.
Effect of idazoxan on haloperidol-induced catalepsy in the bar test. Rats given haloperidol (1 mg/kg s.c.) were injected subcutaneously with saline (open columns) or various doses of idazoxan (solid columns) 3 h later. Descent latency was measured 4 h after haloperidol. Mean±SEM of eight rats. *P<0.05 vs saline (Tukey–Kramer's test).
In the grid test, 2.5 mg/kg idazoxan reversed catalepsy induced by 1 mg/kg haloperidol, whereas 1.5 mg/kg of the drug had no significant effect (Figure 2).
Effect of idazoxan on haloperidol-induced catalepsy in the grid test. Rats given haloperidol (1 mg/kg s.c.) were injected subcutaneously with saline (open columns) or 1.5 and 2.5 mg/kg idazoxan (solid columns) 3 h later. Catalepsy was measured 4 h after haloperidol. Mean±SEM of 4–10 rats. *P<0.05 vs saline (Tukey–Kramer's test).
As shown in Figure 3, RS-15385-197 dose-dependently reduced descent latency in rats given 1 mg/kg haloperidol 3 h before (F(3,40)=15.3, P<0.001). Post hoc comparisons showed that the effect of RS-15385-197 was significant at 0.3 and 1 but not at 0.1 mg/kg.
Effect of RS-15385-197 on haloperidol-induced catalepsy. Rats given haloperidol (1 mg/kg s.c.) were given saline (open columns) or various doses of RS-15385-197 (solid columns) orally 3 h later. Descent latency was measured 4 h after haloperidol. Mean±SEM of 8–12 rats. *P<0.05 vs saline (Tukey–Kramer's test).
Effect of Idazoxan on Haloperidol-Induced Rise of Extracellular DA in the Striatum
A 1 mg/kg dose of haloperidol raised extracellular DA by 164%, 180 min after the injection (Figure 4). The increase was significant from 40 min to the end of the observation period. Idazoxan (0.31 and 2.5 mg/kg) had no effect on basal (F(2,13)=1.3, P>0.05) and haloperidol-induced rise of extracellular DA (F(2,13)=0.1, P>0.05) (Figure 4.
Effect of idazoxan on basal and haloperidol-induced rise of extracellular DA in the striatum. Haloperidol (HAL; 1 mg/kg) or vehicle (VEH) was injected once basal extracellular concentrations of DA were stable (first arrow). After 3 h, (second arrow), rats were given 0.31 and 2.5 mg/kg idazoxan (IDZ) or saline (SAL), and DA release was followed for 2 h. Mean±SEM of five to six rats.
Effect of 5,7-DHT on the Anticataleptic Effect of Idazoxan
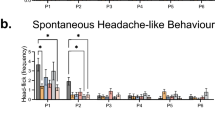
Intraventricular injection of 150 μg 5,7-DHT had no effect on haloperidol-induced catalepsy, but significantly attenuated the anticataleptic effect of 2.5 mg/kg idazoxan (Figure 6) (F5,7-DHT × IDZ(1,20)=6.3, P<0.05). 5-HT concentrations in the forebrain were reduced by 90% in rats given 5,7-DHT intraventricularly (n=10) compared to those receiving vehicle (n=8) (vehicle 498±12, 5,7-DHT 50±6 ng/g, P<0.001, Student's t-test); the forebrain concentrations of DA (vehicle 1137±18; 5,7-DHT 1177±41) and NA (vehicle 226±8 and 5,7-DHT 226±7) were not significantly modified.
Effect of 2.5 mg/kg idazoxan (solid columns) or saline (open columns) on catalepsy induced by 1 mg/kg haloperidol in rats injected intraventricularly with vehicle or 150 μg/10 μl 5,7-DHT 3 weeks earlier. Mean±SEM of 9–11 rats. *P<0.01 vs vehicle+saline; °P<0.01 vs 5,7-DHT+saline; #P<0.05 vs vehicle+idazoxan (Tukey–Kramer's test).
Effect of WAY100 635 on the Anticataleptic Effect of Idazoxan
As shown in Figure 7, haloperidol (0.3 and 1 mg/kg) dose dependently increased descent latency. Idazoxan significantly reduced the increase induced by 0.3 mg/kg haloperidol, whereas 0.1 mg/kg WAY100 635, a 5-HT1A receptor antagonist, had the opposite effect (Figure 7). Two-way ANOVA found no significant interaction between WAY100 635 and idazoxan (FWAY × IDZ(1,28)=0.04, P>0.05), indicating that pretreatment with WAY100 635 did not modify the anticataleptic effect of idazoxan.
Effect of WAY100 635 on the anticataleptic effect of idazoxan. Rats given 0.3 mg/kg (upper panel) or 1 mg/kg (lower panel) haloperidol were injected with 0.1 mg/kg WAY100 635 or saline 30 min before 2.5 mg/kg idazoxan (solid columns) or saline (open columns). Catalepsy was measured 1 h after idazoxan. Mean±SEM of seven to eight rats. *P<0.05 vs saline+saline; °P<0.05 vs WAY100 635+idazoxan (Tukey–Kramer's test).
A 1 mg/kg dose of haloperidol caused a near-maximal increase of descent latency, and pretreatment with 0.1 mg/kg WAY100 635 had no significant effect on catalepsy induced by this dose. As shown in Figure 7, idazoxan significantly reversed the increase in descent latency induced by 1 mg/kg haloperidol but this effect was not significantly modified by pretreatment with 0.1 mg/kg WAY100 635 (FWAY × IDZ(1,28)=0.9, P>0.05).
DISCUSSION
As in previous studies (Costall et al, 1975; Invernizzi et al, 1988), 1 mg/kg haloperidol caused maximal cataleptic response in rats and this effect was associated with increased extracellular concentrations of DA in the striatum (Zetterström et al, 1984; Imperato and Di Chiara, 1985).
The α2-adrenoceptor antagonist, idazoxan, potently reverses haloperidol-induced catalepsy in rats (ED50=0.25 mg/kg), an effect shared by other α2-adrenoceptor antagonists such as yohimbine and RX821002 (Al-Shabibi and Dogget, 1978; Kalkman et al, 1998). Thus, the mechanism of the anticataleptic effect of idazoxan probably involves blockade of α2-adrenoceptors. This interpretation is supported by the finding that RS-15385-197, a selective α2-adrenoceptor antagonist with no affinity for the nonadrenoceptor imidazoline-binding site (Brown et al, 1993), antagonized haloperidol-induced catalepsy. Idazoxan and RS-15385-197 are both α2-adrenoceptor antagonists, but they belong to different chemical classes. This chemical distinction increases the likelihood that their effects on haloperidol-induced catalepsy are based on their ability to act as α2-adrenoceptor antagonists and not on some secondary effect of either drug.
The present results are in apparent contrast with a previous study in which 1.5 mg/kg idazoxan did not affect the catalepsy induced by the selective D2/3 receptor antagonist raclopride, measured in the grid test (Hertel et al, 1999a). In the same grid test, we found that 2.5 mg/kg idazoxan reduced the catalepsy induced by 1 mg/kg haloperidol whereas 1.5 mg/kg had no such effect. Thus, differences in the sensitivity of the test used to assess the anticataleptic effect of idazoxan may account for the discrepancy between the present results and those of Hertel et al (1999a). Other factors such as the type and dose of neuroleptic used in the two studies, treatment schedules, and the criteria for measuring catalepsy may also account for the results.
The reversal of catalepsy by α2-adrenoceptor antagonists may be because of increased striatal release of DA that would compete with haloperidol to counteract its effect on striatal postsynaptic D2 receptors responsible for catalepsy (Nutt, 1994; Kalkman et al, 1998). In the present study, doses of idazoxan (0.3 and 2.5 mg/kg) blocking haloperidol-induced catalepsy had no effect on extracellular DA in the striatum and did not modify the rise of extracellular DA induced by 1 mg/kg haloperidol. These results are in line with previous findings that systemic doses of idazoxan in the range of those showing anticataleptic effect did not affect basal or the raclopride-induced rise of striatal extracellular DA (Hertel et al, 1999a); this argues against the theory that idazoxan reverses haloperidol-induced catalepsy by increasing striatal DA release. The finding that idazoxan and other α2-adrenoceptor antagonists antagonized muscular rigidity in reserpinized rats (Colpaert, 1987; Wagner and Anderson, 1982) is consistent with an action of idazoxan independent of DA release, and suggests that the drug might overcome the motor side effects associated with impairment of pre- and postsynaptic DA transmission in the nigrostriatal system.
Haloperidol-induced catalepsy might be reversed by idazoxan through an action on dopaminergic mechanisms in a brain region not examined in the present study. The drug strongly potentiates the increase of prefrontocortical extracellular DA induced by the selective D2/3 receptor antagonist raclopride (Hertel et al, 1999a), and injection of DA into the prefrontal cortex attenuates haloperidol-induced catalepsy (Tucci et al, 1994). Thus, it is conceivable that idazoxan given in combination with haloperidol enhances the rise of cortical DA release caused by the neuroleptic and, as a consequence, attenuates catalepsy.
Catalepsy induced by neuroleptic drugs is modified by agents interfering with serotonergic neurotransmission (Hicks, 1990; Invernizzi et al, 1988; Neal-Beliveau et al, 1993). We found that the anticataleptic effect of 2.5 mg/kg idazoxan was attenuated in rats whose serotonergic neurons had been selectively destroyed by intraventricular 5,7-DHT. This is compatible with the finding that doses of idazoxan in the range of those blocking catalepsy increased extracellular 5-HT in the brain (Matsumoto et al, 1998; Garrat et al, 1991), and suggest that increased 5-HT release might contribute to the anticataleptic effect of idazoxan. It is conceivable that by removing the α2-adrenoceptor inhibitory tone on 5-HT neurons in the raphe (Svensson et al, 1975; Garrat et al, 1991) or nerve terminals (Maura et al, 1982; Garrat et al, 1991), idazoxan enhances serotonergic transmission attenuating haloperidol-induced catalepsy. However, further studies are needed to prove that an increase in 5-HT transmission is involved in the anticataleptic effect of idazoxan.
Idazoxan can act as a 5-HT1A receptor agonist, albeit at high doses (Kawai et al, 1994; Llado et al, 1996) and stimulation of 5-HT1A receptors potently reverses neuroleptic-induced catalepsy (Hicks, 1990; Invernizzi et al, 1988). Similar to idazoxan, the ability of the 5-HT1A receptor agonist 8-OH-DPAT to reverse haloperidol-induced catalepsy is counteracted by the destruction of brain 5-HT neurons (Invernizzi et al, 1988) and is not associated with altered DA release in the striatum (Lucas et al, 1997). These findings prompted us to examine whether the selective 5-HT1A receptor antagonist WAY100 635 (Forster et al, 1995) antagonized the anticataleptic effect of idazoxan. WAY100 635 did not antagonize this effect, suggesting that 5-HT1A receptors are not involved. Consistent with previous findings (Prinssen et al, 1998), WAY100 635 enhanced catalepsy induced by 0.3 mg/kg haloperidol, a dose inducing a submaximal increase in descent latency.
In conclusion, the present results show that idazoxan potently reverses haloperidol-induced catalepsy. The anticataleptic effect is not dependent on an increase of DA availability in the striatum, but may be at least partly related to the drug's ability to interact with central serotonergic neurons. Finally, idazoxan apparently does not act by stimulating 5-HT1A receptors to reverse haloperidol-induced catalepsy. Whether the stimulation of 5-HT transmission by other 5-HT receptor subtypes plays a role in the anticataleptic effect of idazoxan has yet to be determined.
References
Ahlenius S, Hillegaart V (1986). Involvement of extrapyramidal motor mechanisms in the suppression of locomotor activity by antipsychotic drugs: a comparison between the effect produced by pre- and postsynaptic inhibition of dopaminergic neurotransmission. Pharmacol Biochem Behav 24: 1409–1415.
Al-Shabibi UMH, Dogget NS (1978). On the central noradrenergic mechanism involved in haloperidol-induced catalepsy in the rat. J Pharm Pharmacol 30: 529–531.
Baik J-H, Picetti R, Saiardi A, Thiriet G, Dierich A, Depaulis A et al (1995). Parkinsonian-like locomotor impairment in mice lacking dopamine D2 receptors. Nature 377: 424–428.
Bezard E, Brefel C, Tison F, Peyro-Saint-Paul H, Ladure P, Rascol O et al (1999). Effect of the α2-adrenoceptor antagonist, idazoxan, on motor disabilities in MPTP-treated monkey. Prog Neuro-Psychopharmacol Biol Psychiatry 23: 1237–1246.
Breese GR, Cooper BR (1975). Behavioral and biochemical interaction of 5,7-dihydroxytryptamine with various drugs when administered intracisternally to adult and developing rats. Brain Res 98: 517–527.
Brown CM, MacKinnon AC, Redfern WS, Hicks PE, Kilpatrick AT, Small C et al (1993). The pharmacology of RS-15385-197, a potent and selective α2-adrenoceptor antagonist. Br J Pharmacol 108: 516–525.
Calderon SF, Sanberg PR, Norman AB (1988). Quinolinic acid lesions of rat striatum abolish D1- and D2-dopamine receptor-mediated catalepsy. Brain Res 450: 403–407.
Colpaert FC (1987). Pharmacological characteristics of tremor, rigidity and hypokinesia induced by reserpine in rat. Neuropharmacology 26: 1431–1440.
Costall B, Fortune DH, Naylor RJ, Marsden CD, Pycock C (1975). Serotonergic involvement with neuroleptic catalepsy. Neuropharmacology 14: 859–868.
Dickinson SL, Gadie B, Tulloch IF (1988). α1 and α2 adrenoceptor antagonists differentially influence locomotor and stereotyped behaviour induced by d-amphetamine and apomorphine in the rat. Psychopharmacology 96: 521–527.
Doxey JC, Roach AG, Smith CF (1983). Studies on RX 781094: a selective, potent and specific antagonist of alpha2-adrenoceptors. Br J Pharmacol 78: 489–505.
Farde L, Nordström A-L, Wiesel F-A, Pauli S, Halldin C, Sedvall G (1992). Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine: relation to extrapyramidal side effects. Arch Gen Psychiatry 49: 538–544.
Forster EA, Cliffe IA, Bill DJ, Dover GM, Jones D, Reilly Y et al (1995). A pharmacological profile of the selective silent 5-HT1A receptor antagonist, WAY-100635. Eur J Pharmacol 281: 81–88.
Garrat JC, Crespi F, Mason R, Marsden CA (1991). Effects of idazoxan on dorsal raphe 5-hydroxytryptamine neuronal function. Eur J Pharmacol 193: 87–93.
Ghika J, Tennis M, Hoffman E, Schoenfeld D, Growdon J (1991). Idazoxan treatment in progressive supranuclear palsy. Neurology 41: 986–991.
Grondin R, Tahar AH, Van Diep D, Ladure P, Bédard PJ (2000). Noradrenoceptor antagonism with idazoxan improves l-DOPA-induced dyskinesia in MPTP-treated monkeys. NS Arch Pharmacol 361: 181–186.
Henry B, Fox SH, Pegs D, Crossman AR, Brotchie JM (1999). The α2-adrenergic receptor antagonist idazoxan reduces dyskinesia and enhances anti-Parkinsonian actions of L-dopa in the MPTP-lesioned primate model of Parkinson's disease. Mov Disord 14: 744–753.
Hertel P, Fagerqvist MV, Svensson TH (1999a). Enhanced cortical dopamine output and antipsychotic-like effects of raclopride by α2-adrenoceptor blockade. Science 286: 105–107.
Hertel P, Nomikos GG, Svensson TH (1999b). Idazoxan preferentially increases dopamine output in the rat medial prefrontal cortex at the nerve terminal level. Eur J Pharmacol 371: 153–158.
Hicks PB (1990). The effect of serotonergic agents on haloperidol-induced catalepsy. Life Sci 47: 1609–1615.
Imperato A, Di Chiara G (1985). Dopamine release and metabolism in awake rats after systemic neuroleptics as studied by trans-striatal dialysis. J Neurosci 5: 297–306.
Invernizzi R, Morali F, Pozzi L, Samanin R (1990). Effects of acute and chronic clozapine on dopamine release and metabolism in the striatum and nucleus accumbens of conscious rats. Br J Pharmacol 100: 774–778.
Invernizzi RW, Cervo L, Samanin R (1988). 8-hydroxy-2-(di–propylamino)tetralin, a selective serotonin1A receptor agonist, blocks haloperidol-induced catalepsy by an action on raphe nuclei medianus an dorsalis. Neuropharmacology 27: 515–518.
Kalkman HO, Neumann V, Hoyer D, Tricklebank MD (1998). The role of α2-adrenoceptor antagonism in the anticataleptic properties of the atypical neuroleptic agent, clozapine, in the rat. Br J Pharmacol 124: 1550–1556.
Kapur S, Remington G, Zipursky RB, Wilson AA, Houle S (1995). The D2 dopamine receptor occupancy of risperidone and its relationship to extrapyramidal symptoms: a PET study. Life Sci 57: 103–107.
Kapur S, Zipursky RB, Jones C, Remington G, Houle S (2000). Relationship between dopamine D2 occupancy, clinical response and side effects—a double blind PET study in first episode schizophrenia. Am J Psychiatry 157: 514–520.
Kawai N, Yamamoto T, Baba A, Yamamoto H, Maroji T (1994). Inhibitory effect of idazoxan on forskolin-stimulated adenylate cyclase activity through 5-hydroxytryptamine1A receptors. Arzneim-Forschung 44: 1–3.
Llado J, Esteban S, Garcia-Sevilla JA (1996). The α2-adrenoceptor antagonist idazoxan is an agonist at 5-HT1A autoreceptors modulating serotonin synthesis in the rat brain in vivo. Neurosci Lett 218: 111–114.
Lucas G, Bonhomme N, De Deurwaerdère P, Le Moal M, Spampinato U (1997). 8-OH-DPAT, a 5-HT1A agonist and ritanserin, a 5-HT2A/c antagonist, reverse haloperidol-induced catalepsy in rats independently of striatal dopamine release. Psychopharmacology 131: 57–63.
Matsumoto M, Yoshioka M, Togashi H, Mori K, Ueno K, Saito H (1998). Effects of idazoxan on dopamine release in the pre-frontal cortex of freely moving rats. Eur J Pharmacol 343: 165–170.
Maura G, Gemignani A, Raiteri M (1982). Noradrenaline inhibits central serotonin release through alpha2-adrenoceptors located on serotoninergic nerve terminals. Naunyn–Schmiedeberg's Arch Pharmacol 320: 272–274.
Mavridis M, Colpaert FC, Millan MJ (1991). Differential modulation of (+)amphetamine-induced rotation in unilateral substantia nigra-lesioned rats by α1 as compared to α2 agonists and antagonists. Brain Res 562: 216–224.
Neal-Beliveau BS, Joyce JN, Lucki I (1993). Serotonergic involvement in haloperidol-induced catalepsy. J Pharmacol Exp Ther 265: 207–217.
Nutt DJ (1994). Putting the ‘A’ in atypical: does α2-adrenoceptor antagonism account for the therapeutic advantage of new antipsychotics? J Psychopharmacol 8: 193–195.
Nutt DJ, Lalies M, Hudson A (1993). The effects of alpha-2-adrenoceptor antagonists on extracellular dopamine concentrations in the rat striatum. In: Colpaert F, Briley M (eds). Noradrenergic Mechanisms in Parkinson Disease. Academic Press: New York. pp 159–172.
Paxinos G, Watson C (1982). The Rat Brain in Stereotaxic Coordinates. Academic Press: Sydney.
Peyro-Saint-Paul H, Rascol O, Blin O, Senard JM, Viallet F, Plétan Y et al (1995). A pilot study of idazoxan, an α2 antagonist, in Parkinson's disease. 1st Congress of the Eur Ass Clin Pharmacol Ther, Paris, 27–30 September.
Pozzi L, Invernizzi R, Garavaglia C, Samanin R (1999). Fluoxetine increases extracellular dopamine in the prefrontal cortex by a mechanism not dependent on serotonin: a comparison with citalopram. J Neurochem 73: 1051–1057.
Prinssen EPM, Kleven MS, Koek W (1998). The catalepto-genic effects of neuroleptic nemonapride are attenuated by its 5-HT1A receptor agonist properties. Eur J Pharmacol 356: 189–192.
Rascol O, Arnulf I, Peyro-Saint-Paul H, Brefel-Courbon C, Vidaihlet M, Thalamas C et al (2001). Idazoxan, an alpha-2 antagonist, and L-DOPA-induced dyskinesias in patients with Parkinson's disease. Mov Disord 16: 708–713.
Reavill C, Kettle A, Holland V, Riley G, Blackburn TP (1999). Attenuation of haloperidol-induced catalepsy by a 5-HT2C receptor antagonist. Br J Pharmacol 126: 572–574.
Robinson TE, Whishaw IQ (1988). Normalization of extracellular dopamine in striatum following recovery from a partial unilateral 6-OHDA lesion of the substantia nigra: a microdialysis study in freely moving rats. Brain Res 450: 209–224.
Sanberg PR (1980). Haloperidol-induced catalepsy is mediated by post-synaptic dopamine receptors. Nature 284: 472–473.
Svensson TH, Bunney BS, Aghajanian GK (1975). Inhibition of both noradrenergic and serotonergic neurons in brain by the α-adrenergic agonist clonidine. Brain Res 92: 291–306.
Tucci S, Fernandez R, Baptista T, Murzi E, Hernandez L (1999). Dopamine increase in the prefrontal cotex correlates with reversal of haloperidol-induced catalepsy in rats. Brain Res Bull 35: 125–133.
Wadenberg ML (1996). Serotonergic mechanisms in neuroleptic-induced catalepsy in the rat. Neurosci Biobehav Rev 20: 325–339.
Wadenberg MLG, Kapur S, Soliman A, Jones C, Vaccarino F (2000). Dopamine D2 receptors occupancy predicts catalepsy and the suppression of conditioned avoidance response behavior in rats. Psychopharmacology 150: 422–429.
Wagner BH, Anderson RJ (1982). Prevention of reserpine rigidity by alpha-2 adrenergic antagonists. Pharmacol Biochem Behav 16: 731–735.
Zetterström T, Sharp T, Ungerstedt U (1984). Effect of neuroleptic drugs on striatal dopamine release and metabolism in the awake rat studied by intracerebral dialysis. Eur J Pharmacol 106: 27–37.
Acknowledgements
This work was partially supported by Institut de Recherche Pierre Fabre. We are grateful to Pharmacia and Roche Bioscience for their generous supply of drugs and M Carli for a critical reading of the manuscript, and J Baggot for linguistic assistance. RWI dedicates this work to the memory of R Samanin and F Morali.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Invernizzi, R., Garavaglia, C. & Samanin, R. The α2-Adrenoceptor Antagonist Idazoxan Reverses Catalepsy Induced by Haloperidol in Rats Independent of Striatal Dopamine Release: Role of Serotonergic Mechanisms. Neuropsychopharmacol 28, 872–879 (2003). https://doi.org/10.1038/sj.npp.1300119
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300119
Keywords
This article is cited by
-
The α2-adrenergic antagonist idazoxan counteracts prepulse inhibition deficits caused by amphetamine or dizocilpine in rats
Psychopharmacology (2012)
-
Rate-dependent behavioral effects of stimulation of central motoric ?1-adrenoceptors: hypothesized relation to depolarization blockade
Psychopharmacology (2005)
-
Anticataleptic properties of ?2 adrenergic antagonists in the crossed leg position and bar tests: differential mediation by 5-HT1A receptor activation
Psychopharmacology (2005)
-
Serotonergic influence on the potentiation of D-amphetamine and apomorphine-induced rotational behavior by the α2-adrenoceptor antagonist 2-methoxy idazoxan in hemiparkinsonian rats
Journal of Neural Transmission (2005)