Abstract
Digital transformation in the health sector can revolutionize a country’s healthcare system. However, the effective sustainability of digital health relies on various factors that influence its implementation. Addressing such implementation challenges is crucial in designing and delivering digital health services. Therefore, this systematic review attempted to identify the potential barriers to the implementation of digital transformation in the health sector of India. Systematic searches were employed across databases PubMed, PsycINFO, Science Direct, Web of Science, and Google Scholar for studies that reported digital transformation in India from inception to December 2022. Following narrative synthesis, studies were assessed for quality using JBI and the Mixed Methods Appraisal Tool (MMAT). Out of 1129 initially identified records, 26 studies that met the inclusion criteria were deemed eligible for final analysis. Although digital transformation in India’s health sector occurred rapidly, especially during the COVID-19 pandemic, there are still potential barriers that impede its successful implementation in the country. Barriers identified are mainly associated with limited technological and medical infrastructure, data security and privacy, and a lack of physical examination. The need to address these barriers, recommendations for government and healthcare practitioners, and implications for future research are discussed.
Similar content being viewed by others
Introduction
The emergence of several digital innovations, including the Internet of Things (IoT), robots, and artificial intelligence (AI), opens up novel business opportunities and income streams in various industries when used appropriately and effectively. Digital transformation involves using information and communication technology (ICT) in basically new business capabilities, public administration, and the lives of individuals and society (Martin, 2008) to enable substantial advancements like effective operations, better consumer experiences, or new business models (Fitzgerald et al., 2014). Besides, it is the net effect of many digital technologies resulting in new actors and actor constellations, values, practices, and structures, as well as the beliefs that change, replace, threaten, or complement current game norms in the organizations, industries, fields, or ecosystems (Hinings et al., 2018). Undoubtedly, digital transformation created a favorable business environment that has expanded employee work opportunities and, thereby, a better quality of life in many spheres. The extensive environmental, institutional, and societal implications of digital transformation made it central research attention in the last two decades (Kraus et al., 2021).
The tidal wave of digital innovations, which has intensified into a technological tsunami over the past several years, has also impacted the healthcare sectors across the globe. Digital health includes a variety of domains, such as advanced computing sciences, patients, healthcare providers, public health authorities, research institutes, and universities (WHO, 2021). Likewise, traditional healthcare providers, including hospitals, doctors, laboratories, regulators, and insurers, are no longer the only ones involved in healthcare; new actors are also entering from industries like mobility, telecommunications, retail, and logistics. These changes can be attributed to the revolutionary forces in information and knowledge management that alter how people relate to health, well-being, disease prevention, and work-life balance (Belliger and Krieger, 2018). Additionally, literature has revealed the impact of certain emerging digital health innovations, including mobile health, electronic medical record (EMR) systems, health cloud, telemedicine services, clinical decision support systems, and computerized physician order entry (e.g., Heath and Porter, 2019; Zobair et al., 2020). These technology-driven revolutions in the health sector have markedly enhanced the diagnosis and management of healthcare (Choi et al., 2019).
Even though research has shown technology-based improvements in health industries, various stakeholders express their resistance to such innovations (e.g., Kelly et al., 2017; Sarradon-Eck et al., 2021), with overt and covert forms of opposition to digital advancements (Talwar et al., 2021). For instance, Bhattacherjee and Hikmet (2007) revealed that resistance to change was an aspect that had a negative influence on physicians’ intentions to utilize digital care in the health sector. Likewise, a similar opposition has been observed in implementing other healthcare technologies, such as EMR systems (Ilie and Turel, 2020) and mobile health applications (Sarradon-Eck et al., 2021). Thus, the adoption and acceptance of digital technologies face several barriers, including organizational, technological, financial, behavioral, structural, and legal barriers (Gleiss and Lewandowski, 2022). On the other hand, the outbreak of the novel coronavirus posed unexpected challenges to healthcare systems across the globe and influenced stakeholders’ approaches toward digital transformation. Digital healthcare innovations, such as telehealth found to enable quality remote care during the pandemic (Monaghesh and Hajizadeh, 2020). Yet, recent reviews suggested that patients and healthcare providers continue to resist the digital transformation in the health sector despite its several applications and benefits (Rajkumar et al., 2023; Singh et al., 2022). In this sense, identifying the barriers to digital transformation in the health sector is crucial for informing and guiding healthcare providers and stakeholders who wish to develop and implement digital health technology that meets patient-provider needs. In order to provide some insight into this phenomenon, a systematic review of the barriers to implementing digital transformation in the health sector is required.
The healthcare sector in India is one of the key areas for investment, primarily through accessible digital platforms, affordability, and high quality. However, the industry is also facing many difficulties due to an increase in the aging population, change in the burden of illness, limited access to healthcare in remote areas, scarcity of healthcare providers, and insufficient public sector investment. In addition, only 33 percent of doctors in India work in rural regions, despite the fact that 71 percent of the country’s population resides in rural areas (Census of India, 2011). Hence, transformation to digital technology has the potential to deal with these healthcare challenges in the country. In response to this impact, the Government of India introduced the flagship program Digital India Campaign in 2015, which included public health initiatives geared at adopting digital technologies to penetrate healthcare services in rural areas. A complete digital healthcare system was subsequently envisioned under the National Health Policy of 2017, which resulted in the launch of the Digital Health Mission in India. With this policy, the National Digital Health Blueprint (NDHB) of 2019 outlined the fundamentals and an implementation strategy for digital health in India. Based on the NDHB, on August 15, 2020, the Ministry of Health and Family Welfare unveiled the National Digital Health Mission (NDHM) to build a digital health ecosystem. After a year of operation, it was renamed “Ayushman Bharat Digital Mission” and is now applicable across the country.
While the nation is moving steadily toward a digital healthcare revolution, it still confronts various barriers to successfully implementing digital transformation. India has one of the world’s lowest public health spending ratios at just over one percent of its gross domestic product. According to the National Health Profile statistics (2019), there are 7,13,986 beds in government hospitals, representing 0.55 beds per 1000 patients, of which only 5–8 percent are intensive care unit (ICU) beds. Moreover, few district hospitals have an electronic health record (EHR) system, and primary healthcare clinics lack the basic physical infrastructure, including medical equipment, labor rooms, adequate beds, a computer with an internet connection, and even regular water and electricity supplies. Undoubtedly, digital technologies can revolutionize the country’s healthcare system, but the barriers to digital transformation make it a far-fetched reality. Recognizing this current scenario, the present study examines the barriers to implementing digital transformation in the health sector of India. This review could help all stakeholders improve digital transformation’s comprehensive implementation and sustainability in the country’s health sector. Thus, the review aims to address the following research question: What are the barriers to implementing digital transformation in the health sector of India?
Methods
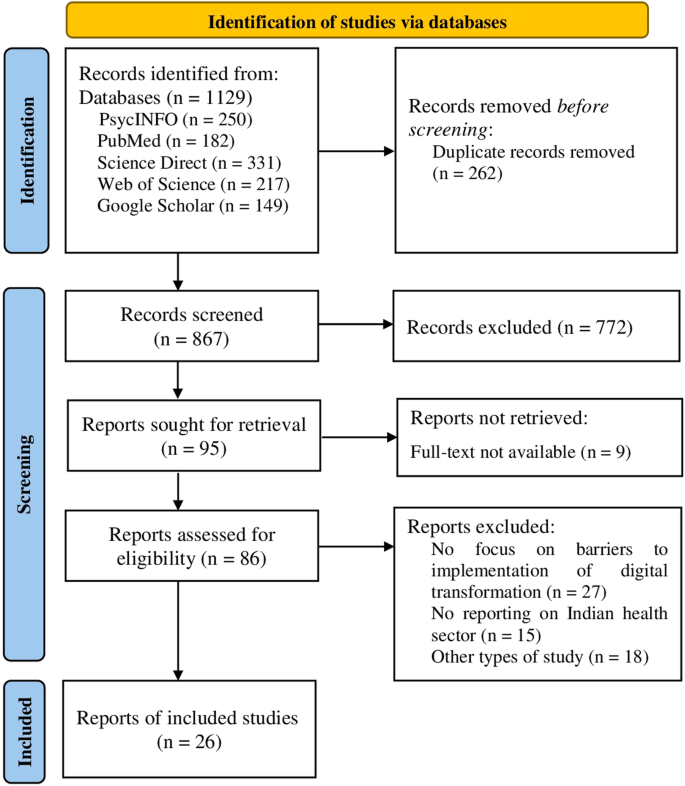
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (Page et al., 2021).
Eligibility criteria
The present study included peer-reviewed qualitative and quantitative studies published in English from inception till December 2022. Specifically, reports that provide data on barriers to implementing digital transformation in the health sector of India were included. Both patient-provider level barriers to the uptake of digital health transformation were considered. This review defined barriers as factors hindering the health sector’s digital transformation, such as a switch to various technological innovations, including telemedicine and mobile health. However, case reports, conference abstracts, editorials, commentaries, and reviews were excluded.
Information sources and search strategy
A systematic search was carried out in major electronic databases, including PsycINFO, PubMed, Science Direct, Web of Science, and Google Scholar, in December 2022. Several synonyms were used to capture the maximum relevant records published on digital transformation limited to the Indian health sector. The search terms were appropriately operated in each database depending on their strategy using Boolean operators “AND” and “OR”. The search used in PubMed was (challenges[Title/Abstract]) OR (barriers[Title/Abstract]) AND (transformation[Title/Abstract]) OR (implementation[Title/Abstract]) OR (experience[Title/Abstract]) AND (“digital health”[Title/Abstract]) OR (telehealth[Title/Abstract]) OR (mHealth[Title/Abstract]) OR (e-health[Title/Abstract]) OR (teleconsultation[Title/Abstract]) OR (telemedicine[Title/Abstract]) OR (“remote consultation”[Title/Abstract]) OR (telerehabilitation[Title/Abstract]) OR (“mobile health”[Title/Abstract]); in PsycINFO searched on the EBSCO platform was AB Abstract (challenges OR barriers OR concern AND transformation OR implementation OR experience AND “digital health” OR telehealth OR e-health OR teleconsultation OR telemedicine OR “remote consultation” OR telerehabilitation OR “mobile health”); in Science Direct was Title, abstract, keywords: (challenges OR barriers) AND (“digital health” OR telehealth OR e-health OR teleconsultation OR telemedicine OR telerehabilitation OR “mobile health”), and in Web of Science was (((((((((((((TS = (challenges)) OR TS = (barriers)) AND TS = (transformation)) OR TS = (implementation)) OR TS = (experience)) AND TS = (“digital health”)) OR TS = (telehealth)) OR TS = (mHealth)) OR TS = (e-health)) OR TS = (teleconsultation)) OR TS = (telemedicine)) OR TS = (“remote consultation”)) OR TS = (telerehabilitation)) OR TS = (“mobile health”).
Selection process and data extraction
The first three authors have conceptualized the present study. Two authors independently searched for relevant records in electronic databases. Three authors screened titles and abstracts of studies yielded from this systematic search. Two authors screened full-text reports for inclusion and performed the data extraction. Disagreements were settled through discussion and, when needed, by consulting a third author. Authors’ details, study location, type of study, participant characteristics, and the barriers to implementation of digital transformation in the health sector in India were extracted from each finalized study.
Quality assessment and evidence synthesis
The methodological quality of the qualitative and quantitative studies was assessed using JBI critical appraisal tools. Quality scores were based on evaluating various study domains, including eligibility criteria, participant characteristics, and data analysis. Rating scales of ‘yes,’ ‘no,’ ‘unclear,’ and ‘not applicable’ with 8, 11, and 10 questions were used for cross-sectional, cohort, and qualitative studies, respectively (Moola et al., 2015). The mixed-method studies were appraised with the MMAT (Hong et al., 2018). The methodological quality of the included studies in this review was assessed by four independent researchers and verified by one researcher. The extracted information was compared and contrasted in a narrative synthesis, and themes were generated. The reviewers often met to discuss the study findings and reached an agreement.
Results
Study selection
A total of 1129 articles were returned in search of the electronic databases. Of these, 250 were from PsycINFO, 182 were from PubMed, 331 were from Science Direct, 217 were from Web of Science, and 149 were from Google Scholar. The PRISMA flow diagram depicts the complete search process for this systematic review (Fig. 1). After deduplication, the title and abstracts of 867 records were screened according to the inclusion and exclusion criteria. Subsequently, title and abstract screening resulted in the removal of 772 studies. Nine of the 95 records searched for retrieval could not be obtained because the full text was inaccessible. Hence, 86 reports were assessed for selection, and 60 studies were removed because they did not meet the eligibility criteria (no focus on the barriers to implementation of digital transformation in the health sector (n = 27), other types of studies, such as conference proceedings or review papers (n = 18), and no focus on health sector in India (n = 15)). Thus, the final synthesis included 26 studies emphasizing the barriers to implementing various digital technologies in the health sector.
Study characteristics
The final sample for the present review included 26 studies conducted across India from 2017 to 2022 (Table 1). Two studies in 2022 (Prakash and Das, 2022; Sampathkumar et al., 2022), 16 were published in 2021 (Bairapareddy et al., 2021; Banerjee et al., 2021; D’Souza et al., 2021; Garg et al., 2021; Ghoshal et al., 2021; Kumar et al., 2021; Mathew et al., 2021; Menon et al., 2021; Nair et al., 2021; Naveen et al., 2021; Raheja et al., 2021; Sandhu et al., 2021; Satgunam et al., 2021; Shambu et al., 2021; Faujdar et al., 2021; Ullas et al., 2021), four in 2020 (Biswas et al., 2020; Pandey et al., 2020; Puliyath et al., 2020; Thenral and Annamalai, 2021), two in 2018 (Bhatt et al., 2018; Sinha Deb et al., 2018), and two in 2017 (Mohan et al., 2017; Powell et al., 2017). Included studies consisted of quantitative/cross-sectional studies (n = 10) (Bairapareddy et al., 2021; Sinha Deb et al., 2018; Ghoshal et al., 2021; Kumar et al., 2021; Mohan et al., 2017; Nair et al., 2021; Pandey et al., 2020; Powell et al., 2017; Raheja et al., 2021; Ullas et al., 2021), quantitative/cohort studies (n = 8) (Biswas et al., 2020; D’Souza et al., 2021; Garg et al., 2021; Naveen et al., 2021; Puliyath et al., 2020; Satgunam et al., 2021; Sandhu et al., 2021; Shambu et al., 2021), qualitative studies (n = 5) (Banerjee et al., 2021; Bhatt et al., 2018; Menon et al., 2021; Faujdar et al., 2021; Thenral and Annamalai, 2021), and mixed-methods studies (n = 3) (Mathew et al., 2021; Prakash and Das, 2022; Sampathkumar et al., 2022). Participants included the general population, delivered women, healthcare professionals, patients and caregivers, experts from academia, smartphone users, and technology experts. The current study findings offer a comprehensive understanding of barriers to the implementation of digital transformation in the health sector of India.
Risk of bias in studies
The risk of bias in quantitative cross-sectional studies (n = 10) and qualitative studies (n = 5) was low, while the risk of bias for cohort studies was generally low to moderate (see Supplementary information). The detailed results of the quality assessment of mixed-methods studies (n = 3) can be found in the supplementary table (see Supplementary Table 4). Also, no studies were excluded based on the level of quality assessment.
Barriers to the implementation of digital transformation in the health sector
Several previous studies have identified potential barriers to implementing digital transformation in India. Identifying the country’s barriers to digital health transformation is necessary to fulfill the need for successful transformation to digital health. As a result, the findings were synthesized into the following themes: lack of network coverage and information technology (IT) infrastructure, high installation and operating cost, lack of medical records and experts, lack of physical examination, data accuracy and misdiagnosis, data privacy and confidentiality, language and communication barriers, user barriers, and ethical, legal, and accountability concerns.
Lack of network coverage and IT infrastructure
Weak network coverage (Banerjee et al., 2021; Desingh and Baskaran, 2021; Menon et al., 2021; Puliyath et al., 2020; Raheja et al., 2021; Sampathkumar et al., 2022; Sandhu et al., 2021; Ullas et al., 2021), and lack of IT infrastructure (Desingh and Baskaran, 2021) were described as key barriers to digital transformation in the health sector. Relatedly, a lack of basic technical infrastructures, such as smartphones, is a potential barrier to implementing digital health in India (Kumar et al., 2021; Puliyath et al., 2020; Sandhu et al., 2021). In this context, patients had to use their family members’ smartphones to attend teleconsultations (Garg et al., 2021).
High installation and operating costs
Financial concern was identified as a barrier to implementing and adopting digital transformation in the health sector (Bairapareddy et al., 2021; Bhatt et al., 2018). A study by Powell et al., (2017) revealed that hospitals that had EHR systems perceived several barriers to implementation, including the capital required to buy and implement an EHR, concerns about the ongoing cost of maintaining an EHR system, and the ambiguity on the return on investment (ROI) from an EHR (Powell et al., 2017). Relatedly, the lack of repair facilities at installation sites also acts as a major barrier (Menon et al., 2021). On the other hand, the qualitative interviews in a study revealed the high cost of smart devices as a barrier to using mobile-based apps for health care (Sinha Deb et al., 2018).
Lack of medical records and experts
Digital health is a novel platform in India that has been developing recently. Rapid implementation of digital transformation can lead to difficulty in the availability of EHRs (Menon et al., 2021; Puliyath et al., 2020) and experts in the country (Bairapareddy et al., 2021). A study reported that the main difficulties for clinicians in the use of teleconsultation include a lack of expertise in operating technology (Sandhu et al., 2021). Similarly, in another study, 53% of healthcare professionals identified a lack of expertise to be the chief barrier to the effective implementation of smartphone-based telerehabilitation programs for chronic obstructive pulmonary disease patients (Bairapareddy et al., 2021).
Lack of physical examination
One of the key barriers to the acceptance of digital health is the absence of physical examination, a necessary prerequisite for an effective doctor-patient relationship (Kumar et al., 2021; Mathew et al., 2021; Puliyath et al., 2020; Raheja et al., 2021; Ullas et al., 2021). Besides, patients expressed dissatisfaction with the rapport they otherwise established following an in-person consultation (Garg et al., 2021). Similarly, in a study by D’Souza et al. (2021), elderly patients prefer face‑to‑face consultations. This flaw of digital transformation might be remedied by referring any patient whose symptoms or reports necessitate a physical examination to a nearby healthcare center (Kumar et al., 2021).
Data accuracy and misdiagnosis
Another possible barrier to the successful implementation of digital health practice is the accuracy of data transmission. In a study by Raheja et al. (2021), six percent of participants faced difficulties during teleconsultations because of misinterpretation of prescriptions by patients or pharmacists. Similarly, it was difficult for the patients to comprehend the medical advice and medicines attributed to limited connectivity (Banerjee et al., 2021), unfamiliar technology (Sinha Deb et al., 2018; Ghoshal et al., 2021; Sandhu et al., 2021; Ullas et al., 2021), illiteracy (D’Souza et al., 2021; Kumar et al., 2021; Naveen et al., 2021), and lack of clarity of advice given by clinicians (Sandhu et al., 2021).
Data privacy and confidentiality
Compared with in-person consultations, digital health is more vulnerable to security and privacy risks. Data protection is threatened in a digital health system due to the leakage of confidential information and data sharing with third-party apps (Biswas et al., 2020; Menon et al., 2021). Concerns about data security and confidentiality pose significant challenges to the adoption of digital health transformation since the healthcare industry is one of the most critical sectors owing to the very sensitive patient data that has to be secured (Desingh and Baskaran, 2021; Powell et al., 2017; Prakash and Das, 2022; Puliyath et al., 2020; Thenral and Annamalai, 2021; Ullas et al., 2021).
Language and communication barriers
Effective patient-provider communication is essential and is often connected to the success of digital health. This is indeed a challenge during the implementation of digital transformation in the health sector (Menon et al., 2021; Mathew et al., 2021; Naveen et al., 2021; Raheja et al., 2021). Language is one of the critical issues of digital transformation (Sinha Deb et al., 2018; Mohan et al., 2017; Naveen et al., 2021; Sandhu et al., 2021). In their study, Satgunam et al. (2021) reported that although most respondents found downloading and using teleconsultation apps comfortable, patients who could not follow the English language may face some difficulty dealing with the applications. Further, Pandey et al. (2020) reported that poor means of communication on the patient’s side could be a possible reason for reduced teleconsultations. Relatedly, another study by Kumar et al. (2021) showed that the unavailability of proper surroundings for communication is a major barrier to integrating teleconsultations into practice. Notably, two studies reported that video-based teleconsultations are patients’ most preferred mode of communication (Raheja et al., 2021; Nair et al., 2021).
Usage barriers
Several user challenges in digital health serve as barriers to adopting digital transformation in the healthcare industry. Findings highlight various barriers to the use of teleconsultations, such as difficulty in getting an appointment with a routine doctor or obtaining medicine on time (Ullas et al., 2021), long-distance travel for lab tests and reports uploading, at least two in-person consultations before transiting to digital mode (Shambu et al., 2021), dependence on computers and digital technicians (Faujdar et al., 2021), lack of repair facilities at installation sites (Menon et al., 2021), and challenges in availability of drugs (Kumar et al., 2021).
Ethical, legal, and accountability concerns
A common reason for not using digital consultations was the concern for possible legal implications. While implementing teleconsultations, there is a risk of misdiagnosis, which might have severe medicolegal repercussions (Pandey et al., 2020). Relatedly, in a study by Thenral and Annamalai (2021), the problems related to ethical, legal, and accountability implications were cited as challenges to digital consultations by almost all respondents. Additionally, another study reported that the increased transparency in implementing the digital health system made healthcare professionals feel insecure because it increased their work stress and they had to be more careful with data entry (Faujdar et al., 2021).
Discussion
This systematic review included 26 studies highlighting various factors that impede the implementation of digital transformation in the health sector of India. The Government of India is taking the lead in creating a National Digital Health Ecosystem to support international initiatives aimed at accelerating innovation and digital health to meet Sustainable Development Goal (SDG) 3 (NDHM, 2020). However, any change to the current system will face some opposition; thus, it is crucial to comprehend why stakeholders resist it so that change agents can develop action plans effectively. In this context, the current study is crucial as it reports common barriers to digital health implementation including lack of network coverage and IT infrastructure, high installation and operating costs, lack of medical records and experts, lack of physical examination, data accuracy and misdiagnosis, data privacy and confidentiality, language and communication barriers, user barriers, and ethical, legal, and accountability concerns.
Lack of network coverage and IT Infrastructure capture barriers associated with the availability of internet connectivity and smartphones to implement digital transformation in healthcare organizations. The review found that limited internet access hampers digital health services in India. Restricted internet connectivity and access to adequate medical equipment are the country’s main infrastructural problems in digital health, among other things. These results corroborate those of Alkhaldi et al. (2014), which reported that infrastructure issues in a country, such as limited internet connectivity and proper medical equipment related to digital health. In addition, the current results are consistent with previous reviews that pointed to a lack of technology resources and poor internet access as obstacles to the adoption of digital health in India (Venkataraman et al. 2024; Rajkumar et al., 2023). Similarly, another review reported that issues with network access, such as unstable internet connectivity, could limit the application of digital technology in India, specifically in the North-Eastern states of the country (Maroju et al., 2023). Notably, rural areas lag behind urban areas in access to ICTs as the spectrum allocations in the lower–frequency coverage bands and low investment in technological infrastructure due to decreased revenue from rural areas (Mukherjee et al., 2016).
On the other hand, according to the Telecom Regulatory Authority of India (TRAI), as of September 30, 2022, there were 34.38 crore internet subscribers in rural areas. The central government has implemented plans to enhance connectivity in rural villages, with initiatives like BharatNet aiming to provide high-speed internet access to over 2.5 lakh gram panchayats using optic fiber and wireless technologies. As the demand for internet connectivity grows, optical fiber networks are crucial for the successful implementation of digital healthcare in India. Thus, given the increasing demand for internet connectivity, optical fiber networks are largely becoming the backbone of the successful implementation of digital healthcare in the country. Hence the current review suggests that in addition to these efforts by the government to provide optic fiber to rural areas, it is vital to connect smaller administrative and healthcare institutions, such as public health clinics and health and wellness centers, with larger hospitals and medical college hospitals.
Although the number of smartphone users in India is estimated to reach 1.55 billion by 2040 (Sun, 2023), the present findings report that limited resources at the patients’ end might be a barrier to adopting and using digital health innovations. Relatedly, high installation and maintenance costs hinder digital transformation in the healthcare services industry. Existing evidence from the Indian context indicates that the lower adoption of digital health can be attributed to financial limitations, such as the cost of educating healthcare staff, buying and maintaining equipment, and covering ongoing expenses (Bairapareddy et al., 2021; Ghai, 2020). Thus, the review suggests that economic barriers must be assessed against factors such as technology cost, annual equipment maintenance, and ROI.
Findings highlight that the unavailability of EHRs is one of the key obstacles to digital health transformation. EMR systems are crucial to accessing accurate patient information for providing the best advice (Das et al., 2020). It has been noted that a safe, retrievable EMR with free patient access is necessary for an ideal digital health system. India is making significant strides towards transforming healthcare by establishing a digital health system that will cater to the entire population. This initiative aims to develop longitudinal digital health records for individuals, providing doctors with a more comprehensive understanding of their medical history and past treatments. For instance, the nation has launched several verified registries for different stakeholders such as patients (e.g., The Ayushman Bharat Health Application), healthcare professionals (e.g., Health Professional Registry), health facilities (e.g., Health Facility Registry), drugs available and approved in the country (e.g., Drug Registry). Besides, the Unified Health Interface (UHI) enables easy access to precise and comprehensive healthcare data in India, which can be utilized to shape policies and enhance healthcare outcomes. However, the existing literature reveals that the technological illiteracy of people makes it difficult to implement an EHR system in the country (Bhargava and Sarkar, 2020). Yet, schemes like “Pradhan Mantri Gramin Digital Saksharta Abhiyan”, which targets making one person from every family in rural India digitally literate in the coming years, can have a remarkable impact on the technological literacy of the population.
Further, the review showed that a lack of experts to deliver digital health could impede the implementation of digital transformation. Therefore, along with technological infrastructure, the digital health system should include well-qualified individuals (Safi et al., 2018), and it is crucial to employ and educate the right people to operate technology (Rutledge et al., 2017). A recent review highlighted that a major obstacle to the integration of digital health into the primary and secondary healthcare systems in the country is insufficient training and awareness among healthcare providers regarding the utilization of telehealth and the associated equipment (Venkataraman et al., 2024).
Additionally, the findings indicate that a lack of physical examination is a major barrier to implementing digital transformation in the health sector. Consistent with these findings, an earlier study suggested that patients in India are accustomed to physically visiting hospitals/clinics and may find it difficult to accept medical advice delivered over the phone (Kesavadev et al., 2015). Likewise, a lack of physical examination can lead to challenges regarding data accuracy and establishing rapport, thereby limiting the acceptance of digital health services. Nonetheless, in the evolving healthcare delivery landscape, characterized by the presence of artificial intelligence (AI), AI-enabled capabilities can be effectively employed to foster long-term relationships with patients (Wang et al., 2020; Yu et al., 2021). Previous research has emphasized the utilization of AI in healthcare to perform tasks such as analyzing images, recognizing the voice, implementing precision medicine, and processing clinical notes (Wang et al., 2020). Furthermore, it would enhance the competencies of medical personnel and enable them to cultivate trust and exceptional rapport with patients (Teece et al., 2016). In India, tools powered by AI have transitioned from being an emerging technology segment to an established one. Thus, considering the limited physical examination and the related consequences in digital healthcare, the present findings support the integration of AI in the healthcare system of the country as it is essential to maintain a quality relationship with the patients.
Furthermore, the review suggests that efforts should be directed toward addressing the concerns related to data privacy and confidentiality because of various medicolegal implications associated with digital health. Literature reveals that many legal issues surround digital consultations, including acquiring explicit consent from patients, maintaining patient confidentiality, eliminating the need for an in-person physical examination, prescribing medicines without an accurate diagnosis, and recommending government-prohibited medicines (Ateriya et al., 2018). The health record system in India is rigorously protected by privacy and security regulations, which are essential for ensuring the integrity, confidentiality, and availability of healthcare information. Alongside security requirements, EHRs are also governed by privacy laws specific to the country. The Union Cabinet of India approved the personal data protection bill in 2019, which aims to protect sensitive personal data by requiring explicit consent for its processing and preventing unauthorized access by other organizations. The bill aligns with the IT Act 2000, which safeguards digitally stored and transmitted data through data privacy rules. These rules cover personal information related to psychological and physical health conditions and patient history.
Also, the findings highlight the need to appropriately handle communication and language barriers while using ICT. Thus, along with overcoming the technological and other usage barriers, proper training, improved documentation, better communication, and adherence to information management principles should be maintained to avoid medicolegal issues.
Strengths, limitations, and future recommendations
The strengths of the present review include an evidence-based, comprehensive systematic review methodology that offers a rigorous and replicable opportunity to critically analyse the existing literature in the study area. Additionally, the authors performed data screening, extraction, and synthesis independently. A high inter-rater agreeability observed reduces the risk of single-reviewer bias. Further, the review used a broad search strategy with no restriction on the year of publication to obtain the maximum pertinent studies focused on barriers to implementing digital transformation in the health sector. The present study also identified a significant gap in the existing literature: most included studies took either a patient or provider perspective to understand the barriers to digital health implementation. Therefore, future research can also focus on barriers to digital health adoption and acceptance from the perspective of other relevant stakeholders, such as caregivers, rehabilitation workers, health administrators, researchers, and policymakers.
The current review is not without limitations. Many of the included studies were carried out during the COVID-19 pandemic, which could have influenced the participants’ approach toward implementing digital transformation in the health sector. As a result, studies based on sample data collected even after the pandemic could provide more statistical inferences about perceptions of digital health services among various stakeholders. Further, the review could not include relevant articles published in languages other than English; thus, some articles on these themes in the literature might be missed in the analysis.
Conclusion
The present study sheds light on the potential barriers to the implementation of digital transformation in the health sector of India. The barriers identified include lack of network coverage and IT infrastructure, high installation and operating costs, lack of medical records and experts, lack of physical examination, data accuracy and misdiagnosis, data privacy and confidentiality, language and communication barriers, user barriers, and ethical, legal, and accountability concerns. This comprehensive view of barriers can be a solid foundation for designing future interventions to enhance digital transformation’s acceptance and long-term success in the country’s health sector. The review suggests that the effective implementation of digital transformation requires a partnership among governments, nongovernmental organizations, healthcare professionals, patients, and their caregivers. Findings further highlight the need for policy reform in the country to improve digital healthcare.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information file.
References
Alkhaldi B, Sahama T, Huxley C, Gajanayake R (2014) Barriers to implementing eHealth: a multi-dimensional perspective. Stud Health Technol Inf 205:875–879
Ateriya N, Saraf A, Meshram VP, Setia P (2018) Telemedicine and virtual consultation: the Indian perspective. Natl Med J India 31(4):215–218. https://doi.org/10.4103/0970-258X.258220
Bairapareddy KC, Alaparthi GK, Jitendra RS, Prathiksha, Rao PP, Shetty V, Chandrasekaran B (2021) “We are so close; yet too far”: perceived barriers to smartphone-based telerehabilitation among healthcare providers and patients with Chronic Obstructive Pulmonary Disease in India. Heliyon 7(8):e07857. https://doi.org/10.1016/j.heliyon.2021.e07857
Banerjee D, Vajawat B, Varshney P, Rao TS (2021) Perceptions, Experiences, and challenges of physicians involved in dementia care during the COVID-19 Lockdown in India: a qualitative study. Front Psychiatry 11. https://doi.org/10.3389/fpsyt.2020.615758
Belliger A, Krieger DJ (2018) The Digital Transformation of Healthcare. In: North, K., Maier, R., Haas, O. (eds) Knowledge management in digital change. Progress in IS. Springer, Cham, p 311–326. https://doi.org/10.1007/978-3-319-73546-7_19
Bhargava S, Sarkar R (2020) Impact of COVID-19 pandemic on dermatology practice in India. Indian Dermatol Online J. 11(5):712–719. https://doi.org/10.4103/idoj.IDOJ_240_20
Bhatt S, Isaac R, Finkel M, Evans J, Grant L, Paul B, Weller D (2018) Mobile technology and cancer screening: lessons from rural India. J Glob Health 8(2). https://doi.org/10.7189/jogh.08.020421
Bhattacherjee A, Hikmet N (2007) Physicians’ resistance toward healthcare information technology: a theoretical model and empirical test. Eur J Inf Syst 16:725–737. https://doi.org/10.1057/palgrave.ejis.3000717
Biswas S, Adhikari SD, Gupta N, Garg R, Bharti SJ, Kumar V, Mishra S, Bhatnagar S (2020) Smartphone-based telemedicine service at palliative care unit during nationwide lockdown: our initial experience at a tertiary care cancer hospital. Indian J Palliat Care 26(Suppl 1):S31–S35. https://doi.org/10.4103/IJPC.IJPC_161_20
Census of India (2011). https://censusindia.gov.in/census.website/. Accessed 15 Dec 2022
Choi W, Zheng H, Franklin P, Tulu B (2019) mHealth technologies for osteoarthritis self-management and treatment: a systematic review. Health Inform. J. 25(3):984–1003. https://doi.org/10.1177/1460458217735676
Das AV, Rani PK, Vaddavalli PK (2020) Tele-consultations and electronic medical records driven remote patient care: Responding to the COVID-19 lockdown in India. Indian J. Ophthalmol. 68(6):1007–1012. https://doi.org/10.4103/ijo.IJO_1089_20
Desingh V, Baskaran R (2021) Internet of things adoption barriers in the Indian healthcare supply chain: an ISM-fuzzy MICMAC approach. Int J Health Plann Manag 37(1):318–351. https://doi.org/10.1002/hpm.3331
D’Souza B, Suresh RS, Hisham S, Shetty A, Sekaran VC, Pallagatte MC, G S, Suresh RT (2021) Healthcare delivery through telemedicine during the COVID-19 pandemic: case study from a tertiary care center in South India. Hosp Top 99(4):151–160. https://doi.org/10.1080/00185868.2021.1875277
Faujdar DS, Singh T, Kaur M, Sahay S, Kumar R (2021) Stakeholders’ perceptions of the implementation of a patient-centric digital health application for primary healthcare in India. Health Inf Res 27(4):315–324. https://doi.org/10.4258/hir.2021.27.4.315
Fitzgerald M, Kruschwitz N, Bonnet D, Welch M (2014) Embracing digital technology: a new strategic imperative. MIT Sloan Manag Rev 55(2):1
Garg D, Majumdar R, Chauhan S, Preenja R, Parihar J, Saluja A, Dhamija RK (2021) Teleneurorehabilitation among person with Parkinson’s disease in India: the initial experience and barriers to implementation. Ann Indian Acad Neurol 24(4):536–541. https://doi.org/10.4103/aian.AIAN_127_21
Ghai S (2020) Teledentistry during COVID-19 pandemic. Diabetes Metab Syndr 14(5):933–935. https://doi.org/10.1016/j.dsx.2020.06.029
Ghoshal UC, Sahu S, Biswas SN, Singh P, Chaudhary M, Ghoshal U, Tiwari P, Rai S, Mishra SK (2021) Care of inflammatory bowel disease patients during coronavirus disease‐19 pandemic using digital health‐care technology. JGH Open 5(5):535–41. https://doi.org/10.1002/jgh3.12498
Gleiss A, Lewandowski S (2022) Removing barriers for digital health through organizing ambidexterity in hospitals. J Public Health 30:21–35. https://doi.org/10.1007/s10389-021-01532-y
Heath M, Porter TH (2019) Change management overlooked: physician perspectives on EHR implementation. Am J Bus 34(1):19–36. https://doi.org/10.1108/AJB-09-2017-0028
Hinings B, Gegenhuber T, Greenwood R (2018) Digital innovation and transformation: an institutional perspective. Inf Organ 28(1):52–61. https://doi.org/10.1016/j.infoandorg.2018.02.004
Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon MP, Griffiths F, Nicolau B, O’Cathain A, Rousseau MC, Vedel I, Pluye P(2018) The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf 34(4):285–291. https://doi.org/10.3233/EFI-180221
Ilie V, Turel O (2020) Manipulating user resistance to large-scale information systems through influence tactics. Inf Manag 57(3):103178. https://doi.org/10.1016/j.im.2019.103178
Kelly ME, Duff H, Kelly S, McHugh Power JE, Brennan S, Lawlor BA, Loughrey DG (2017) The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: a systematic review. Syst Rev 6(1):259. https://doi.org/10.1186/s13643-017-0632-2
Kesavadev J, Saboo B, Shankar A, Krishnan G, Jothydev S (2015) Telemedicine for diabetes care: an Indian perspective—feasibility and efficacy. Indian J Endocrinol Metab 19(6):764–769. https://doi.org/10.4103/2230-8210.167560
Kraus S, Schiavone F, Pluzhnikova A, Invernizzi AC (2021) Digital transformation in healthcare: analyzing the current state-of-research. J Bus Res 123:557–567. https://doi.org/10.1016/j.jbusres.2020.10.030
Kumar P, Aggarwal M, Dhawan R, Dass J, Kumar G, Sharma V, Mirza S, Senapati J, Ganju N, Vaid T, Vijayran M, Panda T, Pragna GS, Krishna SS, Khandelwal A, Verghese R, Tyagi S, Seth T, Mahapatra M (2021) Tele-medicine services in hematological practice during covid pandemic: its feasibility and difficulties. Indian J Hematol Blood Transfus 37(4):528–533. https://doi.org/10.1007/s12288-020-01385-7
Maroju RG, Choudhari SG, Shaikh MK, Borkar SK, Mendhe H (2023) Role of telemedicine and digital technology in public health in India: a narrative review. Cureus 15(3):e35986. https://doi.org/10.7759/cureus.35986
Sun S (2023). Smartphone users in India 2010–2040. https://www.statista.com/statistics/467163/forecast-of-smartphone-users-in-india/. Accessed 17 Jan 2024
Martin A (2008) Digital Literacy and the “digital society”. Digital Lit Concepts Polic Pract. 30(151):1029–55
Mathew DE, Bothra V, Mathur S, John CM, John NS, Nayak S, Kumar S (2021) Patient perceptions about virtual clinical consultations during current COVID-19 pandemic: a multi-city survey across India. Indian J Community Health 33(2):368–372. https://doi.org/10.47203/ijch.2021.v33i02.025
Menon AK, Adhya S, Kanitkar M (2021) Health technology assessment of telemedicine applications in Northern borders of India. Med J Armed Forces India 77(4):452–458. https://doi.org/10.1016/j.mjafi.2021.03.007
Mohan B, Sharma S, Sharma S, Kaushal D, Singh B, Takkar S, Aslam N, Goyal A, Wander GS (2017) Assessment of knowledge about healthy heart habits in urban and rural population of Punjab after SMS campaign—a cross-sectional study. Indian Heart J. 69(4):480–484. https://doi.org/10.1016/j.ihj.2017.05.007
Monaghesh E, Hajizadeh A (2020) The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health 20(1):1193. https://doi.org/10.1186/s12889-020-09301-4
Moola S, Munn Z, Sears K, Sfetcu R, Currie M, Lisy K, Tufanaru C, Qureshi R, Mattis P, Mu P (2015) Conducting systematic reviews of association (etiology): The Joanna Briggs Institute’s approach. Int J Evid Based Health 13(3):163–169. https://doi.org/10.1097/XEB.0000000000000064
Mukherjee E, Mazar O, Aggarwal R, Kumar, R (2016). Exclusion from digital infrastructure and access. Digital Empowerment Foundation
Nair PP, Aghoram R, Thomas B, Bharadwaj B, Chinnakali P (2021) Video teleconsultation services for persons with epilepsy during COVID-19 pandemic: An exploratory study from public tertiary care hospital in Southern India on feasibility, satisfaction, and effectiveness. Epilepsy Behav 117:107863. https://doi.org/10.1016/j.yebeh.2021.107863
National Digital Health Mission, Make In India (2020). https://www.makeinindia.com/national-digital-health-mission. Accessed 19 Jan 2024
National Health Profile (2019). http://www.cbhidghs.nic.in/showfile.php?lid=1147. Accessed 16 Dec 2022
Naveen R, Sundaram TG, Agarwal V, Gupta L (2021) Teleconsultation experience with the idiopathic inflammatory myopathies: a prospective observational cohort study during the COVID-19 pandemic. Rheumatol Int 41(1):67–76. https://doi.org/10.1007/s00296-020-04737-8
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Pandey N, Srivastava RM, Kumar G, Katiyar V, Agrawal S (2020) Teleconsultation at a tertiary care government medical university during COVID-19 Lockdown in India—a pilot study. Indian J Ophthalmol 68(7):1381–1384. https://doi.org/10.4103/ijo.IJO_1658_20
Powell AC, Ludhar JK, Ostrovsky Y (2017) Electronic health record use in an affluent region in India: findings from a survey of Chandigarh hospitals. Int J Med Inf 103:78–82. https://doi.org/10.1016/j.ijmedinf.2017.04.011
Prakash AV, Das S (2022) Explaining citizens’ resistance to use digital contact tracing apps: a mixed-methods study. Int J Inf Manag 63:102468. https://doi.org/10.1016/j.ijinfomgt.2021.102468
Puliyath N, Huda F, Rai A, Munnamgi S, David LE, Kumar P, Saxena V, Basu S (2020) The utility of telemedicine in general surgery during the Covid-19 pandemic and beyond: our experience. Int J Curr Med Pharm Res 6:5455–5458. https://doi.org/10.24327/23956429.ijcmpr202012939
Raheja A, Manjunath N, Garg K, Tandon V, Gupta V, Mishra S, Ather S, Suri A, Chandra PS, Singh M, Shariff A, Kale SS (2021) Turning a new chapter in neurosurgery outpatient services: telemedicine a “savior” in this pandemic. Neurol India 69(2):344–351. https://doi.org/10.4103/0028-3886.314523
Rajkumar E, Gopi A, Joshi A, Thomas AE, Arunima NM, Ramya GS, Kulkarni P, Rahul P, George AJ, Romate J, Abraham J (2023) Applications, benefits and challenges of telehealth in India during COVID-19 pandemic and beyond: a systematic review. BMC Health Serv Res 23(1):7. https://doi.org/10.1186/s12913-022-08970-8
Rutledge CM, Kott K, Schweickert PA, Poston R, Fowler C, Haney TS (2017) Telehealth and eHealth in nurse practitioner training: current perspectives. Adv Med Educ Pract 8:399–409. https://doi.org/10.2147/AMEP.S116071
Safi S, Thiessen T, Schmailzl KJ (2018) Acceptance and resistance of new digital technologies in medicine: qualitative study. JMIR Res Protoc 7(12):e11072. https://doi.org/10.2196/11072
Sampathkumar S, Sankar M, Ramasamy S, Sriram N, Saravanan P, Ram U (2022) Uptake, engagement and acceptance, barriers and facilitators of a text messaging intervention for postnatal care of mother and child in india-a mixed methods feasibility study. Int J Environ Res Public Health 19(15):8914. https://doi.org/10.3390/ijerph19158914
Sandhu A, Agarwal A, Kaur P, Sharma M, Sra H, Singh M, Jaiswal N, Chauhan A, Gupta A, Singh M (2021) Evaluation of Tele-rheumatology during the COVID-19 pandemic in Asian population: a pilot study. Int J Telemed Appl:5558826. https://doi.org/10.1155/2021/5558826
Sarradon-Eck A, Bouchez T, Auroy L, Schuers M, Darmon D (2021) Attitudes of general practitioners toward prescription of mobile health apps: qualitative study. JMIR Mhealth Uhealth 9(3):e21795. https://doi.org/10.2196/21795
Satgunam P, Thakur M, Sachdeva V, Reddy S, Rani PK (2021) Validation of visual acuity applications for teleophthalmology during COVID-19. Indian J. Ophthalmol. 69(2):385–390. https://doi.org/10.4103/ijo.IJO_2333_20
Shambu SK, B SPS, Gona OJ, Desai N, B M, Madhan R, V R (2021) Implementation and evaluation of virtual anticoagulation clinic care to provide incessant care during COVID-19 times in an Indian tertiary care teaching hospital. Front Cardiovasc Med 8:648265. https://doi.org/10.3389/fcvm.2021.648265
Singh V, Sarbadhikari SN, Jacob AG, John O (2022) Challenges in delivering primary care via telemedicine during COVID-19 pandemic in India: A review synthesis using systems approach. J Fam Med Prim Care 11(6):2581–2588. https://doi.org/10.4103/jfmpc.jfmpc_1559_21
Sinha Deb K, Tuli A, Sood M, Chadda R, Verma R, Kumar S, Ganesh R, Singh P (2018) Is India ready for mental health apps (MHApps)? A quantitative-qualitative exploration of caregivers’ perspective on smartphone-based solutions for managing severe mental illnesses in low resource settings. PLoS One 13(9):e0203353. https://doi.org/10.1371/journal.pone.0203353
Smartphone users in India 2010–2040 (2023). https://www.statista.com/statistics/467163/forecast-of-smartphone-users-in-india/. Accessed 2 Jan 2024
Talwar M, Talwar S, Kaur P, Tripathy N, Dhir A (2021) Has financial attitude impacted the trading activity of retail investors during the COVID-19 pandemic? J. Retail Consum Serv. 58:102341. https://doi.org/10.1016/j.jretconser.2020.102341
Teece DJ, Pisano G, Shuen A (2016) Dynamic capabilities and strategic management. Strateg Manag J 18(7):509–533. http://www.jstor.org/stable/3088148
Thenral M, Annamalai A (2021) Challenges of building, deploying, and using AI-enabled telepsychiatry platforms for clinical practice among urban Indians: a qualitative study. Indian J. Psychol. Med 43(4):336–342. https://doi.org/10.1177/0253717620973414
Ullas S, Pradeep M, Surendran S, Ravikumar A, Bastine AM, Prasad A, Mohan A (2021) Telemedicine during the COVID-19 pandemic: a paradigm shift in non-communicable disease management?—A cross-sectional survey from a quaternary-care center in South India. Patient Prefer Adherence 15:2715–2723. https://doi.org/10.2147/PPA.S332636
Venkataraman A, Fatma N, Edirippulige S, Ramamohan V (2024) Facilitators and Barriers for Telemedicine Systems in India from Multiple Stakeholder Perspectives and Settings: A Systematic Review. Telemedicine journal and e-health: the official journal of the American Telemedicine Association. Advanced online publication. https://doi.org/10.1089/tmj.2023.0297
Wang Y, Xiong M, Olya H (2020) Toward an understanding of responsible artificial intelligence practices. In Proceedings of the 53rd Hawaii International Conference on System Sciences. Hawaii International Conference on System Sciences (HICSS), pp. 4962–4971
World Health Organization (2021). https://www.who.int/health-topics/digital-health#tab=tab_1. Accessed 17 Dec 2022
Yu M, Tang A, Brown K, Bouchakri R, St-Onge P, Wu S, Reeder J, Mullie L, Chassé M (2021) Integrating artificial intelligence in bedside care for covid-19 and future pandemics. BMJ 375:e068197. https://doi.org/10.1136/bmj-2021-068197
Zobair KM, Sanzogni L, Sandhu K (2020) Telemedicine healthcare service adoption barriers in rural Bangladesh. Australas J Inf 24. https://doi.org/10.3127/ajis.v24i0.2165
Author information
Authors and Affiliations
Contributions
Conceptualization: SI, ER, AG; Methodology: SI, AG, ER; Investigation: SI, RE, AG, KSVM; Formal analysis: SI, ER, KSVM, KSS; Data curation: SI, AG, KSVM, KSS; Writing—original draft: ER, AG, KSVM, KSS; Writing—review and editing: SI, ER, AG; Validation: ER; Visualization: AG, KSVM, KSS.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study is designed to provide an objective, honest, and unbiased review. This article does not contain any studies with human participants performed by any of the authors.
Informed consent
This article does not contain any studies with human participants performed by any authors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Inampudi, S., Rajkumar, E., Gopi, A. et al. Barriers to implementation of digital transformation in the Indian health sector: a systematic review. Humanit Soc Sci Commun 11, 632 (2024). https://doi.org/10.1057/s41599-024-03081-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1057/s41599-024-03081-7