Abstract
Subjectivity and ambiguity of visual field classification limits the accuracy and reliability of glaucoma diagnosis, prognostication, and management decisions. Standardised rules for classifying glaucomatous visual field defects exist, but these are labour-intensive and therefore impractical for day-to-day clinical work. Here a web-application, Glaucoma Field Defect Classifier (GFDC), for automatic application of Hodapp-Parrish-Anderson, is presented and validated in a cross-sectional study. GFDC exhibits perfect accuracy in classifying mild, moderate, and severe glaucomatous field defects. GFDC may thereby improve the accuracy and fairness of clinical decision-making in glaucoma. The application and its source code are freely hosted online for clinicians and researchers to use with glaucoma patients.
Similar content being viewed by others
Introduction
Glaucoma is a heterogenous group of diseases characterised by cupping of the optic nerve head and visual-field damage1. It is the most frequent cause of irreversible blindness worldwide2. Interpretation of visual fields is an essential part of diagnosis, severity grading, and prognostication in glaucoma. However, clinical assessment of visual fields is unreliable due to subjectivity and ambiguity in guidance documentation3. This leads to differential treatment of patients based on arbitrary factors which can lead to adverse outcomes. For instance, decisions to certify patients as visually impaired depend on the severity of patients’ visual field defects which are explicitly defined as a clinical decision (rather than being based on explicit objective criteria) in United Kingdom guidelines4. Patients eligible for social support due to sight impairment are frequently unregistered as a consequence of such subjectivity5,6,7. Glaucoma patients eligible on the basis of visual field defects are significantly more likely to miss out on registration than patients eligible on the basis of visual acuity, because of significant disagreement between ophthalmologists evaluating visual fields using idiosyncratic and subjective clinical criteria6,8,9,10. Moreover, risk stratification of glaucoma patients is a priority when timely glaucoma care is challenged by increasing demand for services, as was highlighted during the COVID pandemic11. Staging glaucomatous field defects is an important component of such risk stratification12.
Standardised rules for classifying glaucomatous field defects were proposed by Hodapp, Parish, and Anderson in 1993, who defined ‘early’, ‘moderate’, and ‘severe’ defects based on the mean deviation, global plot, and pattern deviation on Humphrey visual field test printouts13. The Hodapp-Parish-Anderson (HPA) criteria have been used widely in research studies for their clarity and reproducibility, and HPA decisions align closer with glaucoma subspecialists than general ophthalmologists without specific expertise9,14. Moreover, the HPA criteria are less likely to underestimate the severity of glaucomatous damage than simpler global parameters such as mean deviation or the visual field index, perhaps because they incorporate mean deviation in addition to other parameters15,16. However, use in regular clinical practice is limited due to the labour intensive requirement to evaluate multiple parameters presented on perimetry plots for every assessment. Accelerating incorporation of HPA criteria into clinical workflows could improve the accuracy, reliability, and fairness of visual field assessment for glaucoma patients. Here, GFDC (Glaucoma Field Defect Classifier), a web-application which automates grading based on HPA criteria without requiring patient-identifiable data to be inputted, is presented and validated.
Accuracy and practicality
For every perimetry result, GFDC web-application output matched the ground truth defined by human researchers applying HPA criteria (Fig. 1). As no fields with glaucomatous field defects were classified as having no defect, and no severe defects were classified as exhibiting a mild or moderate defect, the sensitivity of detecting any glaucomatous field defect and a severe glaucomatous field defect was 100%. Specificity for detecting severe glaucomatous field defects was also 100%. As no fields exhibited no field defect, the specificity of detecting any glaucomatous field defect was undefined. Accuracy overall and F1 score for detecting severe glaucomatous field defect were 100%. Agreement between human graders (ground truth) and GFDC was perfect (κ = 1.00). Blinded human researchers appraising the same plots exhibited disagreement in 5 cases (κ = 0.97).
A contingency table depicting perfect agreement between glaucomatous field defect classification by human researchers (y-axis) and the Glaucoma Field Defect Classifier (GFDC; x-axis) when using Hodapp-Parrish-Anderson criteria to grade perimetry results. In every case, GFDC reached the same conclusion as the ground truth defined by human researchers, indicating perfect accuracy.
Perimetry appraisal using GFDC was significantly faster than manual application of HPA criteria (Table 1). However, the duration of manual appraisal exhibited greater variation, with some manual assessments being faster than any GFDC-facilitated assessment. Researchers commented that they did not need to apply every HPA criterion in some cases, such as where mean deviation was sufficient to grade a field defect as severe irrespective of other parameters. Allowing researchers to make similar judgements when using GFDC—for instance, instantly interpreting mean deviation readings less than -20 dB as severe rather than inputting all parameters into GFDC—would likely decrease the average duration and increase the variability of duration of GFDC-facilitated appraisal in a similar fashion.
Interpretability and explainability
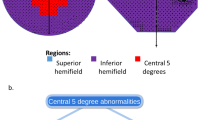
Simple thresholds for mean deviation and central global plot decibel values (detailed in Table 2) are explicitly coded into the algorithm. To interpret pattern deviation plots, a computer vision algorithm is designed to identify plot boundaries and result points as shown in Fig. 1. A matrix is generated based on the pattern deviation identified at each result point (Fig. 2), which is then used to apply encoded HPA criteria described in Table 1.
A screenshot taken from model diagnostics and interpretability work undertaken during development of the Glaucoma Field Defect Classifier (GFDC). A computer vision algorithm recognises the bounds of the pattern deviation plot and superimposes a grid to capture test loci, before categorising pattern deviation at each locus to facilitate count computation and application of Hodapp-Parrish-Anderson criteria. The same schema may be applied to work with different plot sizes, colour schemes, legends, and perimetry parameters such as total points (e.g. 30-2 rather than 24-2 SITA), and defined significance levels. Alternative classification criteria may also be incorporated.
The web-application validated here has the potential to facilitate incorporation of HPA-based visual field assessment at scale. 100% sensitivity for detection of any glaucomatous field defect and a severe field defect suggests that no patients would be dismissed as a false negative by GFDC, maximising safety with deployment. 100% specificity for detecting severe field defects indicates that the algorithm can identify patients at high risk or with significant deficits without compromising efficiency by including other patients as false positives. Adopting standard criteria for visual field appraisal in glaucoma clinics would ameliorate one of the most severe sources of arbitrary discrepancy in diagnosis, assessment of progression, prognosis, and identification of vision impairment.6,7,14 Using an explicitly coded computer vision algorithm reduces the time-requirement for clinicians to leverage validated criteria, overcomes black box limitations associated with machine learning approaches, and minimises the possibility of erroneous decisions made for uninterpretable reasons17. Another application may be in providing a more precise and systematic approach to the grading of visual fields required by some countries’ social service benefit criteria. For example, an automated HPA interpretation of an integrated binocular visual field may offer more specificity than the visual field index (as used in some countries), in judging visual function or disability.
Two limitations should be considered alongside potential applications of the web-application. First, HPA criteria may overestimate or underestimate glaucomatous damage, and alternative criteria may be more appropriate for clinical practice9,15,18. Second, different perimetry machines may display results in formats incompatible with the code used above. Both limitations may be ameliorated by simple modifications to the published code, which can be easily adapted to adjust criteria for classification, incorporate other classification schemata, or work with alternative results formats. Subsequent work is underway using GFDC to explore the clinical utility of automated HPA-based appraisal of glaucoma patients. External research teams are welcome to use and adapt the code and web-application for the benefit of patients and ophthalmologists. Reducing subjectivity of perimetry analysis without compromising clinical accuracy and precision may help ensure glaucoma patients receive equitable and optimal care.
Methods
Web-application development
HPA criteria were distilled into a three-level algorithm corresponding to the format of the 24-2 Humphrey visual field results obtained at a tertiary centre for glaucoma (Table 2)13,19. The algorithm was transposed into Python code accepting three inputs: mean deviation, central four decibel (dB) readings from the global plot, and pattern deviation plot. OpenCV was used to convert pattern deviation plots into matrices with identities corresponding to levels of pattern deviation20. A graphical-user interface was developed in CSS, JavaScript, and HTML, and deployed online for researchers to use (https://gfdc.app). Code is publicly available on a GitHub repository (https://github.com/RohanSanghera/gfdc).
Validation
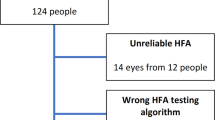
To validate the accuracy of the web-application, its output was compared to human clinical researchers using the same Hodapp-Parish-Anderson criteria (Table 1). 168 consecutively recorded visual fields from glaucoma clinics were used for the study. Each researcher graded 30-40 visual fields, with a total of 168 eyes from 89 patients comprising the validation dataset. To mitigate human error, every visual field was evaluated by two independent researchers, with disagreement resolved by a third researcher acting as arbiter. These human decisions were accepted as gold-standard ground truth and used to define whether the web-application was correct or not for every visual field in the dataset.
To evaluate the practicality of GFDC, a single researcher conducted screening on consecutive records with conventional manual and novel application-facilitated methods in randomised fashion: evaluation method was determined by a coin flip until both methods had been used at least 20 times. A blinded, independent researcher measured the time required to generate a final grading.
This retrospective study comprised part of an ongoing service improvement project (ID4167) granted approval by the Cambridge University Hospitals NHS Foundation Trust Audit Department (PRN10167).
Statistical analysis
Agreement between human researchers and the web-application was quantified through calculation of a Kappa statistic. Confusion matrix analysis was also employed to evaluate the overall accuracy of the web-application in identifying patients with any visual field defect, and a ‘severe’ visual field defect (which would correspond to automatic eligibility for sight impairment certification based on UK guidelines)4. To determine if there was any difference between the duration of appraisal with and without GFDC, a t-test was computed with p = 0.05 taken as the accepted level of statistical significance. Statistical analysis and data visualisation were conducted in R (version 4.1.2; R Foundation for Statistical Computing, Vienna, Austria).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All data required to replicate analyses are available from the authors.
Code availability
All code required to implement GFDC is publically available on a GitHub repository at the following link: https://github.com/RohanSanghera/gfdc.
References
Jonas, J. B. et al. Glaucoma. Lancet 390, 2183–2193 (2017).
GBD 2019 Blindness and Vision Impairment Collaborators & Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health 9, e144–e160 (2021).
Iester, M. et al. Agreement to detect glaucomatous visual field progression by using three different methods: a multicentre study. Br. J. Ophthalmol. 95, 1276–1283 (2011).
Dementia and Disabilities Unit, Social Care, Ageing and Disability Directorate. Certificate of Vision Impairment - Explanatory Notes for Consultant Ophthalmologists and Hospital Eye Clinic Staff in England. (2017).
Barry, R. J. & Murray, P. I. Unregistered visual impairment: is registration a failing system? Br. J. Ophthalmol. 89, 995–998 (2005).
King, A. J. W., Reddy, A., Thompson, J. R. & Rosenthal, A. R. The rates of blindness and of partial sight registration in glaucoma patients. Eye 14, 613–619 (2000).
Guerin, E., Bouliotis, G. & King, A. Visual impairment registration: evaluation of agreement among ophthalmologists. Eye (Lond.) 28, 808–813 (2014).
Banegas, S. A. et al. Evaluation of the retinal nerve fiber layer thickness, the mean deviation, and the visual field index in progressive glaucoma. J. Glaucoma 25, e229–e235 (2016).
Lin, A. P. et al. Agreement of visual field interpretation among glaucoma specialists and comprehensive ophthalmologists: comparison of time and methods. Br. J. Ophthalmol. 95, 828–831 (2011).
Pardhan, S. et al. Confusion around Certification of Vision Impairment (CVI) and registration processes—are patients falling through the cracks? Eye 1–5 https://doi.org/10.1038/s41433-023-02520-0 (2023).
Pujari, R., Chan, G. & Tapply, I. Addenbrooke’s Glaucoma COVID response consortium & Bourne, R. R. The impacts of COVID-19 on glaucoma patient outcomes as assessed by POEM. Eye 36, 653–655 (2022).
Poostchi, A., Kastner, A., Konstantakopoulou, E., Gazzard, G. & Jayaram, H. Clinical risk stratification in glaucoma. Eye (Lond) 1–7 https://doi.org/10.1038/s41433-023-02480-5 (2023).
Hodapp, E., Parrish, R. K. & Anderson, D. R. Clinical Decisions in Glaucoma. in 52–61 (Mosby, Maryland Heights, 1993).
King, A. J. et al. Treatment of Advanced Glaucoma Study: a multicentre randomised controlled trial comparing primary medical treatment with primary trabeculectomy for people with newly diagnosed advanced glaucoma—study protocol. Br. J. Ophthalmol. 102, 922–928 (2018).
De Moraes, C. G. et al. Association of Macular Visual Field Measurements With Glaucoma Staging Systems. JAMA Ophthalmol. 137, 139 (2019).
Sousa, M. C. et al. Suitability of the visual field index according to glaucoma severity. J. Curr. Glaucoma Pr. 9, 65–68 (2015).
Thirunavukarasu, A. J. et al. Large language models in medicine. Nat. Med 29, 1930–1940 (2023).
Stubeda, H. et al. Comparing five criteria for evaluating glaucomatous visual fields. Am. J. Ophthalmol. 237, 154–163 (2022).
Brusini, P. & Johnson, C. A. Staging functional damage in glaucoma: review of different classification methods. Surv. Ophthalmol. 52, 156–179 (2007).
Bradski, G. The OpenCV Library. Dr. Dobb’s Journal of Software Tools (2000).
Acknowledgements
The authors extend their thanks to Professor David Crabb (Department of Optometry and Visual Sciences, City, University of London) for his assistance with distilling Hodapp-Parrish-Anderson criteria into a workable algorithm for computer vision-based analysis.
Author information
Authors and Affiliations
Contributions
A.J.T., N.J., H.C.C.Y. and R.B. conceptualised the study. A.J.T., R.S. and F.L. developed the application and undertook troubleshooting exercises. A.J.T., N.J., S.M., A.E. and H.C.C.Y. collected data and undertook manual grading to validate the application. A.J.T. conducted data analysis and visualisation. A.J.T. and R.B. coordinated the research team. R.B. provided resources and academic supervision. A.J.T. wrote the manuscript with feedback from N.J., R.S., F.L., S.M., A.E., H.C.C.Y. and R.B.
Corresponding authors
Ethics declarations
Competing interests
R.B. has received consultancy fees/honoraria from Thea, Santen, and AbbVie. A.J.T. and R.S. have received funding from HealthSense for research work unrelated to this study. The remaining authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thirunavukarasu, A.J., Jain, N., Sanghera, R. et al. A validated web-application (GFDC) for automatic classification of glaucomatous visual field defects using Hodapp-Parrish-Anderson criteria. npj Digit. Med. 7, 131 (2024). https://doi.org/10.1038/s41746-024-01122-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-024-01122-8